30 - anorectal and pelvic floor disorders
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
what are haemorrhoids
enlarges anal cushions
- no clear cause
- common in pregnancy, obesity and increased age
bleeding, painless, straining
management/treatment of haemorrhoids
treat underlying causes e.g. constipation
topical treatment - anusol, lidocaine cream, ointments
haemorrhoidal artery ligation, rubber band ligation
haemorrhoidectomy
stapled haemorrhoidectomy
what are anal fissures
small tear in lining of anus
symptoms of anal fissures
sharp pain on defaecation (due to passing hard faeces)
bleeding
treatment of anal fissures
treat underlying cause
GTN ointment/dlitiazem + lignocaine
surgical - botox, sphincterectomy
what is a perianal abscess
type of anorectal abscess that occurs in perianal space
symptoms of perianal abscess
excruciating pain
signs of sepsis
risk factors for perianal abscess
diabetes
BMI high
immunosuppression
trauma
treatment of perianal abscess
antibiotics if septic
incision and drainage
do not go looking for fistulas - causes pain
symptoms of anorectal fistula
pus discharge
faecal soiling
treatment of anorectal fistula
surgery is really only option but only success in 50%
what is pelvic floor disturbance
collection of wide spectrum of symptoms related to defaecation
aetiology of pelvic floor disturbance
childbirth
surgery
abuse
perianal sepsis
what is chronic constipation
difficult or reduced frequency of defaecation
types of chronic constipation
organic
drug related
dietary
functional
- slow transit
- evacuation related - blockage?
what drugs cause constipation
iron - most common side effect
anti-muscarinics
TCA's
anti-epileptics such as carbamazepine, gabapentin, pregabalin
anti-psychotics
antispasmodics
diuretics
opioids
verapamil
assessment of chronic constipation
exclude sinister cause
- colonoscopy
- CT colon
- exclude anaemia
- qFIT
- IgG for coeliac
- faecal calprotectin
detailed history to establish type
colonic transit studies
treatment of chronic constipations
1. baseline laxatives - ensure compliance
2. proculopride (women only) if failed with 2 or more regular laxatives from different classes at highest dose for 6 moths and invasive measures considered
- lubiprostone (all adults) same reason
- linaclotide - IBS-C
surgical options for chronic constipation
sigmoid colectomy
subtotal colectomy with end ileostomy
subtotal colectomy with ileorectal anastomosis
trial w/ ileostomy prior to major operative intervention
types of faecal incontinence
passive - internal sphincter defect
urge - rectal pathology, functional
mixed - prolapse
overflow - constipation
how to assess faecal incontinence
detailed history- determine type
obstetric/surgical history
trauma/abuse?
clinical examination
anorectal physiology
endo-anal ultrasound
defector proctogram
PR exam
what does anal manometry measure
anal sphincter function - resting pressure, squeeze increment, duration
estimation of functional length of anal canal
anorectal pressure response during abrupt increase in intra-abdominal pressure
changes in anal pressure during defaecation
recto-anal inhibitory reflex - internal sphincter
what is the best modality for assessing anatomy and dynamic function in anorectal dysfunction
defaecation proctogram
what does a defaecating proctogram provide info on
pelvic floor mobility
pathological function of musculature
changes to form and axis of organs
compensated/decompensated function
internal hernias
management of faecal incontinence
low fibre diet
loperamide
pelvic floor exercises
EMG if required
irrigation
anal plug
surgical intervention of faecal incontinence
sphincter repair
correct anatomical defect
sacral nerve stimulator
anal bulking agent for passive faecal incontinence
name 2 mixed anorectal disorders
rectocoel
internal rectal prolapse
what is rectocoel
passive loss of stool from being trapped due to incomplete evacuation
what is internal rectal prolapse
symptoms of obstructive defaecation and faecal incontinence
management of mixed anorectal disorders
improve rectal evacuation with various techniques
biofeedback
enemas
loperamide
surgical intervention
different types of fistula
submucosal fistula - fistula track passes superficially beneath the submucosa and does not involve any sphincter muscle
inter-sphincteric fistula - track passes through the internal sphincter and continues in the inter-sphincteric plane to the perianal skin, not including the external anal sphincter
trans-sphincteric fistula - track crosses through the internal and external anal sphincter on its exit towards the perianal area
suprasphincteric fistula - fistulous tract passes through the internal sphincter but traverses the external sphincter below the puborectalis muscle
extrasphincteric fistula - fistulous track may pass outside the sphincter complex through the ischiorectal fossa to the perianal skin, very high up, hard to treat
Chronic pelvic pain
found in complex patients with multiple behavioural psychological issues
manage with EUA, pudendal nerve block, regular enemas/suppositories
In any anorectal disorder should you mesh?
NO
if have to biological mesh
rectal prolapse
rectum stretched and sticks out anus
prehabilitation with biofeedback
if fit/active rectopexy
Which colorectal imagine characterises pathologies in rect and anal canal, rules out fistulas, sepsis and mainly used for anal/rectal staging cancer?
MRI rectum
Out of CT colonoscopy and colonoscopy which is better and why?
colonoscopy better because can take biopsy at same time whereas CT colonoscopy can’t
which special functional colorectal imaging is useful in obstetric anal sphincter injuries and in fistula disease
Endoanal USS
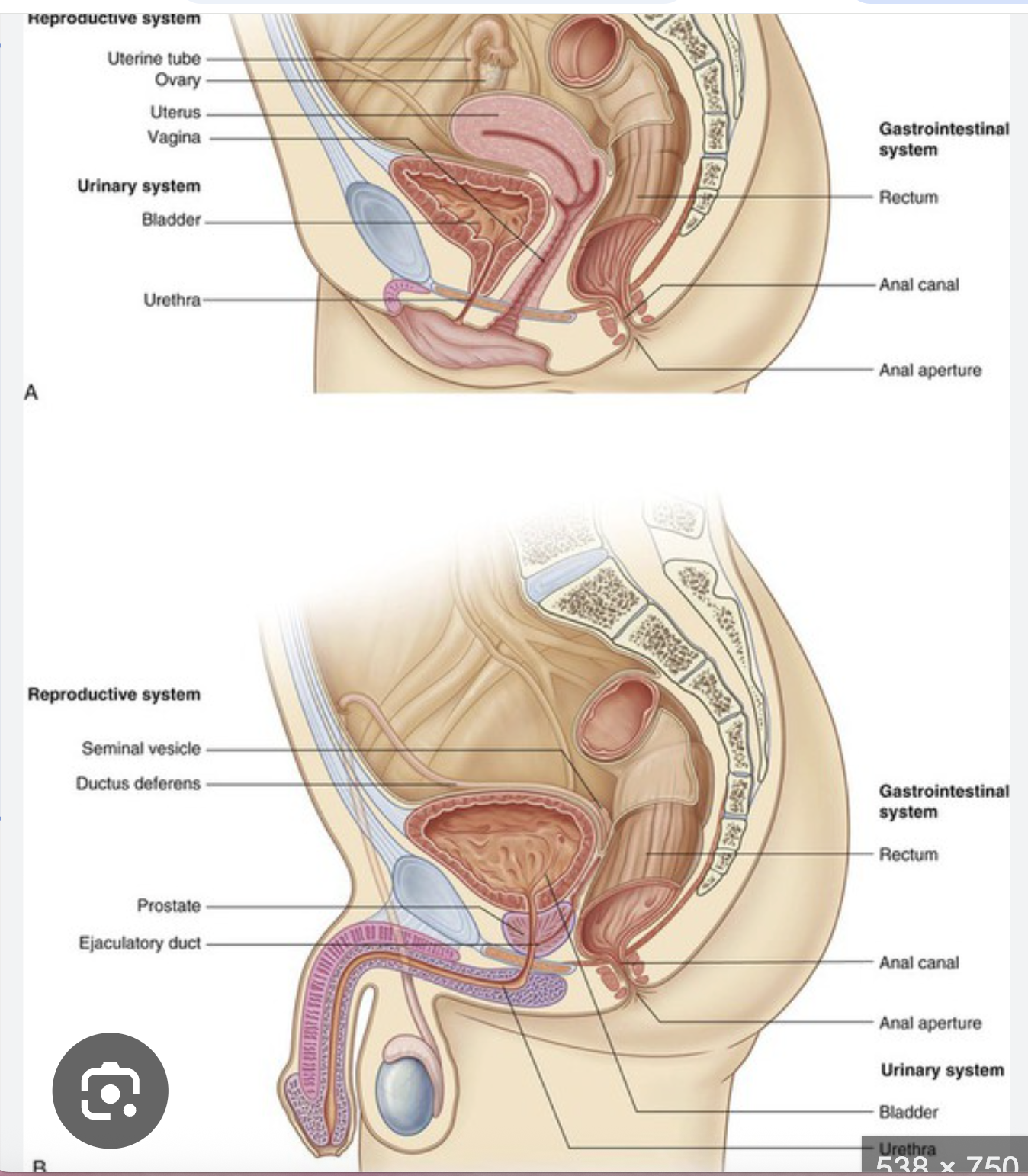
anorectal anatomy & physiology
anorectum -control of defeacation -maintenance of continence
anorectum split into -upper -middle -lower rectum folds
function requires -pelvic floor -rectal compliance -intact pelvic neurology
in lower rectum transition zone from columnar mucosa proximally and squamous mucus distally
rectal cushions present in the zone
difference in male and female anorectal anatomy
female sphincter bulkier than male
anorectal angle not as acute in males as in female
anorectal canal: 4.4cm in men - 4cm