pharmacology exam 4
1/161
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
162 Terms
true/false: most cases of hypertension are asymptomatic
true
baroreceptors
pressure sensitive neurons in aortic arch, carotid sinuses, and sympathetic nervous system. responsible for rapid moment-to-moment regulation of bp
renin-angiotensin-aldosterone system
kidney provides long-term regulation of bp. alters blood volume
hypertension treatment strategies
the goal of hypertensive therapy is to reduce cardiovascular and renal morbidity/mortality
lowering bp even a modest amount significantly reduces cardiovascular disease
mild hypertension can be treated w one drug along with lifestyle changes. however, most patients req more than one drug to help control their bp
diuretics (3)
can be used as first-line drug therapy for hypertension. lowers blood volume
low dose is safe, inexpensive, effective
can combine w other meds
beta-adrenoceptor blocking agents — description
used as a first-line drug therapy for hypertension when other diseases are present
beta-adrenoceptor blocking agents — therapeutic use and 5 examples
hypertensive patients with concomitant diseases — useful in treating conditions that may coexist with hypertension
supraventricular tachycardia, previous MI, angina pectoris, chronic heart failure, migraines
beta-adrenoceptor blocking agents — adverse effects (3 categories)
common effects: bradycardia, fatigue, lethargy, insomnia, hallucinations, hypotension, decr libido
alterations in lipid profile: may disturb lipid metab, decr HDL, incr triglycerides
drug withdrawal: abrupt withdrawal can induce angina, MI, or sudden death. must be tapered over 2-3 weeks
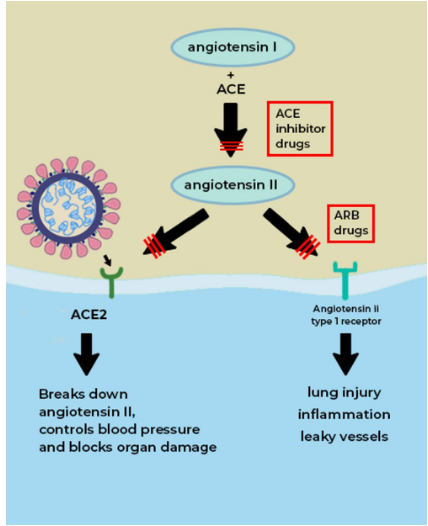
ACE inhibitors overview
recommended when diuretics or beta blockers are ineffective or can’t be used
ACE inhibitors — therapeutic uses (2)
management of patients w chronic heart failure
standard in care of patients who have had MI
ACE inhibitors — adverse effects (6)
dry cough, rash, fever, altered taste, hypotension, hyperkalemia
angiotensin II-receptor antagonists (ARBs) (4)
alternatives to ACE inhibitors
block the AT1 receptors
effects similar to those of ACE inhibitors
adverse effects are similar to ACE inhibitors — also toxic to fetuses
renin inhibitors (4)
directly inhibits renin
lowers bp as effectively as ARBs, ACE inhibitors, and diuretics
can be combined w any of the treatments listed above
can’t be used if woman is pregnant
calcium-channel blockers overview (2)
recommended when the first line agents are not effective or can’t be prescribed
effective in patients that are hypertensive with angina or diabetes
3 classes of calcium channel blockers
diphenylalkylamines (higher affinity for heart)
benzothiazepines (higher affinity for heart)
dihydropyridines (higher affinity for blood vessels)
calcium channel blockers actions (2)
antagonists block the inward movement of calcium by blocking L-type channels
causes smooth muscle to relax and dilates many arterioles
calcium channel blockers therapeutic uses (3)
natural natriuretic effects (discharge of sodium thru urine)
don’t req use of diuretics
useful in treating patients w asthma, diabetes, and/or peripheral vascular disease
calcium channel blockers adverse effects (3)
constipation occurs in 10% of patients
dizziness, fatigue
should be avoided in patients with congestive heart failure — HF due to systolic dysfunction (contractility problem) rather than diastolic dysfunction (relaxation + abnormal filling problem)
centrally acting adrenergic drugs — clonidine (catapres, kapvay, nexiclon) (3)
decr sympathetic output in brain stem
alpha2-agonists that are used to treat hypertensive patients who have not responded to 2+ drugs
does not decr renal flow
centrally acting adrenergic drugs — alpha-methyldopa (3)
inhibits DOPA decarboxylase which decr sympathetic output
alpha2-agonist
does not decr renal blood flow
vasodilators
act by producing relaxation of vascular smooth muscle
these actions cause reflex actions that incr contractility and heart rate. can lead to MI, angina pectoris, or cardiac failure in predisposed patients
incr renin → incr water retention. can use along w diuretic and beta blocker to decr side effects
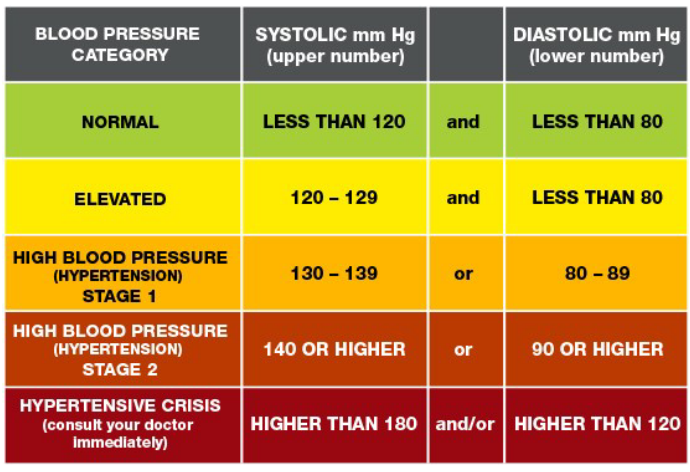
hypertensive emergency
occurs when bp is 180/120 or higher. can cause strokes, MI, damage to organs
therapeutic goal is to rapidly reduce bp
drugs administered thru IV and cause prompt vasodilation. drop in bp has to be smooth. sodium nitroprusside (prodrug that becomes NO). nitroglycerine, calcium channel blockers
3 important dysfunctions of blood that drugs treat
thrombosis — formation of unwanted clot in blood vessel. most common abnormality
bleeding — failure of hemostasis
anemia — low RBC count. nutritional deficiencies or problems w bone marrow
thrombosis vs embolus
thrombus — a clot that adheres to a vessel wall
embolus — a clot that floats in the blood
both are dangerous. may block blood vessels, depriving tissues of oxygen
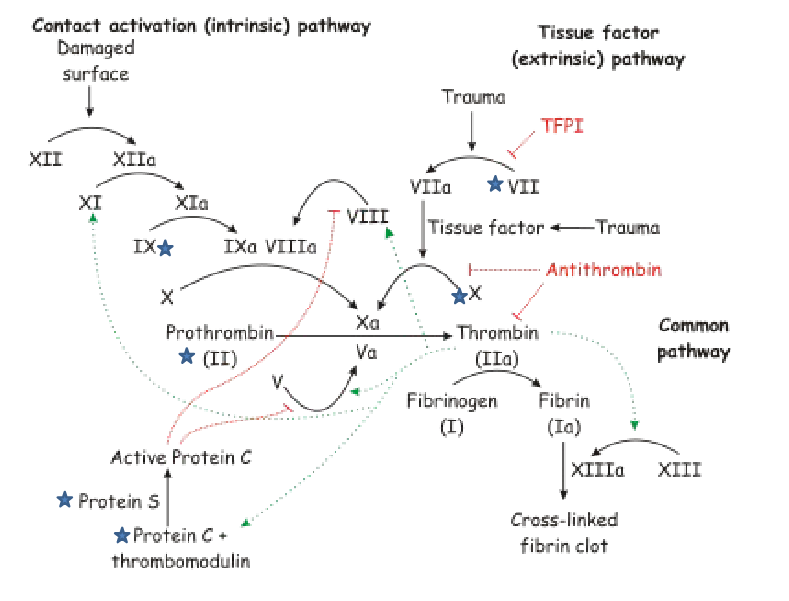
to form a stable clot, there are two pathways that must both work to completion:
platelet plug formation — platelets bind, are activated, and aggregate at injury site. not stable and can be swept away due to shear forces in smaller vessels
fibrin overlay/stable clot formation — activation of many different coagulation factors w the end result being the formation of fibrin
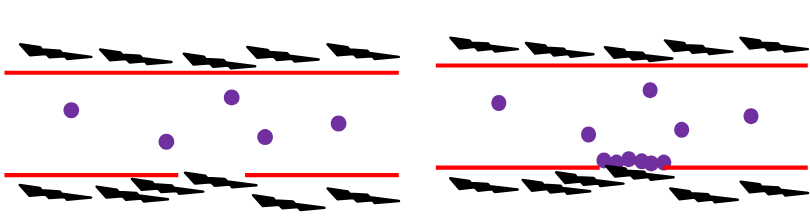
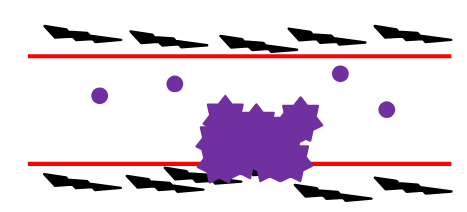
3 steps of platelet response to vascular injury
platelet adhesion
platelet activation/platelet release reaction
platelet aggregation
platelet response to vascular injury step 1 — platelet adhesion (2)
when endothelium is injured, the platelets adhere to and cover the exposed collagen and VWF (von Willebran factor; secreted by endothelial cells, platelet aggregation + attachment to endothelium).
forms a thin layer @ area of injury
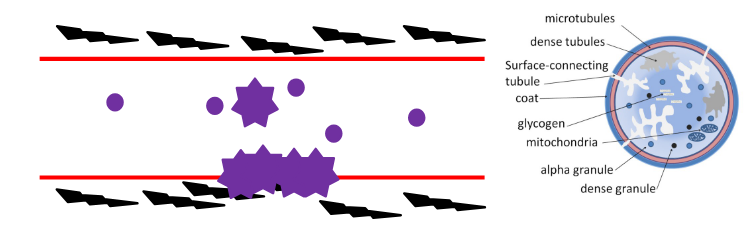
platelet response to vascular injury step 2 — platelet activation / platelet release reaction (3)
platelets undergo morphological changes. will send out pseudopodia and release the contents of alpha and dense granules
the molecules sent out by the activated platelet activate other resting platelets in the circulation
compare to pufferfish blowing up
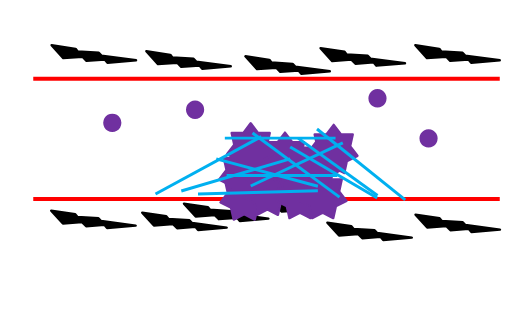
platelet response to vascular injury step 3 — platelet aggregation
platelets aggregate at site of injury and will attach together via various receptors/proteins (main one is GP Ilb/Illa)
stable clot formation (2)
complex series of events involving activation of various factors to their active forms, ultimately leading to formatino of thrombin. thrombin is formed by cleaved of prothrombin by Factor X
thrombin cleaves fibrinogen (soluble) to make fibrin (insoluble). fibrin is incorporated into the growing platelet aggregate — this stabilizes the clot
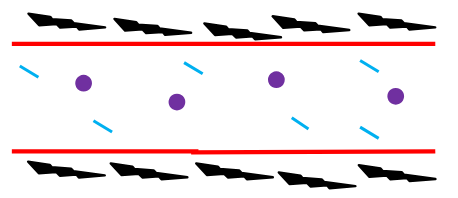
dissolving the clot — fibrinolysis (2)
while the clot is forming, the fibrinolytic pathway is activated locally. plasminogen is cleaved to form plasmin by tPA
plasmin cleaves the fibrin meshwork as the wound heals. releases fibrin degradation products (FDPs)
platelet aggregation inhibitors (3)
aspirin (acetylsalicylic acid)
ticlopidine (ticlid) and clopidogrel (plavix)
abciximab
aspirin (acetylsalicylic acid)
when platelets are stimulated (thrombin, collagen, ADP, etc) this results in activation of phospholipases that cut arachidonic acid from membrane phospholipids
arachidonic acid is converted to prostaglandin H2 by cyclooxygenase (COX) enzyme — prostaglandin H2 is converted to thromboxane A2. thromboxane A2 is released + is essential for rapid formation of a clot + acts as a vasoconstrictor
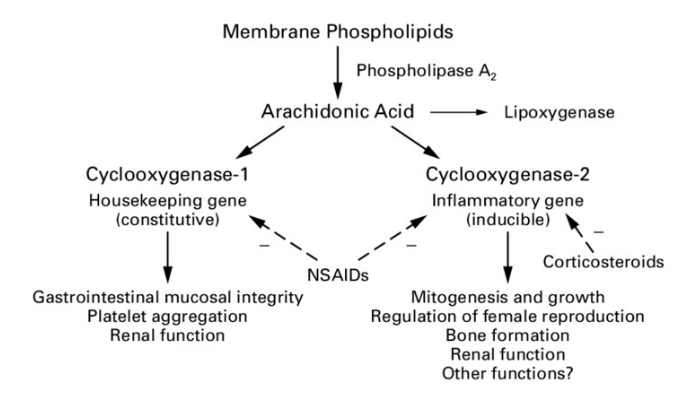
aspirin (non-selective COX inhibitor)
blocks the actions of COX-1 (and COX-2 to a lesser extent) and impedes platelet aggregation
lasts as long as the life of the platelet — 7-10 days
used to prevent transient cerebral ischemia (TIA), prevent stroke, prevent MI, decr mortality in patients who have suffered MI
aspirin cont.
bleeding time is prolonged for those on aspirin treatment. depends on dose given. can be incr incidence of hemorrhagic stroke and GI bleeding
often used w other drugs that have anti-clotting properties
other NSAIDs (like ibuprofen — also non-selective!) inhibit COX-1 and COX-2 by competing with aspirin for the active site
ibuprofen doesn’t have the same bleeding risk as aspirin
ticlopidine (ticlid) and clopidrogel (plavix)
irreversibly inhibit the binding of ADP to its receptors on the platelet. this inhibits the action of GP Ilb/Illa receptors — platelets can’t bind to fibrinogen or each other
ticlopidine is used to prevent ischemic attacks and strokes in patients who have had a prior thrombotic event. has some severe adverse rxns: aplastic anemia (RBC, WBC, platelets), thrombotic thrombocytopenic purpura (TTP — blood clots in small vessels). only used in patients who don’t respond to other therapies

ticlopidine and clopidogrel cont
clopidogrel is used for prevention of atherosclerotic events following MI, stroke, or established PAD. side effects are not as bad as those with ticlopidine but patients can still get TTP
ticlopidine and clopidogrel cont cont
food interferes with absorption of ticlopidine
both bind to plasma proteins
undergo metab by CYP450 system. active metabolites of these drugs have yet to be identified
max effect is in 3-5 days
elim by both renal and fecal routes
abciximab
an antibody to the GP Ilb/Illa receptor
given in IV along with heparin (IV only) or aspirin
usually given to patients during and after coronary artery procedures to prevent platelets sticking together
major side effect is possibility of bleeding
also expensive which limits its use
anticoagulants: inhibition of coagulation (3)
coagulation needs to be restricted to the site of injury
several inhibitors of this system: protein C, protein S, antithrombin III
the mech of action for several of these agents (like heparin) activate the endogenous inhibitors
anticoagulants — thrombin inhibitors: mechanism of action
heparin binds to antithrombin III to form heparin-AT complex (inactivates thrombin and other coagulation factors). speeding up the actions of antithrombin — it normally acts slowly w thrombin and Factor Xa, but with heparin bound, it speeds up the enzymatic rxns by 1000x
LMWHs do the same thing, only just with Factor Xa
anticoagulants — thrombin inhibitors: therapeutic uses (4)
heparin and LMWH prevent fibrin formation
used to treat deep-vein thrombosis and pulmonary embolism
used in patients undergoing surgery to prevent venous thrombosis
treatment of acute MI
anticoagulants — thrombin inhibitors: drugs of choice
heparin and LMWH are the drug of choice for pregnant women because they don’t cross the placenta due to their large size and negative charge
heparin is largely being replaced with LMWHs — use of the LMWH doesn’t req the same intense monitoring → saves on cost
anticoagulants — thrombin inhibitors: pharmacokinetics
absorption — the anticoagulant effect of heparin begins in minutes after IV; 1-2 hrs after SC
the actions of LMWH occurs 4 hours after SC
anticoagulants — thrombin inhibitors: adverse effects (6)
bleeding complications: chief adverse effect of heparin is hemorrhage. bleeding time must be monitored
hypersensitivity rxns: heparin is prepared from pig → risk it may be antigenic
thrombosis: chronic or intermittent admin of heparin can lead to reduction of antithrombin III activity → causes decr in inactivation of coagulation factors and incr risk of thrombosis
thrombocytopenia (low platelets): caused by heparin. type I is common, not serious, occurs within first 5 days of treatment. type II is rare, more dangerous, and can be life-threatening. platelets are activated via an immune response and aggregate (lowers number in circulation). can lead to thrombosis. heparin therapy must be stopped
elevation of aminotransferase levels: indication of liver disease, but when heparin is stopped, levels return to normal
osteoporosis and alopecia can also occur w chronic use
anticoagulants — vitamin K antagonists: overview (2)
warfarin (coumadin) antagonizes the cofactor function of vitamin K
warfarin is widely used as an oral anticoagulant, but use is decr in favor of LMWHs and platelet aggregate inhibitors
anticoagulants — vitamin K antagonists: mechanism of action (4)
several of the coagulation factors req vitamin K as a cofactor (prothrombin, factor VII, factor IX, factor X)
blocks the action of vitamin K epoxide reductase (responsible for activating vit K)
anticoagulant effects are not seen until 8-12 hrs after admin
peak effects seen at 72-96 hrs after admin. this is how long it takes to deplete the pool of clotting factors
anticoagulants — vitamin K antagonists: therapeutic uses (3)
warfarin is used to prevent progression or recurrence of acute deep-vein thrombosis or pulmonary embolism
used for prevention of venous thromboembolism during orthopedic or gynecological surgery
used in patients with MI, chronic atrial fibrillation, prosthetic heart valves
anticoagulants — vitamin K antagonists: pharmacokinetics (2)
warfarin rapidly absorbed after oral admin
can readily cross the placenta
anticoagulants — vitamin K antagonists: fate (2)
catalyzed by CYP450 system
excreted in urine and feces
anticoagulants — vitamin K antagonists: adverse effects (3 bleeding disorders + 1 warning)
hemorrhage is principle adverse effect. if patient bleeds, can be given vit K.
skin lesions and necrosis are rare complications observed primarily in women.
purple toe syndrome — painful, blue-tinged discoloration caused by cholesterol emboli
should NEVER be used during pregnancy
anticoagulants — vitamin K antagonists: drug interactions
EXTENSIVE list of drug interactions that can potentiate its anticoagulant effects
anticoagulants — vitamin K antagonists: disease states (3)
vit K deficiency, hepatic disease, hypermetabolic states
thrombolytic drugs overview
acute thrombolytic disease can be treated with drugs that convert plasminogen to plasmin — plasmin breaks down fibrin to dissolve clots
thrombolytic drugs: therapeutic uses (3)
originally used for treatment of deep-vein thrombosis and pulmonary embolism — these drugs are not being used for these conditions as much anymore
used in restoring catheter and shunt functions by lysing clots that occlude these devices
used to dissolve clots involved in ischemic strokes
thrombolytic drugs: adverse effects (2)
these drugs can’t tell the difference between fibrin in unwanted clot vs one that’s supposed to be there → hemorrhage is a side effect
ppl with healing wounds, pregnant, history of cerebrovascular accident should not be given these drugs
thrombolytic drugs — alteplase: overview, therapeutic uses (3)
formerly known as tPA — a serine protease that cleaves plasminogen to plasmin
approved for treatment of MI, massive pulmonary embolism, acute ischemic stroke
thrombolytic drugs — alteplase: pharmacokinetics and adverse effects
very short half-life (~5 mins)
bleeding complications (GI and cerebral)
drugs used to treat bleeding
bleeding disorders can be inherited (hemophilia, VWD), arise after surgery, or result after being given an anticoagulant
these drugs can block plasminogen activation, heparin, or plasmin
can inject missing clotting factors (factor VIII or IX)
vit K can also be given
define anemia
below-normal plasma hemoglobin conc from decr red blood cells or an abnormally low total hemoglobin content per unit of blood volume
anemia causes
chronic blood loss, bone marrow abnormalities, endocrine deficiencies, renal failure
nutritional anemias are caused by deficiencies of iron, folic acid, and vitamin B12
anemia treatment
can be temporarily reversed by transfusion
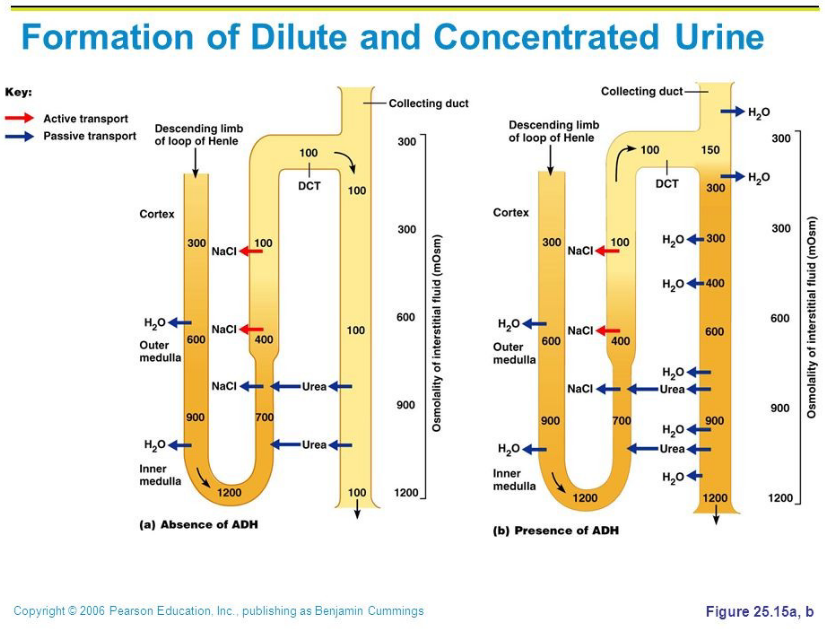
diuretics overview (3)
drugs that incr urine.
block renal ion transporters that block reabsorption of sodium so sodium and other ions enter the urine in greater than normal amounts → water diffuses in to maintain osmosis
can also change urine pH
normal regulation of fluid and electrolytes by the kidneys — list regions (4)
proximal convoluted tubule
descending loop of henle
ascending loop of henle
distal convoluted tubule
normal regulation of fluid and electrolytes by the kidneys —proximal convoluted tubule
almost all reabsorption occurs here (all glucose and amino acids, most bicarbonate, Na, Cl, K, water)
water follows passively from lumen to blood
if water and solutes didn’t get reabsorbed, we would become extremely dehydrated
acid and base secretory system: this system is saturable and diuretic drugs compete with endogenous organic acids. can see an incr in a build up of uric acid (gout)
normal regulation of fluid and electrolytes by the kidneys — desc loop of henle (2)
the remaining filtrate (isotonic) enters the desc loop of henle
osmolarity incr (conc of solutes). the water is being reabsorbed
normal regulation of fluid and electrolytes by the kidneys — asc loop of henle (3)
the cells here are relatively impermeable to water → keeps water in the tubule
active reabsorption of Na, K, Cl
diluting portion of the nephron
normal regulation of fluid and electrolytes by the kidneys — distal convoluted tubule
cells here are also impermeable to water
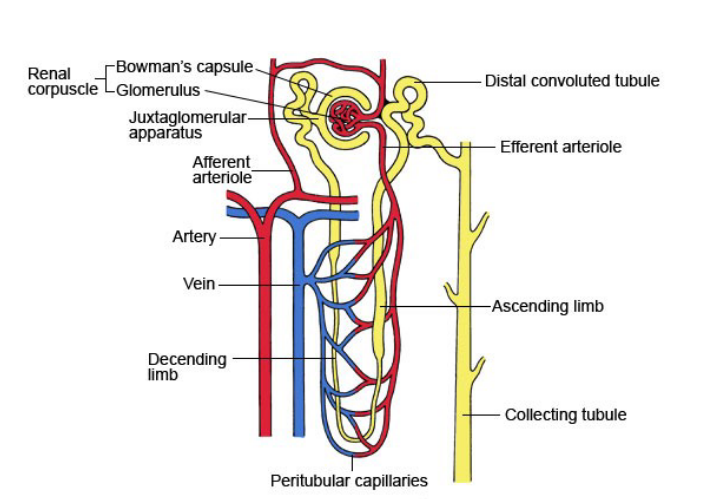
image on other side too
edema (2)
in many diseases, the amt of sodium and chloride reabsorbed by the kidney tubules is high
leads to retention of water, incr in blood volume, expansion of extravascular fluid compartment → results in edema of tissues
causes of edema (6)
HF: diseased heart can’t incr output and the incr vascular volume results in edema
hepatic ascites: incr portal bp. blood flow is often obstructed by cirrhosis (scarring). fluid escapes the vasculature and collects in abdomen
secondary hyperaldosteronism: fluid retention is also promoted by elevated levels of aldosterone → incr Na and water reabsorption. incr vascular volume
nephrotic syndrome: when glomerular membranes are damaged by disease, they allow proteins to enter the filtrate. loss of protein from plasma reduces colloidal osmotic pressure, so water leaks from capillaries back into tissues → edema. retention of sodium will also lead to edema
premenstrual edema: result in imbalance in hormones, i.e. estrogen excess. facilitates loss of fluid to extracellular space
abnormal lymphatic drainage
nonedematous states: list 3
hypertension, hypercalcemia, diabetes insipidus
nonedematous states: hypertension
thiazide reduces blood volume and dilate arterioles
nonedematous states: hypercalcemia (2)
a serious condition that req fast response
loop diuretics are usually employed since they promote calcium excretion
nonedematous states: diabetes inspidius (2)
patients w this condition suffer from high amounts of urine being excreted (poluria) and excessive thirst (polydipsia).
they respond to thiazide diuretics — thiazide reduces blood volume, causing a drop in glomerular filtration rate (GFR) and promoting reabsorption of Na and water
thiazides and related agents overview (3)
most widely used diuretics
all thiazides affect the DCT
all have equal maximum diuretic effects. differ in potency
thiazides and related agents: actions (4)
decr reabsorption of Na (incr excretion) — causes excretion of very hyperosmolar urine → this is unique to this class: others are unlikely to produce hyperosmolar urine
loss of K — bc the Na is being kept in the tubule, the body tries to get more Na out into the cells by exchanging it for K, depleting K in the tissues. potassium levels must be measured often
decr urinary calcium excretion — promote reabsorption of Ca. this contrasts w loop diuretics that keep Ca in the urine
reduced peripheral vascular resistance — decr in blood volume results in decr bp and therefore decr cardiac output
thiazides — therapeutic uses (4)
hypertension — may have been the mainstay for a long time in treating hypertension bc inexpensive, convenient, well tolerated. many patients can take thiazides for years without need for other meds
HF — diuretic of choice for HF. if thiazides fail, loop diuretics may be useful
hypercalciuria — bc they inhibit urinary Ca2+ these drugs are useful for treating hypercalciuria
diabetes insipidus (nephrogenic form) — the amt of urine can be decr from 11 L/day to about 3L/day
thiazides: pharmacokinetics (3)
effective orally
take 1-3 weeks to produce stable reduction in bp
prolonged half life (40 hrs)
thiazides: adverse effects (8)
K depletion, hyponatremia, hyperuricemia, volume depletion (causing hypotension), hypercalcemia, hyperglycemia, hyperlipidemia, hypersensitivity (esp to those allergic to sulfa drugs)
loop or high-ceiling diuretics — bumetanide, furosemide, torsemide: mechanism of action (2)
inhibit cotransport of Na/K/Cl in the asc loop of henle → reabsorption of these ions is decr
most efficacious of the diuretics
bumetanide, furosemifde, torsemide: actions (2)
act quickly even in patients who have poor renal function or do not respond to thiazides
incr Ca2+ content of urine
bumetanide, furosemifde, torsemide: therapeutic uses (3)
drug of choice for reducing acute pulmonary edema of HF
used in emergency situations
treat hypercalcemia
bumetanide, furosemifde, torsemide: pharmacokinetics (3)
admin orally or parenterally
duration of action 2-4 hrs
secretion in urine
bumetanide, furosemifde, torsemide: adverse effects (5)
ototoxicity (damage to ear) (w furosemide being highest risk)
hyperuricemia (high uric acid)
acute hypovolemia
potassium depletion
hypomagnesemia (particularly in elderly)
potassium-sparing diuretics: overview (3)
act on the DCT and collecting duct to inhibit Na reabsorption and K excretion
major use of these is in the treatment of hypertension. used in conjunction w a thiazide
patients on these drugs need to be monitored closely for potassium levels (can get too high)
potassium-sparing diruetics — aldosterone antagonists (spironolactone and eplerenone): mechanism of action
these antagonize aldosterone @ receptor sites.
the complex can’t be internalized and bind to DNA.
normally, the aldosterone/receptor would turn on genes made in response to aldosterone → these proteins would stimulate the Na/K exchange sites of the collecting tubule
potassium-sparing diruetics — aldosterone antagonists (spironolactone and eplerenone): actions (1) and therapeutic uses (2)
in most edematous states, aldosterone levels are high — instrumental in retaining Na
secondary hyperaldosteronism (excessive RAAS); HF
potassium-sparing diruetics — aldosterone antagonists (spironolactone and eplerenone): pharmacokinetics
completely absorbed orally and strongly bound to proteins
potassium-sparing diruetics — aldosterone antagonists (spironolactone and eplerenone): adverse effects (2)
GI upset and peptic ulcers
can cause gynecomastia (large mammary gland in males) and menstrual irregularities → drug should not be given chronically
lipoproteins
make up plasma lipids
spherical macromolecular complexes of lipids and specific proteins (apolipoproteins). the clinically important ones are LDL, VLDL, and HDL
treatment goals aimed at decr LDL — decr risk of CAD; diet and exercise also play a role
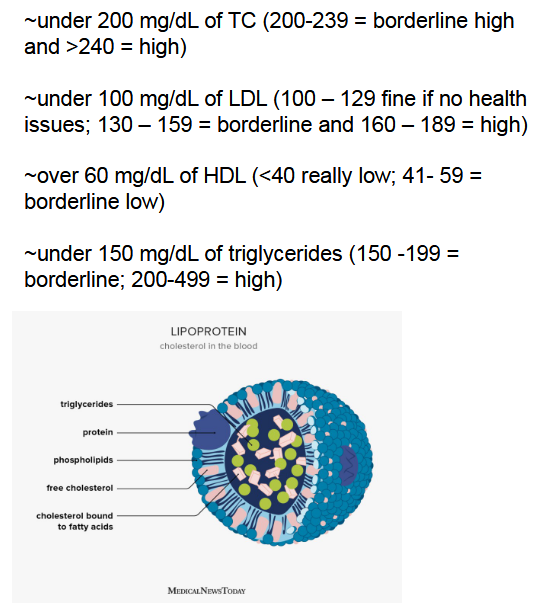
drugs that lower the serum lipoprotien concentration
HMG CoA reductase inhibitors, niacin (nicotinic acid), bile acid-binding resins
HMG CoA reductase inhibitors: overview (2)
known as statins. lower LDL
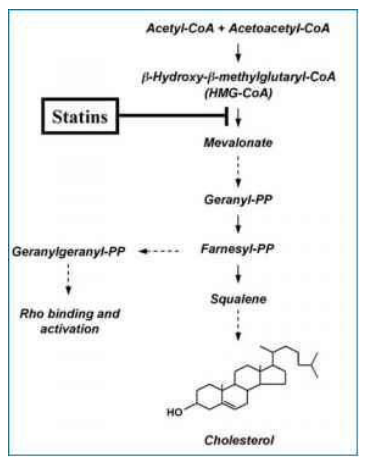
HMG CoA reductase inhibitors: mech of action (3)
competitive inhibitors
these drugs are analogs of HMG-CoA (3-hydroxy-methyl-glutaryl — precursor of cholesterol
they have high affinity for HMG CoA reductase — RDS for cholesterol synthesis