HYMS B9, W4
1/121
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
122 Terms
active vs passive immunity
Active = individual has memory cells - can make their own antibodies & provides long term immunity
Passive = person given antibodies, these work then die, no long term immunity, no memory cells.
Give examples of infections for which vaccination is a successful strategy.
- in 2017, the UK had reached elimination status with measles via vaccination
- in 2018, emergence of more strains and cases means the WHO could no longer consider the UK to have 'eliminated' measles.
what process is an essential feature of an acquired immune response against a pathogen?
clonal expansion
name types of vaccines + an example
1 - Live Attenuated Vaccines - weakened version of living bacteria or virus. e.g. MMR
2 - Inactivated Vaccines - killed version of pathogen. e.g. polio, hep A, rabies
3 - Subunit, Recombinant, Polysaccharide, and Conjugate Vaccines - use specific pieces of the pathogen (such as protein, sugar, or a casing). e.g. HPV, Hib, shingles.
4 - Toxoid Vaccines - safe version of the bacteria toxin. e.g. tetanus.
5 - Messenger RNA (mRNA) Vaccines - e.g. Pfizer-BioNTech and Moderna COVID-19 vaccines.
6 - Viral Vector Vaccines - virus is modified to contain the genetic material of the pathogen. e.g. Oxford-AstraZeneca's COVID-19 vaccine and the Johnson & Johnson's Janssen COVID-19 vaccine.
what are some of the methods of delivering a vaccine?
- intramuscular
- subcutaneous (under skin but above muscle)
- transdermal (in dermis of skin)
- oral
- nasal (a spray)
- intranasal (similar to nasal spray but in a droplet form)
- jet injection (instead of needle)
- patches
- implantable devices
- aerosol
what is an adjuvant?
an ingredient used in some vaccines that helps create a stronger immune response in people receiving the vaccine.
some examples:
- Lipid nanoparticles (LNPs) inCOVID-19 mRNA vaccines
- AS04 (aluminum hydroxide andmonophosphoryl lipid A) in HepBand HPV vaccine
- AS03 (squalene-based) in H1N1vaccines
- MF59 (squalene) in flu vaccines
Why could smallpox be eradicated by vaccination?
- diseases causes distinct symptoms (=facilitated rapid intervention and containment)
- Only one dominant variant
- vaccine was effective at inducing sterile immunity (no carriers remain)
- No animal reservoir
- Vaccination was coupled with active surveillance and containment
Are fungi prokaryotic or eukaryotic?
Eukaryotic
describe the epidemiology of infectious fungi
250,000 species
1500 new species discovered annually
1000 or so pathogenic to humans
12 or so colonise humans
why are most fungi described as saprophytes?
most fungi live on dead or decaying organic matter.
why do fungi act as secondary pathogens to humans?
- No fungi are primary pathogens of humans ie main survival technique is not though harming the host
- However, humans are sometimes accidental hosts for saprophytic fungi. this makes them secondary or opportunist pathogens (in vulnerable or immunocompromised patients)
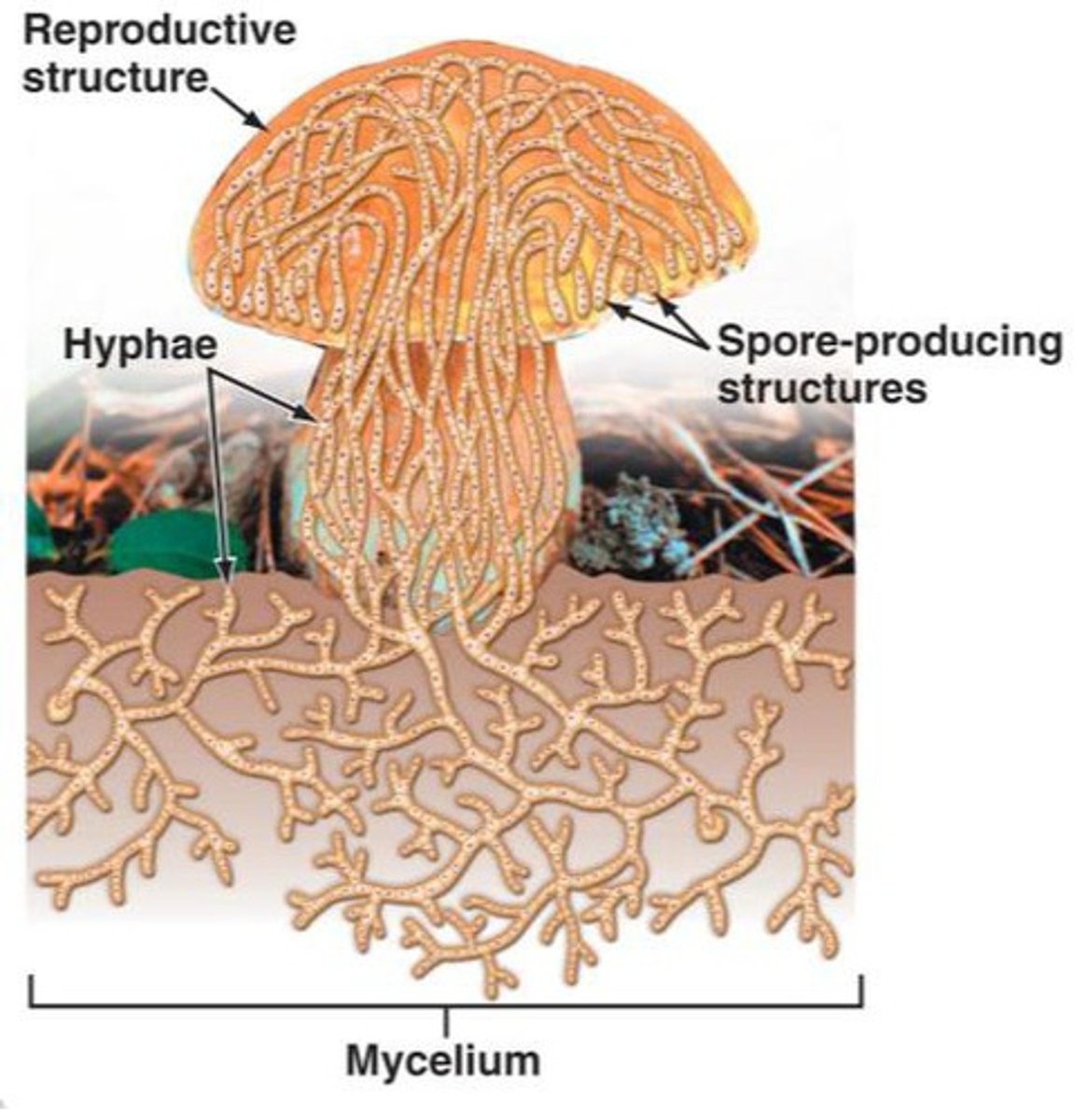
describe the general structure + features of a fungi
- Eukaryotes
- Can be multicellular
- Cell wall containing chitin
- DNA on several chromosomes
- Distinct nucleus
- Cytoplasm has membrane-bound organelles
- 80S ribosomes
- Reproduction may be sexual or asexual
why are fungal infections rare in humans?
- Saprophytes are not well adapted to growth at 37°C
- Their enzymatic pathways function most efficiently at redox potentials found in non-living substrates
- Poorly adapted to using human nutrients
- Host defence mechanisms are efficient at dealing with inhaled/ingested fungi
- Slow growing
- Don't need to - highly successful in environment
what are the main three types of fungi that cause infection in humans?
Moulds
Yeast
Dimorphic (fungi that have a yeast (or yeast-like) phase and a mold (filamentous) phase)
how does mould grow?
- Growth by formation of filaments (called hyphae)
- Entangled mass of hyphae forms a mycelium which can be visible to the naked eye
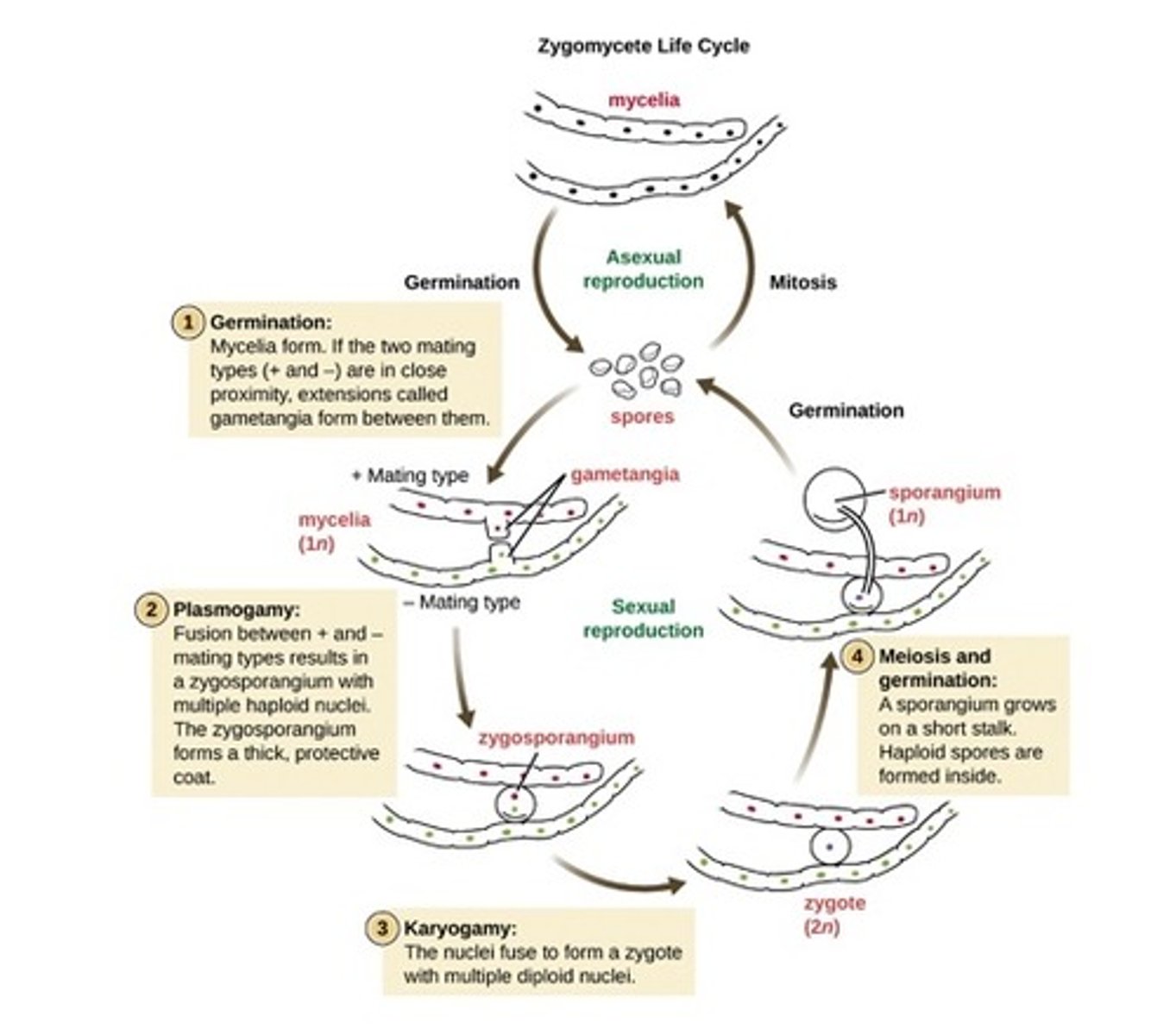
how does mould reproduce?
- Asexually - conidia (aka asexual spores) are on aerial hyphae. they detach when mature.
- Sexual - + and - hyphal tips fuse nuclei to form a sexual spore.
name a species of mould that can cause human disease
Aspergillus
usually affects the respiratory system
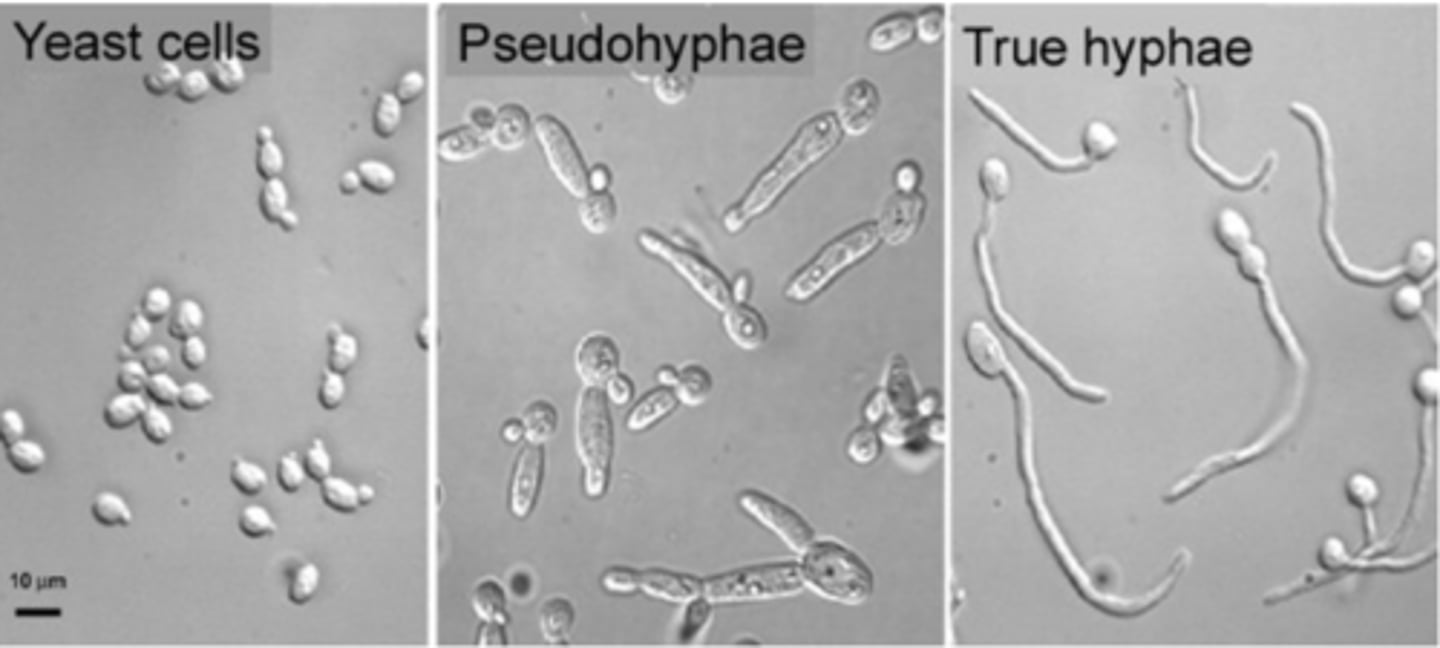
describe the shape of yeast
Single-cell organisms
Round or ovoid
how does yeast reproduce?
asexually by budding
name two pathogenic yeasts that affect humans
Candida species
Cryptococcus neoformans (cryptococcosis is a rare infection commonly associated with immunosuppressive individuals)
how is Candida albicans diagnosed under microscope?
Formation of true hyphae (aka 'germ tube' formation)
pseudohyphae vs true hyphae (yeast)
the width of pseudohyphae cells is always larger than the hyphal cells
what are dimorphic fungi?
Fungi that can exist in yeast form and mold form
non of them are endemic in the UK
name a dimorphic fungi
Coccidiodes immitis (coccidiodomycoses)
outline the non-infectious clinical signs of a fungal infection
- Mycotoxins are released by some moulds (such a ergotism)
- Hypersensitivity
- Asthma
- Farmer's lung
general feeling of being unwell is called...
malaise
mycosis meaning
a disease caused by infection with a fungus
what fungal species causes pityriasis versicolor?
Malassezia furfur

what is superficial mycoses?
- a superficial cosmetic fungal infections of the skin or hair shaft.
- No living tissue is invaded
- No cellular response from the host. Essentially no pathological changes are elicited.
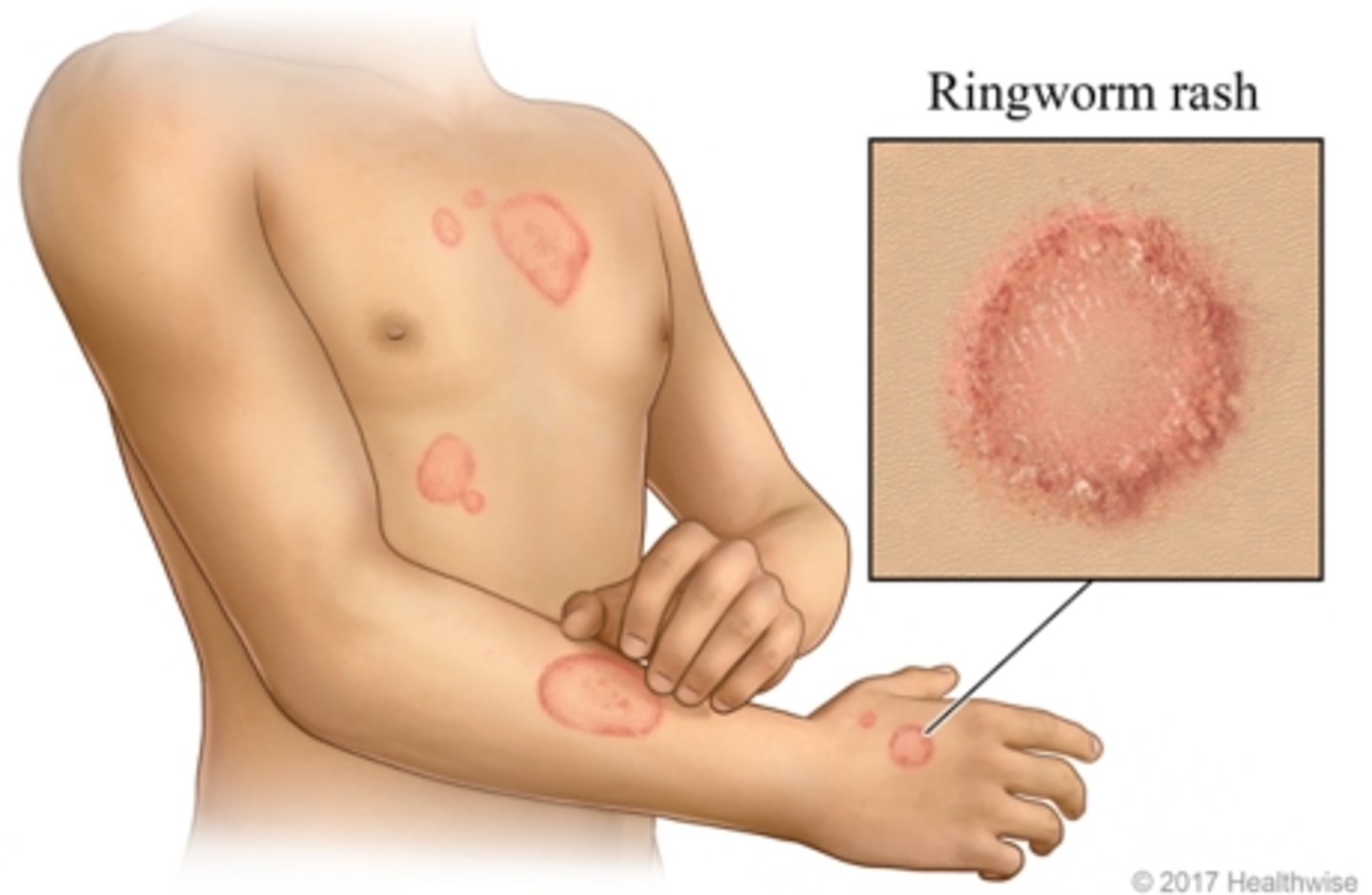
what is dermatophytosis? what is also known as?
- a fungal infection of the hair, skin, or nails caused by a dermatophyte.
- all dermatophytes feed on keratin
- type of superficial mycoses
- also known as ringworm or tinea
describe a ringworm rash
- not itchy
- can be anywhere besides elbows and knees
- circular 'ring' with raised borders and a clear centre
Anthropophilic fungi meaning
one of the three types of dermatophytoses (superficial mycoses). the other two are Geophilic and Zoophilic.
Anthropophilic fungi are in contact with humans and are the only fungi which require humans for survival
what type of fungal infection causes brittle, discoloured nails (usually toes)?
Tinea unguis (aka onychomycosis)
Caused by Trichophyton rubrum [anthropophilic fungi]
![<p>Tinea unguis (aka onychomycosis)</p><p>Caused by Trichophyton rubrum [anthropophilic fungi]</p>](https://knowt-user-attachments.s3.amazonaws.com/3ec99cc5-11da-425e-a8cf-6540f7658afd.jpg)
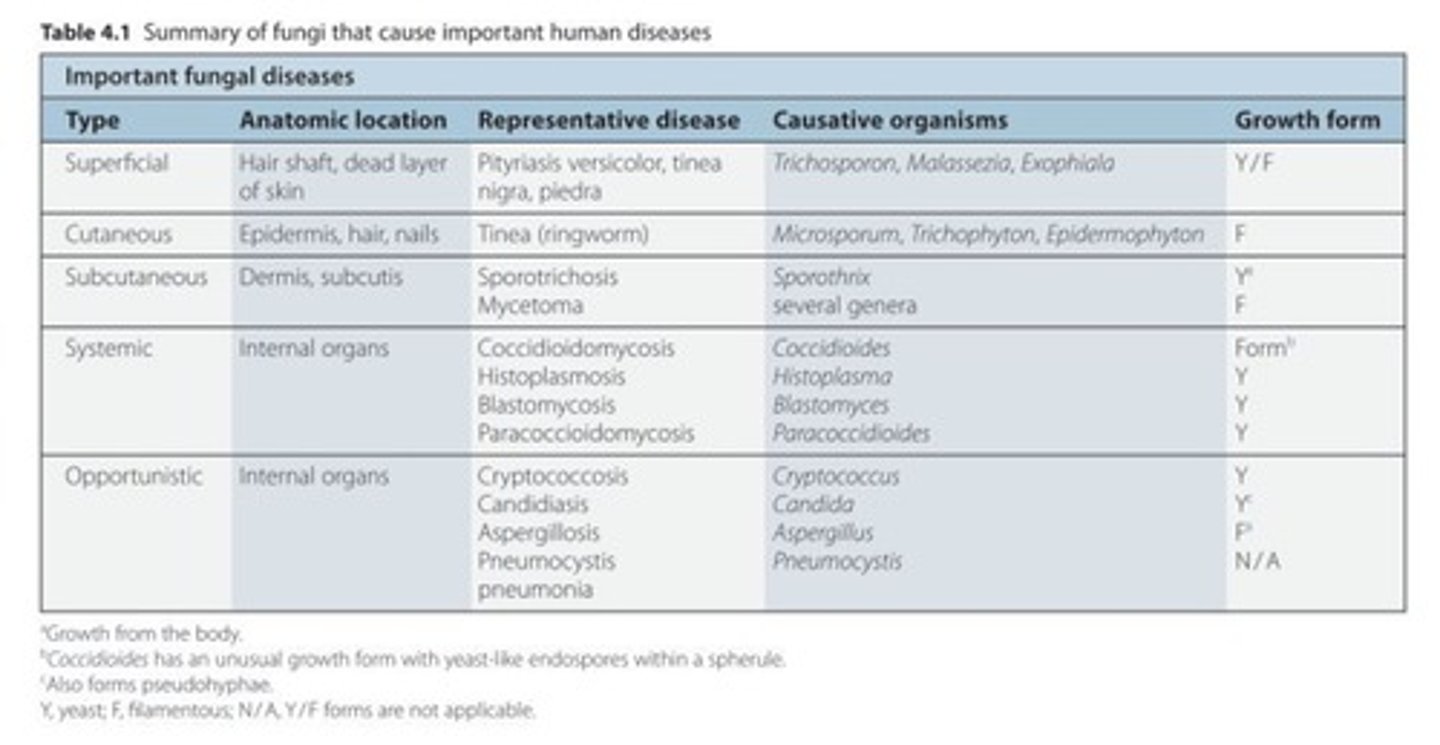
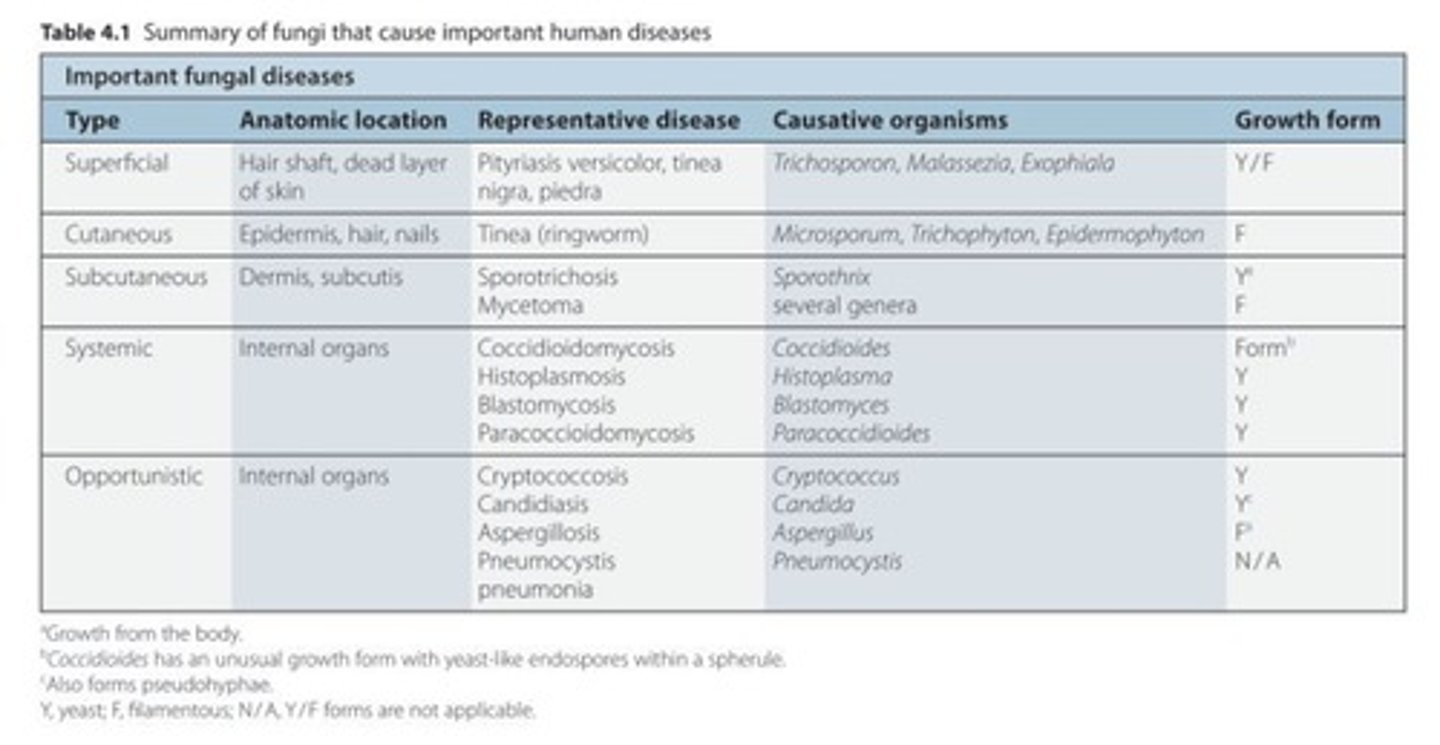
how are fungal infections classified?
Mycoses are classified as superficial, cutaneous, subcutaneous, or systemic (deep) infections depending on the type and degree of tissue involvement and the host response to the pathogen.
what is a subcutaneous mycoses?
- fungal infection beneath the skin (dermis and subcutis)
- follows traumatic inoculation
- usually seen in tropics/sub-tropics
- chronic infection which can be locally invasive and involve bone

what is a deep / systemic mycoses?
affects internal organs
what problems can candida cause?
- Oesophagitis
- Candidaemia (candida in the blood)
- Endocarditis
- Hepatosplenic candidiasis
how can yeast infections be diagnosed?
- Microscopy of e.g. abscess aspirate
- Grows slowly on normal culture plates
- 'sterile blood cultures' (Diagnosis is confirmed by cultures from normally sterile sites)
- PCR
- Antigen tests: B glucan
risk factors for systemic candidiasis
use of central venous catheters
exposure to broad-spectrum antibiotics
neutropenia
how are moulds diagnosed?
- Seen mainly in tissue
- Grows very slowly on culture plates - extended culture
- Does not grow in blood culture
- There is no PCR test for it
- Antigen tests: gallactomanan
how is deep mycoses usually acquired?
through inhalation of spores (found in soil)
chronic lung infection may develop and disease may also disseminate to other organs
name a dymorphic fungi that causes a deep mycoses. where is this found?
- Coccidioidomycosis
- found in south western USA
- Spores inhaled
- Immunosuppression increases risk but not essential
- Causes respiratory and flu symptoms mainly, and a maculopapular rash
- causes nodules/cavities/fibrosis and chronic lung damage
name a toxic antifungal drug
- Amphotericin
- expected renal damage and causes chills/fever during course
- Lipid-associated formulations much less toxic so higher dose can be given
name a broad spectrum antifungal
Amphotericin
amphotericin mechanism of action
binds to ergosterol in the fungal cell membrane, which leads to the formation of pores, ion leakage and ultimately fungal cell death.
-azoles mechanism of action
All act by inhibiting lanosterol demethylase: interrupt ergosterol biosynthesis, the primary sterol in the fungal cell membrane.
The depletion of ergosterol alters the fluidity of the cell membrane and alters the action of the membrane-associated enzymes.
Caspofungin class
Echinocandins
an antifungal
which fungi are becoming more resistant to Caspofungin?
Cryptococci
Dermatophytes
both of these are ALWAYS resistant
caspofungin indications
Invasive aspergillosis
Invasive candidal infections
caspofungin mechanism of action
Inhibits glucan synthase (inhibits cell wall synthesis)
which plasmodium species is the most virulent to humans?
Plasmodium falciparum
what makes a good anti-parasite drug?
1. Selective toxicity to parasites
2. Target many species and life stages
3. Cost effective
4. Easy to administer/ distribute
5. Unlikely to develop resistance
how do anti-helminthic agents generally work/target?
- current drugs mostly targeted to non-proliferating adult organisms.
- neuromuscular coordination (needed for feeding movements, location of the worm within the host)
- carbohydrate metabolism (major source of energy)
- microtubular integrity (needed for egg laying and hatching, larval development, glucose transport, enzyme activity and secretion)
how do anti-protozoa agents generally work/target?
- targeted at relatively rapid proliferating, young, growing cells.
- Nucleic acid synthesis
- Protein synthesis
- Specific metabolic pathways (e.g., folate metabolism)
- Detoxification mechanisms
diagnosis of malaria
blood smear (microscopy)
or Rapid Diagnostic Test
these should both be supported by the quality assurance test
what causes a fever in malaria ?
Rupture of RBC by schizont to release merozoites
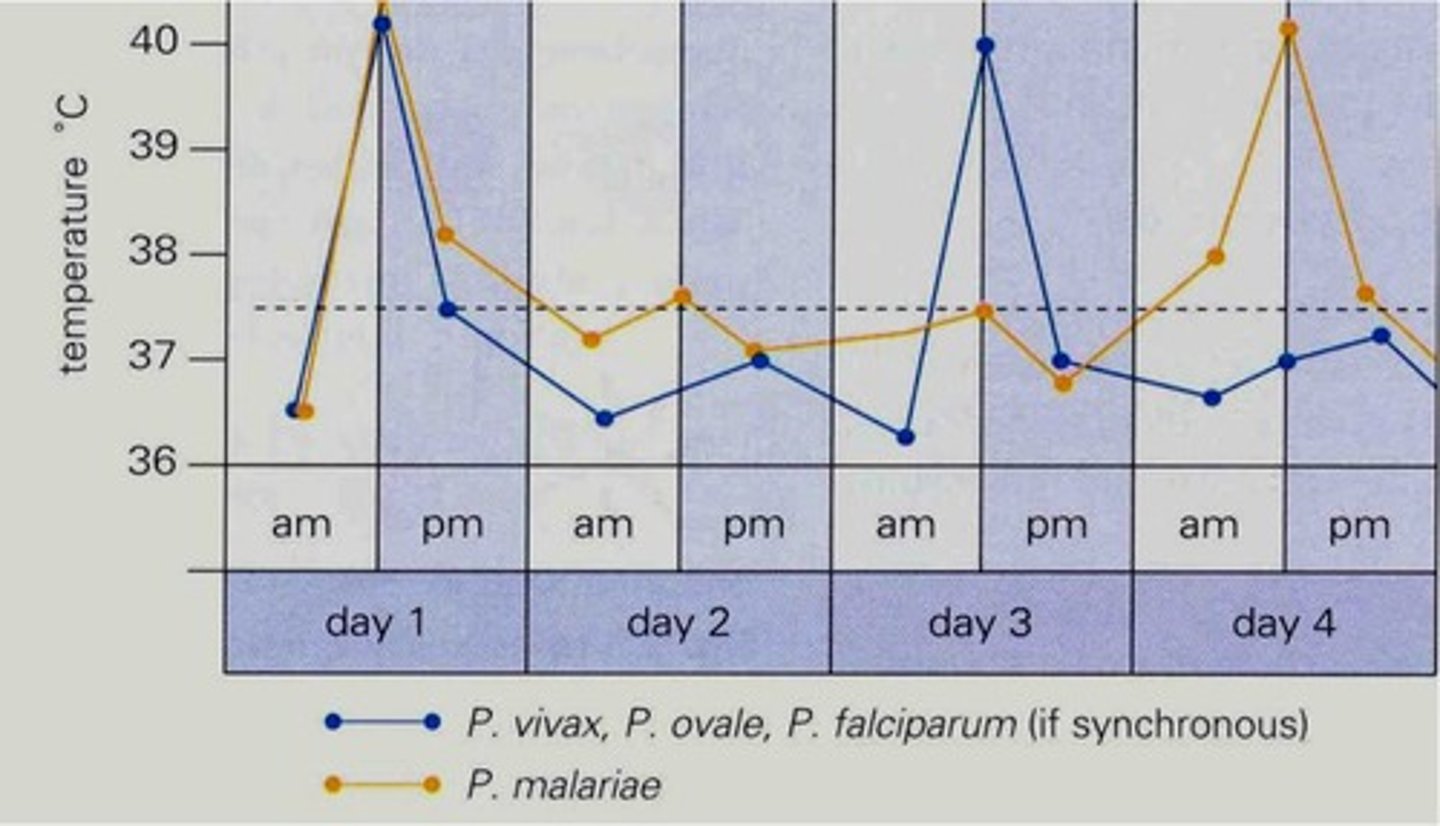
What is tertian malaria?
- A brood of schizonts matures every 48 hr, so the periodicity of fever is tertian (“tertian malaria”)
- happens in P vivax and P ovale malaria
Quartan malaria
72 hour fever cycle
occurs with P malariae
describe the fever frequency in malaria
tertian - 48 hrs
quartan - 72 hrs
fever cycles
sequestration in malaria
- the adherence of infected erythrocytes containing late developmental stages of the parasite (trophozoites and schizonts) to the endothelium of capillaries and venules
- characteristic of Plasmodium falciparum infections.
- can happen in the brain, spleen, lungs, skin, heart, GIT
which 3 drug classes are used in malaria chemotherapy?
Quinolines
Anti-folates
Artemisinin compounds (newer)
these are usually used in combination to prevent resistance.
Artemisinin compounds mechanism of action
Interacts with Heme-Iron. Generation of free radicals that alkylate and oxidize proteins and lipids within infected red blood cells
African trypanosomiasis vector
tsetse fly
what is South American Trypanosomiasis also known as?
Chagas disease
a protozoa
South american trypanosomiasis vector
triatomine bug ("kissing bugs")
Other routes of infection (congenital transmission,blood transfusion, feces contaminated food, etc.)
what is African Trypanosomiasis also known as?
sleeping sickness
a protozoa
Leishmaniases vector
femalephle botomine sandflies
focal areas of more than 90 countries in thetropics, subtropics, and southern Europe- from rain forests to deserts.
diseases caused by Leishmaniasis
- may be asymptomatic
- Cutaneous leishmaniasis (causes skin sores)
- Visceral leishmaniasis (kala-azar)
- Others: Mucosal leishmaniasis
what disease does Toxoplasma gondi cause?
Toxoplasmosis
Mild lymphadeopathy in adults
Complications in immunocompromised individuals
Serious HIV-associated opportunist
Congenital toxoplasmosis - abortion, hydrocephalus
medication for Toxoplasmosis
Anti-folates
Entamoeba histolytica causes what disease?
Amoebiasis
can be asymptomatic
diarrheal illness + liver abscess
can be intestinal & extraintestinal infections
worldwide distribution
Giardia lamblia causes what disease?
Giardiasis
diarrheal illness
worldwide distribution
Trichomonas vaginalis causes what disease?
Trichomoniasis
genital infection; sexuallytransmitted
worldwide distribution
Amoebiasis, Giardiasis and Trichomoniasis drugs treatment
Metronidazole
Tinidazole
name some protozoa (7)
1. Trypanosomiasis (african = sleeping sickness); (south american = Chagas disease)
2. Leishmaniases
3. Toxoplasmosis
4. Amoebiasis
5. Giardiasis
6. Trichomoniasis
7. malaria
what is the main difference between protozoa and helminths?
Protozoa are single-celled organisms, while helminths are multicellular animals.
Protozoa are members of the kingdom Protista, while helminths are members of the kingdom Animalia.
name three types of helminths
Tapeworms: Cestodes
Flukes: Trematodes
Round worms: Nematodes
What is a Helmith?
parasitic worm
How can helminths be transmitted?
1. swallowing infective eggs or larvae via faecal-oral route.
2. swallowing infected larvae in the tissues of another host.
3. active penetration of the skin by larval stages.
4. the bite of an infected blood-sucking insect vector.
what serious infection can flukes cause?
- Schistosomiasis, also known as bilharzia
- Although the worms that cause schistosomiasis are not found in the United States, people are infected worldwide.
- second mostly impactful parasitic disease (to malaria)
Hookworm, ascaris, whipworm, onchocerciasis, dracunculiasis and lymphatic filariasis are all types of what?
Round worms: Nematodes
Echinococcosis and Taeniasis are types of what?
Tapeworms: Cestodes
how is Taeniasis acquired?
Eating raw or undercooked beef (T. saginata) or pork (T. solium and T. asiatica).
complications of taenuasis infection?
Taenia solium tapeworm infections can lead to cysticercosis, which is a disease that can cause seizures, so it is important seek treatment.
name two arthropods
scabies
nits/lice
transmission of scabies
direct, prolonged, skin-to-skin contact with a person who has scabies.
scabies symptoms
The microscopic scabies mite burrows into the upper layer of the skin where it lives and lays its eggs. The most common symptoms of scabies are intense itching and a pimple-like skin rash.

what is the term for the signs and symptoms that occur with cancer, not directly caused by the tumour itself?
Paraneoplastic syndrome
It is generally immune (autoantibody or T cell mediated) or hormone mediated
Examples of paraneoplastic syndromes
Cachexia
Neurological: pretty much anything
Skin: various rashes
Endocrine: calcium, Cushing, carcinoid
Haematological: abnormal blood counts, thrombosis
what are some ways cancer is classified?
1. Organ of origin
2. Tissue of origin
3. Benign versus malignant
4. Degree of differentiation
5. (Genomic/biomarker features)
what is the difference between a benign and malignant tumour?
Benign: basement membrane intact, no spread
Malignant: basement membrane breached, potential for cancer cells to spread. Some (but not all) benign tumours progress to malignant tumours
adenoma
a benign tumor that arises in or resembles glandular tissue (epithelial tissue)
carcinoma
a malignant (cancerous) tumor that occurs in epithelial tissue
how are muscle & connective tissue tumours described?
Benign tumour = -oma e.g. fibroma
Malignant tumour = sarcoma e.g. fibrosarcoma
what is a teratoma?
Embryological tumours containing all 3 germ layers. Usually arise in gonads and can be benign or malignant. It is very rare.
what is hamartoma?
Disorganised tissue overgrowth
Benign- 1-3 germ layers
May be part of a genetic syndrome eg Cowden's
what is an anaplastic carcinoma?
Undifferentiated (anaplastic) carcinoma is a variant of ductal adenocarcinoma in which there is a loss of glandular differentiation and tumor cells display large, polygonal to spindled, often bizarre (anaplastic) and multinucleated features.
poor differentiation of cells in a tumour usually indicates... (more/less aggressive cancer)
high grade cancer
aggressive
what does the grade of cancer refer to?
degree of differentiation
what does the stage of cancer refer to?
degree of spread around the body