Electrolyte abnormalities (sodium and potassium)
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
What is pH?
amount of H+ ion in the blood normally between 7.35-7.45
What is PaO2?
partial pressure of oxygen
refers to amount of oxygen dissolved in the blood normally between 11-13kPa
What is PaCO2?
amount of CO2 dissolved in the blood usually between 4.7-6kPa
What is HCO3?
amount of bicarbonate in the blood
usually between 22-26mmol/L
it is excreted and reabsorbed by the kidneys
What is lactate?
end product of anaerobic respiration, usually <2mmol/L
caused by poor oxygenation and tissue perfusion (sepsis, shock, heart failure), or increased oxygen demand (liver/kidney failure)
What does a low blood pH mean?
pH <7.35 indicates acidaemia either due to CO2 retention (as this is acidic), or Hco3 loss (as this is a base)
What does a high blood pH mean?
pH >7.45 indicates alkalaemia due to HCo3 retention, or CO2 loss
How does the acid base system work?
both renal and respiratory systems work together to maintain acid-base balance so when one system fails another may compensate
What is hypernatremia?
high sodium concentration >146mmol/L
What are causes of hypovolemic hypernatremia with high concentrated urine?
severe dehydration, eg: poor oral intake, diarrhoea, vomiting, diuretics
What are causes of euvolemic hypernatremia with normal urine?
mild dehydration. eg: poor oral intake, diarrhoea, vomiting, diuretics
What are causes of hypovolemic hypernatremia with dilute urine?
diabetes insipidus
What are causes of hypervolemic hypernatremia with dilute urine?
sodium gain, eg: excess IV fluids
hypervolemia can be recognised through peripheral oedema
What are risk factors for hypernatremia?
water loss
diabetes insipidus
sodium gain
How does hypernatremia present?
fatigue
weakness
confusion
seizures
thirst
How are sodium levels controlled?
through the action of aldosterone on the DCT and collecting duct to increase sodium reabsorption from the urine
natriuretic peptides: ANP, BNP, CNP contribute to sodium homeostasis by reducing sodium reabsorption from the DCT and inhibiting renin
What investigations are done for hypernatremia?
U&Es showing high NA+, high urea, high albumin
urine osmolarity
How is hypernatremia managed?
treat underlying cause
give water orally if possible
IV fluids using 5% dextrose, o.18% NaCL
use 0.9% if hypovolaemic as it causes less marked fluid shifts and is hypotonic in a hypertonic patient
What is hyponatremia?
low serum sodium <133mmol/L
plasma Na+ depends on both sodium and water, so hyponatremia doesn’t necessarily mean sodium depletion
What are risk factors for hyponatremia?
increasing age, hospitalisation, diuretics, SSRIs, anti-psychotics, carbamazepine, heart failure, kidney/liver disease, endocrine disorders
How does hyponatremia present?
nausea, vomiting, lethargy, headache, muscle cramps, weakness, confusion, seizures, reduced Glasgow Coma Scale score
What investigations can be done for hyponatremia?
U&Es
TFTs, cortisol levels, LFTs, nt-proBNP
plasma osmolarity
fluid status, urine osmolarity, urine sodium
How is true hyponatremia determined?
measure serum osmolarity
low plasma osmolarity <275mOsmol/kg is true hyponatremia
normal plasma osmolarity may indicate pseudohyponatremia caused by high serum lipids or proteins
high plasma osmolarity >295mOsmol’kg may be caused by hyperglycaemia
How is hyponatremia managed?
avoid rapid correction to prevent osmotic demyelination syndrome (central pontine demyelination)
correct underlying cause
hypovolaemic hyponatremia: IV fluids with 0.9% may be given under supervision
hypervolaemic hyponatremia: fluid restriction
vasopressor receptor antagonists promote water excretion without loss of electrolytes
emergency- hypertonic (1.8%) saline can be given undersupervisiom
What causes hypovolemic hyponatremia with high urine sodium?
occurs when there is fluid and sodium loss due to renal causes:
primary adrenal insufficiency
renal/cerebral salt wasting
What causes hypovolemic hyponatremia with low urine sodium?
occurs when there is fluid and sodium loss due to extrarenal causes:#
vomiting and diarrhoea
third spacing
What causes euvolemic hyponatremia with high urine sodium?
occurs when there is normal sodium in the body but increased fluid which dilutes the sodium
SIADH
secondary adrenal insufficiency
hypothyroidism
What causes euvolemic hyponatremia with low urine sodium?
primary polydipsia
What causes hypervolemic hyponatremia with low urine sodium?
occurs when there is increased fluid and sodium retention, but more fluid than sodium
heart failure
liver cirrhosis
nephrotic syndrome
What is hyperkalaemia?
high serum potassium >5.5mmol/L
potassium >6.5mmol/L is a potential emergency and needs urgent assessment
What are renal causes of hyperkalaemia?
AKE, drugs, CKS, renal tubular acidosis
What are tissue breakdown causes of hyperkalaemia?
rhabdomyolysis
tumour lysis
haemolysis
What are endocrine causes of hyperkalaemia?
DKA
Addison’s
metabolic acidosis
What is pseudo-hyperkalaemia?
raised potassium due to lysis of RBCs (most commonly due to prolonged transit time to the lab or a difficult venepuncture)
What are symptoms of hyperkalaemia?
fast irregular pulse
chest pain
weakness
light headedness
palpitations
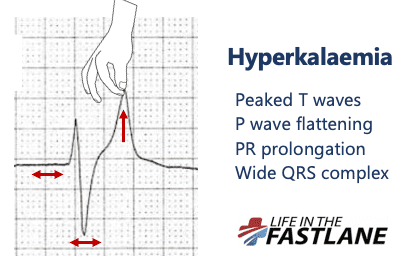
What are ECG changes in hyperkalaemia?
PR prolongation
flattened or absent P waves
tall, tented T waves
wide QRS >0.12s
ventricular tachycardia
bradycardia
sine wave appearance
cardiac arrest
Why does hyperkalaemia affect the heart?
Potassium is the most abundant intracellular cation (positively charged ion) in the body. The intracellular concentration is around 20 times greater than in the extracellular fluid, resulting in a large concentration gradient. This maintains the excitability of nerve and muscle cells.
Hyperkalaemia results in progressive conduction problems, as it lessons the concentration gradient
What drugs can cause hyperkalaemia?
Potassium-sparing diuretics (e.g. amiloride)
Aldosterone antagonists (e.g. spironolactone)
Angiontensin converting enzyme inhibitors (e.g. ramipril)
Angiotensin-II receptor antagonists (e.g. losartan)
Non-steroidal anti-inflammatory drugs (e.g. ibuprofen)
Heparin
How is mild hyperkalaemia (5.5-5.9) managed?
treat cause
remove potassium from the body (calcium resonium or sodium polystyrene sulfonate)
What is calcium resonium?
binds to K+ in the gut preventing absorption and bringing K+ levels down over a few days
How is moderate (6-6.4) hyperkalaemia managed?
cardiac monitoring
shift potassium into cells with glucose/insulin
remove potassium from the body (calcium resonium or sodium polystyrene sulfonate)
How is severe hyperkalaemia (>6.5) managed?
seek expert help and set up cardiac monitoring
cardioprotection: 10ml of 10% calcium chloride IV over 5 minutes
shift potassium into cells with glucose/insulin: 10units short acting insulin with 25g glucose IV over 30 minutes
shift potassium into cells with salbutamol 10-20mg
remove potassium from the body, renal replacement therapy may be indicated if underlying pathology cannot be corrected
What is hypokalaemia?
low serum potassium <3.5mmol/L
<2.5mmol/L requires urgent treatment
What are causes of hypokalaemia?
decreased intake: poor diet, malabsorption
increased loss: GI (diarrhoea), renal (tubular disorders)
endocrine: Cushing’s, hyperaldosteronism
drugs
What medications can cause hypokalaemia?
diuretics
laxatives
steroids
insulin
beta-2 agonists
aminoglycosides (gentamicin)
How does hypokalaemia present?
fatigue
weakness, hypotonia, hyporeflexia
muscle pain
constipation
ascending paralysis
palpitations
tetany (involuntary muscle contractions)
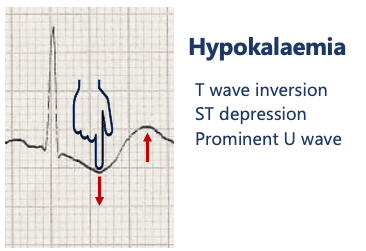
What ECG changes are present in hypokalaemia?
u waves
t wave flattening
ST depression
long PR interval
arrhythmias
What may blood investigations show for hypokalaemia?
hypokalaemia
hypomagnesemia
How is mild hypokalaemia (3-3.5) managed?
oral K+ supplement
treat underlying cause
monitor K+
How is severe hypokalaemia (<2.5) managed?
seek expert advice
cardiac monitoring
IV potassium chloride cautiously (max rate 20mmol/hour, max concentration 40mmol/L) NEVER GIVE A BOLUS
treat underlying cause
monitor K+ every 3 hours