Peritonitis, Ascites, GI Bleeds, Obesity
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
44 Terms
Ligament of treitz
What anatomical structure determines if a GI bleed is upper or lower
Upper GI Bleeding (UGIB)
Bleeding proximal to the ligament of trietz that can present as Hematemesis (moderate/severe) or coffee-ground emesis (limited) → self limited in 80%
Over 1000 mL (melena can be as little as 50-100)
If there is an UGIB with hematochezia what is the estimated blood loss
Peptic ulcer disease (40%), Portal hypertension (10-20%), Mallory-Weiss tears (5-10%), vascular abnormalities, erosive gastritis/esophagitis, gastric neoplasms
Etiology of UGIB
CBC (anemia if chronic, don’t watch Hgb/Hct it takes to 2-3 hrs), CMP (LFTs), H. pylori, 2 16 G IVs, Type and screen, Coags (correct if necessary), EGD (varice ligation, within 12 hours)
45 y/o patient presents to the ER for “throwing up blood” and abdominal pain. He also reports melena and fatigue as well. On a physical exam you note pallor and diaphoresis. Vitals are stable with the exception of 90/50 (sitting) and 134 bpm. What do you want to order?
EGD
What is the definitive diagnostic and treatment for GI bleeds?
Admit to hospital, PPIs, Antibiotics (patients with bleeding varices), Octreotide (only recommended for varices), TXA (no benefit)
Treatment plan for UGIB
Systolic under 100, Postural hypotension, tachycardia
Indications of severe blood loss during a GI Bleed (remember don’t watch Hbg/Hct it ain’t fast enough)
evacuating the stomach pre-EGD
When are NG tubes used for UGIBs
Lower GI Bleed (LGIB)
A bleed distal to the ligament of treitz (colon 95%) usually presenting with hematochezia (blood on toilet paper, in stool, dripping) → spontaneous cessation in 75%
Diverticulosis (50% most common), neoplasms (polyps, cancers, chronic occult blood loss), IBD (ulcerative colitis), hemorrhoids, fissures, ulcers, Ischemic colitis (think this post-MI)
Causes of lower GI bleed
Reported bright red blood from rectum, Rectal exam with frank blood, positive fecal occult blood test, Anoscope visualization of hemorrhoid/rectal vault bleeding
Diagnostic criteria for LGIB
Start with colonoscopy if you don’t find the source → EGD
When treating stable patients with hematochezia
Resuscitate/consider surgery, EGD once stable if you don’t find the source → colonoscopy
When treating unstable patients with hematochezia
PPIs (omeprazole) for risk of ulcers due to NSAID use, Beta blockers for esophageal varices, Preventative EVL in patients with C/I for beta blockers
Prevention measures for GI bleeds
Ascites
An abnormal accumulation of fluid in the peritoneal cavity (more than 20 mL) most commonly caused by portal HTN
Infectious, intra-abdominal malignancy, inflammatory disorders of the peritoneum, ductal disruptions
Etiologies for Ascites (other than portal HTN)
liver disease, EtOH, blood transfusions, tattoos, IV drug use, hepatitis/jaundice at birth
Risk factors for ascites
Paracentesis with cell count/differential, inspection, SAAG, culture, gram stain, cytology; Blood work may show evidence of liver failure or CHF, cirrhosis may show elevated INR, hypoalbuminemia, thrombocytopenia, anemia, and leukopenia
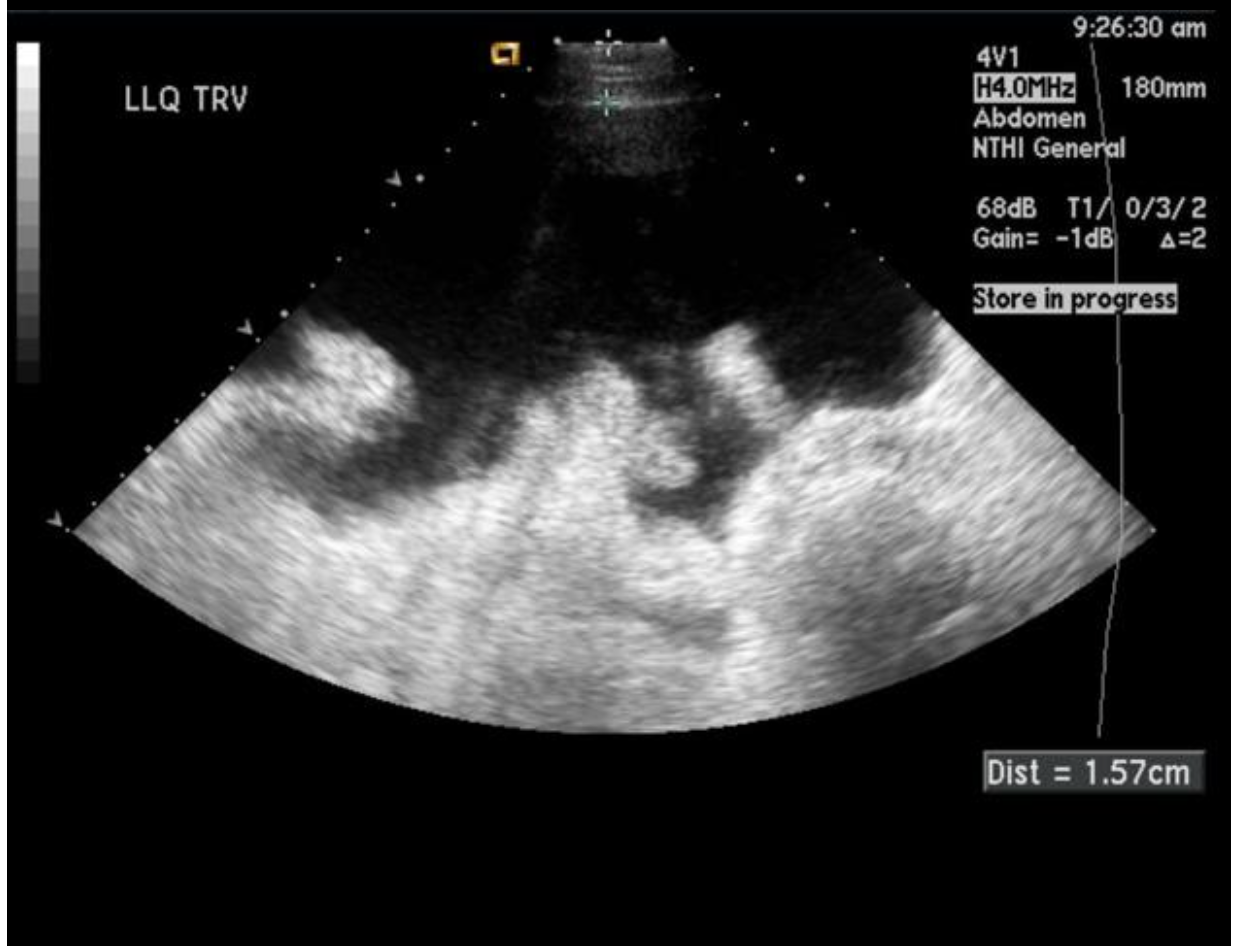
55 y/o male patient presents to the ER for SOB and abdominal fullness. PMHx is positive for alcoholic liver cirrhosis. On a physical exam you note a distended abdomen that has a positive fluid wave. See abdominal U/s. What do you want to order?
NORMAL
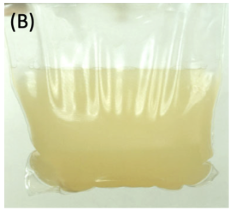
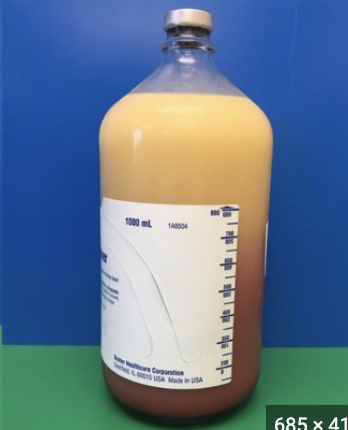
Clear, yellowish, honey-colored para fluid is associated with
infection
Cloudy para fluid is associated with
chylous
Milky para fluid is associated with
trauma, malignancy
Bloody para fluid is associated with

Iatrogenic bacterial peritonitis, organ damage/perforation
While an abdominal paracentesis can be indicated for initial onset of ascites, Sx relief, or diagnosing bacterial periotnitis → what are the complications
Less than 500 WBCs, less than 250 PMNs (if lymph > PMN think viral)
What is a normal cell count/Diff for para fluid
Portal hypertension (anything over 1.1 g/dL)
The Serum Albumin Ascites Albumin Gradient has a 95% specificity for determining
Abdominal U/S (find drainage spots), CT (finding masses), Laparoscopy (visualization and biopsy of suspected malignancy)
What else should be included in the diagnostic eval for acites?
Sodium restriction, Diuresis (spironolactone, furosemide), para (symptomatic relief), TIPS (trans-jugular intraheptic portosystemic shunt) or liver transplant for refractory cases
Treatment plan for ascites → 1st line for peeps with cirrhosis
Spontaneous Bacterial peritonitis
A infection of ascitic fluid with no apparent intra-abdominal source (usually translocation from the gut so think gram neg pathogens)
IV 3G CPH for 5-10 days, IV albumin (protects kidneys, decrease mortality), discontinue non-selective beta blockers
55 y/o male patient presents to the ER for AMS and abdominal pain. Vitals are stable with the exception of a temp of 101.7. On a physical exam you note a red, distended, tender abdomen that has a positive fluid wave, rebound tenderness, and a positive heel tap. See abdominal U/s. Labs are as follows serum WBCs at 13,000, Ascitic fluid PMN of 400, WBCs of 750. What is your treatment plan?
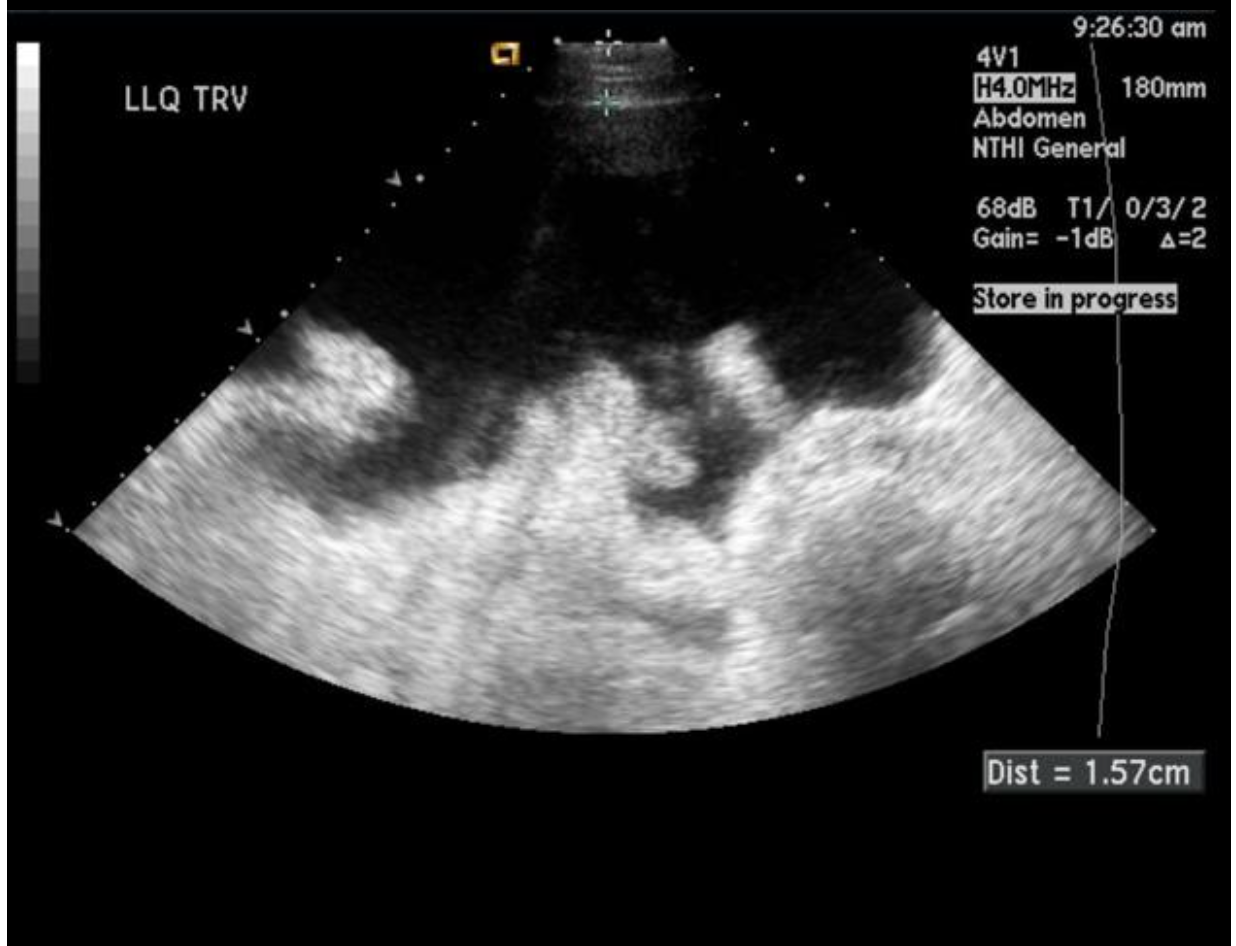
temp over 100, PMNs over 250, abdominal pain/tenderness, AMS
Which bacterial peritonitis patients get empiric therapy → treat early (over 30% mortality if you don’t)?
secondary intra-abdominal infections, perforation, malignancy
DDX for bacterial peritonitis
Long-term prophylatic antibiotics to all survivors (70% relapse)
Prevention plan for Bacterial peritonitis
obesity
An excessive accumulation of body fat, typically a BMI over 30 that is associated with numerous health complications
caloric intake exceeds expenditure, genetic/environement/behavioral, leptin resistance, insulin resistance, altered gut microbiome, chronic low-grade inflammation
Pathophys for obesity
BMI, waist circumference, assess for central obesity
Ways to diagnose obesity
HTN, coronary artery disease
CV effects of obesity
Type 2 DM, dyslipidemia
Metabolic effects of obesity
OSA
Respiratory effects of obesity
osteoarthritis, certain cancers, depression
Other effects of obesity
Caloric deficit with balanced nutrition, 150 min/week of activity, CBT, Bariatric surgery (BMI 35+. 30+ with comorbidities)
Non-pharm management of Obesity
S.C. tirzepatide, semaglutide, liraglutide
1st line Pharm management of Obesity - indicated for BMI 30+ or 27+ with comorbidities
Phenteramine-topiramate (C/I with CVD and uncontrolled HTN), Naltrexone-bupropion, Orlistat, Lorcaserin with liraglutide
Alternative Pharm management of Obesity - indicated for BMI 30+ or 27+ with comorbidities
6 y/o and up
When are we screening for obesity?