Pediatric Cardiac Disorders
1/33
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
Factors Influencing Cardiovascualar Status
Genetic:
Chromosomal alterations
Environmental:
Pollutants
Maternal:
Toxins, infection, chronic illness, alcohol
Certain medications used to treat chronic conditions, such as antiarrhythmic drugs, anticonvulsants, and antidepressants (e.g., lithium and possibly SSRIs).
Multifactorial:
Most common cause (mixture of all three)
Primary cause of CHD; influenced by genetics and environment.
Types of Developmental and Biologic Variances in Cardiovascular Status
Embryonic:
Occurs during embryonic development.
Childhood:
Occurs during childhood development.
Changes are triggered by the first breath:
Pulmonary Artery Drops:
Closure of the ductus arteriosus
Right Atrium Pressure Drops and Pressure in Left Atrium Increases:
Closure of the foramen ovale
Vasoconstriction:
Closure of the ductus venosus
Cardiac Nursing Assessment: Health History
Patient’s History:
Infections
Chromosomal abnormalities
Prematurity
Autoimmune disease
Medications
Maternal & Fetal History:
Birth history
Maternal use of medications
Radiation exposure
Maternal illness (e.g., coxsackievirus, cytomegalovirus, influenza, mumps, or rubella)
Postnatal History
What happened once that baby was born?
Family History:
Heart disease
Hyperlipidemia
Cardiac: Physical Examination
“Across the Room Assessment”:
Cyanosis
Shortness of breath (SOB)
Difficulty breathing (DIB)
Tachypnea
Clubbing
Eating difficulties
Failure to thrive (FTT)
Activity and general appearance
Edema or jaundice (portal HTN → CHF)
**If a caregiver reports that their infant starts sweating during feeds, either breastfeeding or bottle-feeding, this is a red flag! Think cardiac!**
Palpation:
Apical impulse (AI)
Peripheral pulses (all of them!) and capillary refill time (CRT)—will be prolonged with cardiac issue.
Liver borders—an enlarged liver may indicate right heart failure
Auscultation:
Heart sounds
Rate and rhythm
Compare upper and lower extremity blood pressure (BP).

Cardiac: Making a Diagnosis
Depends on the Symptoms:
Holter monitor—(worn for day, weeks, or months)
Chest X-ray
Electrocardiogram (ECG)
Echocardiogram (ultrasound of the heart)
Arteriogram
Prenatal ultrasound (US)—a fetal cardiologist will evaluate any cardiac concerns during pregnancy
Cardiac catheterization

Cardiac Catherization
Pre-Catheterization Checklist:
Thorough health history and physical exam:
Establish a baseline for post-catheterization.
Obtain baseline vital signs
Note fever or other signs and symptoms of infection
Note allergies
Review medications
Note the NPO status
Review labs
CBC, CMP, PT/PTT/INR
For a right-sided catheterization, the catheter is threaded to the right atrium via a major vein such as the femoral vein.
For left-sided catheterization, the catheter is threaded to the aorta and heart via an artery.
Post-Catheterization Care:
Bedrest (4 to 8 hours) with a straight leg (as much as possible).
Record vital signs frequently.
Pay attention to subtle differences (changes in HR)
Monitor for hypotension and bleeding.
Check insertion site.
Monitor and compare catheterized extremities.
Assess the child’s neurovascular status and level of consciousness.
Monitor for arrhythmias, hypotension, or infection.
Monitor site for hematoma and/or bleeding.
If hematoma or bleeding, position flat and apply direct pressure 2.5 cm (1 in) above the catheter site.
Don’t leave the patient/room → phone a friend → PCP!
Types of Cardiac Disease
Congenital:
Tetralogy of Fallot
Tricuspid Atresia
Atrial Septal Defect (ASD)
Ventricular Septal Defect (VSD)
Atrioventricular (AV) Canal Defect
Patent Ductus Arteriosus (PDA)
Acquired:
Heart Failure
Endocarditis
Rheumatic Fever
Cardiomyopathy
Hypertension (HTN)
Kawasaki Disease
Hyperlipidemia
Transplant

Congenital Heart Disease
Decreased Pulmonary Blood Flow:
Tetralogy of Fallot
Tricuspid Atresia
**Cyanosis
Increased Pulmonary Blood Flow:
Atrial Septal Defect (ASD)
Ventricular Septal Defect (VSD)
AV Canal
Patent Ductus Arteriosus (PDA)
**Heart failure, ventricular hypertrophy, fluid retention, pulmonary hypertension.
**CHF cluster care to reduce time of patient stress
Obstructive:
Coarctation of the Aorta
Aortic Stenosis
Pulmonary Stenosis
**Patient has a condition that “obstructs” or limits blood flow.
Mixed:
Transportation of the great vessels
Total Anomalous Pulmonary Vein Connection
Truncus Arteriosus
Hypoplastic Left Heart Syndrome
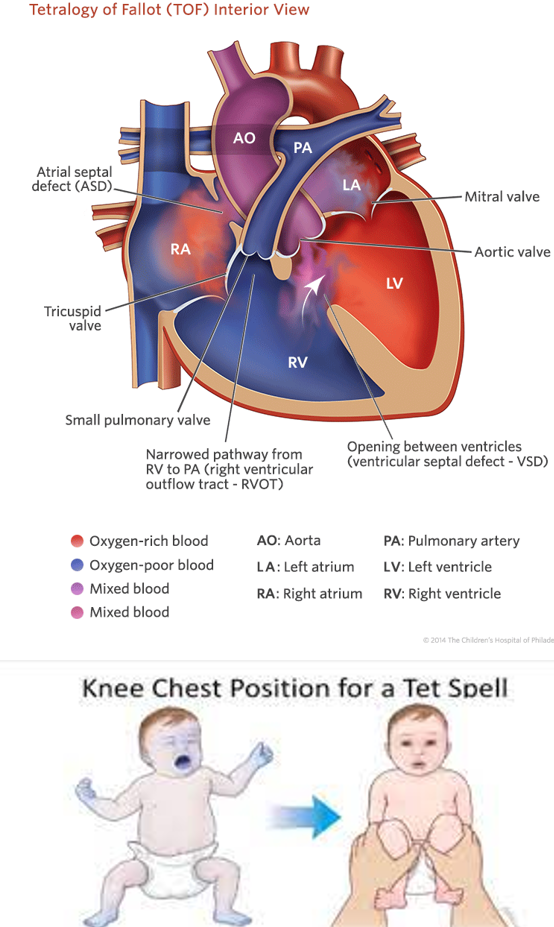
Tetralogy of Fallot
Decreased Pulmonary Blood Flow
4 Defects:
Pulmonary Stenosis (narrowing)
Right Ventricular Hypertrophy—(obstructed blood flow to the lung causes increased right-sided pressure).
Overriding Aorta (goes over the septum)
Ventricular Septal Defect (VSD)
**PROVe = Pulm Stenosis, R Vent Hypertrophy, Overriding Aorta, VSD**
Treatment: Hypercyanotic Spells or “Tet Spells”
Use a calm, comforting approach.
Place in a knee-to-chest position (#1)—it increases peripheral vascular resistance, which reduces right-to-left shunt at the VSD = increased pulmonary blood flow.
Educate parents!
In the Hospital:
Provide supplemental oxygen.
Administer Morphine (IV, IM, or SQ)—helps the child calm, reduces tachypnea, and decreases vascular resistance.
Supply IV Fluids
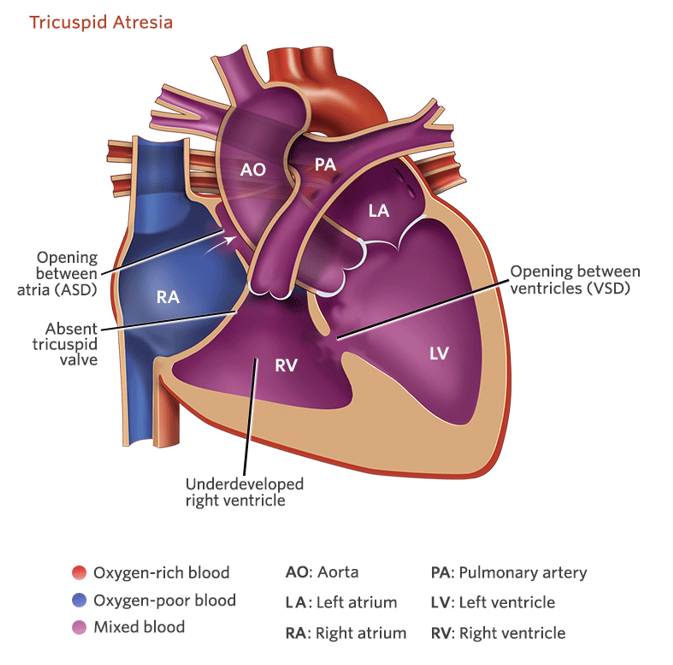
Tricuspid Atresia
Decreased Pulmonary Blood Flow
Tricuspid valve does not develop.
Blood does not go directly into the right ventricle.
Deoxygenated blood passes through a patent foramen ovale (PFO) in the atrial septum.
Blood mixing at the pulmonary artery and aorta.
________________________________________________________
Cyanosis at birth or a few days later.
Rapid respiration and poor feeding.
May have coolness and clamminess to extremities.
**Prostaglandins will be administered to keep the PDA open (connection between the pulmonary artery and the aorta open).
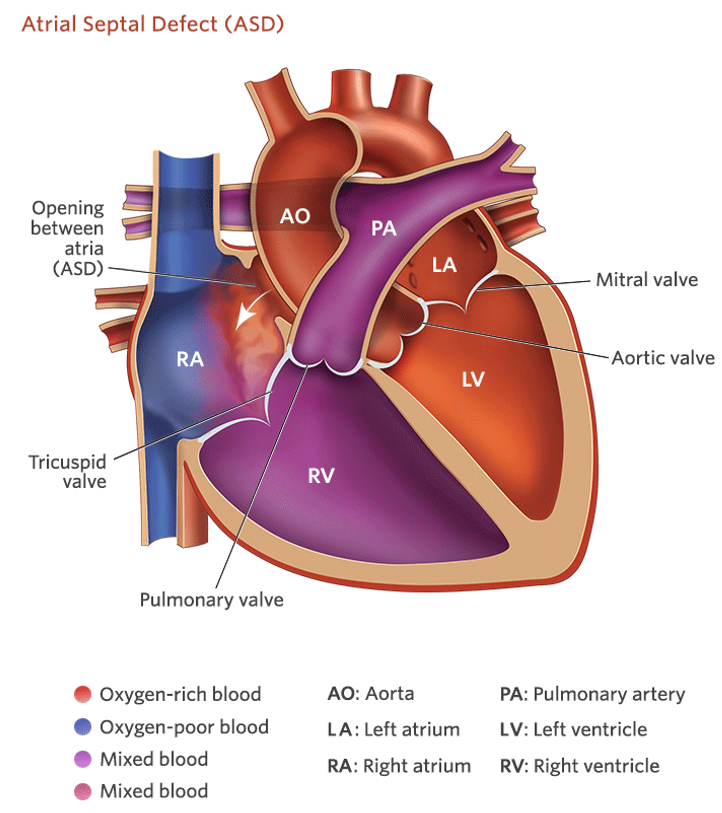
Atrial Septal Defect
Increased Pulmonary Blood Flow
Hole in the wall dividing the left and right atria.
Often asymptomatic.
Unless it is extreme, in which they will develop signs and symptoms of heart failure.
Increased blood flow results in:
Shortness of Breath (SOB)
Fatigue
Failure to Thrive (FTT) over time.
Repairs are usually performed around 2 to 3 years of age.
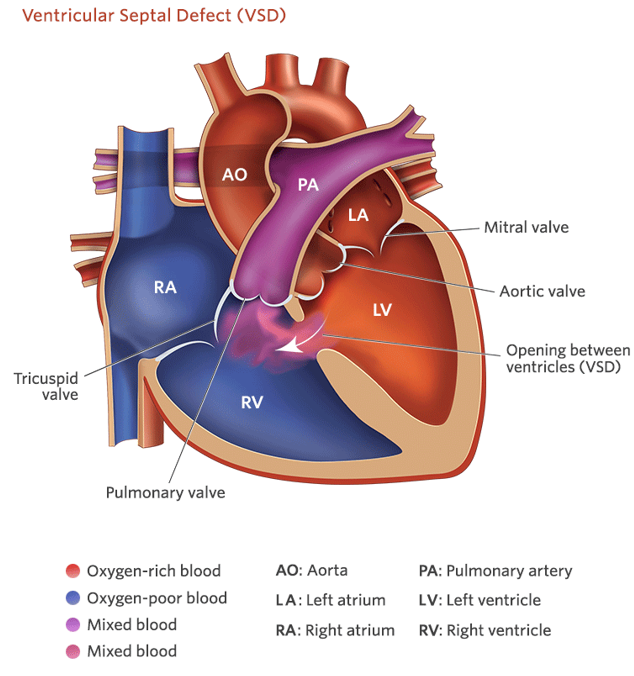
Ventricular Septal Defect
Increased Pulmonary Blood Flow
The most common congenital heart defect!
Hole in the wall between the left and right ventricles.
Asymptomatic if small.
Left to right shunt.
Loud, harsh holosystolic murmur—rapid heartbeat. (can hear without stethoscope)
Increased flow to lungs leading to pulmonary hypertension.
Heart failure if not repaired.
Failure to thrive (FTT).
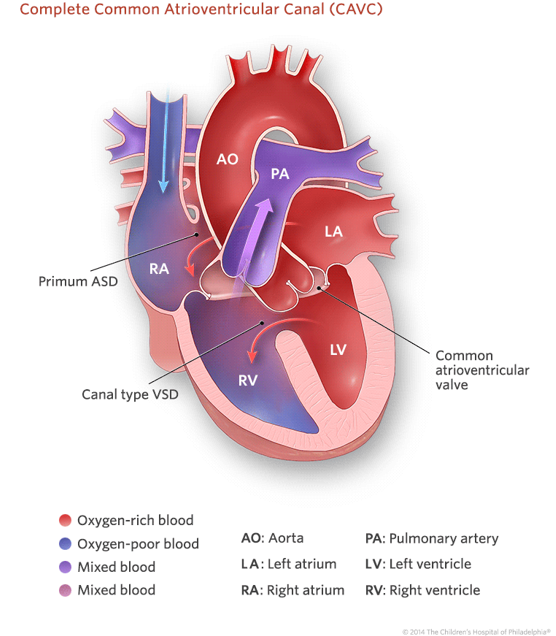
Atrioventricular Canal (AV Canal)
Increased Pulmonary Blood Flow
Failure of endocardial cushions to fuse.
Tricuspid and mitral valves do not get separated.
ASD and VSD are present.
Left to right shunting.
Pulmonary edema.
Often associated with Trisomy 21.
Difficulty breathing, poor weight gain and growth, cyanosis, heart murmur.
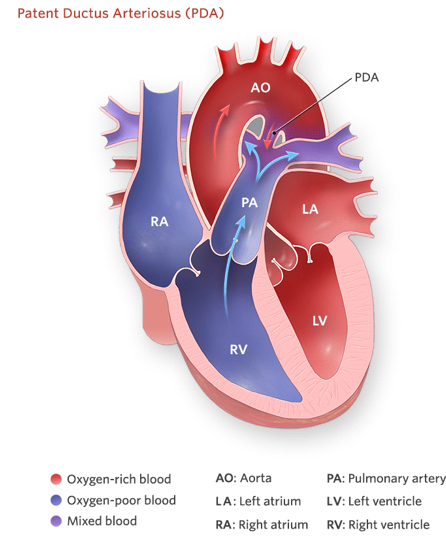
Patent Ductus Arteriosus
Increased Pulmonary Blood Flow
Second most common congenital heart defect!
Persistent connection between the aorta and pulmonary artery.
More common in premature infants and those born in high-altitude areas.
Can occur to accommodate right to left shunting diseases.
If small, may be asymptomatic.
If larger, may exhibit signs of heart failure.
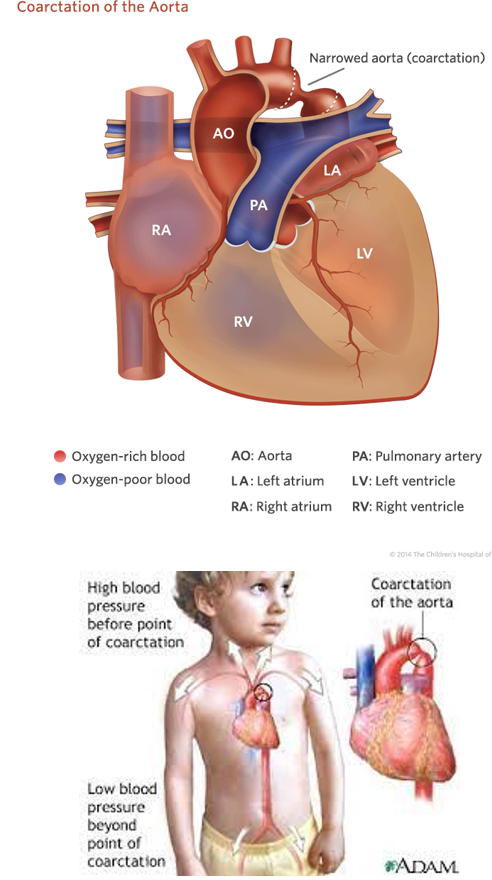
Coarctation of the Aorta (Coarct)
Obstructive Disorder
Narrowing of the aortic lumen.
BP in all 4 extremities:
Upper extremities will be higher than lower.
Heart Failure Symptoms
Care:
Cluster care to minimize stress.
Digoxin administration to help increase cardiac output and perfusion.
Diuretics to reduce edema.
Higher calorie feeds.
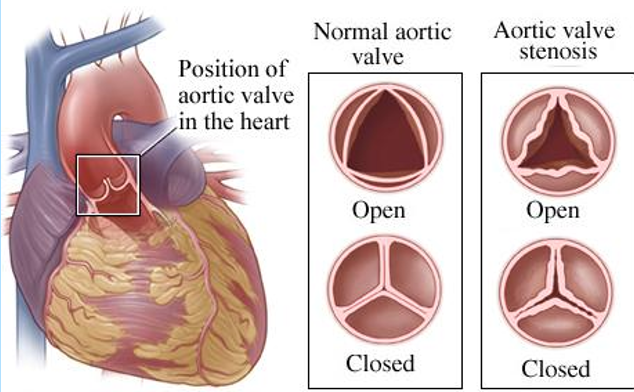
Aortic Stenosis
Obstructive Disorder
Narrowing; Restricted blood flow from the left ventricle to the aorta.
Typically Asymptomatic:
Failure to Thrive (FTT)
Faint pulses
Easy fatigue
Chest pain
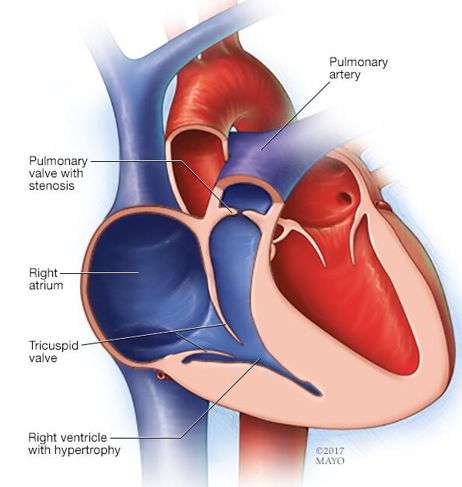
Pulmonary Stenosis
Obstructive Disorder
Narrowing; Restricted blood flow from the right ventricle to the pulmonary artery.
Right ventrical hypertrophy—similar to tetralogy of fallot.
Typically asymptomatic:
Failure to Thrive (FTT)
Faint pulses
Easy fatigue
Chest pain
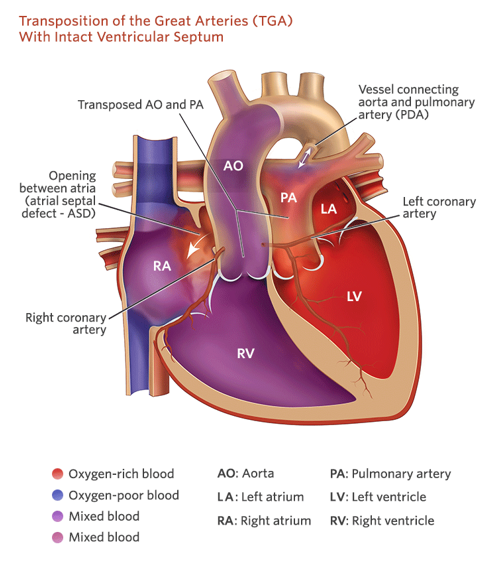
Transposition of the Great Vessels
Mixed Defect
Pulmonary artery and aorta are switched.
May also have ASD or VSD.
Treatment:
Surgical switch*
Balloon atrial septostomy
Prostaglandins (PGE)
****Just to need to know that the great vessels need to be surgically switched****
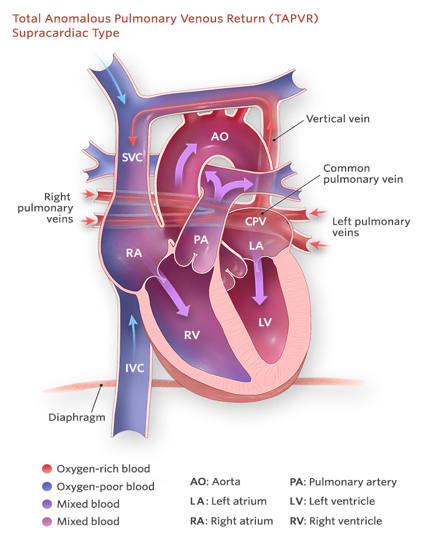
Total Anomalous Pulmonary Vein Connection
Mixed Defect
Pulmonary veins do not connect to the left atrium.
Pulmonary veins connect to the right atrium or superior vena cava.
PFO or ASD is usually present.
Symptoms:
Cyanosis
Fatigue
Poor feeding
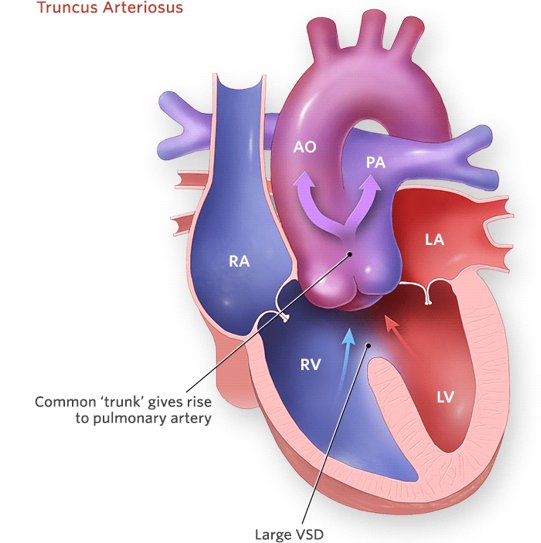
Truncus Arteriosus
Mixed Defect
Single large vessel.
Decreased systemic blood flow.
Requires surgical intervention.
Not compatible with life for long (weeks or months).
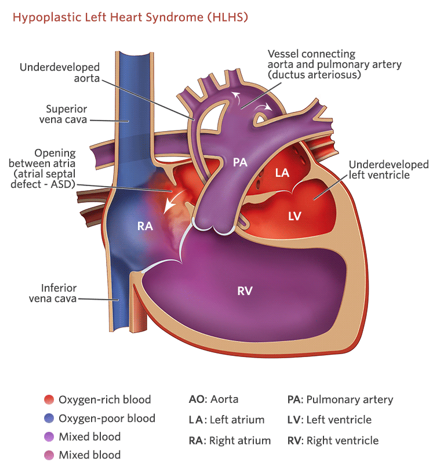
Hypoplastic Left Heart Syndrome
Mixed Defect
Very small left ventricle and a very large right ventricle to compensate.
Often diagnosed prenatally.
Requires several surgeries.
Often leads to transplant.
Congenital Heart Defect: Nursing Management
Medication as prescribed:
Diuretics often prescribed.
Improve Oxygenation:
Frequent assessments.
Semi-Fowlers (child), 45-degree angle (infant).
Use oxygen sparingly (it is a vasodilator—it can decrease BP).
Weigh daily.
Try using the same scale and take it about the same time of day.
Strict I & Os.
Allow for periods of activity and rest.
Cluster care
Adequate Nutrition:
Increased nutritional needs.
Oral with supplements enterally (NGT) as needed.
High-calorie feedings.
Cautious breastfeeding and bottle feeding.
Family Coping/Education.
Infection Prevention.
Acquired Heart Disease: Heart Failure
Most commonly seen in Congenital Heart Disease
Most cases occur by 6 months of age.
Cannot Pump Blood Effectively:
Reduced cardiac output
Hypertrophy
Signs & Symptoms:
Sweating during feeds**
Poor feeding
Increased work of breathing (WOB)/respiratory distress**
Decreased urine output
Poor Cardiac Output:
Low BP
Tachycardia
Gallop heart rhythm
Cool, pale skin**
Fluid Overload:
Edema**
Crackles in lungs**
Nursing Care
Monitor:
Vital signs (V/S), ECG, and cardiac status
Intake & output (I & O), daily weights
Promote Rest:
Cluster care to minimize stress
Provide Adequate Nutrition:
Infant Nutrition:
Feed every 3 hours when rested; hold in a semi-upright position
Allow rest during feedings; gavage feed if unable to consume milk
Increase caloric density of feeds
Encourage breastfeeding mothers to alternate with high-density formula or fortified breast milk

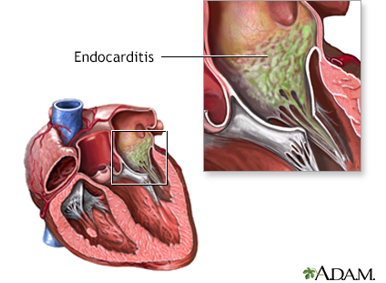
Infective Endocarditis
At-Risk Patients:
Those with CHD, prosthetic valves, and central lines.
Definition:
A microbial infection of the endothelial surfaces of the heart’s chambers, septum, or most commonly, the valves
Causes:
Bacteria or fungi gain access to the endothelium
Infection can spread to other parts of the body
Symptoms:
Vague flu-like symptoms (low-grade fever, pale, etc.)
Fatigue
Anorexia or weight loss
Monitor:
Full Cardiac—ECG leads, HR, RR, Pulse ox, & BP.
Treatment:
IV Antibiotics or antifungals for approximately 4 to 6 weeks.
Acute Rheumatic Fever
Cause:
Delayed sequela of group A streptococcal pharyngitis (strep throat).
Develops 2 to 4 weeks after the initial infection.
Affects joints, CNS, skin, and subcutaneous tissue.
Causes chronic, progressive damage to the heart and valves.
Diagnosis & Lab Tests:
Modified Jones Criteria**
Throat Culture
Detects group A streptococcal pharyngitis (recommended for all school-aged children with sore throats)
ASO Titer (Antistreptolysin O Titer)***
Elevated or rising titer; the most reliable diagnostic test.
Checks for old strep throat
CRP (C-Reactive Protein)
Elevated in response to inflammatory reaction
ESR (Erythrocyte Sedimentation Rate)
Elevated in response to inflammatory reaction
Treatment:
Antibiotics—long time (usually until they are 21 years old)
NSAIDs
Corticosteroids
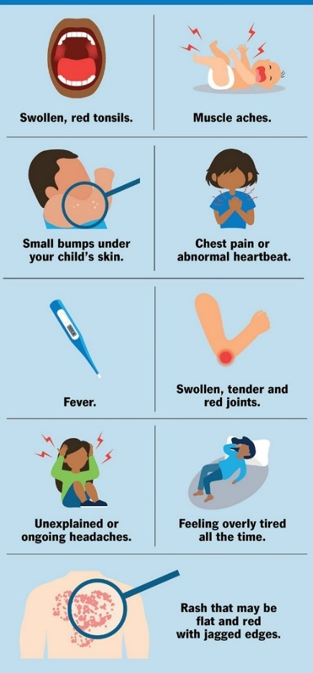
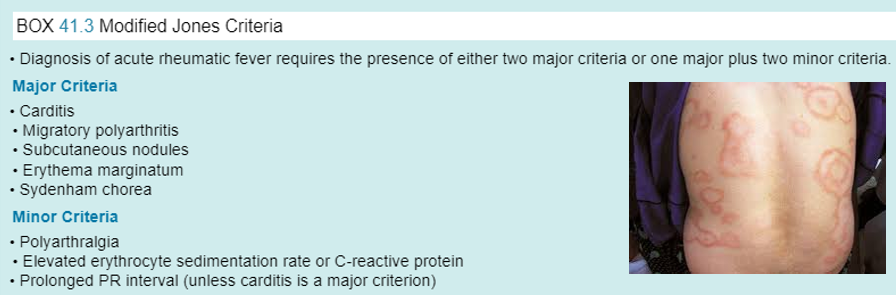
Acute Rheumatic Fever: Modified Jones Criteria
The Diagnosis of Acute Rheumatic Fever requires the presence of either two major criteria or one major plus two minor criteria.
Major Criteria:
Carditis
inflammation of the heart.
Migratory polyarthritis***
multiple joints hurting moving around (not always the same one).
Erythema marginatum**
subcutaneous nodules under the skin (as shown in picture)
Sydenham chorea
CNS features; muscle weakness, falling, trouble speaking, etc.
Minor Criteria:
Polyarthralgia**
multiple areas that hurt (doesn’t necessarily moves around)
Elevated ESR or CRP
Prolonged PR interval (unless carditis is a major criterion)
“Joint pain, chest pain, and a ‘funny rash’ with reported sore throat a month ago…”
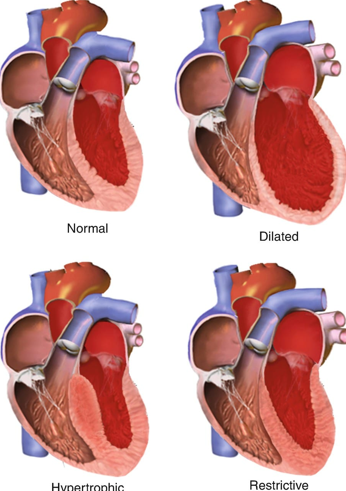
Cardiomyopathy
Myocardium cannot contract properly.
Most cases are idiopathic.
May result in heart failure.
Often requires a heart transplant.
Nursing Management:
Monitor for clots.
Administer vasoactive medications (Beta-blockers, Calcium Channel Blockers, ACE inhibitors).
Provide diuretics.
Administer anticoagulants. (rx for bleeding—medical alert bracelet)
Allow some activity but promote rest.
Hypertension
Increased Prevalence—Primary Hypertension:
Overweight or obesity
≥ 95th percentile for gender, age, and weight
Assessment:
Growth delay
Obesity
Symptoms:
Fatigue
Blurred vision
Headache
Behavioral or vision changes
Treatment:
Weight reduction
Dietary changes
Increased physical activity
Pharmacological treatment
Step-Wise Approach:
Initial Evaluation: If a child has one elevated BP reading and is overweight or obese, start with a urine test to assess renal function. Avoid unnecessary invasive testing initially.
First Intervention: Education on activity and dietary modifications. Schedule a follow-up in 4 weeks to reassess BP.
If No Improvement in 4 Weeks: Perform blood work to evaluate for underlying causes. Consider referral to a nutritionist or lifestyle intervention programs (e.g., weight management camps). Reassess BP after lifestyle modifications.
If BP Remains Elevated Despite Lifestyle Changes: Initiate pharmacological treatment. Continue monitoring and follow-up for treatment efficacy.

[CARDIAC LECTURE] Kawasaki Disease
Acute systemic vasculitis
Unknown etiology
More common in boys than girls
80–90% of cases occur in children <5 years old
Higher prevalence in children of Asian ancestry
Widespread inflammation of medium-sized muscular arteries
Symptoms:
Fever for 5 or more days along with:
Strawberry tongue
Cracked, red lips
Cervical lymphadenopathy (usually on one side)
Redness of palms or soles
Edema of hands or feet
Generalized rash
Bilateral bulbar conjunctival injection (without exudate)—pink eye w/ no drainage
Course & Complications:
Self-limiting, typically resolves in <8 weeks
Potential complications:
Coronary artery abnormalities
Long-term risks: heart failure, myocardial infarction, arrhythmias
Aneurysms
Diagnosis:
Patient must have at least 4 out of 5 criteria from different symptom categories.

[CARDIAC LECTURE] Kawasaki Disease: Nursing Care
Administer IVIG:
Most effective when given within the first 7 to 10 days of illness.
Single infusion over 8 to 12 hours.
Administer Aspirin:
High-dose aspirin until afebrile for 72 hours
Low-dose aspirin for 6 weeks.
**On aspirin because we are worried about aneurysms**
Clinical Monitoring:
**Initial Echocardiogram and then rechecked a couple of times**
Signs & Symptoms to monitor:
Tachycardia
Gallop rhythm
Muffled heart sounds
Arrhythmias (continuous cardiac monitoring recommended)
Comfort Measures:
Control fevers with appropriate medications.
Moisturize lips to prevent dryness.
Hydration: Offer cool liquids and popsicles for comfort.
Caregiver Education:
Monitor fevers at home.
Follow up with PCP and cardiology for ongoing care.
Avoid live vaccines for at least 11 months post-IVIG treatment.

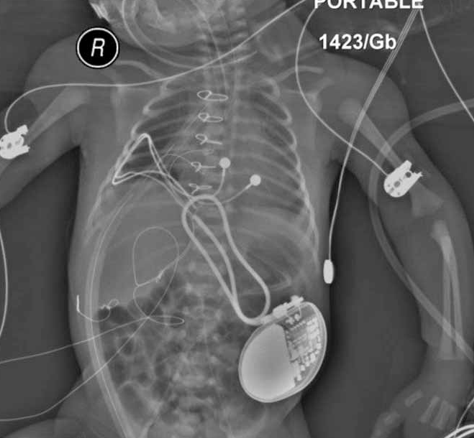
Treatment Options for Cardiac Disease in Children
Interventional catheterization
Cardiac surgery
Pacemakers
Cardiac transplantation
Medical Management Interventions:
Pharmaceutical
Dietary
Activity
Supportive care/community care
Heart Transplant
Over 500 children receive heart transplants per year.
Evaluation of candidacy involves thorough assessment of the child’s overall health and suitability for transplant.
Recovery varies and depends on individual factors, but it typically involves a period of intensive monitoring and care.
Lifelong treatment is necessary, including antirejection medications to prevent organ rejection and ensure the success of the transplant.

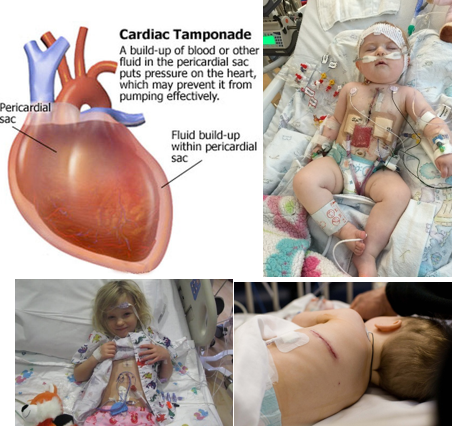
Heart Transplant: Post-Operative Interventions
Maintain cardiac output.
Prevent Cardiac Tamponade:
MEDICAL EMERGENCY:
Hypotension
Muffled heart sounds (beating through water)
Decreased systemic perfusion
Sudden cessation of chest tube drainage (just stops)
Narrowing pulse pressures
Manage temporary pacing wires.
Maintain fluid and electrolyte balance.
Promote respiratory function.
Prevent hemorrhage and arrhythmias.
Monitor neurological functioning.
Prevent infection (incision care).
Manage sedation and pain.
Manage nutrition.
Provide psychosocial support.
Pharmacologic Interventions for Heart Failure
Diuretics: decrease preload
Furosemide (Lasix) and Spironolactone (Aldactone)
Daily weights
Monitor labs and I & Os—low potassium
Encourage the child to eat foods high in potassium (bran cereals, bananas, legumes, leafy vegetables, oranges)
Positive inotropic agents: contractility
Digoxin (Lanoxin)
Hold digoxin for HR < 90 (infants) and < 60 (adolescents)**
Administer at the back of the mouth and give water following (prevents tooth decay).
Do NOT give an extra dose if missed, or readminister if the child vomits.
Observe for digoxin toxicity (decreased HR, appetite, N/V)**
Dopamine, Dobutamine, Epinephrine
Vasodilators:
Nitroglycerin, nitroprusside (Nipride)
Captopril (Capoten), Enalapril (ACE inhibitors)
Monitor BP before and after administration
Monitor for hyperkalemia