Respiratory Medications
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
66 Terms
Dextromethorphan
Antitussives (i.e., cough suppressant)
Can be a non-opioid by itself or and opioid (i.e., when combined with codeine)
Why is dextromethorphan prescribed?
Treatment of nonproductive cough
How does dextromethorphan work (i.e., MOA)?
Works in the CNS to directly suppress the cough reflex in the medullary cough center, which will also cause drying of mucus membranes
What is special or unique about dextromethorphan?
CI/C:
Pregnancy or breastfeeding
Don’t use if the pt has a head injury or CNS depression (i.e., concussion or sedated) since they work directly on the CNS
Don’t use in children under 4 years old due to the risk of CNS effects (i.e., effects are greater in kids)
In men with BPH, this drug can cause urinary retention (i.e., which can lead to a UTI)
Benign prostatic hyperplasia (i.e., enlarged prostate)
Don’t use in pts with chronic respiratory problems (i.e., asthma and emphysema)
AE:
Over-sedation, drowsiness, confusion, dizziness (i.e., CNS effects)
Drying effect (i.e., nausea, dry mouth, nasal irritation, constipation)
Will need to drink water
Tachycardia, HTN, and restlessness
DI:
Codeine and hydrocodone are opiates, so abuse potential exists along with rest of side effects
Avoid ETOH (i.e., increases the effects)
MAOIs can cause hypotension, fever, and coma
What must you tell a pt taking dextromethorphan?
Don’t mix with alcohol (i.e., CNS directionality)
Do not drive or operate heavy machinery while on medication
Oxymetazoline
Topical nasal decongestant/sympathomimetic
Why is oxymetazoline prescribed?
Treatment of nasal/sinus congestion due to overproduction of mucus secretions (i.e., rhinitis, sinusitis, and/or otitis)
How does oxymetazoline work (i.e., MOA)?
Causes vasoconstriction (i.e., activation of the SNS receptors) in the nasal passages and sinuses, shrinking swollen mucous membranes and opening clogged passages
Works within minutes (i.e., fast)
What is special or unique about oxymetazoline?
CI:
Must check nares to make sure no lesions or erosions exist before administering
Mimics sympathetic nervous activity, so the pt might experience increased HR, BP, RR, and agitation
So, caution when underlying conditions are related to this activity (i.e., HTN, anxiety, arrhythmia, insomnia etc.,)
AE: nose bleeds, irritation of the membranes, and erosions (i.e., it takes a long time)
DI: cannot give it with cyclopropane or halothane (i.e., both anesthesia gasses), because it has major CV effects
What must you tell a pt taking oxymetazoline?
Proper technique needed to deliver medication (i.e., sit upright, hold down the opposite nostril when spraying the medication, etc.,)
May be aerosol (so shake well) or spray
Should only use for 3-5 days before risking rebound congestion (i.e., rebound vasodilation called rhinitis medicamentosa)
Pseudoephedrine
Oral decongestant/sympathomimetic
Why is pseudoephedrine prescribed?
Treatment of nasal/sinus congestion due to overproduction of mucus secretions (i.e., rhinitis, sinusitis, and/or otitis)
How does pseudoephedrine work (i.e., MOA)?
Mimics the SNS (i.e., sympathomimetic): causing vasoconstriction (i.e., activating the SNS receptors) in the nasal passages and sinuses, shrinking swollen mucous membranes and opening clogged passages
What is special or unique about pseudoephedrine?
AE: HTN, anxiety, insomnia, and arrhythmias
Caution:
With conditions that “don’t play well” with the SNS (i.e., glaucoma, HTN, diabetes, thyroid disease, prostate problems, and coronary artery disease)
In pregnancy because it’s not really studied, so it’s risk vs reward
Includes breastfeeding bc it can dry up milk
This is a systemic medicine (i.e., whole body is affected), so the SNS effects are more likely and more annoying
Tremor, anxiety, agitation, pallor, sweating, and racing heart
What must you tell a pt who is taking pseudoephedrine?
They should only use it for up to 7 days before risking rebound congestion (i.e., rebound vasodilation called rhinitis medicamentosa)
Not for chronic rhinitis
Fluticasone (i.e., flonase)
Topical nasal steroid
Why is fluticasone prescribed?
Treatment of nasal/sinus congestion due to overproduction of mucus secretions (i.e., rhinitis, sinusitis, and/or otitis), when other decongestants do not work or if the condition is chronic
How does fluticasone work (i.e., MOA)?
Not sure, but the steroids have an anti-inflammatory effect
Therapeutic effect is not immediate and may take up to 2-3 weeks to develop
What’s special or unique about fluticasone?
There are very few AE
We like this medicine because it has very few systemic effects compared to oral steroids or antihistamines
Over-drying of the mucosa
Headaches
Great for pregnant/lactating women
More effective than oral antihistamines for nasal and eye allergy symptoms
What must you tell a pt taking fluticasone?
Proper administration (i.e., spray out towards nasal mucosa, not directly up nose)
Must use consistently to be effective and must have patience since effectiveness is delayed
May cause local burning, irritation, stinging, and headaches
Steroids lower immune response, so don’t give in the presence of an acute infection and avoid airborne infections (i.e., chicken pox, measles, and TB)
May put you at risk for infection (i.e., cold, flu, etc.,) so make sure to wash your hands and avoid sick people
Notify provider if signs of infection occur
Client can take non-NSAID analgesics like Tylenol if they experience headaches
Guaifenesin (i.e., mucinex)
Expectorant
Why is guaifenesin prescribed?
To help cough up thickened secretions in the respiratory tract r/t bronchitis, pneumonia, etc.,
How does guaifenesin work (i.e., MOA)?
Thins out lower respiratory tract secretions by reducing surface tension, making it easier to have a productive cough and clear airways
The increase in the production of respiratory secretions also decreases the viscosity of mucous
What is special or unique about guaifenesin?
CI with clients who have diabetes (i.e., because the drug has a large sugar content)
AE include GI symptoms: n/v and loss of appetite (i.e., anorexia)
What must you tell a pt taking guaifenesin?
The origin of the cough/thickened secretions need to be found as this med may mask symptoms
Do not use longer than one week
Increase fluid intake to help expectorant liquify secretions
This is the only expectorant on the market, so it shows up in many combination OTC meds to treat cold and flu symptoms
Make sure to check what is in each OTC med, so you don’t take excessive doses
Acetylcysteine
Mucolytic
Why is acetylcysteine prescribed?
Increase or liquefy respiratory secretions to aid the clearing of the airways in high-risk respiratory patients who are coughing up thick, tenacious secretions
Patients may be suffering from conditions such as chronic obstructive pulmonary disease (COPD), cystic fibrosis, pneumonia, or tuberculosis
Also used to treat Tylenol overdose
How does acetylcysteine work (i.e., MOA)?
Liquifies lower respiratory tract secretions (i.e., breaks up the protein bonds in the mucous), making it easier to have a productive cough and clear airways
What is special or unique about acetylcysteine?
AE: GI upset, rash, bronchospasm (i.e., because it is inhaled), and rotten egg smell that can induce nausea
Caution:
With acute bronchospasm, peptic ulcers, esophageal varices, or active bleeding in the GI system (i.e., could make these things worse)
No data on pregnancy/lactation so caution
For high-risk respiratory patients, this medication is administered with a nebulizer (i.e., inhaled aerosol)
Monitor respiratory status frequently (i.e., auscultation of lungs)
What must you tell a pt who is taking acetylcysteine?
Encourage them to cough up secretions instead of swallowing them
Have suction equipment available and help the client suction as needed
Diphenhydramine (i.e., benadryl)
Antihistamines: 1st generation
Why is diphenhydramine prescribed?
Seasonal allergies, acute allergy attacks, narrowed airways due to an allergic response, runny nose (i.e., rhinorrhea), and urticaria (i.e., hives)
How does diphenhydramine work (i.e., MOA)?
Selectively blocks histamine receptor sites to blunt the allergic response (i.e., runny nose, watery eyes, sneezing, itchy skin, itchy ears, and anaphylaxis)
Also has anticholinergic properties (i.e., drying things up)
What’s special or unique about diphenhydramine?
CI/C:
Can’t give to children under 2 because of the CNS effects
Can’t give to anyone with narrow angle glaucoma because it may cause sudden increase in intraocular pressure (which is already high)
Caution if patients have renal or liver problems, and closely monitor (i.e., BUN, creatinine, AST, and ALT)
Don’t use with pregnancy or lactation unless benefits outweigh risk
May cause QT elongation, so it cannot be used with anyone who has had an episode of prolonged QT interval (i.e., a problem with the electrical impulse in the heart which can lead to an acute MI/deadly arrhythmia)
AE: major sedation, balance problems, confusion, urinary retention, and constipation (i.e., not the best drug for the elderly, or those at risk for falls)
DI: watch out for those combination meds to make sure you don’t accidentally take too much
What must you tell a pt who is taking diphenhydramine?
Do not mix with alcohol because it may cause life threatening CNS depression
Will likely cause sedation and urinary retention as a normal side effect, so the pt must know how they will react before doing activities
Will dry out skin, so encourage the pt to drink 8 glasses of water if not on fluid restriction
Water also helps to thin secretions
Have the pt take fiber for constipation (i.e., increase fiber in their diet) or use laxatives
Cetirizine (i.e., zyrtec)
Antihistamines: 2nd generation
Why is cetirizine prescribed?
Seasonal allergies, runny nose (i.e., rhinorrhea), and chronic idiopathic urticaria (i.e., hives)
How does cetirizine work (i.e., MOA)?
Selectively blocks histamine receptor sites to blunt the allergic response (i.e., runny nose, watery eyes, sneezing, itchy skin, itchy ears, and anaphylaxis)
What’s special or unique about cetirizine?
CI/C:
Don’t give to infants under 6 months
Caution in breastfeeding women (i.e., dry milk supply)
Caution in pts with renal (i.e., lower back pain, dark urine, etc.,) or liver (i.e., jaundice, ascites, bleeding, leaking, etc.,) problems and closely monitor
AE: over drying, sedation, confusion, and urinary retention
2nd generation antihistamines are non-sedating, and thus a better option for elderly and those at risk for falls
But, cetirizine can still be moderately sedating
DI:
Theophylline can reduce clearance leading to increased risk of toxicity
Caution with CNS depressants
Watch out for those combination meds to make sure you don’t accidentally take too much
What must you tell a pt taking cetirizine?
Drink 8 glasses of water
Theophylline
Methylxanthines
Bronchodilator
How does theophylline work (i.e., MOA)
Relaxes smooth muscles of the bronchi, resulting in bronchodilation
What’s special or unique about theophylline?
CI/C:
Caution with a history of GI, coronary, respiratory, renal, or hepatic disease
Caution with alcoholism and hyperthyroidism
There are no studies on the effects of xanthines in pregnancy, but has been associated with fetal abnormalities and breathing problems
The AE’s are associated with the level of theophylline in the blood (i.e., it has a narrow therapeutic range from 10 to 20 mcg/dl): restlessness, insomnia, GI upset, n/v, irritability, tachycardia, seizures, brain damage, and death
DI: there are lots of drug interactions, so the client will need to notify the physician if they take any additional OTC or prescription meds
What do you need to tell a pt who is taking theophylline?
Take with food (i.e., its a pill)
Avoid other stimulants (i.e., caffeine)
Drug-drug interactions
If they smoke, the dose will need to be increased
Albuterol
Beta₂ adrenergic agonists
Short-acting beta₂ agonists (i.e., SABA)
Bronchodilator
Inhaler
Is used in emergent situations to open the airway
How does albuterol work (i.e., MOA)?
Mimic the effects of the SNS, relaxing smooth muscle and dilating the bronchi (i.e., decreasing wheezing and helping the airways stay open)
What’s special or unique about albuterol?
CI/C:
Depend on the severity of the underlying condition including valvular disease, vascular disease, arrhythmias, diabetes, and hyperthyroidism
Need to be monitored closely because of increase in SNS stimulation
Used in pregnancy and lactation only if the benefits to the mother outweigh the risks to the fetus
AE’s are attributed to sympathomimetic stimulation (i.e., increased BP, tachycardia, decreased renal and GI blood flow, sweating, pallor, flushing, and tremors), increased blood glucose, and hypokalemia
DI: avoid the use of other stimulants, especially if the pt finds the adverse effects of the medication uncomfortable
What must you tell a pt taking albuterol?
Proper delivery of inhaled medication
Avoid caffeine
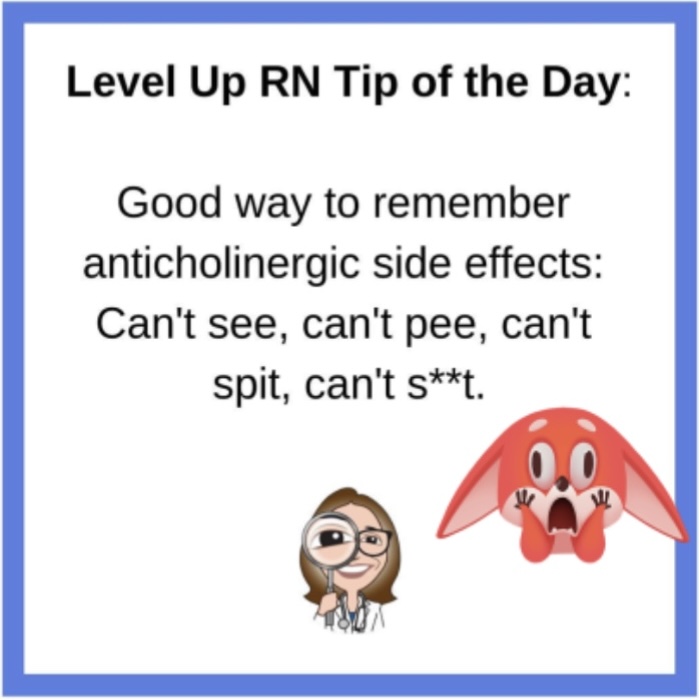
Ipratropium
Anticholinergic
Bronchodilator
How does ipratropium work (i.e., MOA)?
Inhibits the action of acetylcholine at vagal-mediated receptor sites, relaxing smooth muscle leading to bronchodilation
What’s special or unique about ipratropium?
Caution in any condition that could be aggravated by anticholinergic effects (i.e., narrow angle glaucoma, bladder neck obstruction, or prostate hypertrophy)
AE: dizziness, HA, fatigue, nervousness, dry mouth, sore throat, palpitations, and urinary retention
DI: don’t combine with any other anticholinergics
What do you need to tell a pt taking ipratropium?
There are fewer systemic effects than SABA’s but it is not as effective, so do not use in acute asthma exacerbation as a rescue drug
Beclomethasone
Inhaled steroid
Drug that affects inflammation
How does beclomethasone work (i.e., MOA)?
Suppress inflammation (i.e., prevent the release of leukotrienes, prostaglandins, and histamine)
Decreases infiltration of inflammatory cells (i.e., eosinophils and leukocytes)
Decreases edema of airways
Used for long-term management of asthma or COPD
What’s special or unique about beclomethasone?
CI/C:
These medications should not ever be used for the treatment of an acute asthma attack or status asthmaticus
Use with caution in active respiratory infection
AE: due to the route of administration: sore throat, hoarseness, coughing, dry mouth, and pharyngeal/laryngeal fungal infections
Example: oral thrush (i.e., use spacer to decrease drug contact with mouth and oral pharynx)
Inhaled steroids are beneficial because they have fewer systemic effects than oral steroids
What must you tell a pt who is taking beclomethasone?
Contact the MD if there are s/s of respiratory infection
May take 2-3 weeks to reach effective levels
To prevent thrush, the patient needs to wash out mouth well after use
Prednisone
Oral steroid
Drug that affects inflammation
How does prednisone work (i.e., MOA)?
Suppress inflammation (i.e., prevent the release of leukotrienes, prostaglandins, and histamine)
Decreases infiltration of inflammatory cells (i.e., eosinophils and leukocytes)
Decreases edema of airways
What’s special or unique about prednisone?
CI: peptic ulcer disease, diabetes, HTN, renal dysfunction, regular NSAID use, or if the client has systemic fungal infection/recently received a live virus vaccine
AE: suppression of adrenal function, muscle wasting/bone demineralization, hyperglycemia, peptic ulcer disease, immunosuppression (i.e., will have increased risk for infection if on long term therapy), hypernatremia, and hypokalemia
Monitor plasma drug levels to determine the amount of adrenal function suppression
DI:
Furosemide increases the risk of hypokalemia
NSAIDS increase the risk of GIB
Insulin and oral hypoglycemics effectiveness is reduced while on steroids
What must you tell a pt taking prednisone?
Observe for signs of infection that may not include fever or inflammation because these body responses are suppressed by steroids (i.e., sore throat, fatigue, tachycardia, wound discharge etc.,)
Notify provider immediately
For long term use (i.e., 10 or more days), the dose will need to be tapered due to potential for adrenal crisis
Increase intake of calcium and vitamin D to prevent osteoporosis
Report symptoms of hyperglycemia (i.e., polyuria, polyphagia, polydipsia) and monitor blood glucose
Report weight gain, edema, or generalized weakness because it may indicate electrolyte imbalance
Take protective gastric measures to prevent ulcers (i.e., take PPI, avoid NSAIDs, etc.,)
Montelukast
Leukotriene receptor antagonist
Drug that affects inflammation
How does montelukast work (i.e., MOA)?
Either blocks or antagonizes the receptors for the production of leukotrienes D4 and E4, which are components of asthma
What’s special or unique about montelukast?
CI/C:
Caution in pts with hepatic or renal impairment
Fetal toxicity has been reported in animal studies, so use in pregnancy and lactation should benefit the mother more than it risks the fetus
Are not to be used for an emergency asthma attack, this is a maintenance drug (i.e., its a pill)
AE: HA, dizziness, n, diarrhea, abd pain, elevated liver enzymes (i.e., P-450 system), and with zafirlukast, neuropsychiatric symptoms and suicidal ideation
DI:
Phenobarbital, rifampin, and phenytoin may warrant higher doses of montelukast
Zafirlukast can increase levels of warfarin which could cause bleeding
Cromolyn
Mast cell stabilizer
Drug that affects inflammation
How does cromolyn work (i.e., MOA)?
Suppresses inflammation, but does not cause bronchodilation
Effects are less than steroids, so not the preferred drug for asthma but can be useful if there are issues tolerating steroids
Therapeutic use: prophylaxis in mild persistent asthma, exercise induced bronchospasm (EIB), and intranasal can relieve allergic rhinitis
What must you tell a pt taking cromolyn?
Used for prevention of asthma exacerbation
Not to be used for emergent situations
May take several weeks to see therapeutic effects