L1 - Intro to Pain, Classification and Mechanisms of Pain
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
Definition of Pain
An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage
Impact of Pain
Can affect mood, motivation, & cooperation in relation to treatment
Can affect emotional life, cognition, relationships
Can affect mobility and capacity/energy
Can affect work life and financials
Overall quality of life
Why do we experience pain? (6)
It’s the body’s warning/defence system
Plays a role in mobilisation of escape and avoidance behaviors - and is linked to motor systems (Wall 1999)
Triggers mental and physical behaviour to end the physical experience and prevent injury
Promotes learning (repetition of harmful behavior less likely)
Encourages us to disengage from noxious stimulus
Promotes healing process
4 ways to classify pain
Duration
Dimensions of pain experience
Area of pain distribution
Pain mechaninsm
Two ways to classify pain duration
Acute pain vs Chronic/persistent pain
Acute Pain
Occurs directly as a result of tissue damage or potential tissue damage, and is a symptom.
Lasts less than 3 months
Acute pain serves to protect from tissue damage, and if tissue damage occurs, it serves to allow for time to heal
Response to Acute Pain
Immediate - anxiety assures safety from cause eg hopping up after falling
Subsequent response
Wonder about past present and future implications - may affect motivation
Concentration on damage and worry for future consequences - should look for in subjective interview
Seeks relief
Chronic/Persistent Pain
Outlasts normal tissue healing time (3-6months)
Impairment is greater than would be expected form physical findings or injury
Pain occurs in absences of identifiable tissue damage
3 Different Dimensions of Pain
Sensory
Cognitive
Affective
Sensory Pain
The what and where aspect of the pain/the physical aspects of the pain sensation
Eg feeling the throbbing of a headache
Affective Pain
The emotional distress and unpleasantness tied to pain
The motivational drive to escape the painful stimulus eg fear, anxiety, despair
Eg the fear or frustration accompanying chronic pain, or the anxiety it will never stop
Cognitive Pain
The role of thoughts, attention and evaluation in the pain experience
How your mental states nd pain interpretation affects intensity and unpleasantness of pain
Eg if you get distracted you might forget about pain
Areas of Pain
Localised
Referred/Widespread
Localised pain
pain at the origin of injury or around a specific structure
Referred/Widespread Pain
Pain felt at areas remote from the origin of pain or far from the involved structure
Pain Mechanisms (3)
Peripheral Sensitisation/Nociceptive
Neuropathic Pain
Central Sensitisation/Nociplastic Pain
The 2 inputs based pain mechanisms
Peripheral sensitisation
Neuropathic pain
The 1 output based pain mechanism
Nociplastic/Central Sensitisation
Nociceptive Pain
Pain associated with tissue injury or damage or even potential damage
Nociceptors and their stimuli
Nociceptors are activated by potentially noxious stimuli as a body protective mechanism
Thermal, mechanical and chemical stimuli (eg fire, crushing or corrosive acid) all activate nociceptors
The 7 clinical criteria of peripheral nociceptive pain (3 criteria in the absence of 4 criteria)
Pain localised to area of injury/Recent onset
Clear proportionate mechanical/anatomical nature to aggravating and easing factors
Can be intermittent and sharp with provocation, and may be more constantly dull and achy, or throb at rest
IN THE ABSENCE OF
Pain associated with other dysesthesias
Night pain/disturbed sleep
Antalgic postures/movement patterns
Pain described as burning, shooting, sharp or electric shock like
Parasthesia vs Dysesthesia
Parasthesia
An abnormal sensation that’s not unpleasant/painful
eg pins and needles
Dysesthesia
abnormal sensation that’s always unpleasant/painful
Eg burning, stinging, shooting pain
Hyperalgesia
Increased pain from a stimulus that normally provokes less pain
Eg abnormally large pain response to a pinch
can be a symptom of something larger if there’s no clear cause of injury or if injury is healed
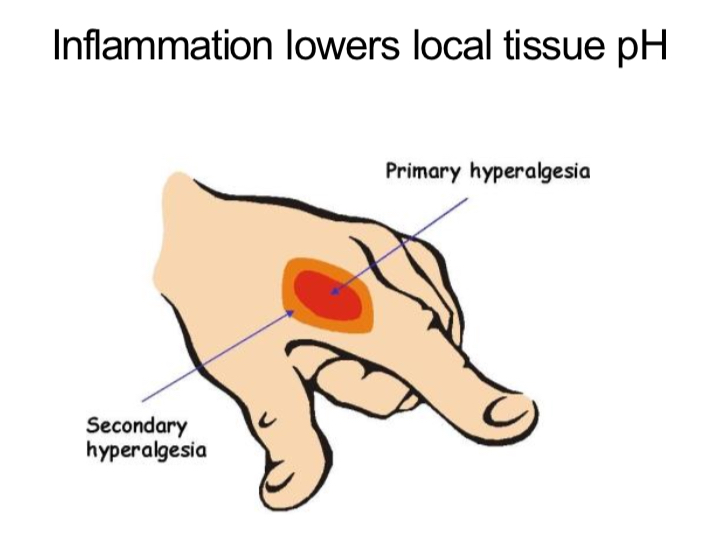
Primary and Secondary Hyperalgesia
Primary Hyperalgesia
increased sensitivity at the injury site to prevent further tissue damage
Secondary Hyperalgesia
increased sensitivity around the injury site as inflammation lowers pH of local tissue (eg red area surrounding small cut)
Allodynia
Pain due to a stimulus that does not normally provokes pain
Eg light touch, pressure or moderate cold and warmth evoke pain
seen in patients with lesions of the nervous system for example
Neuropathic Pain + its 2 subdivisions
Can result anywhere from damage along the neuraxis; peripheral nervous system, spinal or supraspinal nervous system
Subdivided into central neuropathic pain and peripheral neuropathic pain
Central Neuropathic pain
Pain caused by a lesion or disease of the central somatosensory nervous system
Peripheral Neuropathic Pain
Pain caused by a lesion or disease of the peripheral somatosensory nervous system
2 Mechanisms of Nerve ‘Damage’
Mechanical Pressure
Chemical irritation
Mechanical pressure causing nerve damage
Mechanical pressure triggers ectopic nerve impulses in damaged nerves by altering ion channel distributions and excitability.
This creates Abnormal Impulse Generating Sites along the axon, which become hyper-excitable and fire spontaneously even in response to non-noxious stimuli
Chemical irritation and nerve damage
Injury of the nerve can cause ion channels to group at injury and this leads to increased excitability and a loss of potassium channels to modulate/regulate nerve activity
The 2 symptoms and 1 sign of peripheral sensitisation/neuropathic pain
2 symptoms
pain referred in a dermatomal/cutaneous distribution or pattern
History of nerve injury, pathology, or a mechanical compromise
1 sign
Pain/symptom provocation with mechanical tests eg neurodynamic that move or load neural tissue
Anecdotally
descriptors of burning or shooting pain (however this can overlap with central sensitisation)
6 Conditions associated with neuropathic pain - Central Nervous System
Strokes
Spinal cord injuries
Syringomyelia + Syringobulbia (fluid filled cavity in the spinal cord and brain stem respectively)
Trigeminal and glossopharyngeal neuralgias
Neoplastic and other space occupying lesions
Central pain in multiple sclerosis
6 Conditions associated with neuropathic pain - Peripheral Nervous System
Nerve compression/entrapment neuropathies
Post traumatic neuropathy
Phantom limb pain
Disease related neuropathies eg diabetic neuropathy
Complex regional pain syndrome
Central Sesistisation/Nociplastic Pain
PLASTIC=ADAPTED=CENTRAL=BRAIN
Pain that arises from altered Nociceptive despite no clear evidence of actual or threatened tissue damage causing the activiation of nociceptors, OR evidence of disease or lesion of the somatosensory system that would cause this pain.
Pain disproportionate to the nature and extent of the injury or pathology, with a disproportionate and unpredictable pattern of response to aggravating and easing factors.
Strong association with maladaptive psychosocial factors eg negative emotions, pain behaviours, medical conflict
Hickam’s Dictum
“A patient can have multiple coincident unrelated disorders”
meaning we should treat by focusing on the dominant mechanism of pain