Alterations in Intracranial Regulation/Neurologic Disorders
1/27
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
28 Terms
Pediatric Differences
Open Fontanelles:
A child with open fontanelles can compensate for increased volume through widening of sutures and skull expansion; however, spatial compensation is limited.
Once all compensatory mechanisms are exhausted, further volume increase can result in a rapid rise in intracranial pressure (ICP).
Persistence or Reappearance of Primitive Reflexes (e.g., Babinski):
May be an indicator of a pathologic condition.
Importance of Obtaining Pregnancy and Delivery History:
It is important to obtain a thorough pregnancy and delivery history, as both intrauterine and extrauterine factors can influence how the central nervous system matures.

Neurologic Assessment
Loss of Consciousness (LOC):
****A change in LOC is the earliest indicator of improvement or deterioration in neurologic status.****
Full consciousness: Awake and alert; oriented to time, place, and person; exhibits age-appropriate behaviors.
Confusion: Disorientation is present; the child may be alert but responds inappropriately to questions.
Obtunded: Limited responses to the environment; falls asleep unless stimulated.
Stupor: Responds only to vigorous stimulation.
Coma: Cannot be aroused, even with painful stimuli.
Extreme irritability or lethargy is considered an abnormal finding.
Vital Signs:
Temperature may be variable.
Cushing’s Triad (Late Sign):
Elevated blood pressure with widened pulse pressure, bradycardia, and irregular respirations.
Eyes:
Assess pupil size, reactivity, and symmetry.
Motor Function:
Observe for spontaneous activity and response to painful stimuli.
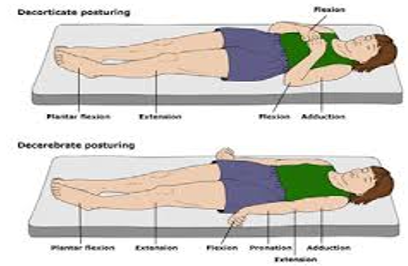
Posturing:
Decorticate (Flexion): Extremities flexed toward the “core.”
Indicates severe dysfunction of the cerebral cortex or lesions to the corticospinal tracts.
Usually happens before decerebrate.
Decerebrate (Extension):
Indicates dysfunction at the level of the midbrain or lesions of the brainstem.
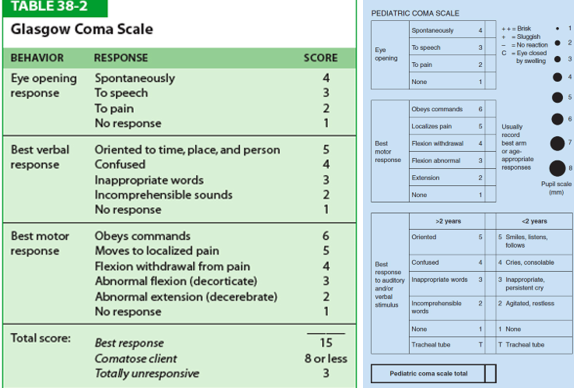
Glasgow Coma Scale (GCS)
Most popular coma scale
Three-part assessment:
Eye response
****Response to pain: squeeze the patient’s fingertip, trapezius muscle, or apply pressure to the supraorbital notch.****
Verbal response
Motor response
Best Motor Responses:
Moves to localized pain: Attempts to reach toward the painful site, bringing the hand above the clavicle.
Flexion withdrawal from pain: Flexes the arm at the elbow to pull away from pain.
Abnormal flexion (decorticate): Internal rotation of the shoulder, flexion of the elbow, pronation of the forearm, and wrist flexion.
Abnormal extension (decerebrate): Head is extended; arms and legs are extended.
Score of 15: Unaltered level of consciousness.
Score of 8 or below: Accepted definition of coma (“Less than 8… intubate.”)
Score of 3: Deep coma or death.
scores 9 to 14—more frequent neuro checks**
[Neuro] Lab and Diagnostics Tests
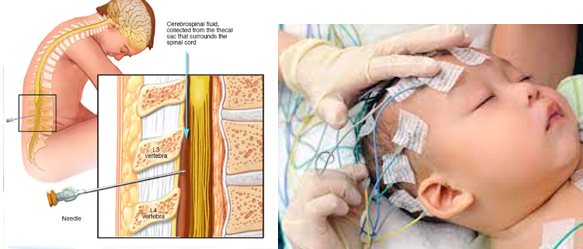
Lumbar Puncture (LP)
Head and Neck X-ray—(a lot of times our starting point)
Computed Tomography (CT)
Ultrasound—(cranial US for open anterior fontanelle)
Magnetic Resonance Imaging (MRI)
Electroencephalogram (EEG)—seizure activity
Intracranial Pressure Monitoring
Signs of Increased Intracranial Pressure (ICP)
Clinical Manifestations in Infants:
Tense, bulging fontanelle
Irritability/restlessness
Drowsiness
High-pitched/neuro cry**
Poor feeding
Setting sun sign (eyes rotated downward)***
Separated cranial sutures
Distended scalp veins
Clinical Manifestations in Children:
Headache
Nausea/vomiting
Diplopia, blurred vision—(kids will get closer to things to see)
Seizures
Indifference, drowsiness
Late Signs in Infants and Children:
Bradycardia
Decreased motor response to command
Decreased sensory response to painful stimuli
Alterations in pupil size and reactivity
Flexion (decorticate) and extension (decerebrate) posturing
Cheyne-Stokes respirations
Papilledema
Decreased consciousness
Coma

Seizures
Epilepsy:
Seizures are triggered recurrently from within the brain.
Many children outgrow seizures, while some will have them for their entire lifetime.
Goal: Manage seizures while maintaining or improving quality of life.
Diagnostic and Laboratory Testing:
EEG, Lumbar Puncture, MRI, CT
CBC, Electrolytes (hyponatremia), Glucose (hypoglycemia), BUN
Nursing Interventions:
Keep the patient safe: suction, oxygen, rail padding, etc.
If a seizure lasts longer than 5 minutes, medicate!
Monitor respiratory status after administering medications.
Management:
Focuses on controlling seizures or reducing their frequency.
Medications: Benzodiazepines, anticonvulsants (e.g., Keppra, phenobarbital, valproic acid, diazepam, lorazepam)
Check blood glucose levels and electrolytes; evaluate the underlying cause.
Surgery: May involve removal of the area of the brain responsible for the seizure.
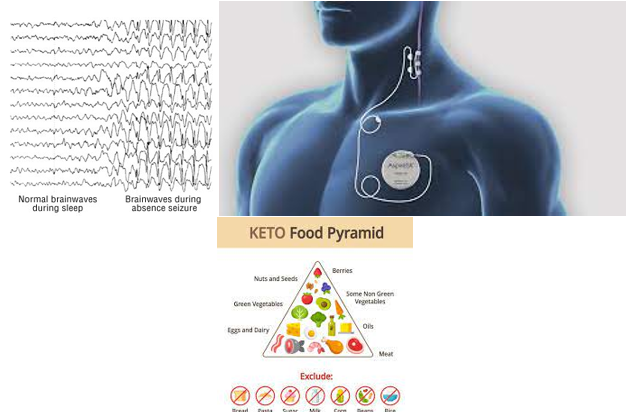
Diet: Ketogenic Diet
High intake of fats, adequate protein, and very low intake of carbohydrates, resulting in a state of ketosis.
The child is maintained in a mild state of dehydration.
Implant: Vagal Nerve Stimulator
A nerve stimulator is implanted, and a lead wire is wrapped around the vagus nerve.
The stimulator is programmed to provide the appropriate dose of stimulation at preset intervals; additional stimulation can be administered if needed.
Patient and Family Education:
No bathing or swimming alone.
May delay or exclude obtaining a driver’s license. (typically have to be seizure-free for a year)
Avoid alcohol or illegal drugs.
Be aware of medication interactions.
Types of Seizures
Febrile Seizure
Absence (Petit mal)
Tonic-Clonic (Grand mal)
Myoclonic
Atonic (Drop attacks)
Status Epilepticus
Febrile Seizure
Most common seizure type in children.
Occurs between 6 months to 5 years of age**
No previous neurologic abnormalities.
Benign and self-limiting**.
Child will receive a physical examination with appropriate tests during assessment.
Returns to alert mental status within 3 minutes.
Rapid rise of fever >100.4°F (38°C)**
Risk factors: Viral infection, family history.
Most children will outgrow this condition.
Absence (Petit Mal)
Sudden cessation of activity or speech with a blank facial expression.
Tonic-Clonic (Grand Mal)
Generalized and most dramatic seizure type.
Often associated with an aura.
Loss of consciousness, may be preceded by a piercing cry.
Tonic phase: Entire body experiences sustained contractions.
Clonic phase: Rhythmic jerking alternating with relaxation of muscles.
Cyanosis may occur due to apnea.
Saliva may collect in the mouth due to inability to swallow (suction + oxygen!).
Child may bite their tongue.
Loss of sphincter control, especially the bladder, is common (incontinence).
Myoclonic
Sudden, brief muscle jerks.
May involve the whole body or one body part.
Child may or may not lose consciousness.
Atonic (Drop Attacks)
Sudden loss of muscle tone.
In children, may present as a sudden drop of the head.
Child regains consciousness within a few seconds to a minute.
Can result in injury due to a sudden, violent fall.
Status Epilepticus
Neurologic emergency!
Prolonged seizure or clustered seizures where consciousness does not return between episodes.
Using up a lot of energy, so check that glucose!
Prognosis depends on child’s age, cause of seizures, and duration of status epilepticus.
Prompt medical intervention is essential to reduce morbidity and mortality.
Postictal Phase
Child may be semi-comatose or in a deep sleep for 30 minutes to 2 hours
Responds only to painful stimuli
No memory of the seizure
May complain of headache and fatigue
Safety of the child is a primary concern
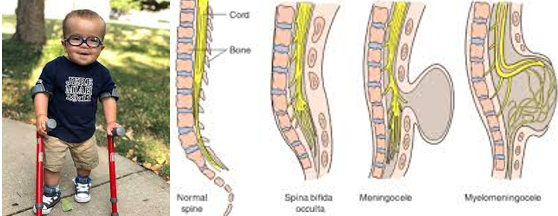
Neural Tube Defects (NTD)
Failed closure of the neural tube around the 3rd or 4th week of gestation.
May involve the entire length of the neural tube or only a small portion.
Cause:
Folic Acid Deficiency is responsible for 50% or more of cases.
All pregnant mothers should take 0.4 mg of folic acid daily!***
A higher dosage is recommended if there is a history of neural tube defects (NTDs).
Other cases are multifactorial in origin.
Types of Neural Tube Defects (NTDs):
Anencephaly
Spina Bifida Occulta
Spina Bifida Cystica:
Meningocele
Myelomeningocele
NTD: Anencephaly
Absence of cerebral hemispheres.
Brainstem function may be intact.
Incompatible with life:
Survival typically only lasts a few hours to a few days.
Death usually occurs due to respiratory failure.
Nursing Management:
Focuses on supportive care and comfort measures for the dying infant.
Provide emotional support for parents.
An infant cap may be helpful for comfort and bonding.

Categories of Spina Bifida
Spina Bifida Occulta:
Not visible externally.
Defect of the vertebral bodies without protrusion of the spinal cord or meninges.
May present with:
• Sacral dimple
• Hairy patch
• Skin discoloration (big birthmark)
Potential complication: Tethered Cord
Spina Bifida Cystica:
Meningocele:
Sac contains meninges and spinal fluid, but no neural elements.
Spinal cord is usually normal
Minor to no neurologic effects
Myelomeningocele:
Sac contains meninges, spinal fluid, and nerves.
Varying and often serious neurologic deficits.
Spinal cord ends at the level of the defect.
Results in absent motor and sensory function below the lesion.

Myelomeningocele: The Sac
May present as a fine membrane.
Could be covered with dura, meninges, or skin.
Location and magnitude of the defect determine the nature and extent of the impairment.
The sac is prone to leakage of cerebrospinal fluid (CSF) and is easily ruptured.
Precautions:
Avoid contamination from urine or feces. Use saran wrap, proper positioning, or a urinary catheter.
Management:
Prevent infection!
If the sac is open, use sterile saline or antibiotic-soaked dressings to prevent drying out.
Positioning: Keep the baby in a prone position.
Assess neurologic status and associated anomalies.
Manage genitourinary function, bowel control, and orthopedic concerns, especially regarding locomotion.
Early closure of the defect is critical.
Maintain a latex-free environment.
Children with spina bifida are often sensitive to latex due to increased exposure during surgeries and catheterizations.

Skull Deformities
Craniosynostosis: “syn = surgery”
Premature closure of the cranial sutures.
Premature closure may lead to decreased brain growth.
When only one suture is fused, neurologic impairments are rarely seen.
When two or more sutures are fused, neurologic complications, such as hydrocephalus with increased intracranial pressure (ICP), are more likely to occur.
Neurological complications: Hydrocephalus with increased ICP.
Treatment: Surgery. “sooner rather than later!”
Plagiocephaly: “P = positional”
Positional plagiocephaly refers to asymmetry in head shape without fused sutures.
The “Back to Sleep” program has led to an increase in this condition.
Treatment:
Increased tummy time when awake.
Avoid keeping the baby in a car seat other than when in the car.
Molding helmet if necessary.

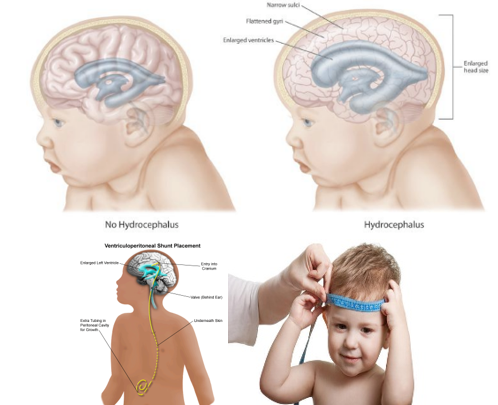
Hydrocephalus
Imbalance in the production and absorption of cerebrospinal fluid (CSF) in the ventricular system.
With the accumulation of CSF, the ventricles dilate, compressing brain tissue and leading to increased intracranial pressure (ICP).
Causes include developmental defects, neoplasms, infections, trauma, or hemorrhage.
Therapeutic Management:
Ventriculoperitoneal (VP) Shunt Placement:
The VP shunt will need to be replaced as the child grows.
Be aware of signs of increased ICP in children with VP shunts.
Shunts may become occluded, infected, or may break.
Endoscopic Third Ventriculostomy (ETV):
Improves the flow of CSF out of the brain.
A tiny hole is made at the bottom of the third ventricle, allowing CSF to divert and relieve pressure.
Sometimes done with choroid plexus cauterization to decrease CSF production.
Choroid plexus cauterization uses an electric current to burn the CSF-producing tissue (the choroid plexus) in the lateral ventricles, reducing CSF production.
Prognosis:
Depends on the rate at which hydrocephalus developed.
The duration of increased ICP.
The underlying cause of hydrocephalus.
Nursing Care Management:
Observe for signs of increasing ICP.
Measure head circumference.
Palpate fontanelles and suture lines.
Post-Operative Care:
Pain management.
Monitor for signs of increased ICP and infection.
Provide family support and education.
Contact sports and activities that promote twisting at the waist should be avoided unless specifically approved by their healthcare provider.
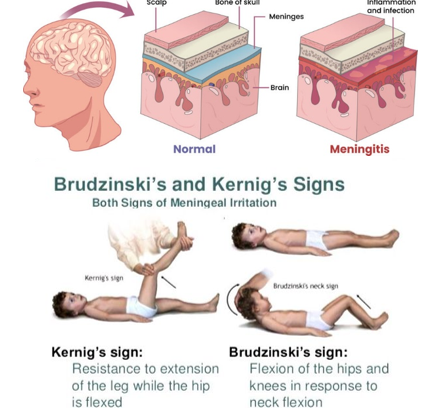
Bacterial Meningitis
Infection of the meninges, the lining that surrounds the brain and spinal cord.
Common pathogens: Haemophilus influenzae type B, Escherichia coli, Neisseria meningitidis (meningococcal meningitis)
Vaccination for Haemophilus influenzae type B and pneumococcal infections has significantly decreased the incidence.
Symptoms:
Stiff neck** (#1 hallmark sign!!)
Fever
Headache
Vomiting
High-pitched cry (infants)
Bulging fontanelle
Photophobia** (lights are dimmed)
Rash (petechiae or purpuric)—doesn’t blanch.
If petechiae or purpura appear on the extremities, it is likely meningococcal meningitis. Rapid treatment is essential to save the patient’s extremities and life.
Positive Kernig (kick) and Brudzinski (bend) signs**
Post-Lumbar Puncture Care:
After a lumbar puncture, the patient should lay flat in bed to prevent CSF leakage and spinal headache.
Lumbar Puncture Results:
CSF pressure will be elevated.
CSF will show:
Elevated white blood cells (WBCs)
Elevated protein (bacterial)
*Low glucose (bacteria feed on glucose—so it’s a big sign its a bacterial infection)
Treatment:
Droplet Isolation:
Nurse wears a mask in the patient’s room.
Patient wears a mask when outside the room.
Isolation maintained until 24 hours after antibiotics have been administered.
Antibiotics:
IV antibiotics started immediately after CSF and blood cultures are obtained.
Seizure Precautions:
Minimize stimuli.
Monitor:
Watch for signs of increased intracranial pressure (ICP).
Full monitor (BP, HR, RR, Pulse Ox).
Fluid Management:
Administer fluids cautiously to avoid worsening ICP.
Fever and Pain:
Treat promptly.
Prevention:
Vaccinations: Hib, meningococcal vaccine.
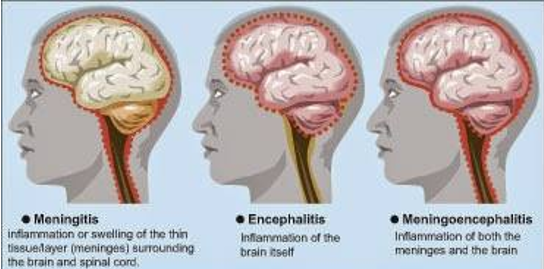
Encephalitis
Is an inflammation of the brain that may also involve the meninges.
Can be caused by protozoan, bacterial, fungal, or viral invasion (most commonly viral).
Common Symptoms:
Fever**
Flu-like symptoms
Altered level of consciousness (LOC)**
Headache**
Lethargy
Generalized weakness
Seizure activity
Diagnostics and Lab Tests:
Lumbar puncture (LP)
CBC
MRI, CT
Electrolytes
Glucose
Treatment:
Antivirals (as the cause is most often viral)
Seizure precautions (suction + oxygen @ bedside)
Monitor LOC
Key Points:
Unlike meningitis, this typically does not involve a stiff neck.
Altered LOC is almost always present in encephalitis.
Seizures are common.
**Clinical hallmark is the triad**:
Fever
Headache
Altered LOC
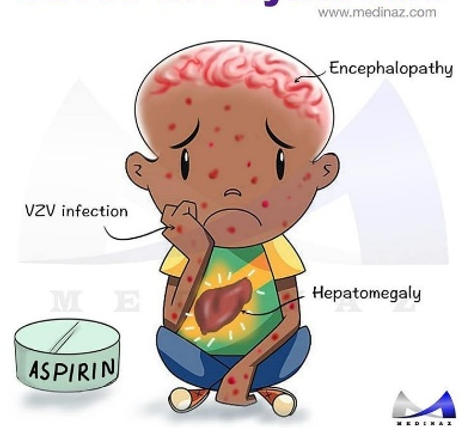
Reye Syndrome
Cause:
Most often a reaction triggered by the use of salicylates to treat a viral infection.
The exact cause of this is not fully understood; salicylates are a common association, but not definitively causal.
Clinical Manifestations:
Brain swelling
Liver failure (look for jaundice)
Potentially fatal (may result in death)
Patient Symptoms:
Profuse vomiting
Change in mental status
Lethargy
Irritability
Hyperreflexia
Seizures
Diagnostic Evaluations:
Elevated ammonia levels (altered LOC/confusion)
Elevated liver enzymes (ALT, AST)
Extended bleeding times (PT/PTT/INR)
Liver biopsy
Nursing Management:
Provide care similar to any unconscious child and for increased intracranial pressure (ICP):
Seizure precautions
IV fluids to correct glucose and electrolyte imbalances
Diuretics to decrease ICP
Vitamin K for correction of bleeding
Plasma and/or platelets as needed
Ammonia detoxicants to reduce ammonia levels
Anticonvulsants for seizure control
Mannitol for increased ICP if indicated
Frequent neuro checks
Family Education:
NO aspirin or aspirin-containing products (e.g., Pepto-Bismol)
Avoid aspirin-containing products for children under 16 years of age
Cerebral Palsy (CP)
Etiology:
Describes a range of non-specific clinical symptoms characterized by abnormal motor patterns and postures caused by nonprogressive abnormal brain function.
80% of causes occur before delivery.
Can also occur in the natal and postnatal periods.
Cause may be unknown.
Most common movement disorder of childhood.
Wide variation in severity of symptoms.
Complications:
Mental impairment
Seizures
Growth problems
Impaired vision or hearing
Abnormal sensation or perception
Hydrocephalus
Classifications:
Spastic (most common type):
Poor control of posture, balance, and movement.
Exaggerated deep tendon reflexes.
Hypertonicity of affected extremities.
Continuation of primitive reflexes.
May fail to develop protective reflexes.
Dyskinetic:
Abnormal involuntary movements; infant appears limp and flaccid.
Uncontrolled, slow, worm-like writhing or twisting movements.
Affects all four extremities; may include face, neck, and tongue.
Movements worsen with stress.
Dysarthria and drooling may be present.
Ataxic:
Affects balance and depth perception; poor coordination.
Unsteady, wide-based gait.
Delayed motor milestones and language skills.
Mixed Type:
Combination of spastic and dyskinetic features.
Therapeutic Management:
Early diagnosis
Optimize mobility, communication, and self-help skills
Provide adapted education
Promote socialization with peers
Encourage rest periods to avoid fatigue
Feeding support (may need special techniques or devices)
Prioritize safety in home and school settings
Implement physical therapy
Provide family support and education
Medical Management:
Medications:
Baclofen: Decreases spasticity
Anticholinergics: Decrease involuntary movements
For spasticity: Baclofen, Dantrolene sodium, Diazepam
Botulinum toxin: Injected into affected muscles to reduce spasticity.

Pediatric Head Injury
Causes:
Falls
Motor vehicle injuries
Bicycle or sports-related injuries
Child abuse
Shaken Baby Syndrome (SBS): Often occurs in infants younger than 9 months.
SBS is a form of child abuse; a significant number of head traumas result from it.
Risk Factors:
Physical characteristics of the child
Immature motor development
Natural curiosity and liveliness
Unattended child
Mild Head Injury:
No loss of consciousness
No penetrating injury to the brain
Typically managed at home with close observation.
Signs and Symptoms to Report:
Vomiting
Slurred speech
Changes in ambulation (walking/movement)
Headache
Fluid draining from the nose or ears
Home Monitoring:
Check the child every 2 hours for changes in responsiveness during the night.
Severe Head Injury:
Requires hospitalization until stable.
NPO (nothing by mouth)
IV fluids
No opioids/narcotics given
Seizure precautions
Close monitoring of fluid and electrolyte balance
Traumatic Brain Injury Therapeutic Management
Nursing Management:
Maintain the child’s airway; monitor breathing, circulation, and neurological status closely.
Implement spinal precautions as indicated.
If a patient has a hard cervical collar and its immobilizing their neck, we do not, as the nurse, take it off!
Treat any other injuries resulting from the trauma.
Frequently reassess neurological status, paying attention to changes in level of consciousness (LOC) and signs of increased intracranial pressure (ICP).
Initiate seizure precautions as ordered.
Medications:
Acetaminophen
Opioids (as prescribed)
Anticonvulsants
Antibiotics
Corticosteroids (if spinal cord injury)
Sedatives (not used in the acute phase)
Surgical Interventions:
Suture of lacerations or torn dura.
Reduction of fracture and/or removal of bone fragments.
Down Syndrome (Trisomy 21)
Is a genetic disorder caused by the presence of all or part of an extra 21st chromosome.
It is the most common chromosomal abnormality associated with intellectual disability.
Occurs in approximately 1 in 730 live births.
Higher incidence with maternal age over 35 years.
Between 1979 and 2003, the number of babies born with Down syndrome increased by about 30%.
Anticipatory Guidance:
Early intervention services: Occupational Therapy (OT), Speech Therapy (ST), Physical Therapy (PT)
Routine pediatric well exams and specialist follow-ups
Family support and education
Common Features of Down Syndrome:
Varying degrees of intellectual disability
Hypotonia (poor muscle tone), short stature
Depressed nasal bridge, small nose
Protruding tongue (appears large relative to the size of the mouth)
Single deep transverse crease on the palm (simian crease)
Short neck with excess skin at the nape
Associated Health Problems:
(1) Congenital heart disease occurs in 40% to 50% of individuals.
Most common heart defects:
AVSD
ASD
VSD
PDA
Tetralogy of Fallot
Increased risk for:
Leukemia (3)
Thyroid disorders (2)

Autism Spectrum Disorder (ASD)
Described as a “spectrum” of disability — ranging from high-functioning to low-functioning.
Etiology is unknown.
Social-Communication Deficits:
Non-verbal communication difficulties:
Trouble interpreting body language
Limited eye contact
Lack of facial expressions
Relationship difficulties:
Struggles with adjusting behavior to fit social context
Difficulty making friends or engaging in imaginative play
Social-emotional challenges:
Abnormal social approach
Poor back-and-forth conversation
Failure to initiate or respond to social interactions
Restrictive and Repetitive Behaviors:
Motor behaviors:
Hand flapping
Finger flipping
Other behaviors:
Excessive adherence to routines/sameness
Highly restricted or fixated interests with abnormal focus or intensity
ASD Severity Levels:
Level 1 – Requires some support
Level 2 – Requires substantial support
Level 3 – Requires very substantial support
Possible Related Conditions:
Restrictive diets
Seizure disorders
Sleep and toileting difficulties
Self-injurious behaviors
Nursing Implications:
Early intervention (Speech Therapy, Occupational Therapy, Physical Therapy)
Develop a plan of care in collaboration with the caregiver.
Coping plan: do they like to be touched, hot, cold, etc?
Avoid physical touch until rapport is built.
Involve a Child Life Specialist