Mesenteric Vasculature
1/128
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
129 Terms
Splanchnic arteries
What is the term used to describe the arteries that supply the bowel
CA (and its branches), SMA, IMA
What are the 3 main arteries that make up the splanchnic arteries which supply the bowel
Common hepatic, splenic, and left gastric
What 3 vessels branch off the celiac axis
Median arcuate ligament of the diaphragm
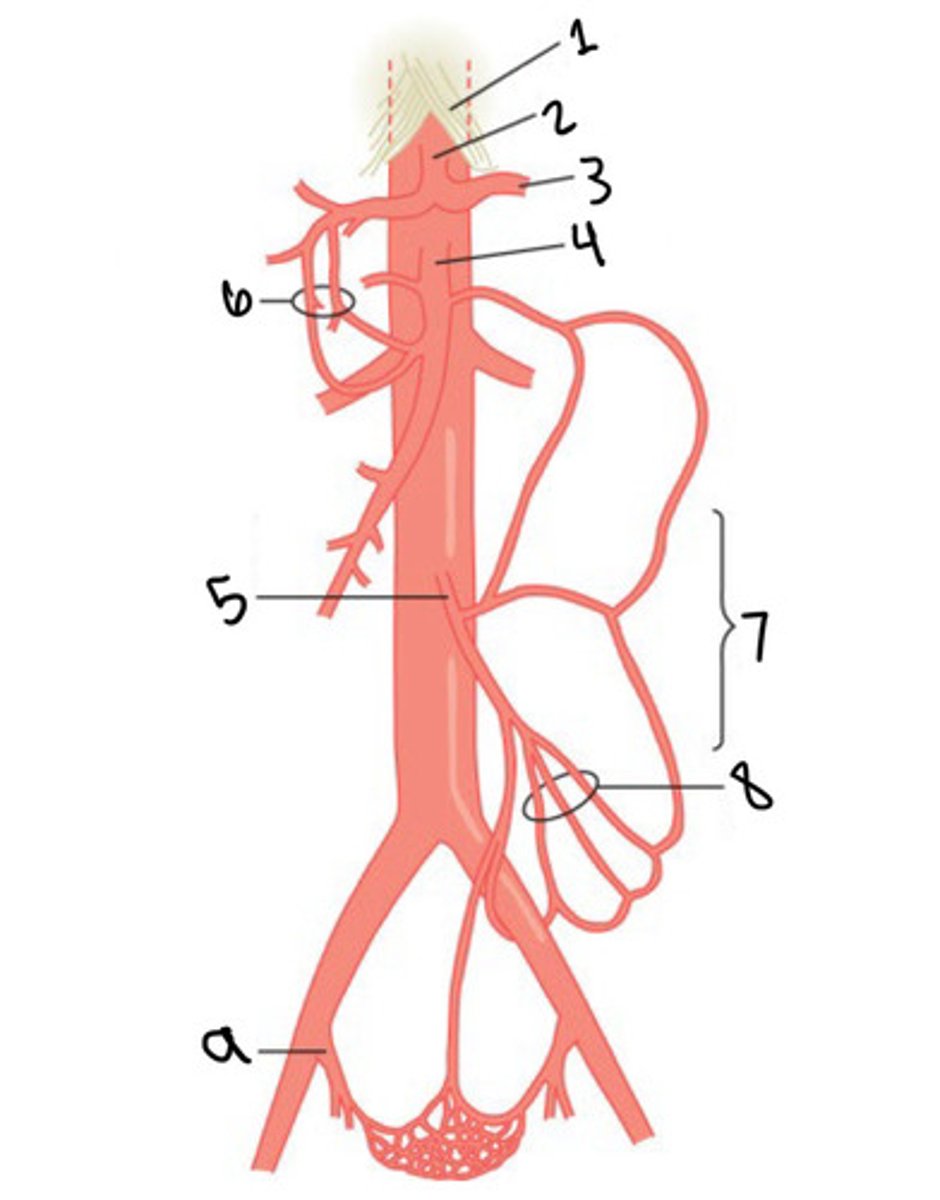
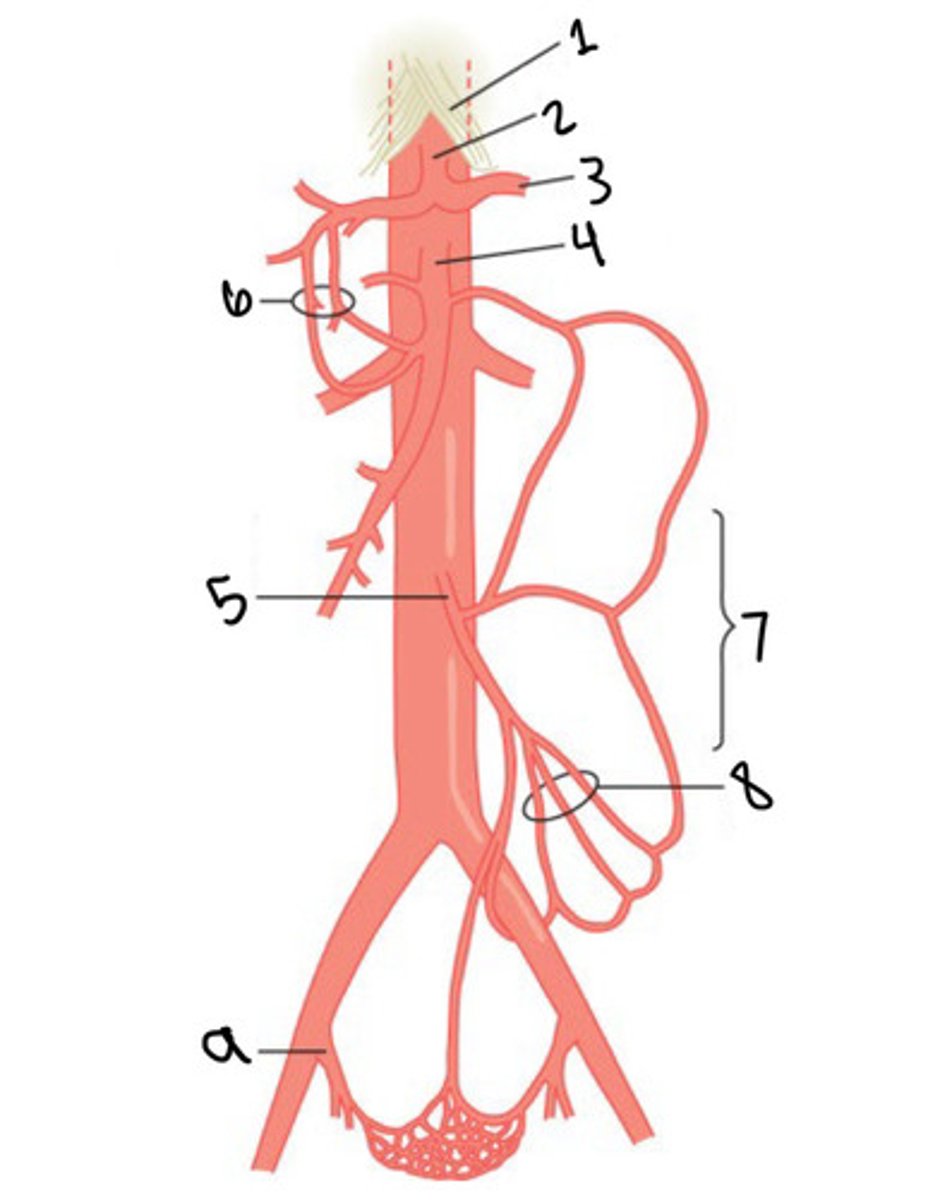
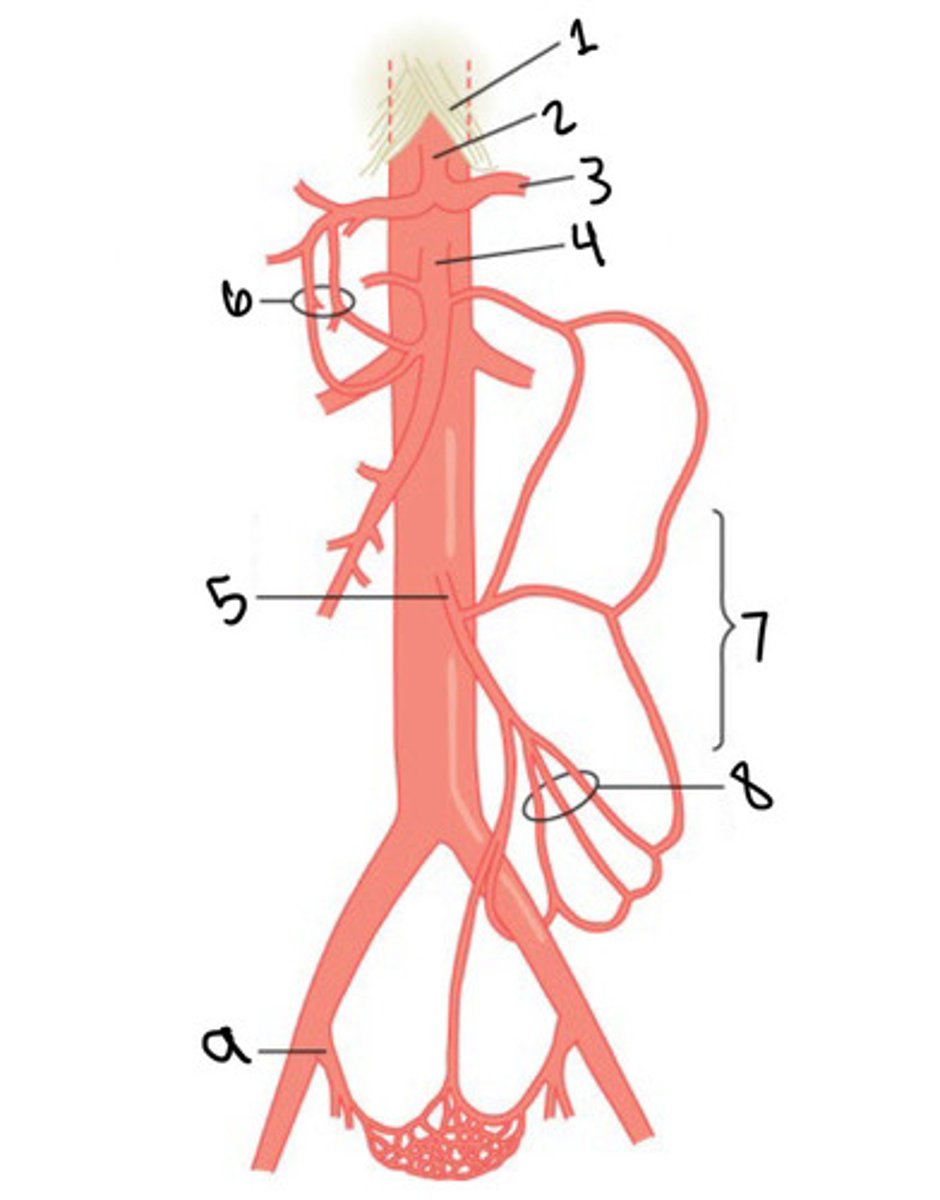
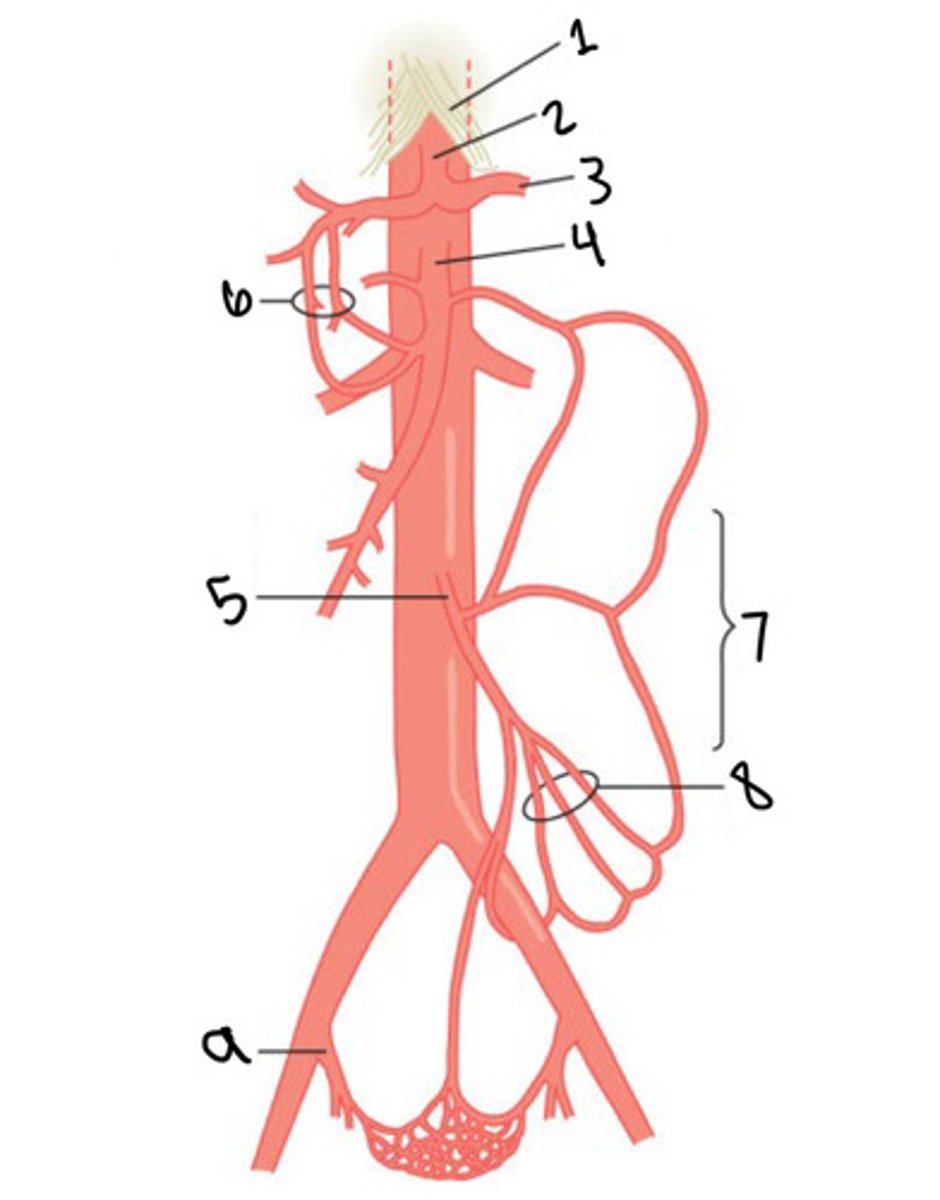
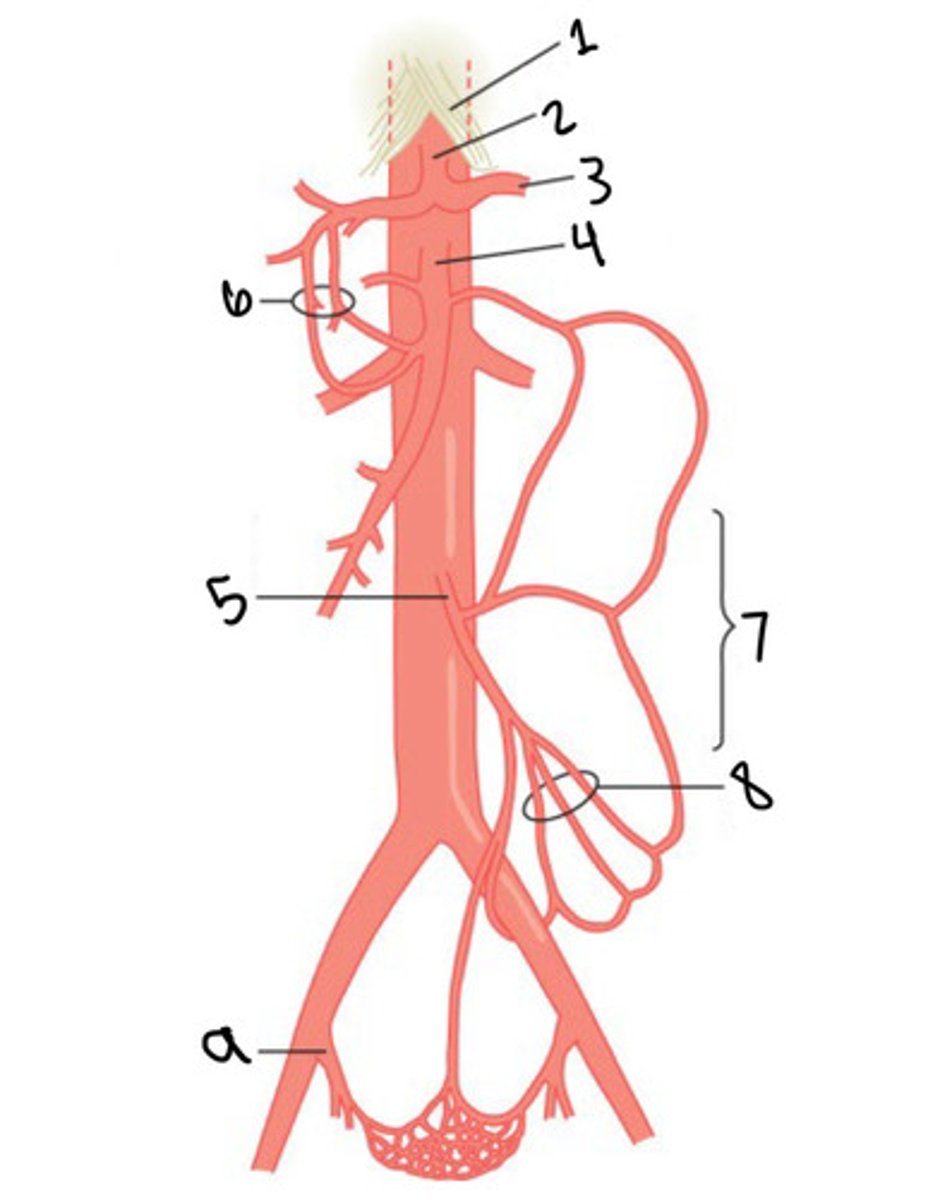
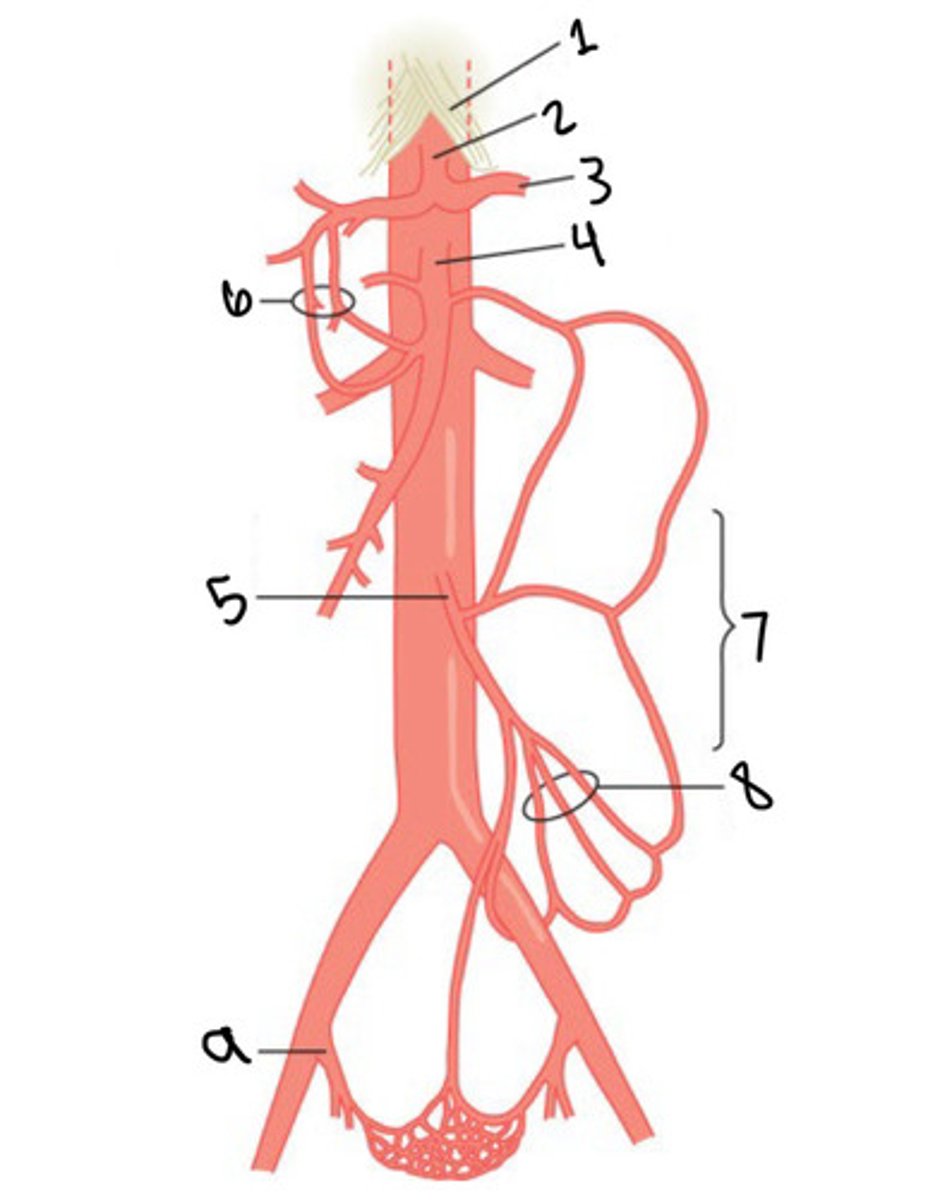
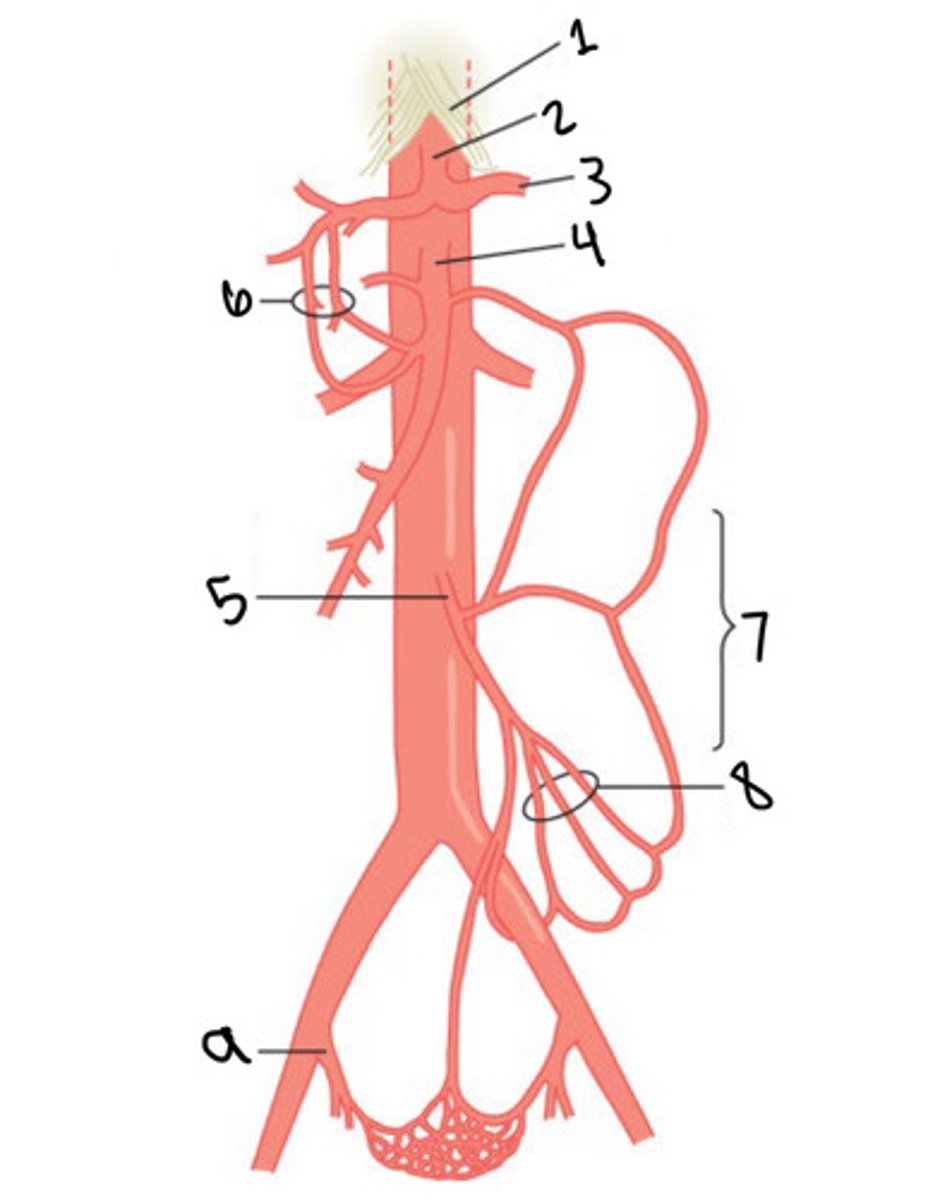
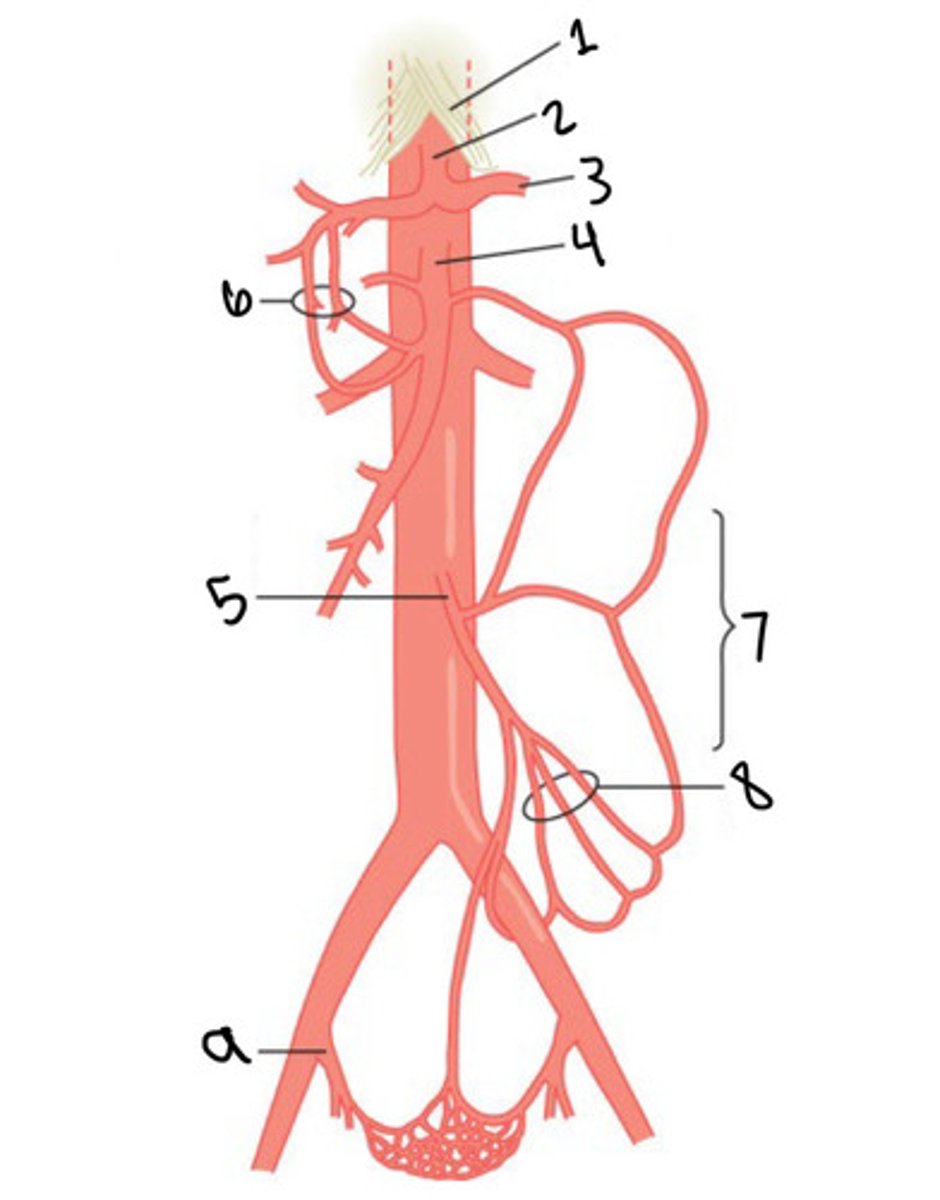
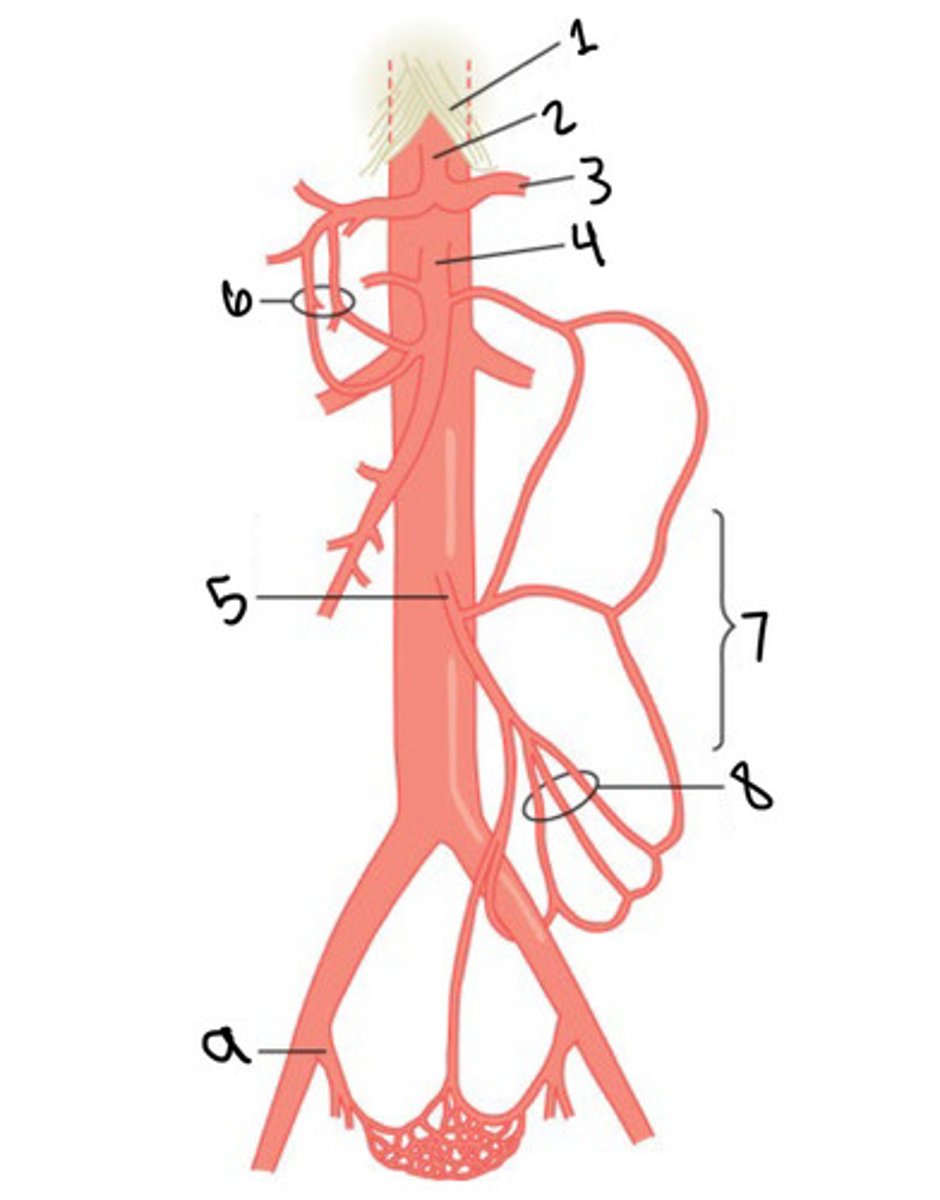
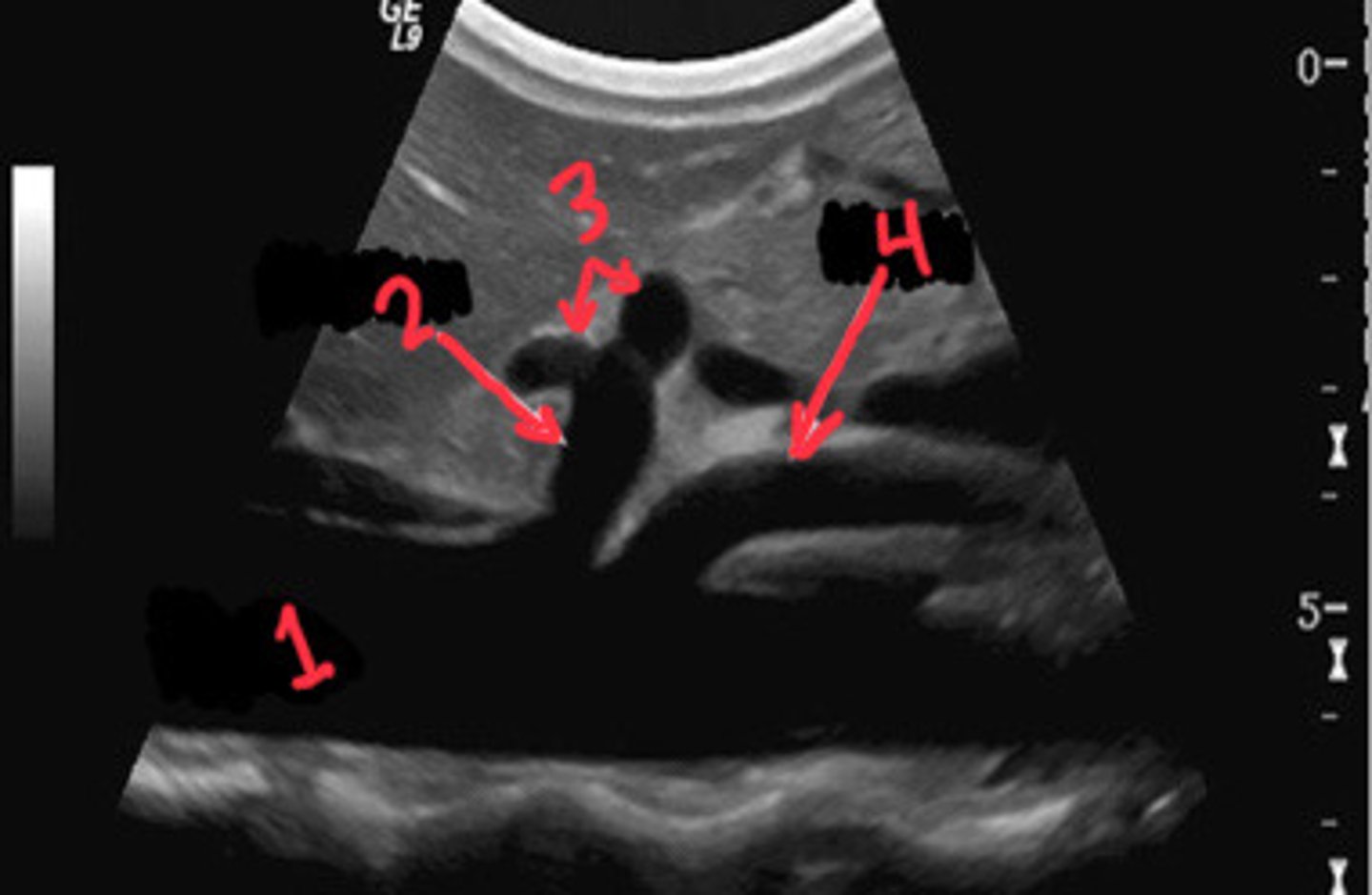
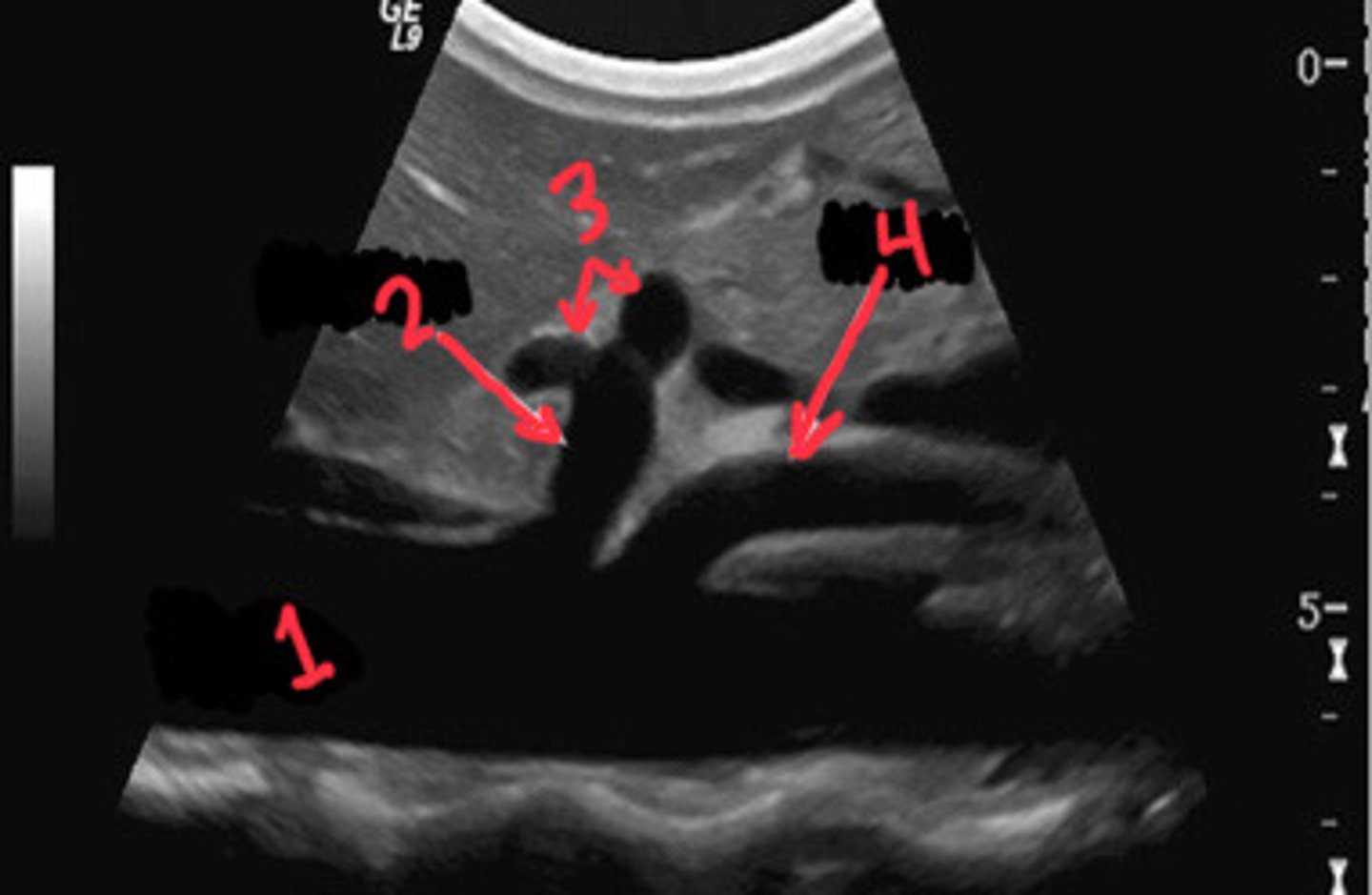
What is 1
Celiac axis
What is 2
Splenic artery
What is 3
Celiac artery
What is the first branch off of the aorta
IMA (inferior mesenteric artery)
What is 5
Gastroduodenal collaterals
What is 6
Mesenteric collaterals
What is 7
Sigmoidal arteries
What is 8
Hypogastric artery (internal iliac artery)
What is 9
SMA (superior mesenteric artery)
What is 4
Common hepatic artery taking off of the SMA instead of the CA
What is an anatomical variant of the common hepatic artery
15%
What % of people have the common hepatic taking off of the SMA instead of the CA
Low resistance
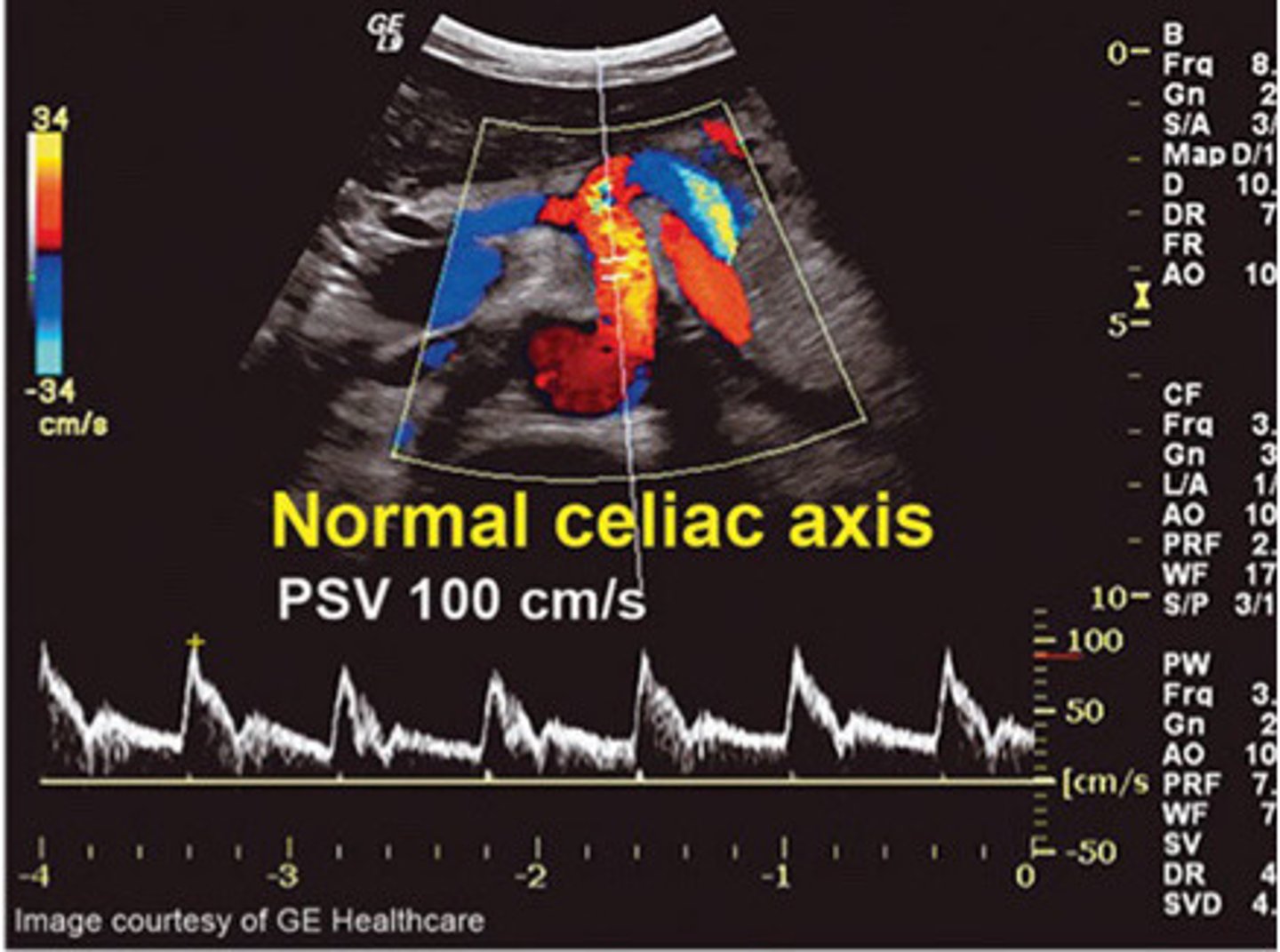
What resistance should the celiac axis bu
50-160cm/s (about, can range higher and still be normal)
What is the normal PSV of the celiac axis
≤55cm/s
What is the normal EDV of the celiac axis
Stomach, liver, pancreas, duodenum, and spleen
What structures does the celiac axis and its branches supply
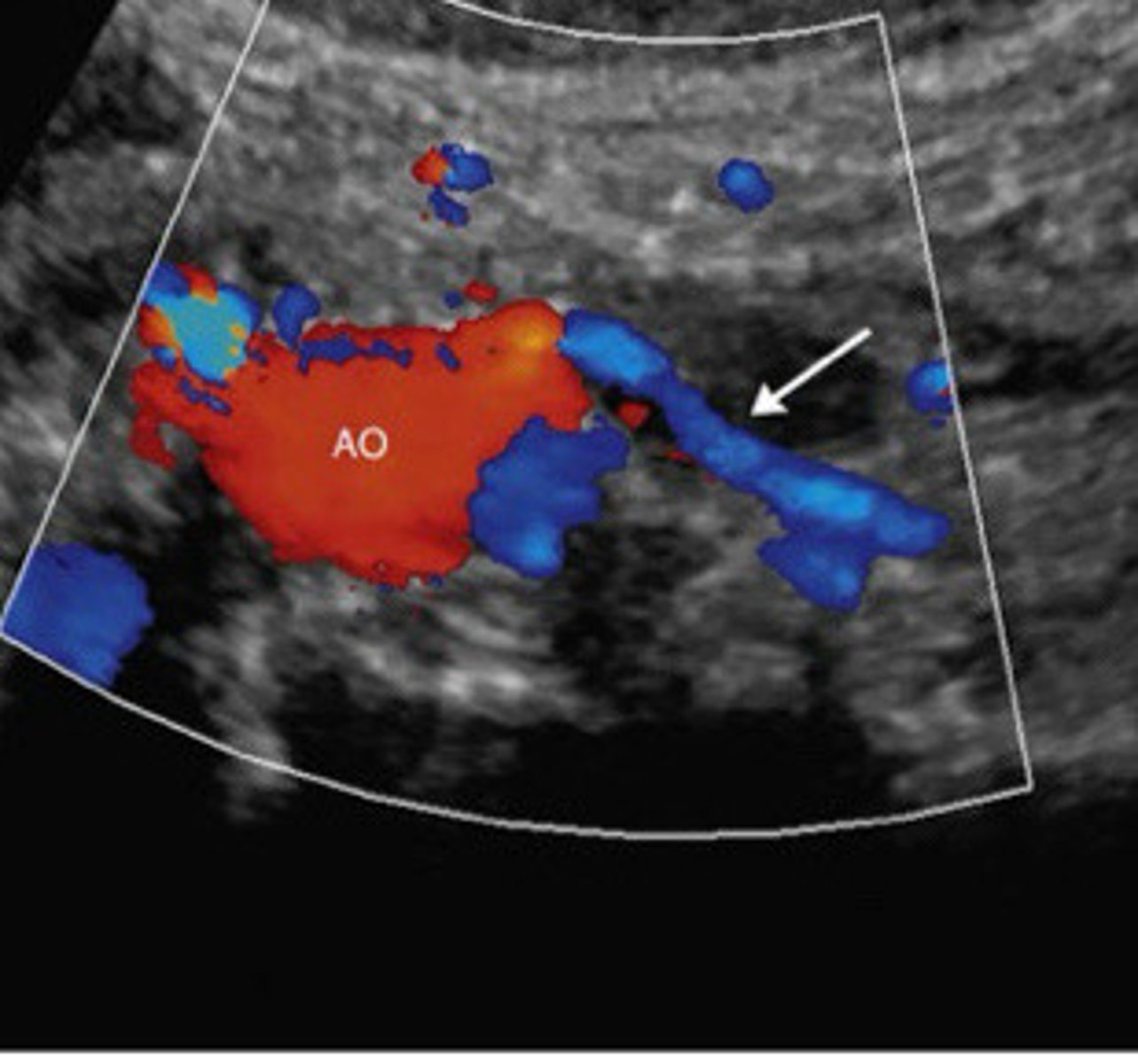
Normal waveform of the celiac axis (low resistance and PSV between 50-160cm/s)
What does this image show
1-2cm
How far distal is the SMA from the celiac axis
True
T/F: there is an anatomical variant in which the SMA and the celiac axis occasionally share a common trunk
Aorta
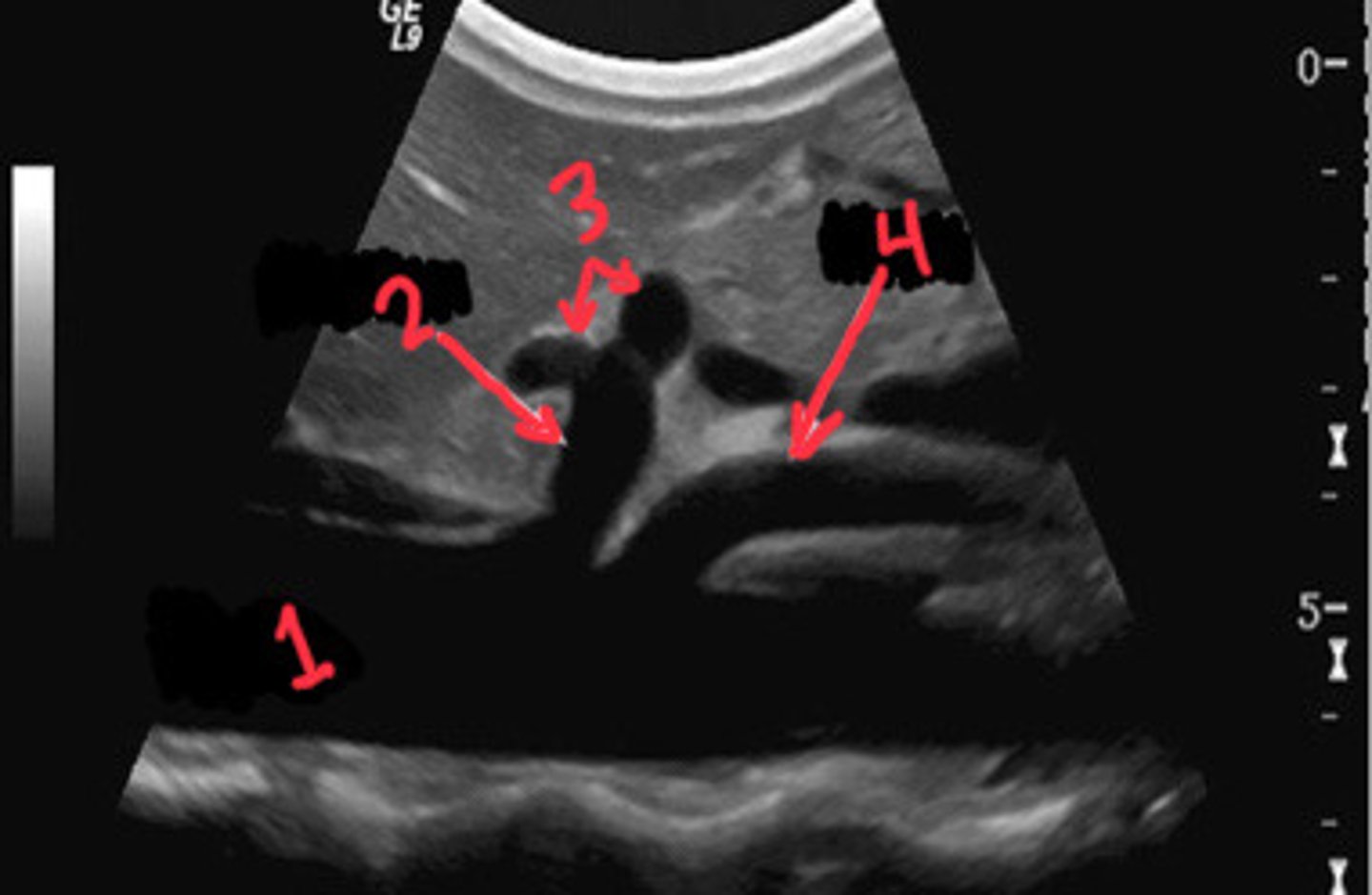
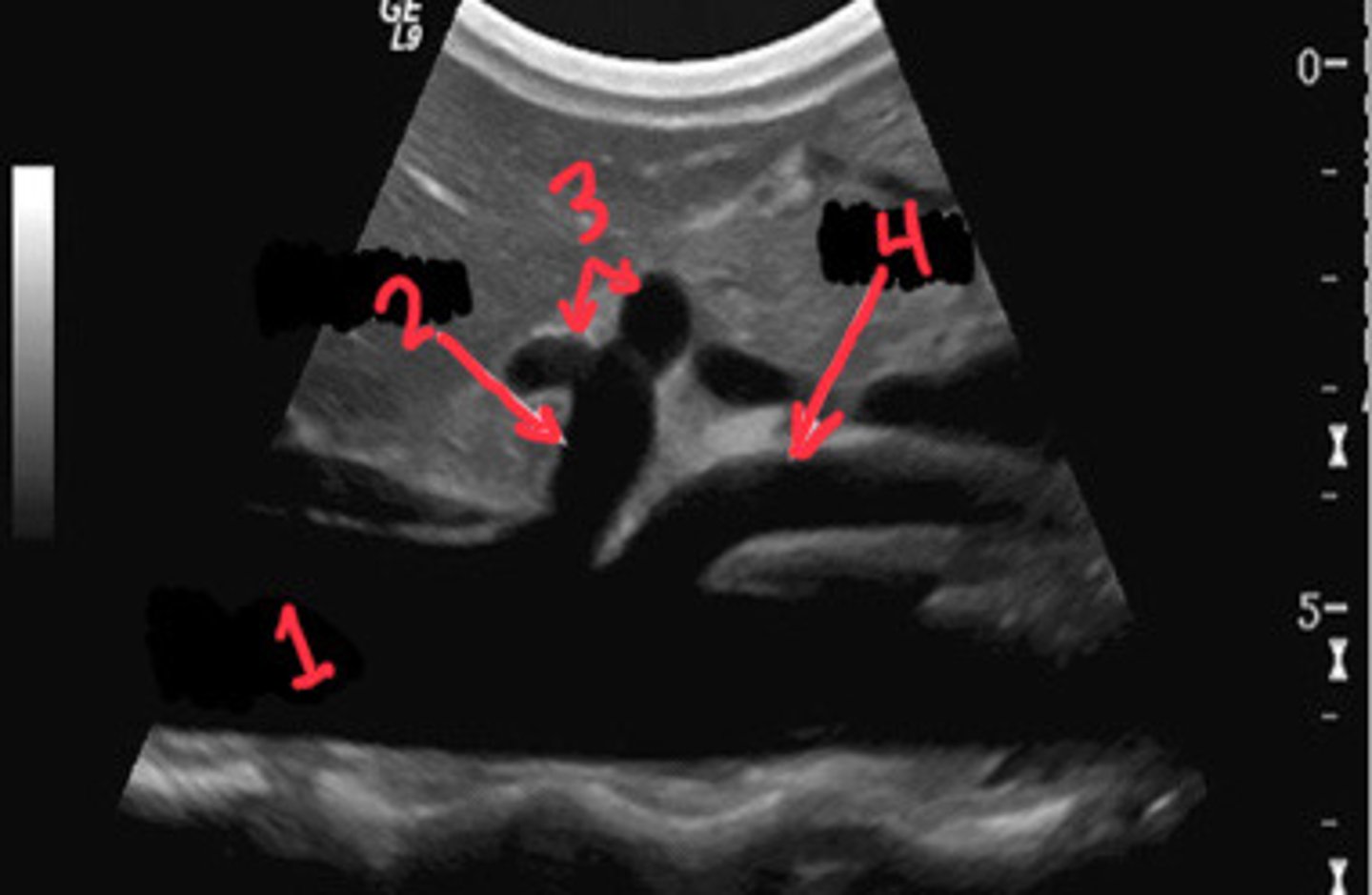
What is 1
CA
What is 2
Branches of the celiac axis
What is 3
SMA
What is 4
Small intestine, cecum, ascending colon, and part of the transverse colon (pretty much small intestine to transverse colon)
What does the SMA supply
Metabolic activity of the gut
What causes the flow to vary within the SMA
High resistance and multiphasic
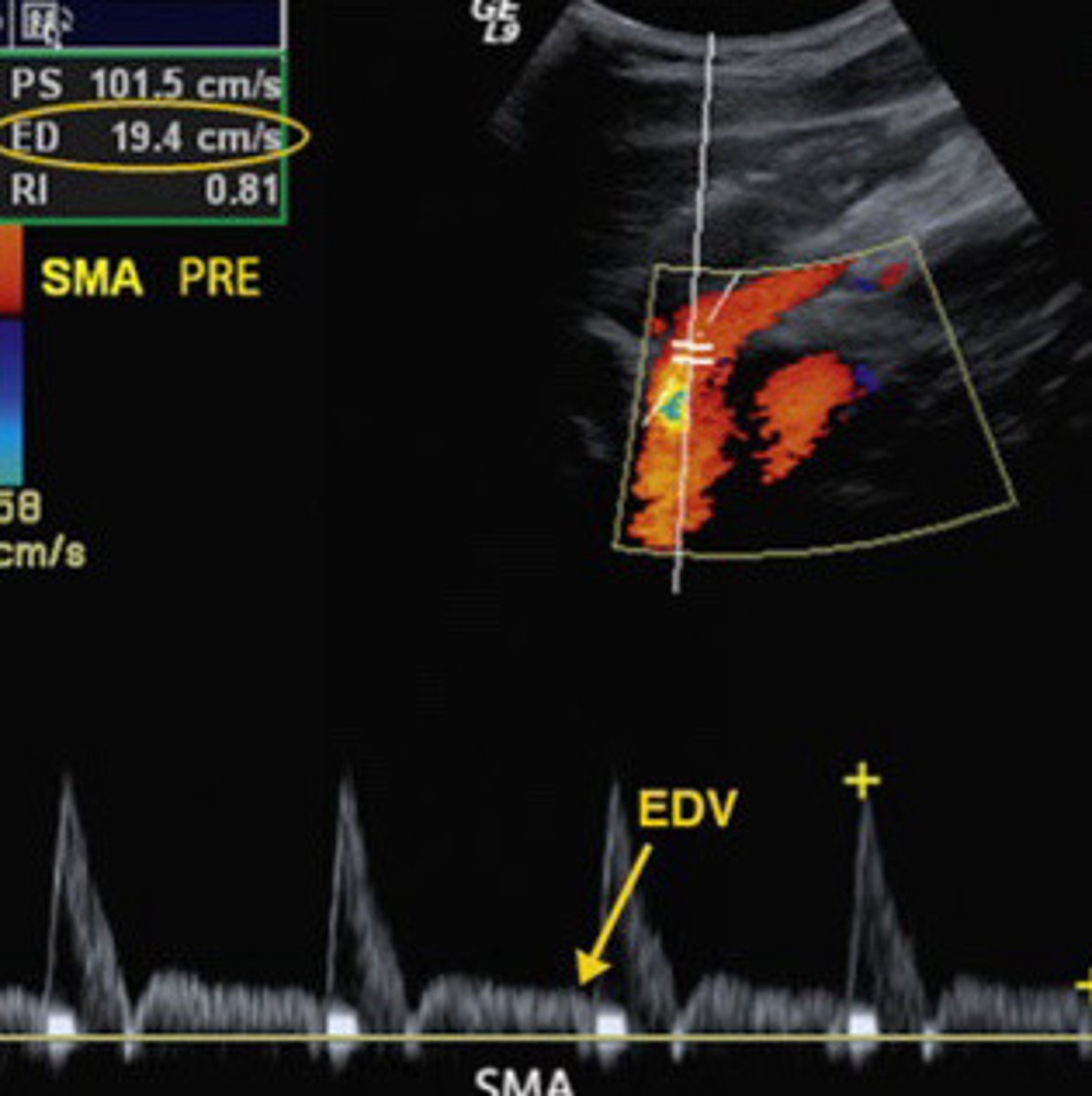
Describe the waveform seen in the SMA when the patient is in a fasting state
110-175cm/s
What about is the normal PSV of the SMA when the patient is in a fasting state
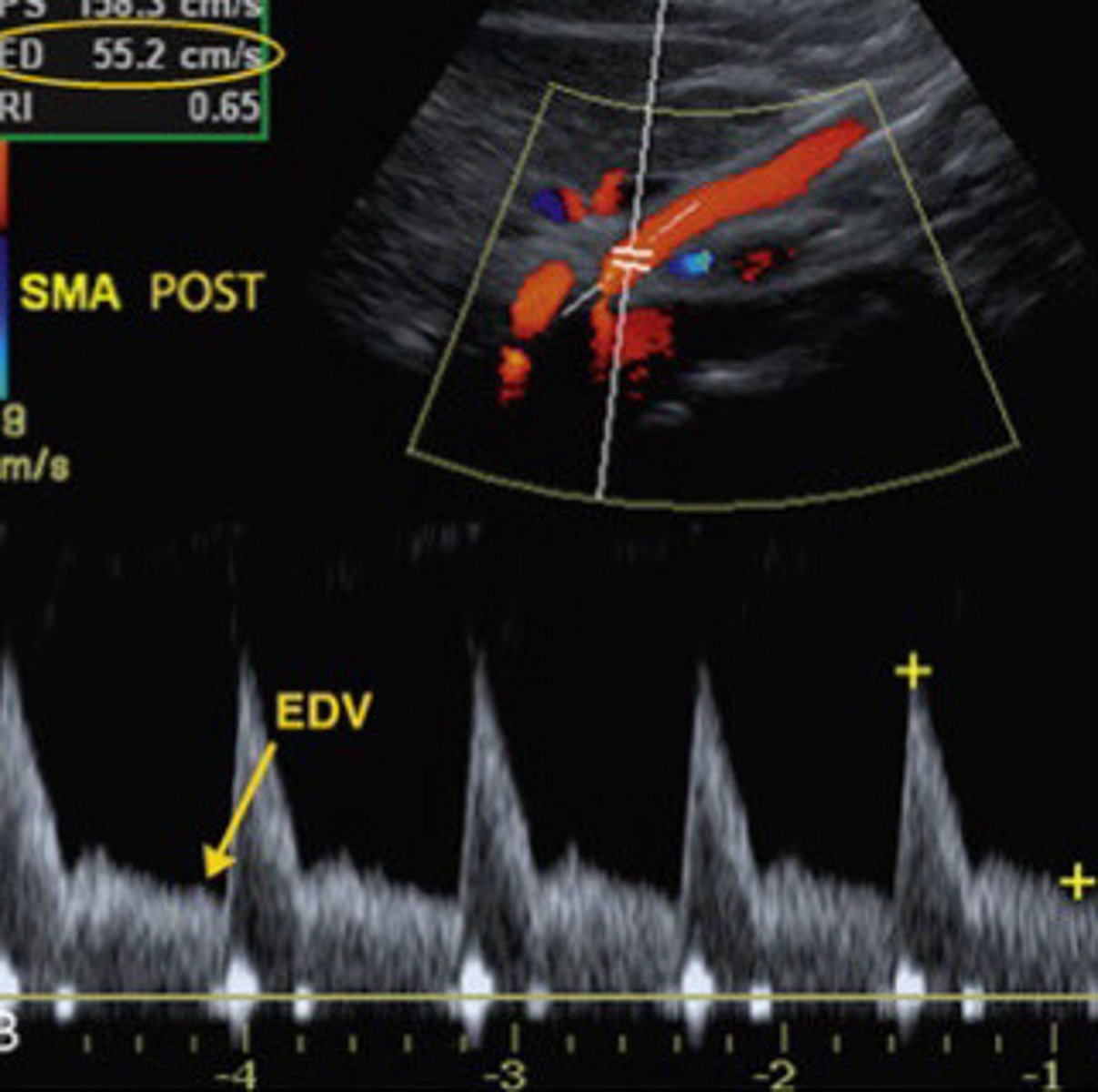
Low resistance (will probably be monophasic)
Describe the waveform of the SMA when the patient is in a post prandial state
Pre prandial
What is another term for fasting
High velocity then pre-prandial (not really an exact #)
What is the normal PSV seen in the SMA when the patient is in a post-prandial state
Fasting/preprandial (higher resistance, can see dicrotic notch and not a lot of diastolic flow)
Is this image taken form the SMA most likely from a patient who is pre-prandial or post-prandial
Post-prandial
Is this image taken form the SMA most likely from a patient who is pre-prandial or post-prandial
3-4cm superior to the bifurcation of the aorta
Where is the IMA located
Around 1:00 in to the left
Describe the take off of the IMA off the aorta that is usually seen in transverse
IMA may get bigger
How may occlusion of other mesenteric arteries alter the IMA
IMA and SMA often help each other out and compensate/collateral when the other is stenosed
Describe the relationship between the IMA and SMA in the case of stenosis
Left have of the transverse colon, descending colon, sigmoid colon, rectum (so basically the last half of the transverse colon to the end of the system)
What does the IMA supply
False, is usually difficult to image especially in patients with more body fat or gas's
T/F: the IMA is easily and readily visible in most patients
SMA occlusion (helping out the SMA as a collateral)
What may an easy visibility of the IMA possible suggest
Normal take off of the IMA
What does this image show
Asymptomatic
What is the usual presentation of splanchnic arterial occlusion
There are multiple routes for collateralization so when one artery gets stenosed, the section of bowel that it was supplying can usually get its blood supply easily from another artery
Describe why most splanchnic arterial occlusions are often asymptomatic
≥ 70% stenosis in at least 2 out of the 3 arteries that make up the mesenteric arteries before symptoms even occur
Describe the severity of mesenteric arterial disease that is usually present before symptoms occur
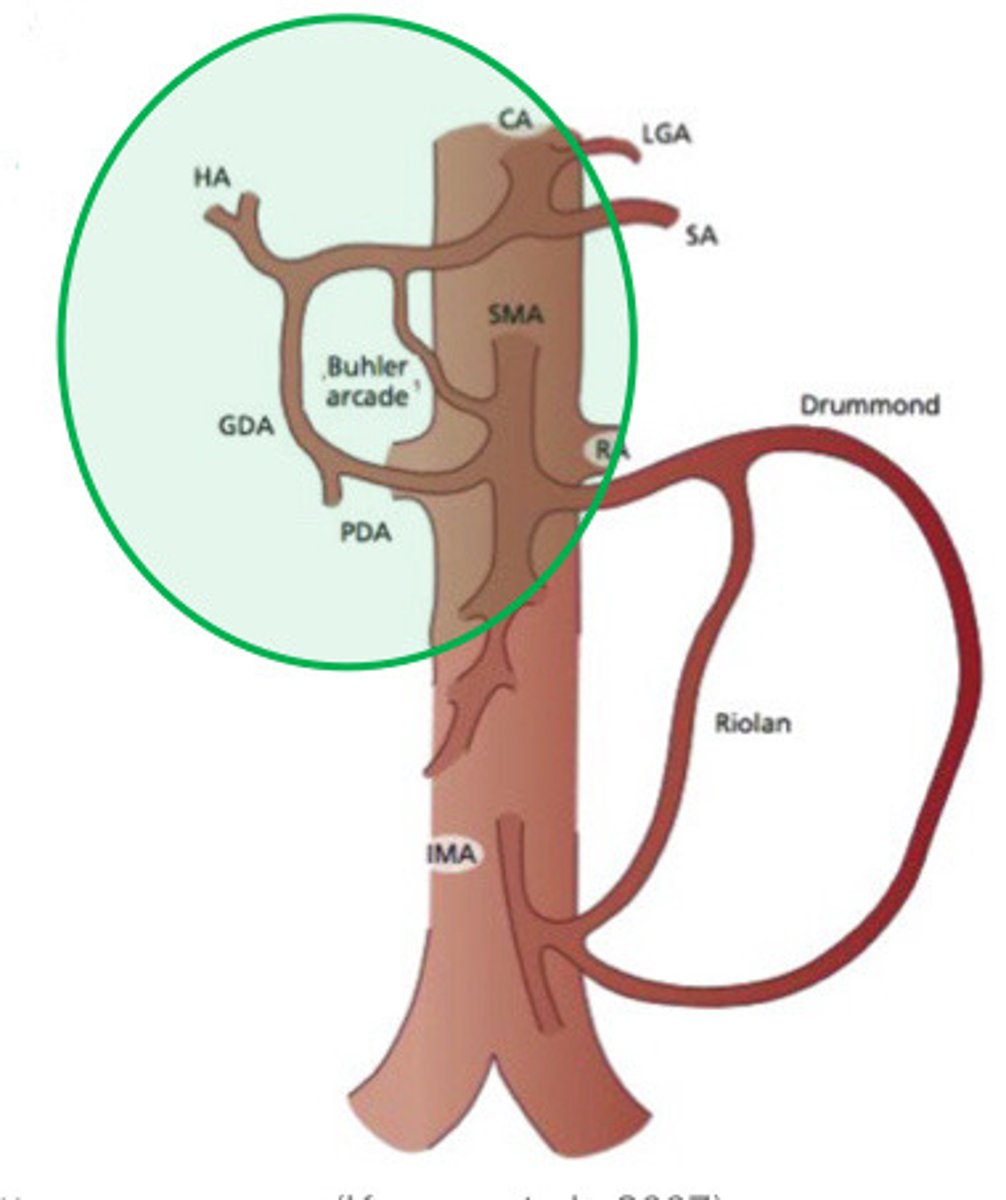
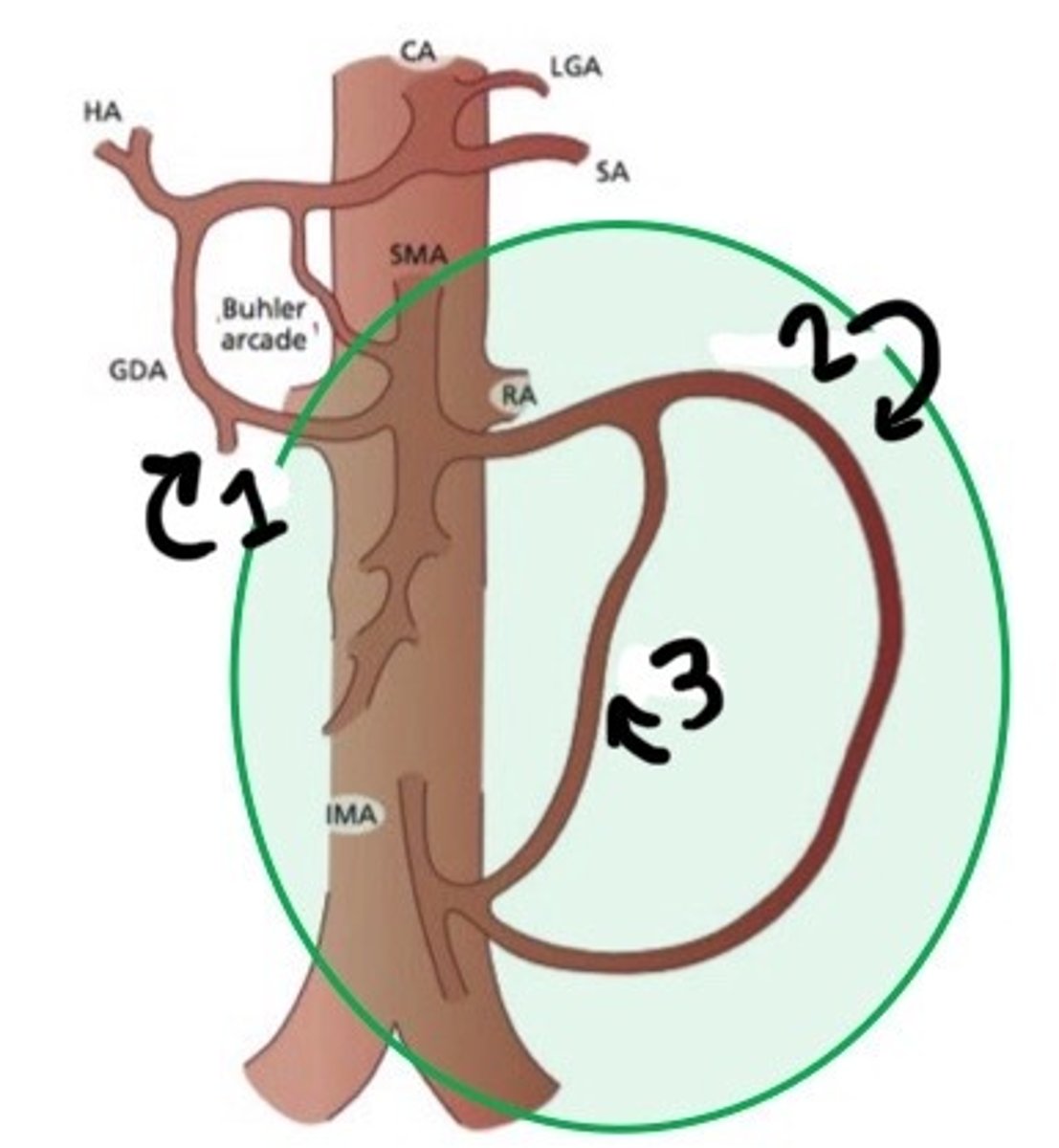
Collateral route that links the CA and SMA via arterial branches that surround the duodenum and pancreas
What is the pancreaticoduodenal aracade
Pancreaticoduodenal aracade
Collaterals between the CA and SMA, think:
Pancreaticoduodenal arcade
What is the green circle indicating
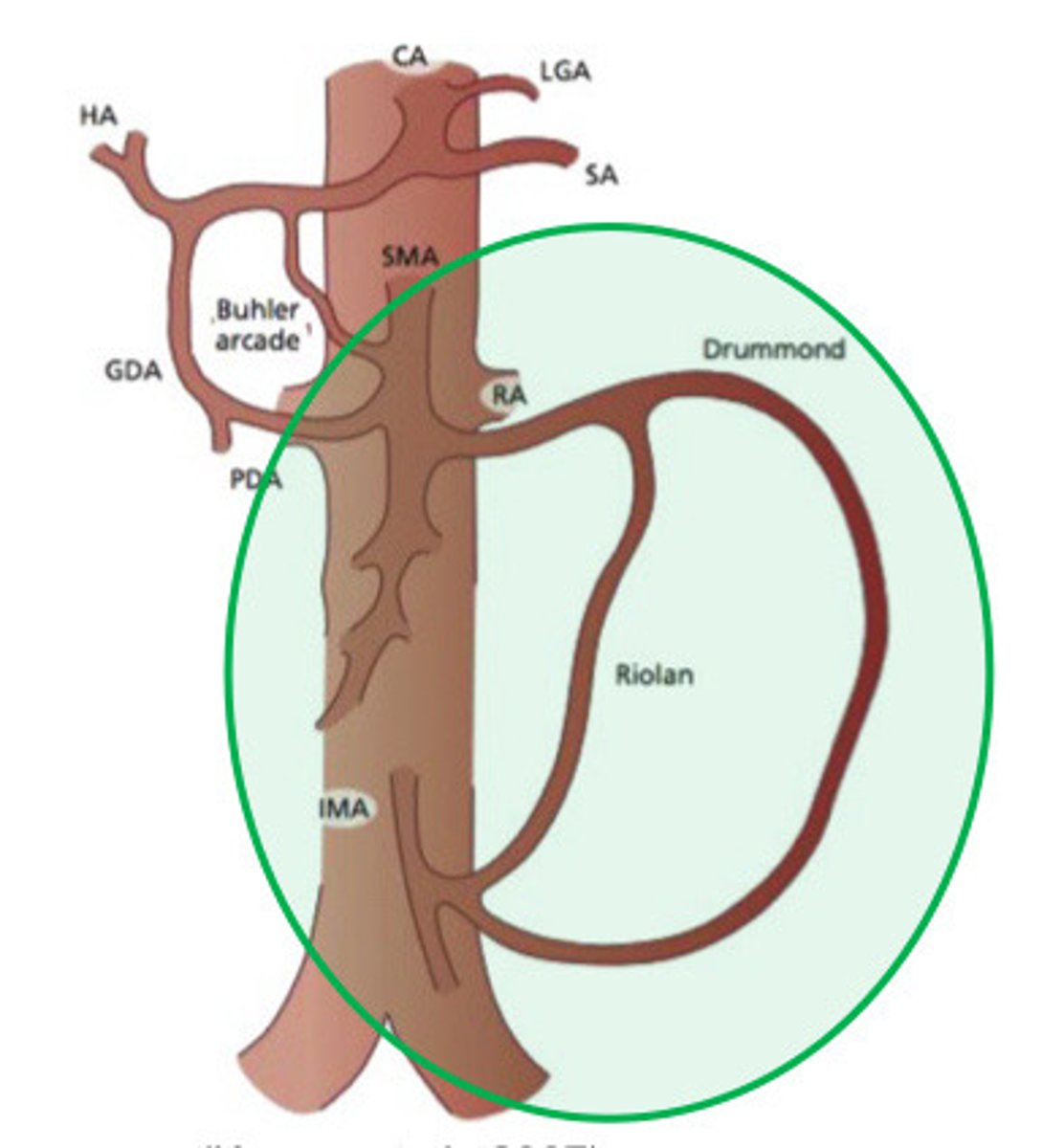
Arc of roiled and marginal artery of Drummond
What are two major collateral pathway that form between the SMA and IMA
Links the IMA and SMA via mesenteric arterial branches
What does the arc of riolan and the marginal artery of Drummond do
Left colic-middle artery
What is a common artery that is used as a collateral between the SMA and IMA
Arc of riolan and marginal artery of Drummond (collateral between SMA and IMA)
What is the green circle indicating
Pancreaticoduodenal arcade
What is 1
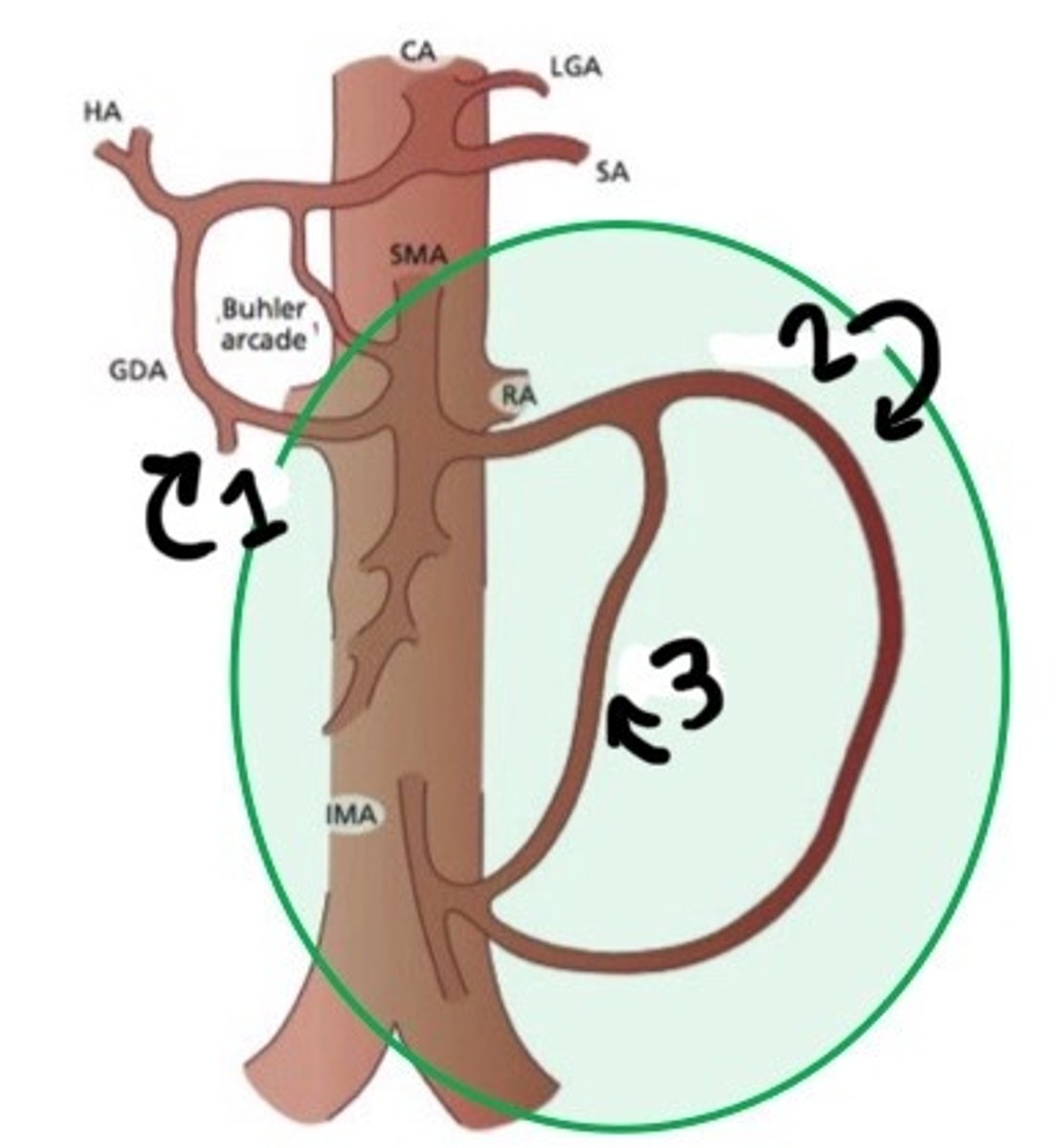
Marginal artery of Drummond
What is 2
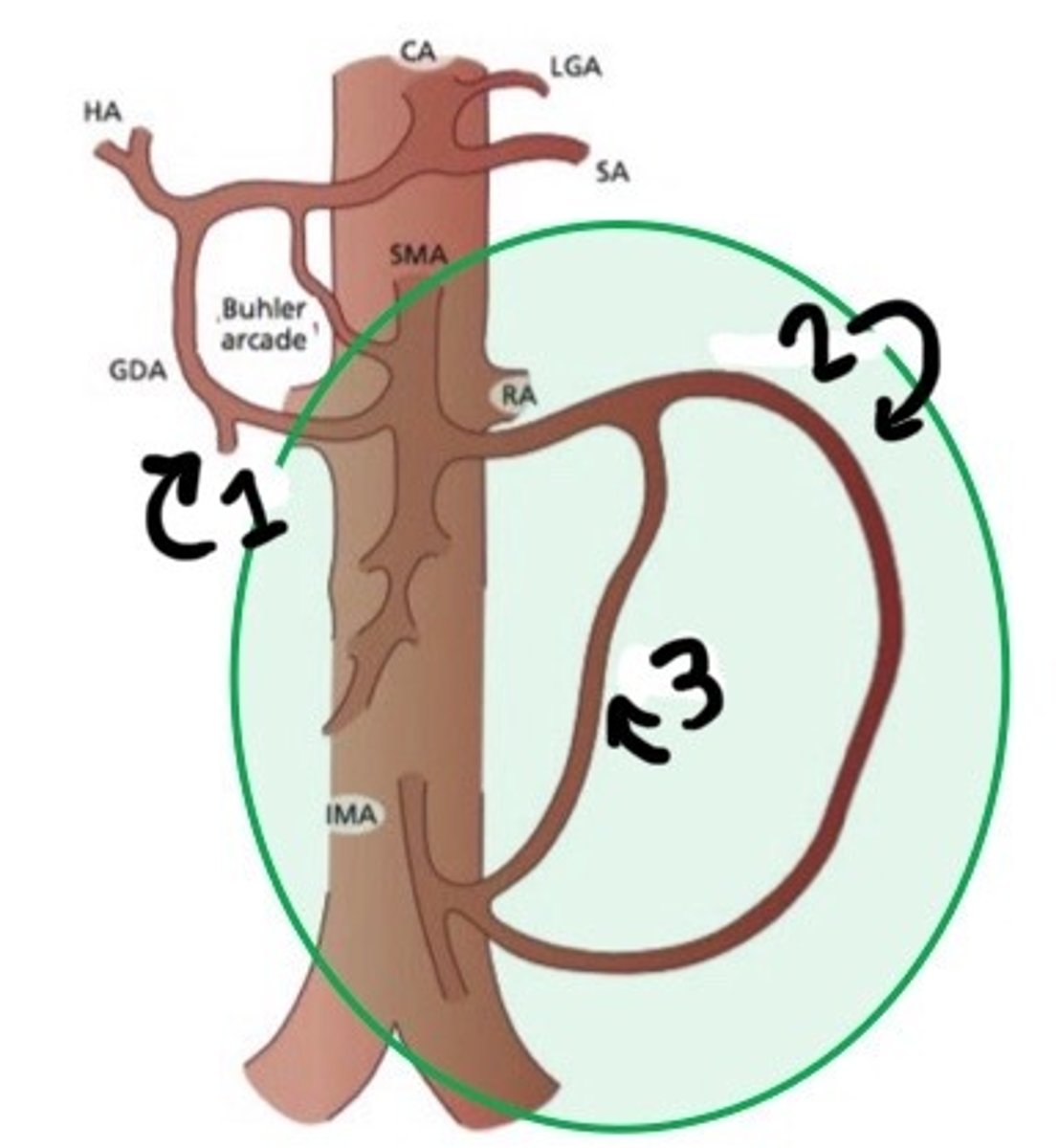
Arc of riolan
What is 3
Chronic mesenteric ischemia
What does CMI stand for
Median arcuate ligament syndrome
What does MALS stand for
suspected CMI, MALS, undergone prior mesenteric intervention
What are the 3 indications for a duplex assessment
Suspected CMI or MALS
What are the 2 main indications for a duplex assessment of the mesenteric arteries
Stents, bypass grafts, etc
What are some examples of prior mesenteric intervention that may need to be evaluated with ultrasound
Aneurysm, atherosclerosis, dissection
What are some other things that may not be the reason the physician ordered the ultrasound assessment, but may be encountered when we are assessing the mesenteric arteries
Bowel is not getting enough blood flow bc too much blockage (would probably be 2/3-3/3 of the splanchnic arteries occluded)
What is mesenteric ischemia
Uncommon
How common is mesenteric ischemia
Due to the multiple potential collaterals, bowel can usually get blood elsewhere when an artery is occluded
Why is mesenteric ischemia uncommon
Acute events
What is usually the cause of mesenteric ischemia
Embolization, thrombosis
What are some examples of acute events that may lead to mesenteric ischemia
Hypotension, small vessel disease, venous obstruction, plaque
What are some other possible, but less common, causes of mesenteric ischemia
Excercise stress test
How do we assess the Mesentery
False! We will NOT get the patient to actually exercise, it will just be assessing them pre and post prandially
T/F: when we assess the Mesentery, we implicate an exercise stress test in which the patient will walk on a treadmill until a THR is reached and then we will assess the affects this has on the bowel. The reasoning behind this is that an increased heart rate will lead to the body not delivering a lot of blood to the bowel
Acute or chronic
What are the two types of mesenteric stenosis or occ lions
Arteriography
What is the gold standard for diagnosis stenoses in the mesenteric artereis
Fasting state
Is mesenteric stenosis or occlusion assessed when the patient is in a fasting or post prandial state
Aorta
What other vessel will be assess in the case of mesenteric stenosis/occluions
The 3 main mesenteric arteries branch directly off of the aorta, so we will be able to see if there is anything from the aorta that is affecting the mesenteric vessels or perhaps there is a thrombus here (since thormbus most commonly occurs at anastomoses)
Why will we look at the aorta before we dive into assessing the mesenteric vessels
Aortic narrowing, aneurysmal, maybe even dissection
What are some aortic pathology that may affect the mesenteric vessels and be causing the problems
Mesenteric vessels pretty hard to see in the average patient due to bowel gas
Why is ultrasound really not the best in assessing mesenteric stenosis or occlusion
≥70%
What is considered a clinically significant stenosis in the mesenteric vesses
≥200cm/s
What PSV of the celiac axis would indicate a stenosis of at least 70%
≥275cm/s
What PSV of the SMA would indicate a stenosis of at least 70%
No PSV parameters (mostly due to it not easily visualized)
What PSV of the IMA would indicate a stenosis of at least 70%
≥3.5
What CA/SMA/IMA PSV: Ao PSV ratio indicate a stenosis of at least 70%
Retrograde common hepatic artery flow
What would be a supporting finding of specially a SEVERE CA stenosis or occluions
CHA will have retrograde flow in order to come back and supply the left gastric and splenic arteries. It is practically acting as the CA when the CA is SEVERLY stenosed (potentially occluded)
Explain why retrograde flow in the common hepatic artery may be seen with severe celiac axis stenosis
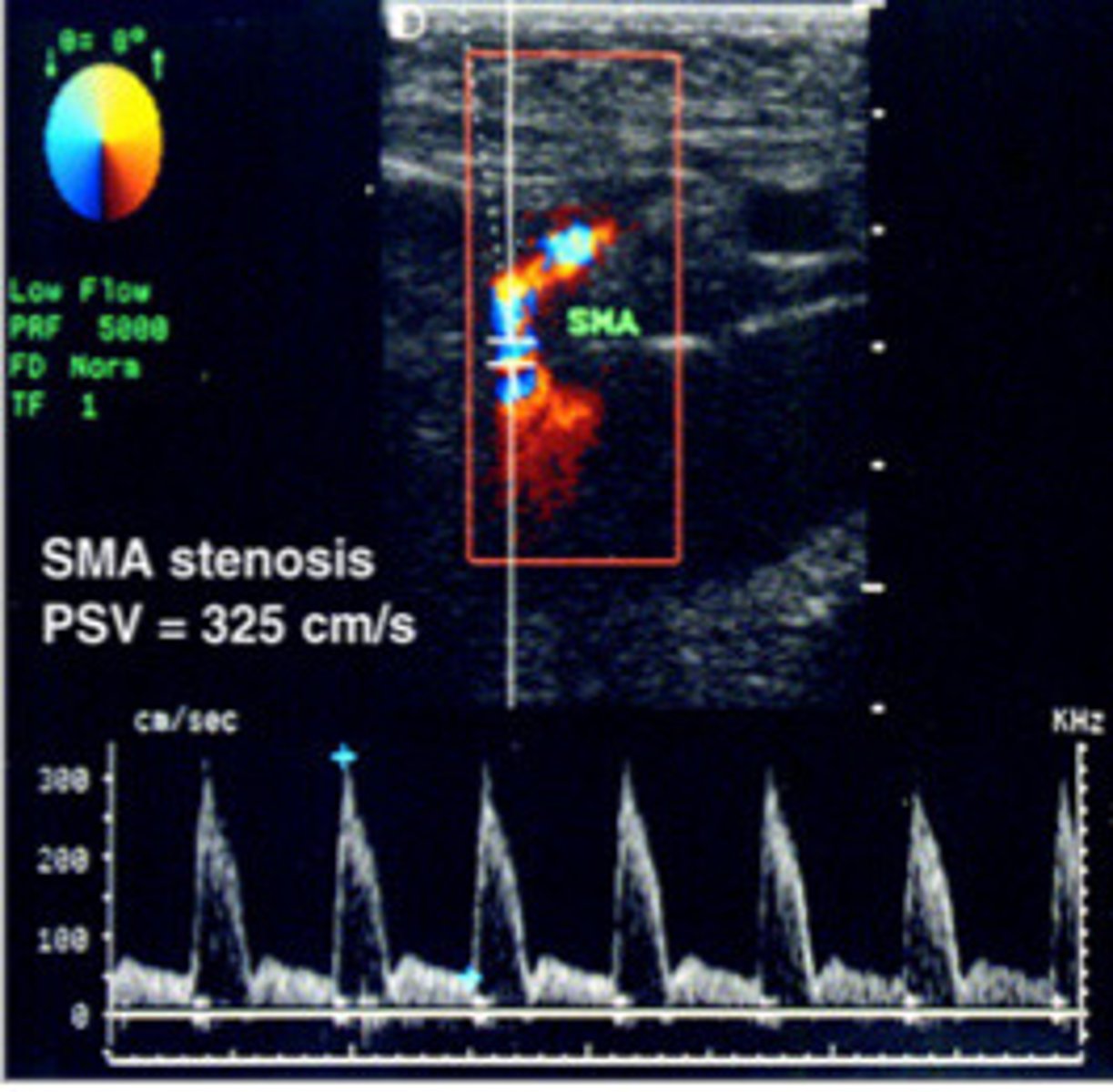
SMA stenosis (note that the PSV is 325cm/s which is higher than our PSV of ≥275cm/s that indicates a stenosis)
What does this image show
Post-prandial pain, patient will get so much pain after they eat that they are practically scared to eat
What is a major symptom of chronic mesenteric ischemia seen in patients
Post-prandial pain, weight loss, bloating, diarrhea, anything really that indicates bowel function is thrown off
What are all the possible symptoms of chronic mesenteric ischemia
Smoking
What habit may increase the risk of chronic mesenteric ischemia
Women that are over 60 y/o (females>males)
What patients is chronic mesenteric ischemia seen in at an increased frequency
Angiography
What is the gold standard modality for chronic mesenteric ischemia
True
T/F: although angiography is the gold standard for a diagnosis of CMI, modalities such as MRA, CTA, and duplex ultrasound are becoming better and more popular in the diagnosis
Scanned pre and post=prandially, study is repeated 20-30min after a high caloric liquid meal
Describe the sonographic assessment of chronic mesenteric ischeia
High resistance
What should the resistance be like in a normla fasting state
20-30min OR once pt is symptomatic (ex/starts experiencing pain)
What are the guidlines for when the study is repeated after the pt has a high-caloric liquid meal
Compare them together
How do we use the pre and post prandially study
SMA
Which mesenteric artery will you most likely see the most difference in the waveforms between the pre and post prandial studies
High resistance
Describe the normal waveform during fasting state
Lower resistance, PSV pretty much doubled and ESV pretty much tripled (compared to the pre-prandial waveform)
Describe the normal waveform post-prandial
Low resistance and high velocities (which is the OPPOSITE of what is should be in a fasting patient)
Describe the characteristics of an abnormal SMA waveform in a fasting patient that would already be diagnostic (you wouldn't need to do the post prandial assessment)
Velocities still high
Describe the abnormal post prandial waveform