The Reproductive system
1/7
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
8 Terms
What is female reproductive system responsible for?
The female reproductive system is responsible for producing eggs (ova), creating sex hormones, facilitating sexual intercourse, menstruating, and nurturing a pregnancy from fertilization to childbirth.
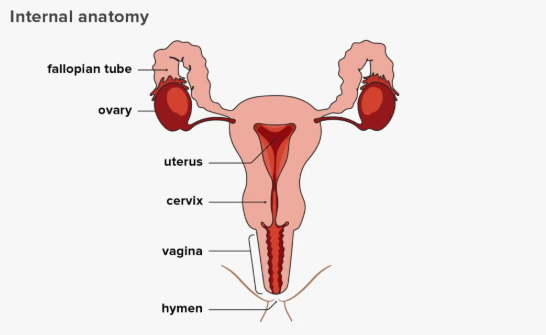
Female reproductive system parts and function
Internal Organs
Ovaries: Two oval glands that produce eggs (ova) and sex hormones (estrogen, progesterone). Contain and release ova.
Fallopian Tubes (Oviducts): Tubes connecting ovaries to the uterus; the usual site for fertilization as they transport eggs to the womb. lined with ciliated cells to help push ovum or zygote along.
Uterus (Womb): A pear-shaped muscular organ that receives a fertilized egg and supports fetal development during pregnancy, expanding significantly. The endometrium thickens for preparation for pregnancy.
Cervix: The lower, narrow part of the uterus that opens into the vagina. Holds the fetus into place and allows sperm to enter and blood to exit.
Vagina: A muscular canal connecting the cervix to the outside of the body, serving as the birth canal and for sexual intercourse.
External Organs (Vulva)
Mons Pubis: Fatty tissue over the pubic bone.
Labia Majora/Minora: Folds of skin protecting the vaginal and urethral openings.
Clitoris: A small, sensitive organ for sexual pleasure.
What is male reproductive system responsible for?
The male reproductive system is responsible for producing, storing, and transporting sperm, secreting male hormones like testosterone, and delivering sperm into the female reproductive system for fertilization, enabling sexual reproduction and male development.
Male reproductive system parts and function
Testes (Testicles): Produce sperm (spermatogenesis) and the primary male hormone, testosterone.
Scrotum: A pouch of skin that hangs outside the body, keeping the testes at a cooler temperature needed for sperm production.
Epididymis: A coiled tube on the testicle where sperm mature and are stored also become motile meaning able to move.
Vas Deferens (Ductus Deferens): Muscular tube that transports mature sperm from the epididymis towards the urethra during ejaculation.
Seminal Vesicles: 2 sac-like glands behind bladder that secrete a nutrient fluid rich in fructose, which produces energy for sperm and is a major component of semen.
Prostate Gland: A walnut sized gland that surrounds the urethra. Secretes an alkaline, milky fluid that nourishes and protects sperm and makes up part of semen.
Ejaculatory Ducts: Form where the vas deferens joins the seminal vesicle duct, emptying into the urethra.
Urethra: A tube that extends from the bladder to the tip of penis and carries semen out of the body during ejaculation and urine out during urination. A muscular ring prevents them from mixing.
Bulbourethral Glands (Cowper's Glands): 2 small glands located below protrate. Produces clear lubricating fluid that is secreted into urethra pre-ejaculation.
Reproductive hormones
Key Female Hormones
Estrogen: Develops female traits, thickens uterine lining, and regulates the menstrual cycle. Produced by a maturing follicle and corpus luteum.
Progesterone: Maintains the uterine lining for potential pregnancy, prepares breasts for milk, and rises after ovulation. Produced by corpus luteum which is an empty follicle after ovulation.
FSH (Follicle-Stimulating Hormone): Stimulates egg maturation and estrogen production in the ovaries. Released by the pituitary gland.
LH (Luteinizing Hormone): Triggers the LH surge, which causes ovulation (mature ovum/egg release). Released by the pituitary gland.
Prolactin: Stimulates milk production.
Oxytocin: Stimulates uterine contractions during childbirth and milk release.
Key Male Hormones
Testosterone: The primary male hormone, responsible for sperm production and male sexual characteristics.
FSH & LH: Also regulate sperm production in males. LH stimulates testosterone production.
what happens if fertilisation occurs or don’t occurs
If fertilization occurs, a zygote forms and develops into an embryo, leading to pregnancy. corpus luteum continous to secretes progesterone.
If fertilization does not occur, the egg cell breaks down, and the uterine lining is shed during menstruation. Corpus luteum breaks down leading to progesterone level dropping.
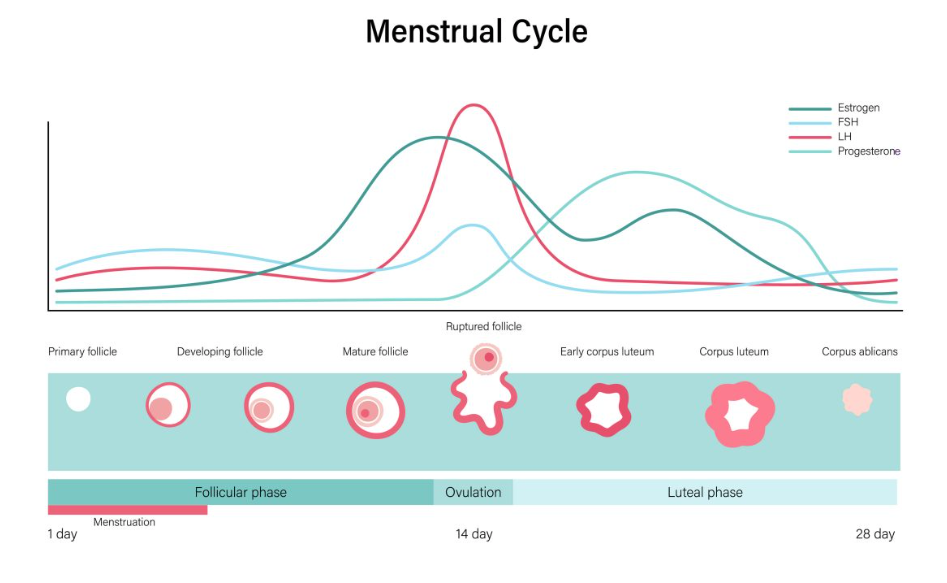
How Hormone Works Together (Menstrual Cycle Example)
Start:
FSH levels rise, causing follicles (egg sacs) to grow and produce estrogen.
Estrogen Rises:
Estrogen builds the uterine lining and inhibits FSH, promoting LH production.
LH Surge:
A sharp increase in LH triggers the release of the mature egg (ovulation).
Progesterone Rises:
After ovulation, LH causes the empty follicle to produce progesterone, which maintains the uterine lining.
Cycle Ends/Continues:
If no pregnancy, progesterone drops, causing menstruation. If pregnancy occurs, progesterone continues.
Stages of menstrual cycle
Menstrual Phase (Period): Starts on Day 1 to 5, when the uterus sheds its lining, causing bleeding. Hormone level drops.
Follicular Phase: (6 to 14) Begins with your period, as hormones signal the ovaries to grow follicles and releases oestrogen and progesterone, each containing an egg; the uterine lining also starts to rebuild.
Ovulation Phase: (14) A surge in LH causes the dominant follicle to release an egg from the ovary, typically around the middle of the cycle to the follipiqn tube.
Luteal Phase: The ruptured/empty follicle becomes the corpus luteum, producing progesterone to thicken the uterine lining for a potential pregnancy; if no pregnancy, hormone levels drop, leading to the start of the next period.
Key Hormones & Changes:
Estrogen & Progesterone:
Levels rise and fall, influencing mood, energy, and uterine lining thickness.
LH & FSH:
Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH) trigger follicle growth and ovulation.