Mod 3: Inflammation and Healing
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
Resolution
Minimal tissue damage; cells recover and return to normal within a short period of time.
Regeneration
Occurs in damaged tissue in cells that are capable of mitosis; damaged tissue is replaced with identical tissue generated by the proliferation of nearby cells.
Replacement
Functional tissue replaced by scar tissue (loss of function).
Primary Intention
Secondary Intention
Wound is free of foreign objects; edges are held close together, and a minimal gap between them. (surgical incisions)
Large break in tissue, which is more inflamed and takes a longer healing process; more scar tissue. (compound fracture)
Factors Affecting Health
Promoting healing: Youth, Good nutrition, no infection, adequate hemoglobin. Delaying healing: Aging, anemia, circulatory problems, infection, excessive mobility.
Complications Affecting Scar Formation:
Loss of Function results from:
Contractures & Obstructions:
Adhesions:
Hypertrophic scar tissue:
Ulceration:
1. results from loss of normal cells and lack of normal organization in scar tissue
2. scar tissue is nonelastic/shrinks so this may restrict ROM and deformity
3. prevent normal movement of structures and cause distortion or twisting of tissue
4. overgrowth of fibrous tissue, which could cause more severe contractures
5. interferes with blood flow in nearby arteries
Healing process:
1. Hemostasis: control bleeding
2. Inflammation
3. Proliferation: Angiogenesis (BV development), granulation, epithelialization, contraction
4. Maturation: Regeneration, Resolution, Scar
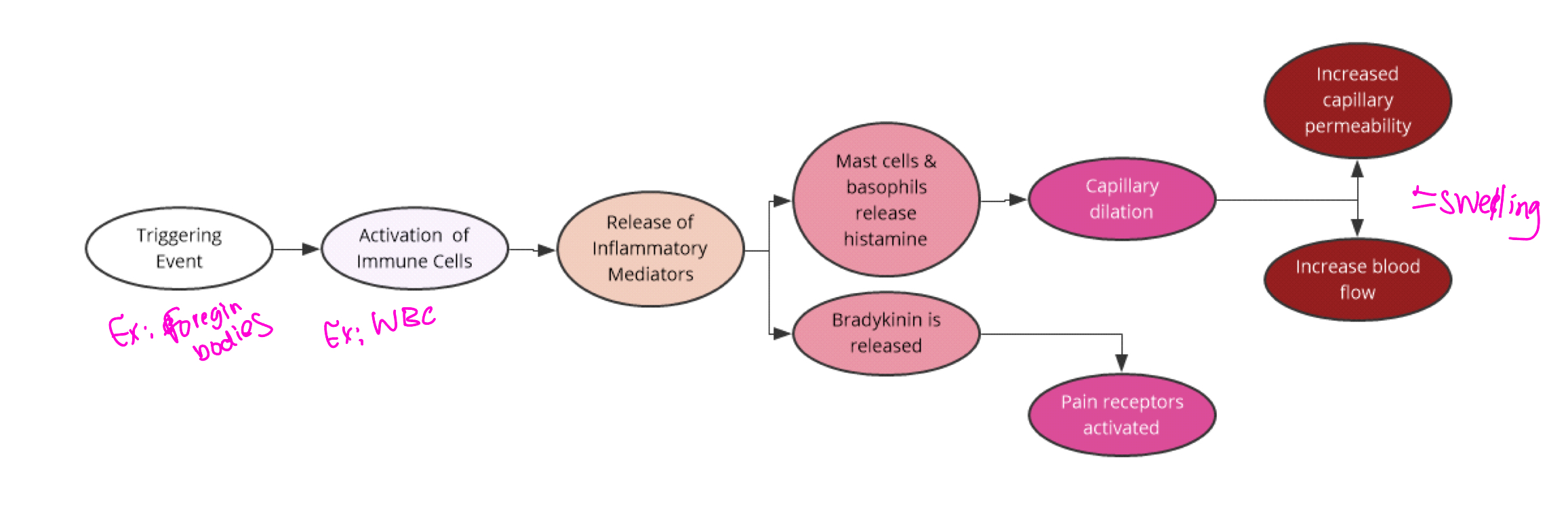
Inflammation
The body's nonspecific response to tissue injury, resulting in redness, swelling, warmth, pain, and sometimes loss of function.
Acute inflammation
cell involved?
Chronic inflammation
cells involved?
Timing of events varies with specific cause; chemical mediators affect blood vessels and nerves in the damaged area.
neutrophils
Follows an acute episode of inflammation with less swelling/exudate. Presence of more lymphocytes, macrophages, and fibroblasts.
What Grows into the gap from nearby connective tissue after foreign materials have been removed (secondary intention)
Granulation Tissue
Causes of inflammation
Direct physical damage, chemicals, ischemia/infarction, allergic reactions, extremes of heat or cold, foreign bodies, infection.
Chemical Mediators:
Histamine causes:
Bradykinin:
Prostaglandins:
Cytokines/Chemokines:
Leukotrienes:
Substances that mediate the inflammatory response.
A chemical mediator released by mast cells that increases blood vessel permeability during inflammation=swelling
A peptide that induces pain and further vasodilation.
A group of lipids that promote inflammation and fever.
generate systemic responses during inflammation
Inflammatory mediators that contribute to bronchoconstriction and increased vascular permeability.
Five Cardinal Signs of Inflammation
- Redness: caused by increased blood flow into the damaged area
- Warmth: caused by increased blood flow into damaged area
- Swelling (edema): caused by the shift of protein and fluid into the interstitial space
- Pain: increased pressure of fluid on nerves and local irritation from mediators like bradykinins
- Loss of function: caused by cells lacking nutrients, or swelling interferes with function
What does mast cells activation results in?
results in releases of granular tissue (histamine) VERY IMPORTANT
OA or RA?
1. Impairs healing?
2. Disrupts healing?
3. Promotes chronic/continuous damage?
4. Pain; localized, secondary inflammation?
5. Pain; chronic inflammation, bilateral?
OA or RA?
1. Impairs healing? OA
2. Disrupts healing? RA
3. Promotes chronic/continuous damage? RA
4. Pain; localized, secondary inflammation? OA
5. Pain; chronic inflammation, bilateral? RA
Systemic Effects of Inflammation
Mild fever (pyrexia), malaise, fatigue, anorexia.
Pyrogens
Fever-producing substances from WBCs.
Course of Fever
Release of pyrogens, reset hypothalamus high, responses include shivering, vasoconstriction, increased heart rate.
Exudate:
- Serous:
- Fibrinous:
- Purulent:
- Hemorrhagic:
A collection of interstitial fluid formed in the inflamed area.
- Serous: Clear, watery (blister fluid)
- Fibrinous: Thick, sticky, ↑risk of scar tissue, chronic inflammation, tough
- Purulent: Pus, dead cells, WBCs, bacteria.
- Hemorrhagic: Blood mixed in, vascular damage.
Labs – Serum
- Leukocytosis:
- Differential count:
- C-reactive protein:
- ESR (erythrocyte sedimentation rate):
Labs – Serum
- Leukocytosis: Elevated WBC count
- Differential count: proportion of each type of WBC altered
- C-reactive protein: Acute inflammation marker
- ESR (erythrocyte sedimentation rate): Chronic inflammation marker
Potential Complications of Inflammation
- Infection: Microorganisms can more easily penetrate, and some resist phagocytosis
- Skeletal muscle spasm: a protective response to pain resulting from injuries such as sprains
- Deep ulcers: from prolonged inflammation, because cell necrosis and lack of cell regeneration cause erosion of tissue
Osteoarthritis vs Rheumatoid Arthritis
- Common sites:
- Etiology:
- Risk factors:
- Patho:
- Pain:
- Swelling:
- Systemic?
- Deformity:
A chronic degenerative joint disorder involving cartilage breakdown.
- Common sites: Synovial joints (hips, spine, knees)
- Etiology: wear and tear, aging, joint stress
- Risk factors: Age, OWO, trauma to joint, repetitive movement
- Patho: Cartilage softens & breaks down due to mechanical stress. Joint space narrows/bone spurs form and synovial inflammation occurs
- Pain: worsens with use
- Swelling: Mild
- Systemic? No
- Deformity: Possible with progression
RA: An autoimmune inflammatory disease targeting the synovial membrane.
- Common sites: small joints (hands, wrists, feet)
- Risk factors: genetics, female gender
- Patho: Immune system attacks synovial lining-> Synovitis-> cartilage erosion joint deformity
- Pain: improves with use
- Swelling: marked, symmetrical
- Systemic? Yes- fatigue, fever, malaise
- Deformity? Common
Healing responses in OA vs RA
Healing in OA involves less inflammation; RA healing is complicated by ongoing inflammation.
Role of inflammation in disease
A key factor in the pathogenesis of various diseases, contributing to tissue damage and dysfunction.
Clinical signs and symptoms of osteoarthritis
Joint pain, stiffness, swelling, and decreased range of motion.
Clinical signs and symptoms of rheumatoid arthritis
Joint pain, swelling, morning stiffness, and systemic symptoms like fatigue.