Week 4 - Sutures, Fluids, Surgical Site Infections
1/129
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
130 Terms
Sutures should be a minimum of ___________ from the wound edge and _____________ apart. .
- 5 mm and 5 mm
- Note: It depends on the tissues requiring approximation. For an equine linea alba, it is optimal to start 15 mm from the wound edge, while for a canine linea alba, 5 mm is optimal.
When considering suture placement and the distance to put between sutures, what is the goal?
- Maximum wound holding with minimal interruption of blood supply
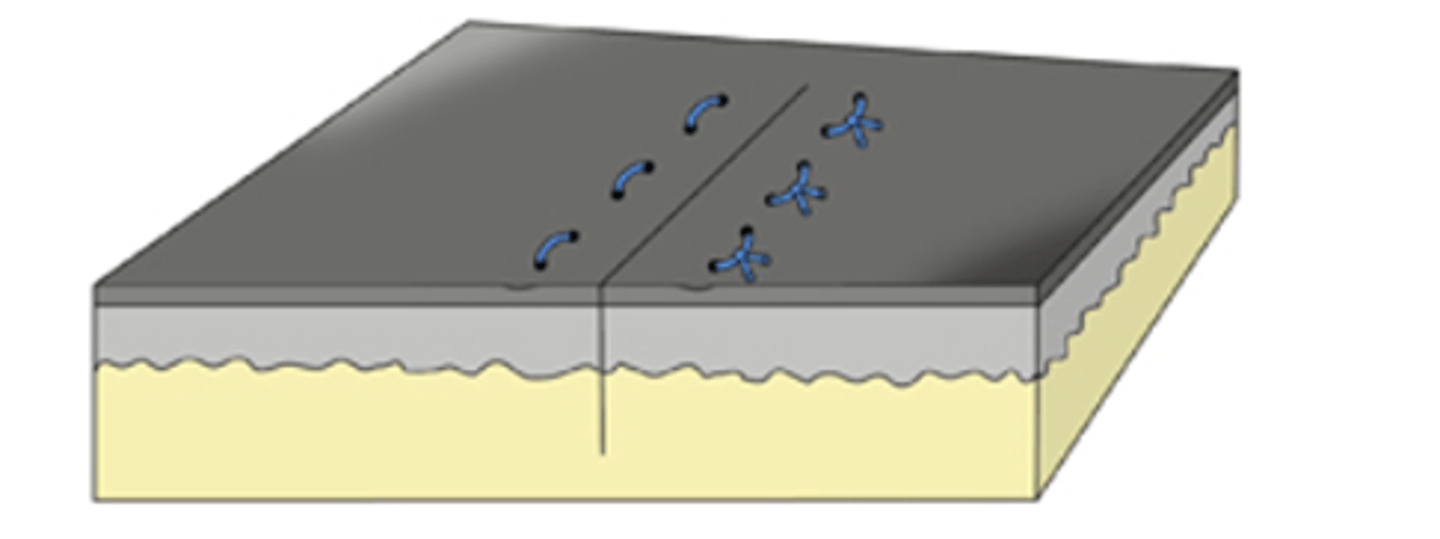
How does one create a buried knot?
- First suture bite deep (deep to dermis in subcutis) to superficial on the near side
- Second suture pass superficial to deep on the far side
- Two ends are tied, pulled parallel to the incision to bury the throw
What are some advantages of the simple interrupted suture pattern?
- Ease and accuracy of placement, useful for non-linear incisions (i.e. limb amputation)
- Adjustable tension
- Loss of knot less disastrous
- Strength
- Tissue mobility
What are some disadvantages of the simple interrupted suture pattern?
- Time requirement
- Material (And associated cost)
What is a continuous suture pattern?
- Series of connected suture passages with one knot at each end of the suture line
What are some advantages of a continuous suture pattern?
- Speed
- Less suture material
- Ease of removal
- Distributes force evenly, may be stronger (as long as you use even tension)
What are some disadvantages of a continuous suture pattern?
- The loss of a knot or suture breakage is more disastrous
Suture is only as strong as the _____________.
- Knots
Describe appositional tissue approximation.
- Opposes the edges of the incision, resulting faster wound healing and is more cosmetic
Describe inverting tissue approximation.
- The edges of the incision roll inwards.
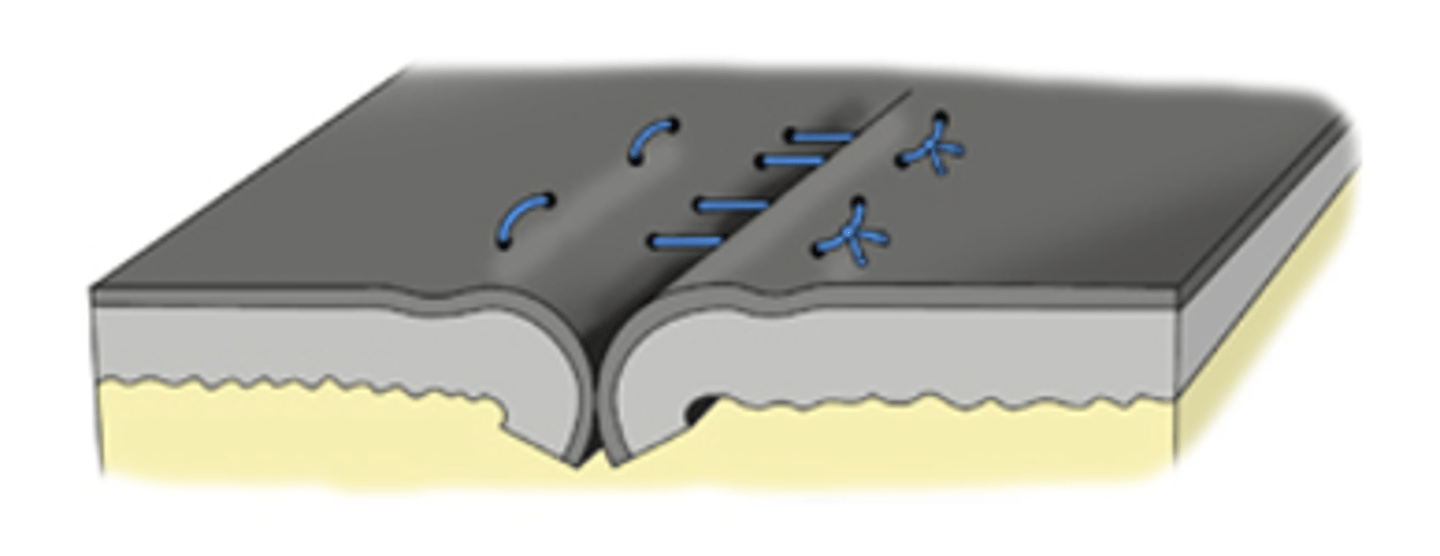
Describe everting tissue approximation.
- The edges of the incision roll outwards
What is a clinical use of everting tissue approximation?
- Used in exotics with scales -> Allows them to shed their skin
What are some advantages of a simple interrupted suture pattern?
- Widely used and versatile (skin/fascia/bowel/mucosa)
- Provides secure anatomic closure
- Precise suture tension possible
- Easily applied
Excessive tension when placing simple interrupted sutures can result in...
- Skin edge eversion (avoid)
What are some advantages of a simple continuous suture pattern?
- Saves time and promotes suture economy
- Good apposition and airtight or watertight seal
What are some applications of a simple continuous suture pattern?
- Good for layers under low tension
- Organs that heal fast or tissues that don't "do" much (subQ, fascia, bladder, stomach)
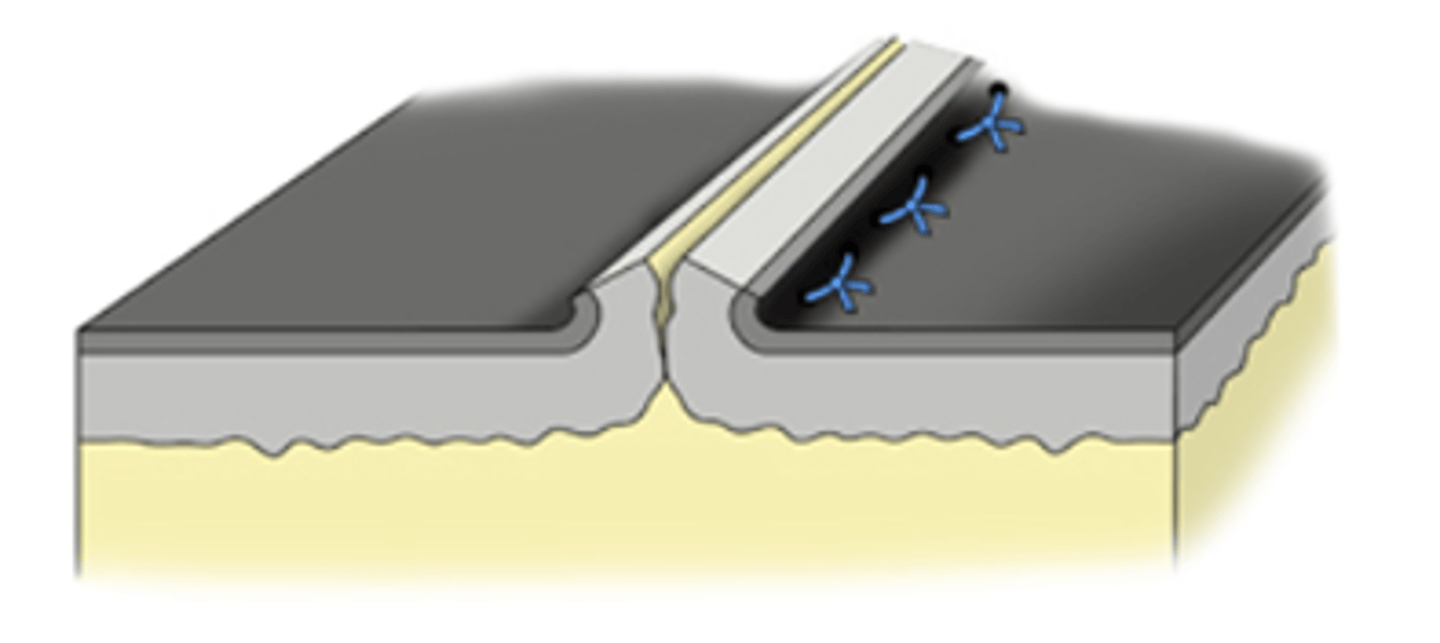
What is another name for the intradermal suture pattern?
- Subcuticular (used interchangeably)
What is the most common clinical use of the intradermal/subcuticular suture pattern?
- Skin closure (avoids external skin sutures)
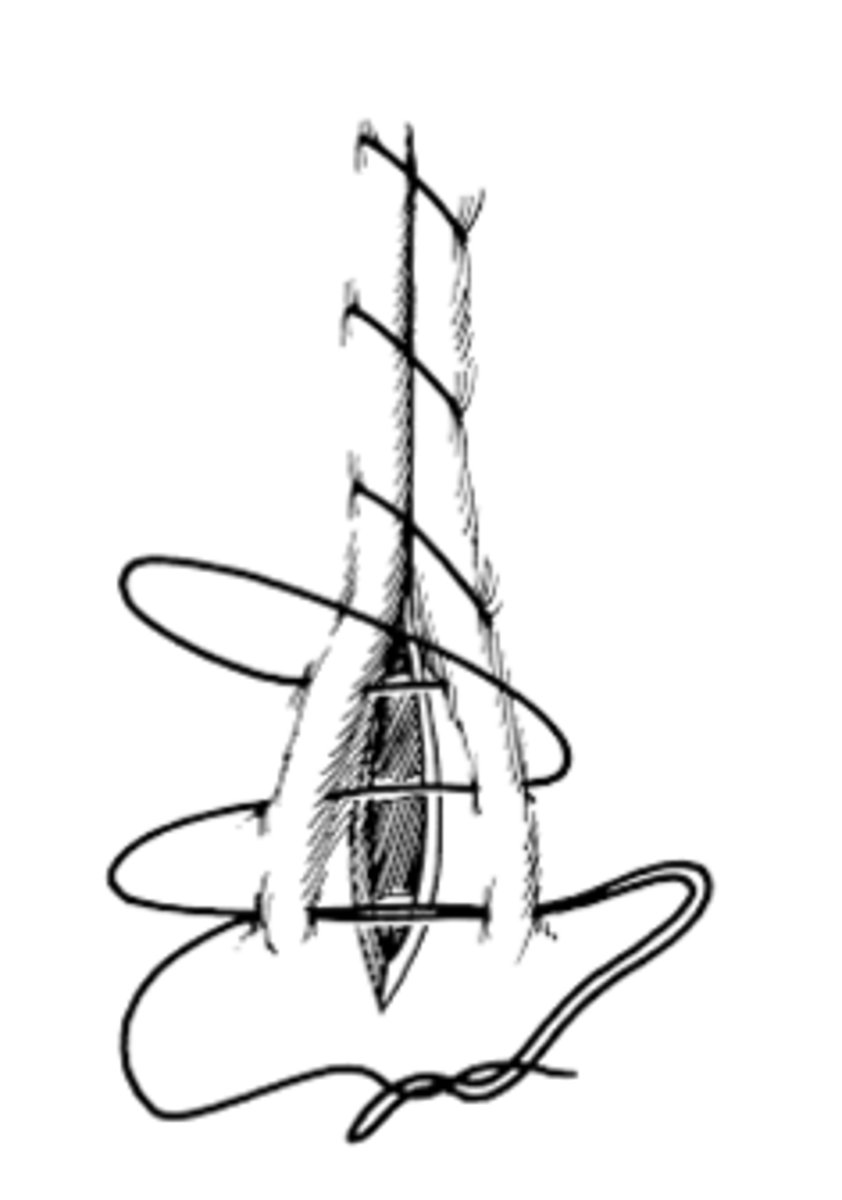
The cruciate suture pattern is a series of two simple interrupted bites tied together in which the external portion forms an X. This forms a ___________ suture which is ___________ relieving.
- Mattress
- Tension
What are the advantages of a cruciate suture pattern?
- Resists tension
- Prevents eversion
What are some clinical uses of the cruciate suture pattern?
- Skin
- Non-linear incisions (e.g., amputation)
- Body wall closure
- Linea alba closure in spay/neuter
The ford interlocking suture pattern is a modified version of the ___________________ pattern and is more commonly used in the skin of large or small animals?
- Simple continuous
- Large animals
What is the holding layer of visceral organs?
- Submucosa (sustains tension, need to bite through it with suture in order for the organ to heal)
The gambee is an interrupted or continuous suture pattern? Where is it used?
- Interrupted
- Used in hollow viscous (organs/intestines)
How is a gambee suture performed?
- Bite on each side passes into serosa, through muscularis and submucosa, mucosa, into lumen, then passes back through mucosa, submucosa and muscularis on the same side
How does a gambee suture differ from a vertical mattress suture?
- Does not pass through the serosa two times on the same side of the incision
What are some advantages of the gambee suture?
- Tends to minimize mucosal eversion
Why is the gambee suture more commonly used in LA than SA?
- SAs are too small to really see the submucosa and confidently grab it without puncturing full thickness
Where are inverting sutures used and why?
- They are most commonly used in hollow organs and supposedly form a watertight and airtight seal
- Avoided in skin as they slow healing
Why are inverting suture patterns more commonly used in LA than SA?
- They decrease the size of the lumen of hollow organs, and there is greater concern for stricture formation in SA
What are some examples of inverting suture patterns?
- Lembert
- Cushing
- Connel
- Purse String
- Parker-Kerr Oversew
Lembert, Cushing, and Connel are all interrupted or continuous suture patterns?
- Continuous
What is the clinical use of a Lembert suture pattern?
- Intestines for large animals - closing or oversew
- Bladder or stomach oversew for small animals
How is a Lembert suture performed?
- Bites on each side of the incision, perpendicular to the incision, pass into serosa, through muscularis and deep to submucosa, then passes back out without entering the lumen.
How is a Cushing suture performed?
- Bites on each side of the incision, parallel to the incision, pass into serosa, through muscularis and deep to submucosa, then passes back out without entering the lumen.
How is a Connel suture performed?
- Bites on each side of the incision, parallel to the incision, pass into serosa, through muscularis and deep to submucosa, then into the lumen and back out.
The pursue string suture pattern is simply a circular version of a _____________ pattern.
- Continuous
What are some uses of purse string patterns?
- Temporarily close an orifice (i.e. anus)
- Secure tubes
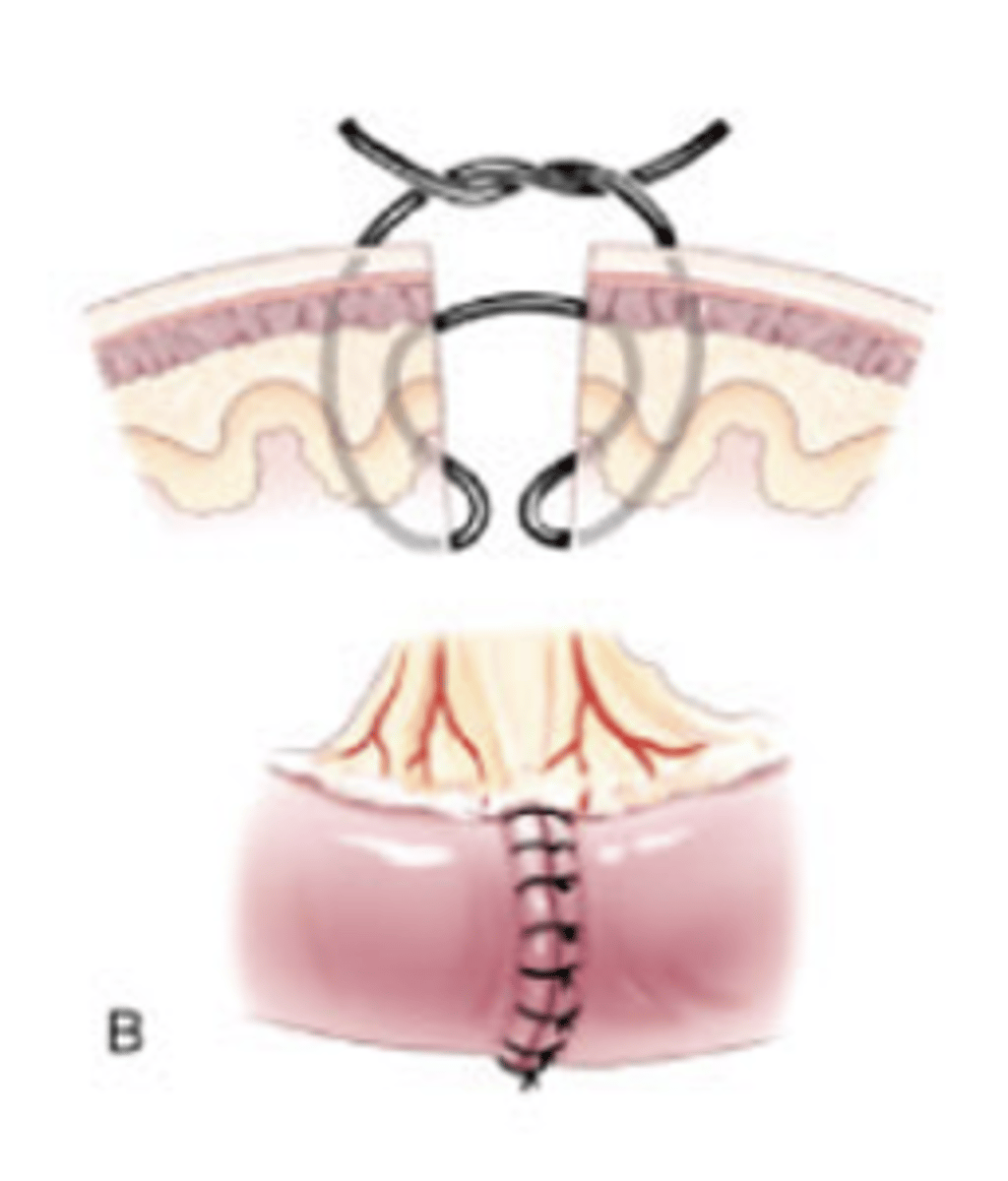
What is the purpose of a Parker-Kerr Oversew?
- Invert a stump of hollow viscus (i.e. uterus after a spay)
How is a Parker-Kerr Oversew performed?
- First layer: Cushing suture over clamp (clamp is withdrawn after suture is tightened)
- Second layer: Lembert placed over the top
What are some examples of tension relieving suture patterns?
- Vertical mattress
- Horizontal mattress
- Far-near-near-Far
All tension relieving suture patterns are interrupted or continuous?
- Interrupted
When performing a vertical mattress suture pattern, the bites closer to the incision should be within _________ of the incision edge.
- 2 mm
Are vertical and horizontal mattress suture patterns inverting, everting, or appositional?
- Everting to appositional
What are some uses of the vertical and horizontal mattress suture patterns?
- Skin
- Fascia
- Muscle (horizontal only)
What is a potential limitation of a horizontal mattress suture pattern?
- Can reduce blood supply to wound edges
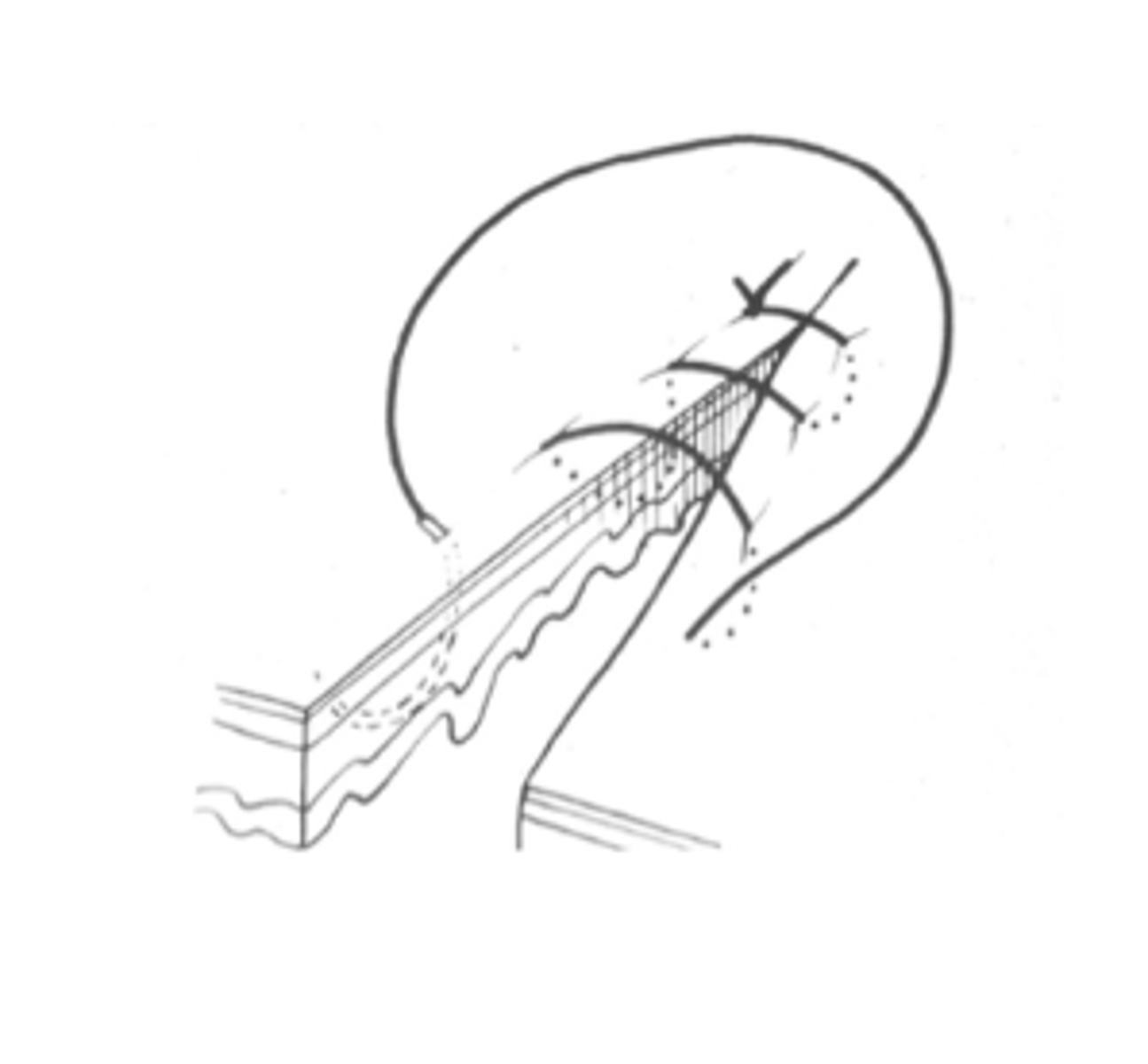
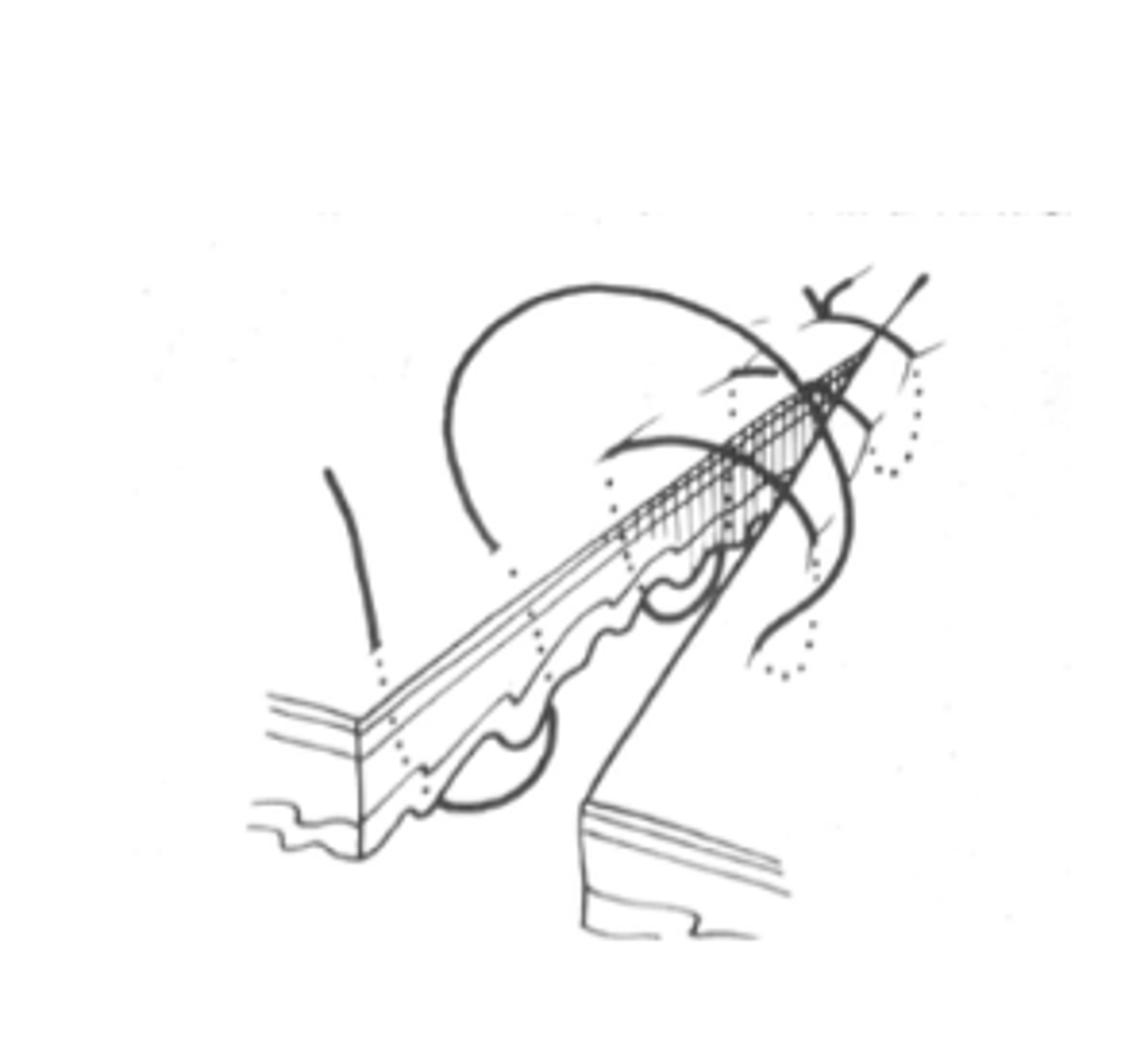
When performing a far-near-near-far suture pattern, the suture works as a ____________. The far suture alleviates _____________ while the near suture is used for _____________.
- Pulley
- Tension
- Apposition
What are some considerations when suturing wounds in the distal limb?
- Excessive tension
- High motion area
- Easily contaminated
Viscera heals ____________ while fascia heals ___________.
- Rapidly
- Slowly
In regards to absorbable vs. non-absorbable, what type of suture would you want to use in viscera and in fascia?
- Viscera (heals rapidly): Absorbable
- Fascia (heals slowly): Slowly absorbable or non-absorbable in some special circumstance
When there is contamination or infection in a wound, what types of suture are generally better?
- Monofilament and synthetic (bacterial environment will break down natural filaments)
What are the 3 major components of fluid administration?
- Resuscitation
- Replacement
- Maintenance
Hydration status is a measure of _________________ fluid content.
- Interstitial
How is hydration status determined/assessed in a physical exam?
- Evaluating skin turgor, moisture of mucous membranes, and possibly enophthalmos
Volume status is a measure of what?
- Tissue perfusion (intravascular space)
How is volume status determined/assessed in a physical exam?
- Mentation
- HR
- CRT
- Pulse quality
- MM color
- BP
In most hospitalized patients, the __________ route is the most appropriate for fluid administration.
- IV
In neonates and small patients in which it is difficult to place an IV catheter, what is a good alternative route of fluid administration?
- Intra-osseous fluid administration
In what case is fluid administration into the peritoneal cavity ideal?
- In dehydrated patients
- Not reliable for promoting diuresis or in oliguric patients
Why is subcutaneous fluid administration not appropriate for a hospital setting?
- May not be absorbed rapidly or completely, and it is not possible to administer a large volume by this route
What are the 4 rules of fluid stewardship?
1) Drug
2) Dose
3) Duration
4) De-escalation
What are the 4 indications for fluid therapy?
- Resuscitation (shock)
- Maintenance
- Replacement
- Nutrition (enteral or parenteral)
What type of fluids are most commonly used?
- Isotonic
What are some examples of isotonic fluids?
- "Physiologic" saline (0.9%)
- Plasmalyte
- LRS
- Normosol-R
Briefly describe the following isotonic fluids:
A. Physiologic saline
B. Plasmalyte
C. LRS
D. Normosol-R
A. No potassium or buffers, and is the fluid of choice for hypercalcemia given that it contains no calcium.
B. Has potassium concentrations similar to plasma and contains acetate buffers to maintain a physiologic pH.
C. Has potassium concentrations similar to plasma and contains a lactate buffer to maintain a physiologic pH.
D. Has potassium concentrations similar to plasma and contains gluconate buffers to maintain a physiologic pH.
Total body water comprises _________% of body weight.
- 60
What percent of total body water is ECF and what percent is ICF?
- ICF: 60% TBW
- ECF: 40% TBW
Extracellular fluid can be divided into which two categories?
- Interstitial (75% ECF)
- Intravascular (25% ECF)
- +/- third space
Water moves between intracellular and extracellular compartments based on _____________ forces. Water moves between interstitial and intravascular compartments due to _____________ forces.
- Osmotic
- Starling's
Sodium moves between intracellular and extracellular compartments via _____________. Sodium moves between interstitial and intravascular compartments _____________.
- Na/K ATPases
- Freely
What is the "saltiest" place in the body?
- Renal medullary interstitium
What are arterial baroreceptors?
- Mechanoreceptors that monitor effective circulating volume and are strategically placed in the carotid sinus and aortic arch. These sensors are stimulated by stretching of the vessel wall and trigger release of neurohormonal signals (Sympathetic nervous system, RAAS, ADH
What is the function of the endothelial glycocalyx, which lines the luminal surface of endothelial cells?
- To maintain the vascular permeability barrier (i.e. "prevent leaky vessels")
In a healthy patient, if 1 liter of fluid is administered, how much volume will reach the interstitial space and the intravascular space?
- 750 mL to interstitial space
- 250 mL to intravascular space
In a patient with a damaged glycocalyx, if 1 liter of fluid is administered, how much volume will reach the interstitial space and the intravascular space?
- 100% of volume to the interstitial space eventually
Describe the relative sodium content of LRS, plasmalyte, and saline.
- LRS < Plasmalyte < Saline
Which isotonic fluid has calcium? Which has magnesium?
- LRS has calcium
- Plasmalyte has magnesium
Would LRS be a good fluid choice for a patient with liver dysfunction?
- No; Do not use LRS, the liver cannot metabolize the lactate
How can a maintenance fluid dose be calculated based on lean body weight in dogs and cats?
- 80*(BW)^0.75 (cats)
- 132*(BW)^0.75 (dogs)
How is replacement fluid dose calculated?
- (% dehydration)(BW kg)(1000ml/kg) to be rehydrated over 12 to 24 hours
What is the fluid dose for neonates and why is it higher than that for adults?
- 100mL/kg/day
- Due to higher total body water content
What is a shock dose of crystalloids?
- 90 mL/kg in dogs
- 45-60 mL/kg in cats
- Note: Give 1/4 aliquots of shock dose over 15 to 30 mins and then reassess the patient
What are the end points/goals of fluid resuscitation?
- Restoration of normal vital signs
- Normalization of abnormal mentation
- Restoration of normal blood pressure (systolic >80-90 mm Hg, MAP >65mmHg)
- Normal serum lactate concentration (<2.5 mmol/L)
- Urine output (UOP) greater than 1 mL/kg/h
What are surgical site infections?
- Infection of incision, tissues surrounding the incision, adjacent organ or viscous (NOT distant infections - these are complications)
What are some classifications of surgical site infections?
- Superficial incisional SSI
- Deep incisional SSI
- Organ or space SSI
How do surgical site infections occur?
- Contamination of tissues/spaces during surgery (= introduction of organisms into a wound)
What are possible effects/consequences of surgical site infections?
- Endotoxemia
- Bacteremia
- Sepsis/septicemia
How do surgical site infections affect the outcomes of surgeries?
- Increased postoperative morbidity/mortality
- Increased cost of therapy
- Prolonged hospitalization
What are some host factors which may increase the risk of SSIs?
- Decreased immune competence
- Prior irradiation of the surgical site
- Older age of the animal (SA > 8 YO)
- Distant sites of active infection
- Abnormal body condition scores
What are some medical management factors which may increase the risk of SSIs?
- Surgery sites clipped any time before anesthetic induction (3x more likely to develop infection)
- Inadequate skin preparation of surgical site
- Propofol as part of anesthetic protocol (lipid-based emulsion, supporting rapid microbial growth at room temperature, use within 12 hours of opening)
What are some surgical factors which may increase the risk of SSIs?
- Duration of anesthesia (>60 mins)
- Duration of surgery (>90 mins)
What is the average critical level of contamination in surgical sites?
- >100,000 CFU*/g tissue results in infection on average (however, this is influenced by pathogenicity/virulence and host factors)
What is the average critical level of contamination in surgical sites in avascular tissues?
- Much lower; 100 CFU* of Staph. aureus sufficient for septic arthritis
What are some factors which may inhibit a patient's local immune response to contamination?
- Blood clots
- Ischemic tissue
- Charred tissue
- Fluid pockets
- Foreign material (orthopedic material, implants, suture, etc.)
Describe the effect that braided/multifilament suture has on the risk of SSIs.
- Reduces the CFUs of Staph. aureus organisms required for surgical site infection from 100,000 to 100; Bacteria can hide in the interstices of the suture.
What are some ways to reduce SSIs?
- High standards of aseptic technique
- Good case selection
- Appropriate/judicious use of antibiotics
- Appropriate preoperative planning
- Excellent surgical technique
- Proper postoperative care
What is antimicrobial prophylaxis?
- Administration of an antimicrobial agent prior to surgical incision (i.e. Cefazolin)
For a clean procedure (i.e. a lumpectomy), is antibiotic prophylaxis needed?
- Antibiotic prophylaxis technically not needed; Can do peri-operatively for 24h
For a clean-contaminated procedure (i.e., anytime you encounter a mucosal surface or there is a break in sterility in what would otherwise be a clean procedure), is antibiotic prophylaxis needed?
- Recommended peri-operatively for 24 hours