Body Defences
1/101
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
102 Terms
Specific vs nonspecific defences
Defences are classified as specific or non-specific depending on what pathogens it works against.
-Non-specific work against all pathogens.
-Specific: directed at a particular pathogen.
Lines of defence
1st line: External nonspecific - skin, cilia etc.
2nd line: Internal nonspecific - Protective reflexes, phagocytes, lymphatic system, inflammatory response, fevers
3rd line: Internal specific - immune response -antigens and antibodies, antibody mediated immunity, cell mediated immunity
Nonspecific defence: External defences
Skin
Mucus
Hair
Cilia
Acids
Lysozyme
Cerumen
Movement of fluid
Nonspecific defence: External defences: Skin
A waterproof barrier that prevents pathogens from entering the internal body system. At openings such as the mouth, bacteria occupies the area, so pathogens find it difficult to become established.
Sebum
is produced by oil glands: Contains some substances that kill some bacteria. Slightly acidic, creating an unsuitable environment.
Sweat
contains salts and fatty acids that prevent the growth of many micro-organisms.
Nonspecific defence: External defences: Mucus
Mucous membranes line the body cavities that open to the exterior.
Secretes mucus, trapping particles and inhibiting the entry of micro-organisms to the organs of the body.
Digestive, urinary, reproductive tracts are all protected by this.
Nonspecific defence: External defences: Hair
Found in the nasal cavity, and in the ears. This and a layer of mucus up to 90% of particles inhaled when breathing.
Nonspecific defence: External defences: Cilia
Tiny, hair-like projections from cells that are capable of a beating motion. In mucous membranes lining the nasal cavity, trachea, and other air passages. Beating movement moves mucus, containing trapped particles and micro-organisms towards the throat where it may be coughed up or swallowed.
Nonspecific defence: External defences: Acids
Stomach juices are strongly acidic. Kills many bacteria taken in with food or those contained in mucus swallowed. Vagina has acid secretions that reduce the growth of micro-organisms.
Nonspecific defence: External defences: Lysozyme
An enzyme that kills bacteria. Eyes are protected by flushing of tears, containing this. Found in saliva, sweat, nose secretions, tissue fluid.
Nonspecific defence: External defences: Cerumen
Ear wax. Protects the outer ear against infection by some bacteria. Slightly acidic and contains lysozymes
Nonspecific defence: External defences: Movement of fluid
The flushing of body fluid helps keep areas relatively pathogen free. Urine flowing through urethra is cleansing. Prevents bacterial growth and helps stop bacteria reaching the bladder and kidneys. Shorter urethra (women) tend to suffer more bladder infections. Tears, sweat, saliva also involved.
Nonspecific defence: Protective reflexes
An automatic, involuntary response to a stimulus. Four reflexes help to protect against infection by removing foreign particles.
Sneezing
Coughing
Vomiting
Diarrhoea
Nonspecific defence: Protective reflexes: Sneezing
Caused by irritation of nasal cavity walls.
Forceful expulsion of air carries mucus, foreign particles and irritating gases out through the mouth.
Nonspecific defence: Protective reflexes: Coughing
Caused by irritation of the lower respiratory tract. Air is forced from lungs to try and remove irritant, driving mucus and foreign matter out the mouth.
Nonspecific defence: Protective reflexes: Vomiting
Psychological stimuli. Caused by excessive stretching of the stomach and bacterial toxins. Contraction of abdominal muslces and diaphragm expels stomach contents.
Nonspecific defence: Protective reflexes: Diarrhoea
Caused by irritation of small and large intestines by pathogens. Causes increased contractions of the muscles of the wall of the intestines so the irritant is quickly removed.
Internal non-specific defences
Phagocytes
Lymphatic system
Internal non-specific defences: Phagocytes
Cells that can engulf and digest pathogens and cell debris through phagocytosis. Most derived from stem cells in the bone marrow.
Internal non-specific defences: Phagocytes: Monocytes
White blood cells. Circulate in the blood or remain in tissues. Differentiate into macrophages or dendritic cells depending on the signals they receive
Internal non-specific defences: Phagocytes: Macrophages
Found in almost all tissues and organs, but rarely in the bloodstream. Phagocytose antigens. Involved with the inflammatory response and the specific immune response as antigen presenting cells
Internal non-specific defences: Phagocytes: Dendritic cells
Present in tissues that are in contact with the body's external environment. Have branched projections. Phagocytosis pathogens. Become antigen presenting cells in the specific immune response
Internal non-specific defences: Phagocytes: Neutrophils
Most common WBC in humans. The first responder during inflammation leaving the bloodstream and reaching the site of infection. Phagocytose pathogens. Boosts the response of other immune cells. Die after phagocytosis, becoming pus.
Internal non-specific defences: Lymphatic system
-A network of lymph capillaries joined to larger lymph vessels
-Lymph nodes, located along the length of some lymph vessels.
Excess tissue fluid is drained into lymph capillaries and circulated around the body passing through lymph nodes, made up of a meshwork of fibres that can trap pathogens. Contains macrophages and lymphocytes. When infections occur, the formation of lymphocytes increases and the lymph nodes become swollen and sore.
Internal non-specific defences: Lymphatic system: Natural Killer (NK) Cells
Able to differentiate between normal and virus infected cells. Detect a lack of self cell surface receptors or certain receptors on the target cell. Can lyse (perforate the cell membrane) and kill virus infected cells and cancer cells
Internal non-specific defences: Lymphatic system: Interferon
A glycoprotein produced by virus infected cells that interferes with viral replication. Cause neighbouring cells to produce anti-viral proteins. Increases the activity of macrophages and killer T cells to detect and destroy abnormal cells.
Internal non-specific defences: Lymphatic system: Complement system
A group of proteins that circulate in the blood that complements other aspects of the immune response
-Recruit phagocytes to site of inflammation and activate them.
-Activate mast cells to release histamine and other inflammatory factors
-Bind to receptors on phagocytes, helping to remove agent of infection
-Lyse
Inflammatory response
-Prevent / reduce the spread and entry of pathogens
-Destroy pathogens
-Removes and repairs damaged tissue.
Signs of inflammation
Redness, swelling, heat, pain
Steps for inflammatory response
Step 1: MECHANICAL Damage and mast cells
Step 2: histamine
Step 3: Heparin
Step 4 : Phagocytes
Step 5 : Pain
Step 6 : pathogen death and pus
Step 7 : Repair through mitosis
Steps for inflammatory response: Step 1
Mechanical Damage and mast cells.
Damage triggers release of small signalling proteins: cytokines
-These activate specialised leucocytes called mast cells. Results in the release of the histamine and heparin.
Steps for inflammatory response: Step 2
Histamine
Diffuses into capillaries, causing them to dilate and become more permeable.
More fluid moves through the capillary wall into the tissue. Results in heat, redness and swelling.
Steps for inflammatory response: Step 3
Heparin
Prevents clotting in the immediate area of the injury. Ensures phagocytes in the bloodstream can reach the damaged tissue. A clot of the fluid forms around the damaged area, which slows the spread of pathogens into healthy tissues.
Steps for inflammatory response: Step 4
Phagocytes
Mast cells release chemicals/complementary system proteins that attract phagocytes to the effected area (CHEMOTAXIS), particularly neutrophils. Phagocytes engulf and digest dead cells or micro-organisms.
Steps for inflammatory response: Step 5
Pain
Abnormal conditions stimulate pain receptors
Steps for inflammatory response: Step 6
Pathogen death and pus
Phagocytes filled with bacteria die and form pus as pathogens are destroyed. Histamine and protein signalling finishes and phagocytes are no longer attracted to the area.
Steps for inflammatory response: Step 7
Repair through mitosis
New cells are produced by mitosis, and repair of the damaged tissue takes place
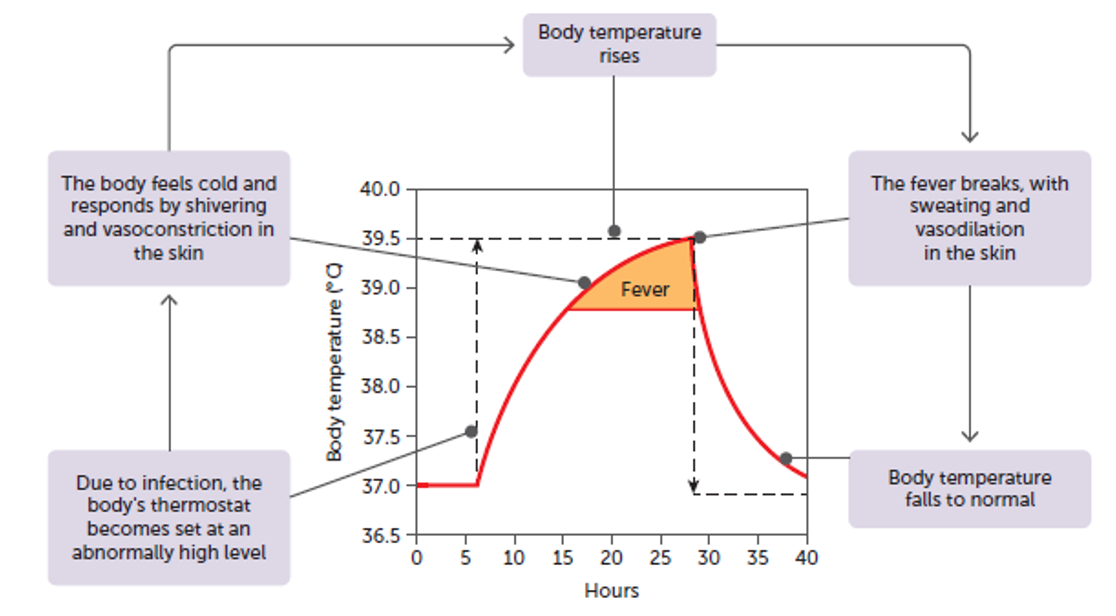
Fever
An elevation of body temperature most often caused by an infection from pathogens.
Steps of a fever
Step 1: pathogen enters body
Step 2: Macrophages respond
Step 3: Thermostat is reset
Step 4: Fever onset
Step 5: Chill phase
Step 6: Crisis phase (Plateau Phase)
Step 7: Fever breaks (defervescence phase)
Steps of a fever: Step 1
Pathogen enters body
Steps of a fever: Step 2
Macrophages respond
Macrophages englufs and destroys the pathogen through phagocytosis, releasing endotoxins. These endotoxins cause the macrophage and other cells such as dendritic and epithelial cells to produce and release pyrogens.
Steps of a fever: Step 3
Thermostat is reset
Pyrogens travels in the blood to the brain and induces the hypothalamus to reset the body’s thermostat to a higher temperature (they make the body think it is cooler than it actually is)
Steps of a fever: Step 4
Fever onset
To reach the new, higher thermostat setting, the hypothalamus causes the body to carry out actions that generate and retain heat.
-Vasoconstriction of blood vessels. Skin arterioles constrict, less heat is lost from the skins surface via radiation, conduction and convection
- Increased metabolic rate
-Shivering: skeletal muscles contact and the respiration that occurs to produce these contraction results in the production of heat
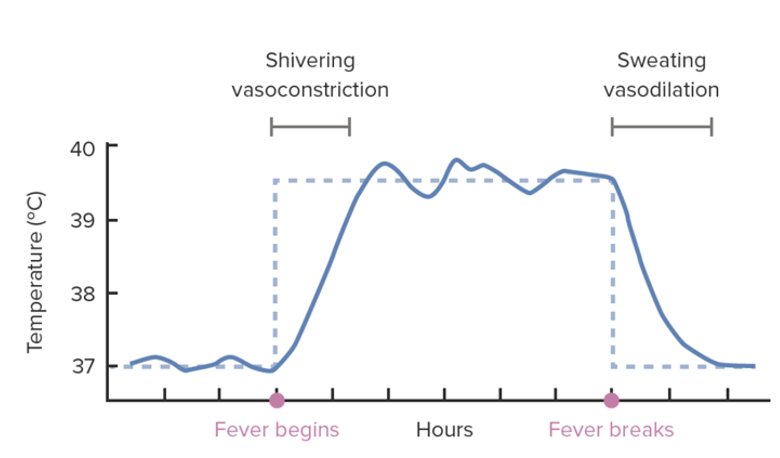
Steps of a fever: Step 5
Chill phase
Even though body’s temperature is elevated, it feels cold and shivering occurs (a chill). When the body reaches the setting of the thermostat, the chill disappears.
Steps of a fever: Step 6
Crisis phase (Plateau Phase)
Body temperature is maintained at the higher setting until the pathogen has been eliminated and macrophages are no longer releasing pyrogens.
Steps of a fever: Step 7
Fever breaks (defervescence phase)
As the pyrogens subside, the thermostat is reset to normal by heat loss mechanisms:
- Sweating
-Vasodilation of skin arterioles
-Person feels warm and looks flushed
-Heat is lost and body temperature is returned to normal
Benefits of a fever
I STOP VIRUSES RUNNING TOGETHER
Create a non-optimal temperature which may inhibit the growth of pathogens.
Speed up the rate of chemical reactions, which can help body cells repair themselves more quickly during a disease.
Inhibit viral replication by increasing effect of interferon.
Increase heart rate/blood flow which enables leucocytes to reach sites of infection faster
Increase the production of killer T cells which speed up the specific immune response
Fever treatment
During the defervescence phase cooling can be enhanced by a cool shower or applying a wet cloth, use of a fan, removal of bedding or clothing.
Managing a fever
Take paracetamol or ibuprofen to help bring the temperature down. Drink plenty of fluids, particularly water to avoid dehydration.
High fever (about 41.5°C or more) is extremely dangerous and could trigger convulsions. Generally, death will result if the body temperature reaches 44.4 – 45.5oC.
Lymphocytes
White blood cells
Name | Type of Defence | Made in | Mature in | End up in |
Natural Killer cells (NK) | Non-specific | Bone marrow | Bone marrow, lymph tissue, thymus | Circulate in blood |
B-Cells (B-lymphocytes) | Specific | Bone marrow | Bone marrow | Lymphoid tissue |
T-cells (T-lymphocytes) | Specific | Bone marrow | Thymus | Lymphoid tissue |
Antigens
Any substance capable of causing a specific immune response. Large molecules. May be:
- whole micro-organisms or part of a bacterium
-virus particles
-toxins
-pollen grains
Types of antigens
Type | Where do they come from | Do they trigger an immune response | Example |
Self-antigen | Produced by a persons own body | No | Antigens on outside of RBCs |
Non-self antigen | Foreign compounds | Yes | tetanus |
How does the body distinguish between self and non-self antigens
The major histocompatibility complex (MHC). MHC are a group of genes that are unique in every individual. Code for small protein molecules that act as ‘self’ markers on all body cells.
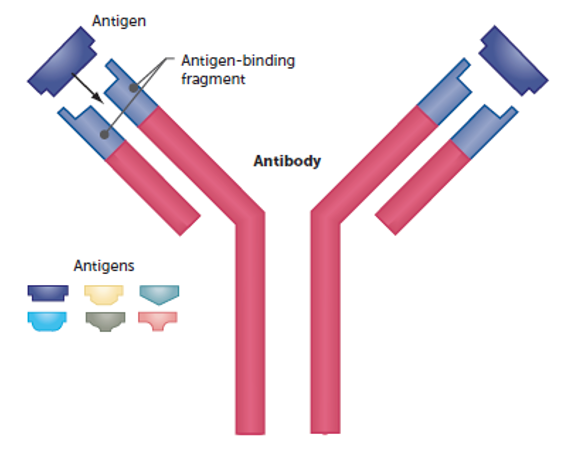
Antibodies
Y-shaped specialised protein produced in response to a non-self-antigen.
Antigen-Presenting Cells
Recognise when a non-self antigen enters the body. Include dendritic cells, macrophages and undifferentiated B-cells.
1) Detect the presence of a non-self antigen
2) Engulf the pathogen
3) Digest the pathogen, producing small fragments that move to the surface of the cell
4) Present the antigen to lymphocytes
Antibody mediated immunity
Involves the production and release of antibodies into the blood and lymph. Provides resistance to foreign substances before they enter the bodys cells
Antibody mediated immunity steps
Step 1: Detection
Step 2: Presentation
Step 3: Activation
Step 4: Production
Step 5: Formation of Antigen-Antibody Complex
Antibody mediated immunity step 1
Detection
Macrophage destroys a pathogen, isolates the antigen and places it on its cell membrane. The macrophage is then called an antigen-presenting cell
Antibody mediated immunity step 2
Presentation
Antigen-presenting cell reaches lymphoid tissue containing many types of B-cells and presents the antigen to lymphocytes. If the B-lymphocyte has a receptor that corresponds to the antigen, the B-cell is sensitised.
The antigen is also presented to helper-T cells which release cytokines that cause the helper-T cells to clone themselves and activate the B-cells.
Antibody mediated immunity step 3
Activation
Sensitized B cells undergo rapid cell division to produce a group of clone of B-cells. Most new B-cells develop into plasma cells
Antibody mediated immunity step 4
Production
Plasma cells produce specific antibodies and release them into the blood and lymph circulating until they reach the site of invasion.
Antibody mediated immunity step 5
Formation of Antigen-Antibody Complex
The antibody can recognise the complimentary antigen it was manufactured for and bind with it at specific active sites. The two molecules to fit together, forming antigen-antibody complex that can inactivate the activity of the pathogen.
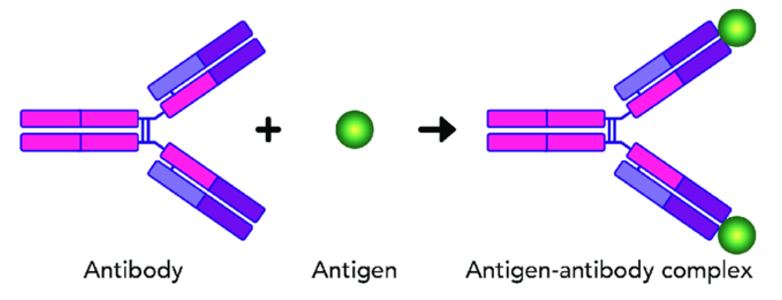
How antigen - antibody complexes work
I BUY CATS CLOTHES REGULARLY
Antibodies do not directly destroy pathogens but :
1. Inactivate substances by combining with them or inhibiting their reactions with other cells or compounds
2. Bind to the surface of viruses and prevent them from entering cells
3. Coat bacteria and make them more easily phagocytosed
4. Cause agglutination (then more easily phagocytosed)
5. React with soluble substances to make them insoluble = more easily consumed by phagocytes
Memory cells
Some of the B-cells form memory cells. Memory cells spread to all body tissues to allow the response to occur more rapidly if the pathogen enters the body again.
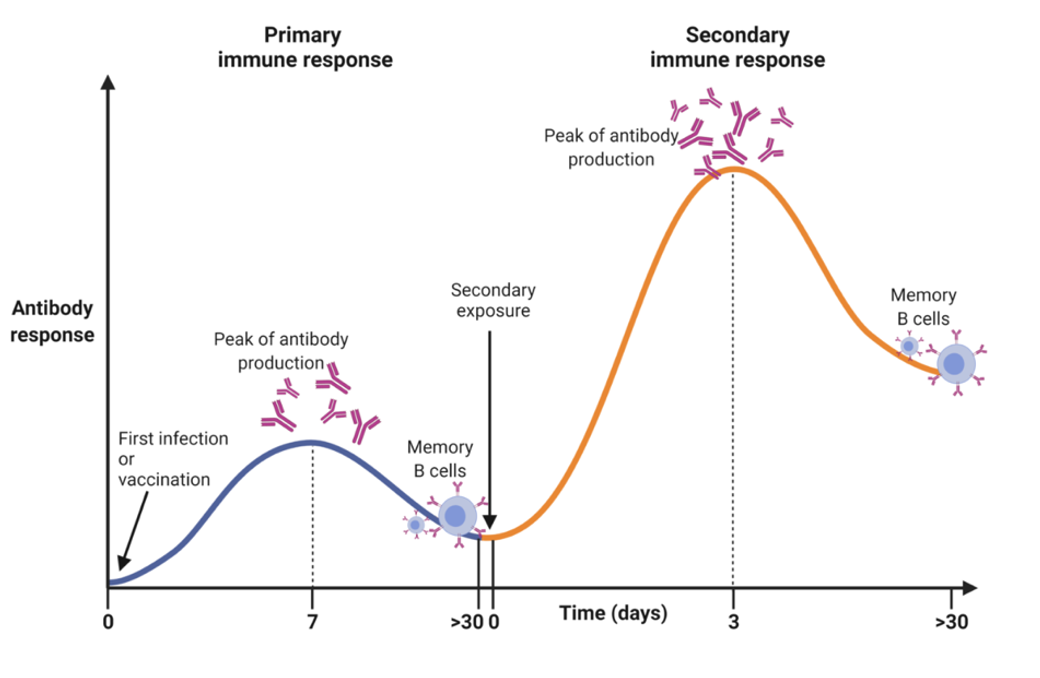
Memory cells: Primary response
First exposure to antigen.
Body responds slowly. Takes days to build up antibodies. Takes time for B-cells to multiply and differentiate into plasma cells. Relatively low numbers of antibodies produced. Leaves the immune system with memory of the particular antigens.
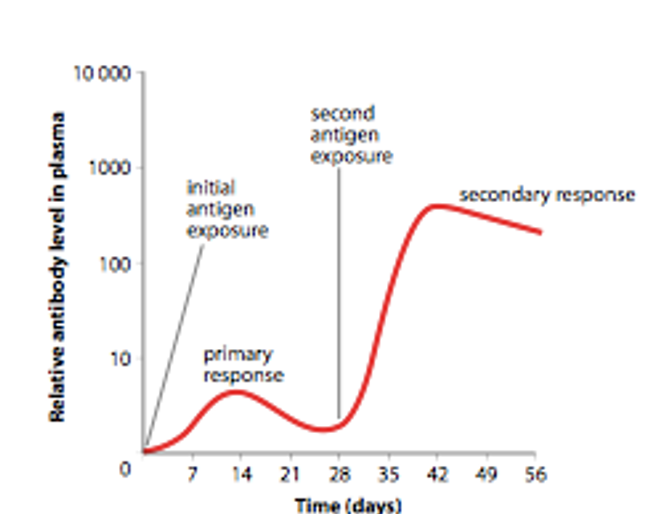
Memory cells: Secondary response
The response to a second or subsequent exposure to a pathogen. Response is faster.
Antibody reach a higher level and last longer.
So quick that antigen little response to effect the body. Some T-cells become memory cells can initiate a faster response if there are subsequent infections
Cell mediated immunity
Involves mostly T-cells. Responds to any cell that displays incorrect MHC markers.
Cell mediated immunity step 1
Detection and presentation
Antigen-presenting cells displaying the antigen on their surface travel to lymph nodes and present to the T-cell programmed for that antigen.
Cell mediated immunity step 2
Activation
The sensitised T-cell are stimulated to undergo rapid division to form a a clone of T-cells.
Cell mediated immunity step 3
Production
Clone cells differentiate into different types of T-cells and memory cells. 3 main types
Killer T cells
Attach to the affected cells and secrete a substance that destroys the antigen, then searches for more antigens.
Helper T cells
Secrete substances stimulating B-cells to produce antibodies and stimulate nonspecific agents to destroy the antigen by:
Attracting lymphocytes to the infection site so they become sensitized and activated
Attracting and intensifying the phagocytic activity of macrophages
Promote the action of killer T-cells
Regulatory T-cells
When the immune activity becomes excessive, or the infection has been dealt with. They inhibit T- and B- cell activity.
Immunity
Resistance to infection by invading micro-organisms.
Can be passive or active
Passive immunity
When someone is given antibodies produced from someone else. The individual's body plays no part in the production of the antibodies. Immunity establishes immediately. Short lived: lasts only until the antibodies are broken down and excreted. Can be either natural or artificial
Active immunity
When the body is exposed to a foreign antigen and manufactures antibodies in response to that antigen.
Prolonged immunity: the memory of the antigen persists through the memory cells. Lasts for many years and often for life. If exposed to the antigen again the antibodies will produce rapidly again.
Natural passive immunity
1. Occurs without human intervention.
2. Body gets antibodies produced by someone else.
3. Antibodies are not long-lasting.
E.g. antibodies that pass across placenta or breast milk from mother to baby
Natural active immunity
1. Occurs without human intervention
2. Body produces antibodies
3. Long lasting.
4. E.g. a person’s ability to manufacture antibodies resulting from an attack of a disease
Artificial passive immunity
1. Uses human intervention
2. A person is injected with antibodies in the bloodstream.
3. Last a few weeks to months
Tetanus, antivenom
Artificial active immunity
1. Uses human intervention
2. Body produces antibodies
3. Long lasting
4. The ability to manufacture antibodies from being given an antigen by vaccination.
Antibiotics
Drugs that are used to fight infections caused by bacteria. They reduced the mortality rates associated with common infectious diseases and contributed to an increase in the average life expectancy. E.g. penicillin and streptomycin
Types of antibiotics
Bactericidal antibiotics
Bacteriostatic antibiotics
Bactericidal antibiotics
Kill bacteria. Changing the structure of the cell wall or cell membrane. Disrupt the action of essential enzymes
Bacteriostatic antibiotics
Stop bacteria from reproducing/replication or inhibit growth. Disrupt protein synthesis
Antibiotic resistance
If antibiotics are used and some bacteria survive because they are resistant, they reproduce and then future bacteria are also resistant to the antibiotic. Some bacteria are resistant to many known antibiotics in part due to the overuse of antibiotics.
Why don’t antibiotics work on viruses?
They target specific structures or functions that are unique to bacteria and not present in viruses.
1. Viruses lack cellular structures, metabolic processes or bacterial processes (like cell wall synthesis) that antibiotics can target.
2. Viruses take over host cells and antibiotics cannot easily target them without harming the host cell.
Antivirals
Used for treating viral infections. Try to disable viral proteins. Inhibit the development/replication of the virus. Need to be given early after infection
E.g Tamiflu
Immunisation
Programming the immune system so that the body can respond rapidly to infecting micro-organisms. Naturally or artificially acquired.
Vaccination
The artificial acquired form of immunisation through the introduction of antigens to a person so that immunity is acquired without suffering illness.
Vaccine
the antigen preparation used in artificial immunisation.
How vaccinations work
1. Vaccines contain weakened or inactive parts of a particular pathogen (antigen) which are introduced into the body
2. Body manufactures its own antibodies (to combat the antigen) also manufactures memory cells (primary response)
3. Memory cells remain in the body for a long period of time
4. when exposed/infected with pathogen are triggered memory cells
5. produces a faster/larger immune response (secondary response)
6. patients should now not experience illness/experience less severe illness
Types of vaccines
Life Is Tough, Stay Calm, Remain Noble.
Live attenuated
Inactive / dead microbe
Toxoid
Subunit vaccines
Conjugate vaccines
Recombinant vaccines
Nucleic acid vaccines
Live attenuated vaccines
Description | Advantage | Disadvantage | Used against |
Consists of weakened micro-organism with a reduced ability to produce disease symptoms. Immunised person doesn’t contract the disease but manufactures antibodies against it. | Closest to developing natural immunity and long-lasting
| Needs to be refrigerated (not good for remote areas) Can revert to virulent form (risk of residual virulence, especially of immunocompromised people) | Polio
|
Inactive / dead microbe vaccines
Description | Advantage | Disadvantage | Used Against |
Contains either whole or parts of killed virus or bacteria. | Safe and stable - easily stored and transported
| Stimulates a weaker/ shorter immune response. Boosters | Whooping cough. |
Toxoid vaccines
Description | Advantage | Disadvantage | Used Against |
Made from the filtrates of bacterial cultures containing toxins that have been inactivated | Safer | Weaker immune response developed. Requires booster.
| Tetanus
|
Subunit vaccines
Description | Advantage | Disadvantage | Used Against |
Using a fragment of the organism instead of the entire organism. May utilise recombinant DNA technology. | Vaccines safer (not handling the pathogen), fewer side effects and easier to produce | The antigens alone may not be sufficient to induce long-term immunity
| Influenza |
Conjugate Vaccines
Description | Advantage | Disadvantage | Used Against |
vaccine contain pieces of bacterial coat including the carrier protein combined together with polysaccharides. Immune system responds to the polysaccharide rather than the protein | relatively simple production | Lack of a protective immune response in young children | influenzae type b |
Recombinant vaccines
Description | Advantage | Disadvantage | Used Against |
Genetically engineered vaccines where a virus protein is inserted into another virus. A small piece of DNA is taken from the virus or bacterium against which we want to protect and is inserted into a bacteria. The bacteria then produces one of the surface proteins from the bacteria or virus, and this is purified and used as the active ingredient in the vaccine. The surface protein triggers an immune response | can be used by people with weakened immune systems or those individuals with allergies to eggs
| Booster shots to maintain the effect of the vaccine | Recombinant Influenza (Flu) Vaccine |
Nucleic Acid Vaccines
Description | Advantage | Disadvantage | Used Against |
prepared by inserting a DNA sequence (that codes for the antigen) or mRNA into a plasmid and transfected to the host cell. The host cell uses the instructions to produce the antigen protein, which triggers an immune response. | No live components, so no risk of the vaccine triggering disease
| Some RNA vaccines require ultra-cold storage Booster shots. | mRNA – Pfizer COVID
|
Vaccine Schedules
When a person gets their initial shot their immune system will activate a certain number of B-cells which will form antibody producing plasma cells and memory cells (primary response). In most cases, the first dose of the vaccine does not enable enough B-cells to become activated so booster shots are required to activate more B-cells.
The timing of the booster shot is also important – too soon after the first immunization and antibodies present in the blood will be eliminated before more B-cells can be activate
Vaccines to newborns
Vaccination should not start too soon after birth. The child’s blood contains antibodies from its mother. If a newborn is given a vaccine, the antibodies from the mother eliminate the antigens in the vaccine. This occurs before the child’s immune system can mount an immune response.