exam 2 notes
1/161
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
162 Terms
causes and clinical signs for oropharyngeal diseases
causes
dental disease
trauma
foreign bodies
infection
ulcerative diseases
congenital anomalies
neoplasia
signs
reluctance / refusal to eat
abnormal chewing movements
retention of feed “quidding”
protrusion and or swelling of the tongue
drooling and or excessive salivation (ptyalism)*
mandibular / maxillary swelling or drainage
halitosis
examination for oropharyngeal diseases
observation: body condition, drooling, swelling of face or jaw, tongue protrusion, quid’s (feed balls) on ground
give some feed and observe mastication
oral examination
facilitated by sedation
irrigation of the mouth
manual / visual exam
thorough examination requires full mouth speculum and an effective light source, headlamp; mirror
ancillary diagnostics
radiography, CT/MRI, oral endoscopy*
Trauma to oropharyngeal diseases
lips, muzzle, cheek and tongue lacerations
superficial lacerations of lips, muzzle, and cheeks heal well by 2nd intention
primary closure for lacerations breaching oral mucosa
clean, local anesthetic, debride, 2-layer closure, no suture exposed at mucosa
these typically heal nicely due to ample blood supply
large tongue lacerations heal well when sutured; can amputate if needed
to level of frenulum if necessary with little problem
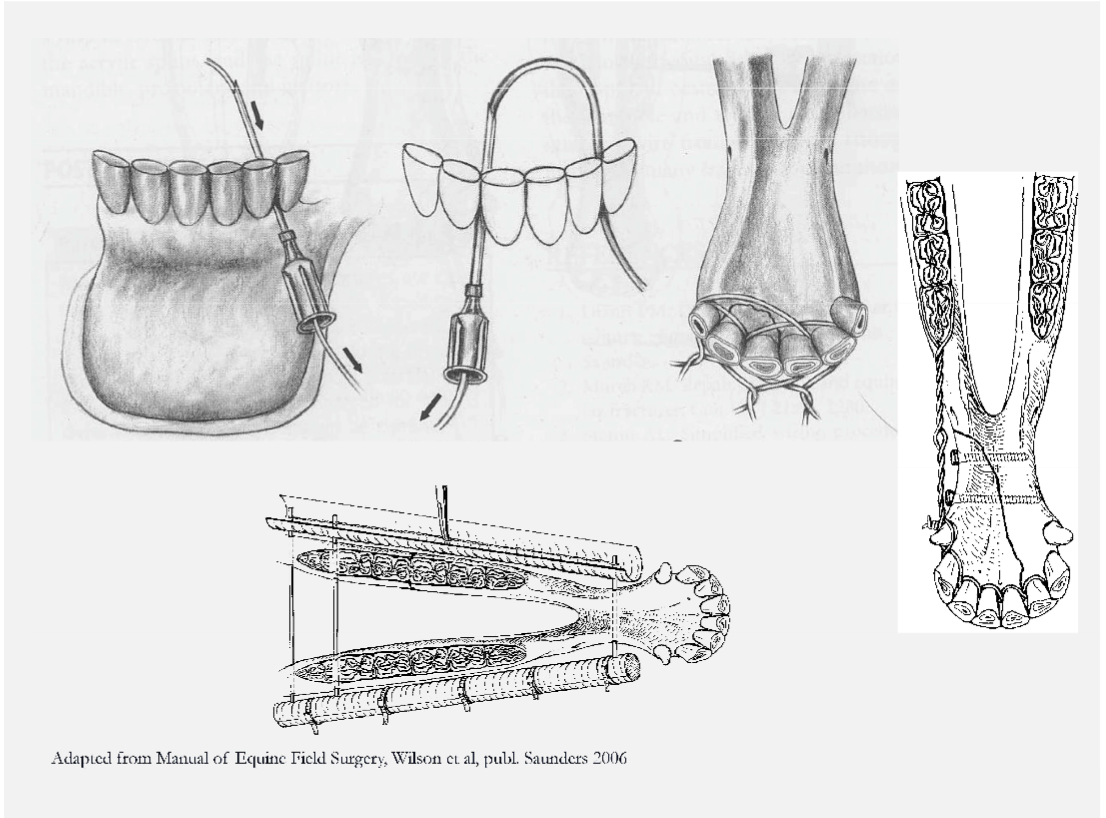
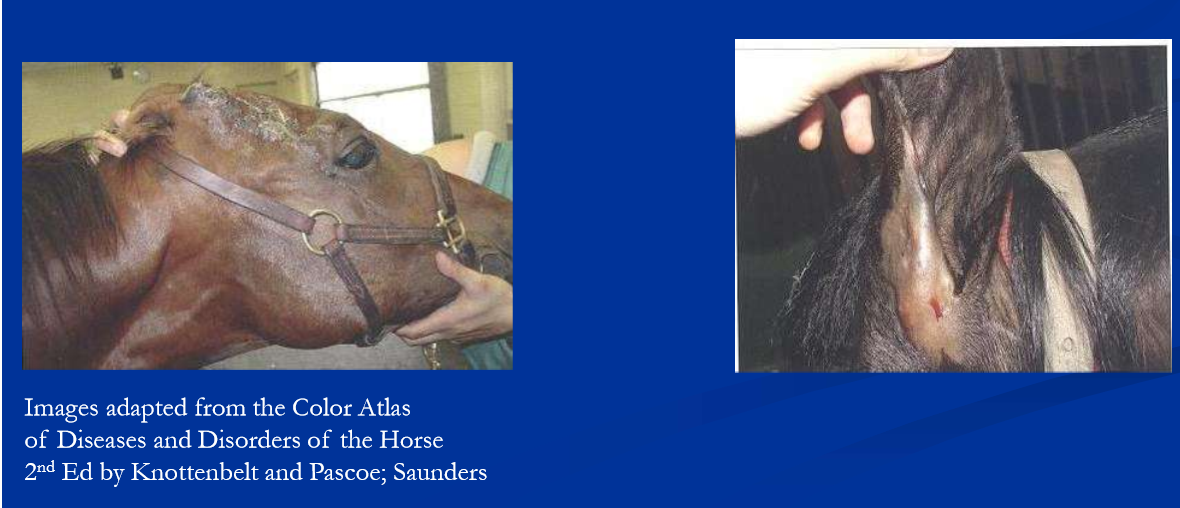
trauma fractures of the mandible and rostral maxilla
kicks, collisions, cribbing, bite injuries, more
can result in fractures of teeth, incisor bone / premaxilla, mandible
fracture configurations range from bone fragments to complex bilateral fractures
signs are drooling, lack of feed intake, mal-alignment and or instability, crepitus, soft tissue swelling, malodorous with time
generally can be managed / repaired with good results
some mandibular fractures are simple bone fragments
may present as sequestrum with draining tract
surgical removal and curettage
minimally displaced unilateral fractures of mandibular bars
managed conservatively with soft feeds, oral rinses, time
instability, malocclusion and bilateral fractures need stabilized
intraoral wiring for loose incisors, fractures of incisive bone / premaxilla and rostral mandible
wiring, bone screws and plates and external fixation for more complex and or caudal fractures
Oropharyngeal foreign bodies
grass awns, splinters, and wires
may locate in lingual, sublingual, intermandibular tissues, buccal recesses, hard palate, soft palate, pharynx
results and signs can include
stomatitis, glossitis, cellulitis, abscess
salivation, halitosis, eating difficulties, feed refusal
careful oral exam using speculum, light source, palpation; radiogrpahy and endoscopy
removal followed by systemic antibiotics if indicated, NSAID, repeated oral lavage

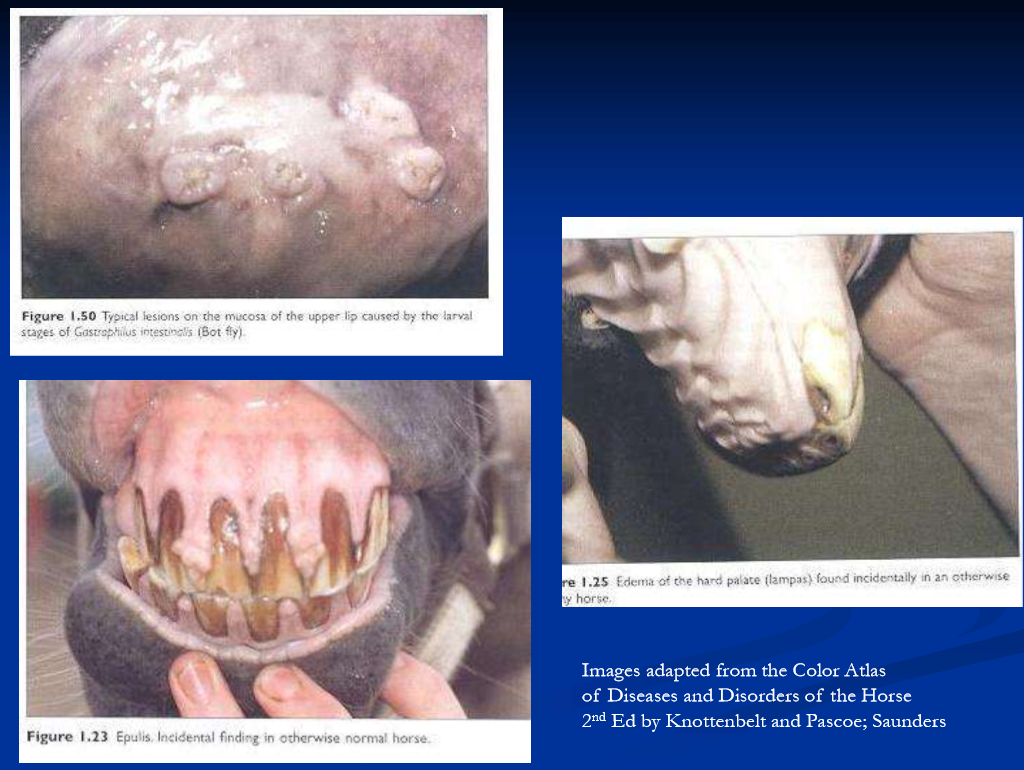
other causes of stomatitis / glossitis
dental points cause tongue / check lacerations; common
parasite larvae: Habronema, Gasterophilus, Helicocephalobus,
Gastrophilus larvae cause stomatitis characterized by ptyalism; all may cause labial / oral granulomas
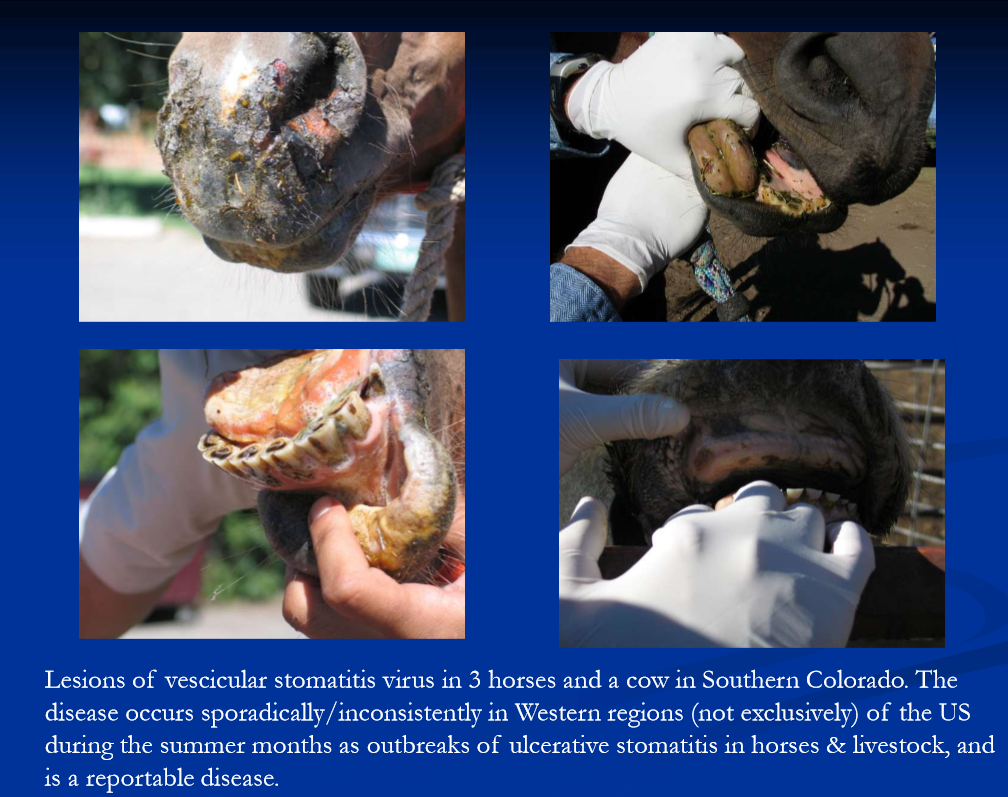
oral ulcers: blister beetles, vesicular stomatitis virus, NSAID toxicity, caustic ingestion, uremia
epulis: gingival hyperplasia associated with chronic irritation example erupting permanent teeth / caps
lampus: benign swelling of hard palate caudal to incisors; eruption of permanent incisors or idiopathic
manage inflammatory / ulcerative / infectious with oral rinses / lavage, NSAIDs, systemic antibiotics if indicated
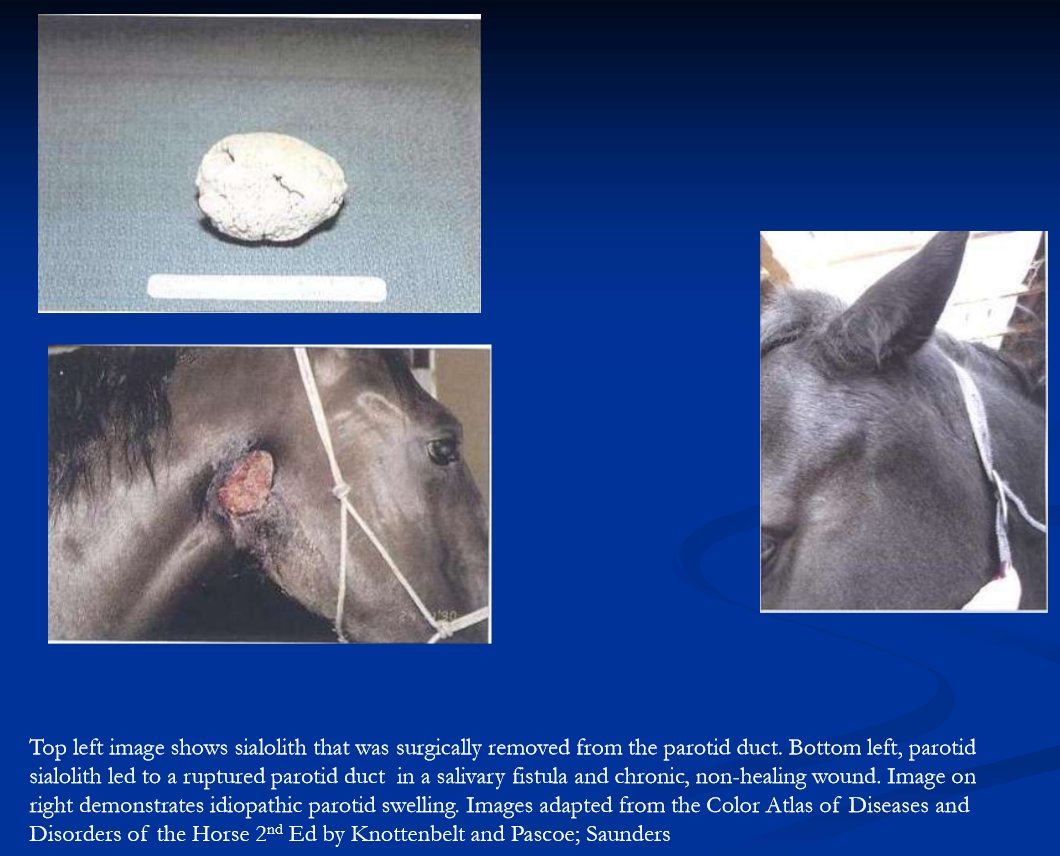
salivary gland disease
Sialoliths: may lead to duct rupture, fistula; sx removal
trauma/lacerations of parotid gland and or duct
lacerated gland, duct/branches may result in salivary fistula
repair severed/lacerated parotid duct if possible
can be corrected with dissection and repair
gland can be destroyed chemically if needed
obstruction of sublingual ducts mucoseal; marsupialize
slaframine toxicity common in some areas
Red clover infected with Rhizoctonia legumencola
Herd outbreaks of ptyalism
remove from source
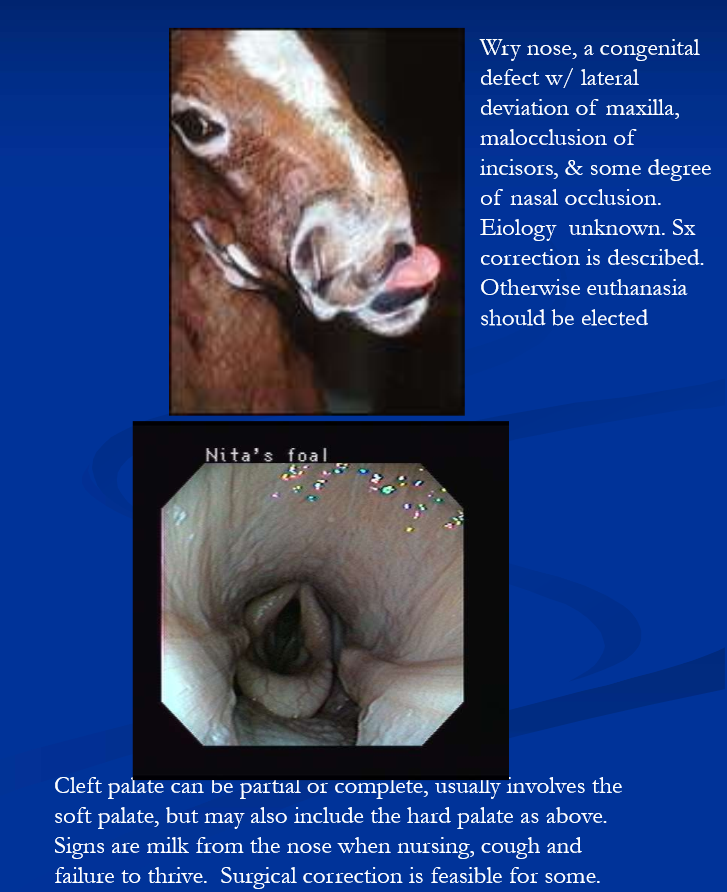
congenital oropharyngeal defects
Cleft palate, tongue, mandible
wry nose
dental anomalies (more later)
parrot mouth (overbite)
sow mouth (underbite)
shear mouth
oligodontia
supernumerary teeth
dentigerous cysts

developmental anomalies of teeth
Oligodontia, supernumerary teeth, crowding of teeth
parrot mouth: maxillary prognathism (or inferior brachygnathism); maxilla protrudes beyond mandible
severe overbite is a
major unsoundness
possibly heritable
corrective orthodontics sometimes performed
sow mouth; mandibular prognathism (or superior brachygnathism)
lower jaw extends beyond maxilla; “underbite”

dentigerous cysts
developmental anomaly; cystic structures in soft tissue over maxilla or mandible, often containing fragments of teeth
often found at base of ear and are presented as draining tract
Oropharyngeal neoplasia
melanoma at commissures
squamous cell carcinoma
less common
bone tumors: benign types are ossifying fibroma, osteoma; osteosarcoma is rare but majority occur in the head
ossifying fibroma in foals/yearlings; usually mandibular; resection via hemi-mandibulectomy; radiation also
primary dental tumors: odontoma, ameloblastoma
tx and px depends on location and histological diagnosis

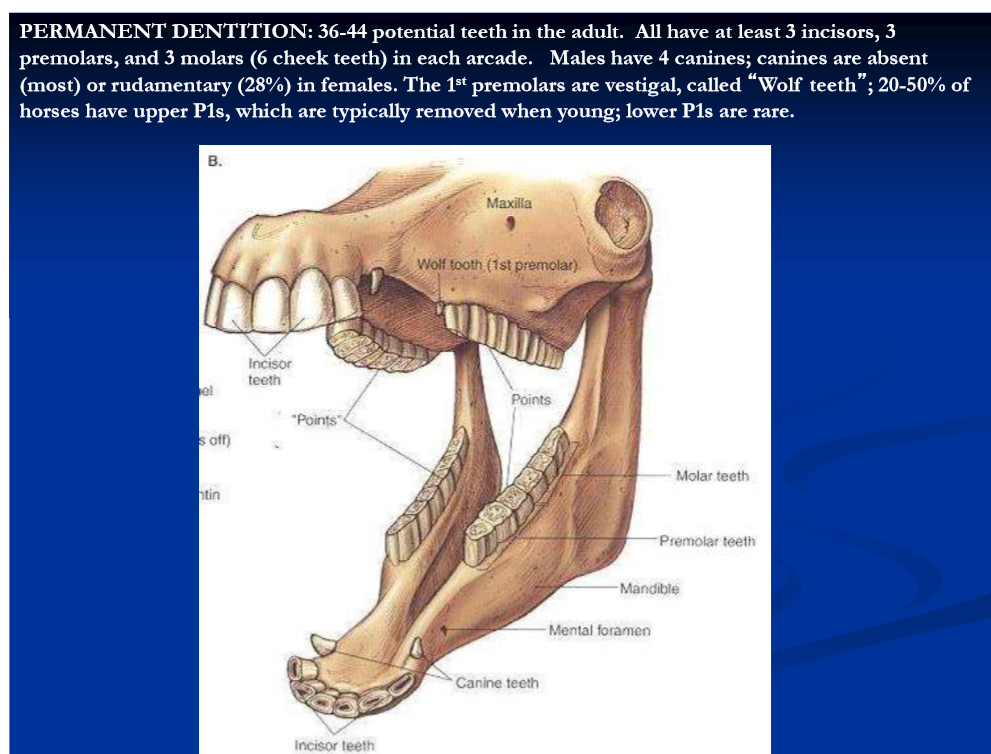
form and function of equine teeth
Hypsodont teeth
long crown, short roots, enamel extends below gum line
incisors grasp, tear and pull the grass
cheek teeth are made for grinding the grass
growth of crown continues until 6-9yr
wear occurs at rate of 2-3mm / yr
reserve crown in alveolar bone erupts continually throughout adult life in response to wear, thus maintaining occlusion
length of reserve crown decreases gradually with this process; aged horse become “smooth mouthed”
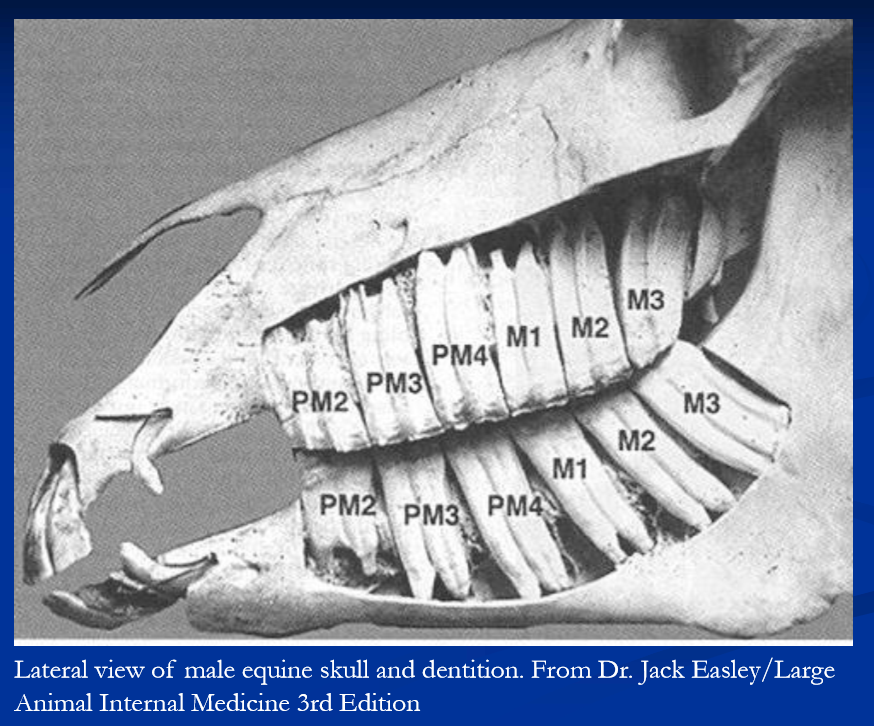
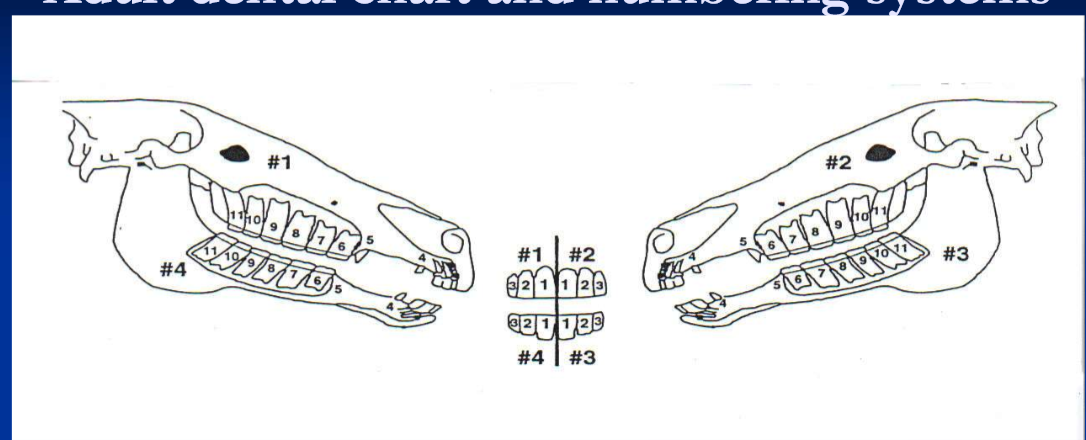
adult dental chart and numbering systems
anatomic: I1-3, C1, P1-4, M1-3
Triadan: quadrants 1-4; upper right = 1, upper left = 2, lower left = 3 and lower right = 4; teeth numbered 1 to 11 in each quadrant.
for example 1st upper right incisor is 101, last lower left molar is 311
for deciduous teeth the quadrants are 5-8
deciduous teeth
24 in total
the deciduous teeth are incisors and premolars; there are no deciduous molars
at 6 months there are 3 deciduous incisors and 3 premolars in each arcade; 4×6 = 24 teeth total (excluding any wolf teeth)
deciduous teeth are white with narrow neck
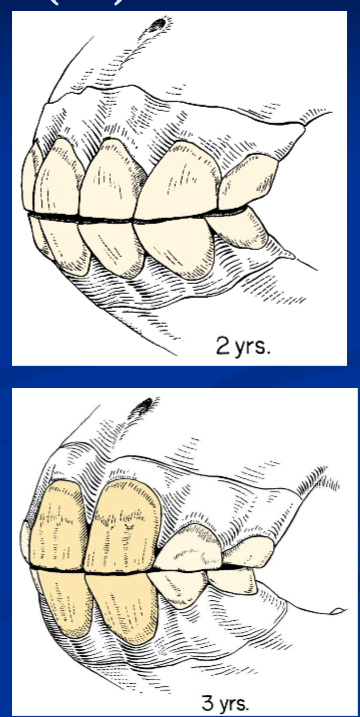
eruption times for permanent teeth
permanent incisors (I1-3) erupt at 2.5, 3.5, 4.5 years
eruption times useful in aging young horses
canine (C1) at 4 to 5 years (all males, some females)
premolars: 2.5, 3 and 4 years for P2-4
(wolf teeth (P1) at 5-6 months when present)
molars (M1-3) at 1,2 and 3.5 to 4 years
clinical signs of dental disease
weight loss
biting problems
reluctance to eat
retention of hay in the cheeks
quidding
tilting head when chewing
halitosis (bad breath)
bloody saliva
facial/mandibular swellings
drainage from maxilla or mandible
malodorous, unilateral purulent nasal discharge
routine dental care
exam at birth: occlusion, congenital defects
exam 1-2x yearly as part of routine prevention
depending on age, diet, pre-existing problems
“floating” to remove points and hooks on cheek teeth
wolf teeth: usually removed at 1-2 yrs of age
dental caps: deciduous teeth being shed as permanent erupts; remove if/when retained, especially premolars
upper and lower P2s sometimes contoured for “bit seat”
canine teeth: file down if sharp
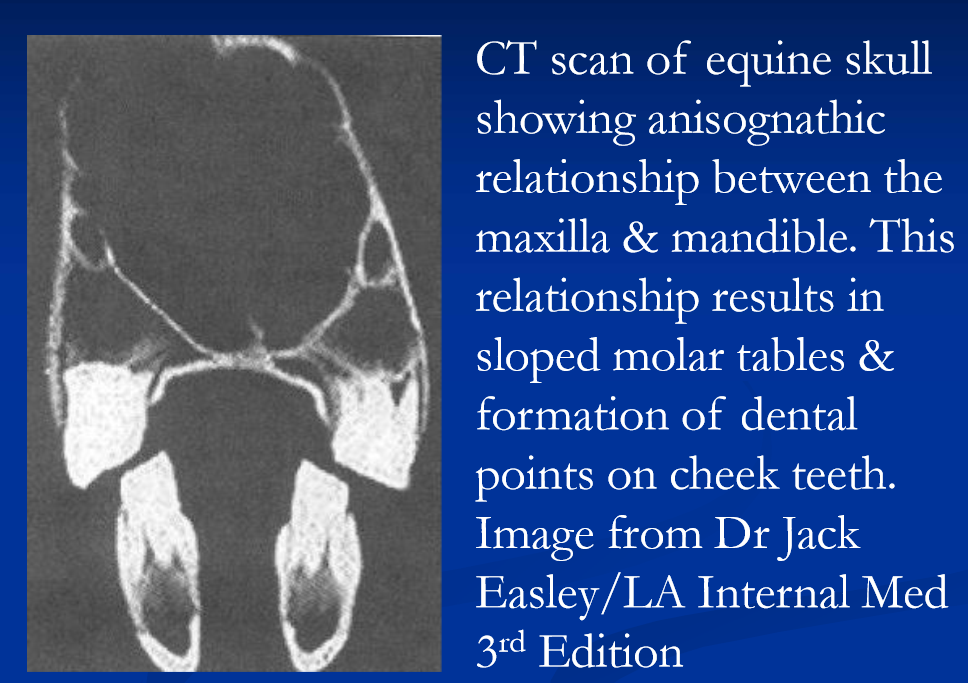
points and hooks
horses have prominent anisognathism; bottom jaw is narrow compared to upper
mastication results in sloped arcades of cheek teeth
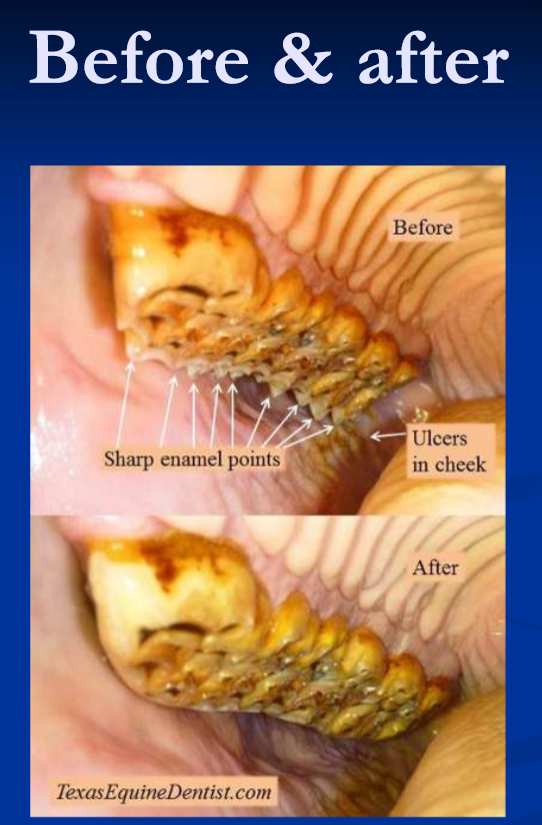
sharp enamel “points” form on outside uppers and inside lowers; lacerations / ulcers on tongue and cheeks
“hooks” form on upper P2 and lower M3
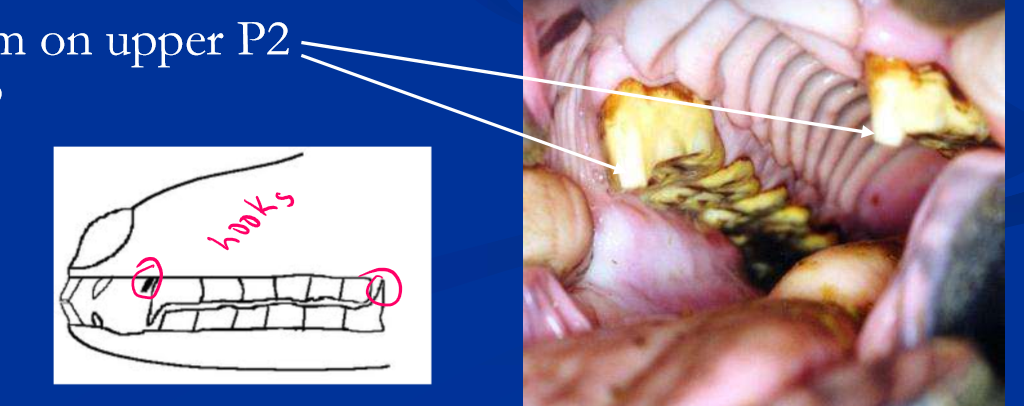
floating teeth: rasping / filling to remove points and hooks
as needed in young horses with deciduous and erupting cheek teeth
once annually for pastured horses
2x/yr for stabled horses
as needed for horses with malocclusions, missing teeth
hand floats or power instruments; careful with power float thermal injection
Incisor abnormalities
retained deciduous incisors may lead to caudal displacement of permanent teeth
extraction of deciduous tooth indicated
trauma to incisors
remove loosened deciduous incisors to protect permanent tooth bud
if permanent incisor, stabilization should be attempted
mandibular and maxillary fractures can displace or destroy tooth buds of permanent teeth
fractures: many are non-problematic but
may involve associated boney structures, requiring fracture stabilization
pulp infection may occur can be managed with endodontics (vital pulpotomy / “root canal”); otherwise may require extraction
extraction of incisors
involves chemical restraint local anesthesia, incision of gingiva directly over root, loosen periodontal ligament, complete extraction of root
need to keep opposing tooth reduced over time
mal-alignment of incisor teeth
smile, frown, and tilt contours are associated with cheek teeth abnormalities
addressing malocclusion of cheek teeth is the key; rasping to change incisor contour is questionable
steps are overgrowth of individual incisors from absence or displacement of opposing tooth; regular rasping to keep level

canine teeth
Blind (un-erupted) canine teeth
may cause mucosal irritation/ulceration and biting problems in 4-6yr old males/geldings, occasional female
incision over the un-erupted end encourages eruption
elongated or sharp canine teeth
may cause bit problems
sharp canines enhance bite injuries
can be filed or cut
very rarely a canine tooth requires extraction
due to fracture below the gum line and death of the tooth
canine extraction is difficult such that removal of a healthy canine should be avoided; bone flap approach
wolf teeth
vestigial 1st premolar
may cause bit problems if loose or sharp
routinely extracted at 1-2yrs; loosen with periosteal elevator, extract with forceps
“Blind” wolf teeth may cause subgingival enlargement and bit problems; remove surgically if needed

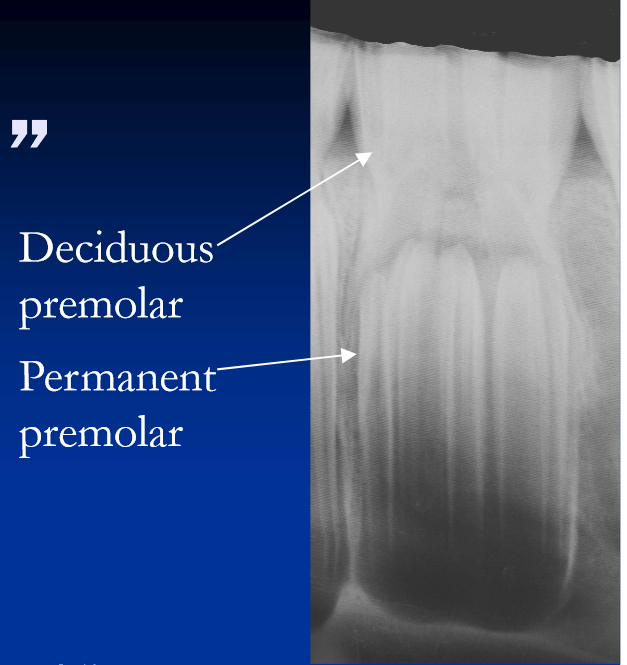
Premolar “caps”
Deciduous premolars being shed as permanents erupt
these are usually shed naturally; however
permanent P3 and P4 erupt at 3 and 4 years and are prone to crowding with retention/delayed shedding of caps
erupt between permanent P2 and M1 which are already in place
retained premolar caps
may cause a localized gingivitis
often cause painless bony swelling around alveolus (“eruption pseudocyst”)
these usually resolve with shedding / removal
remove caps if they are truly retained

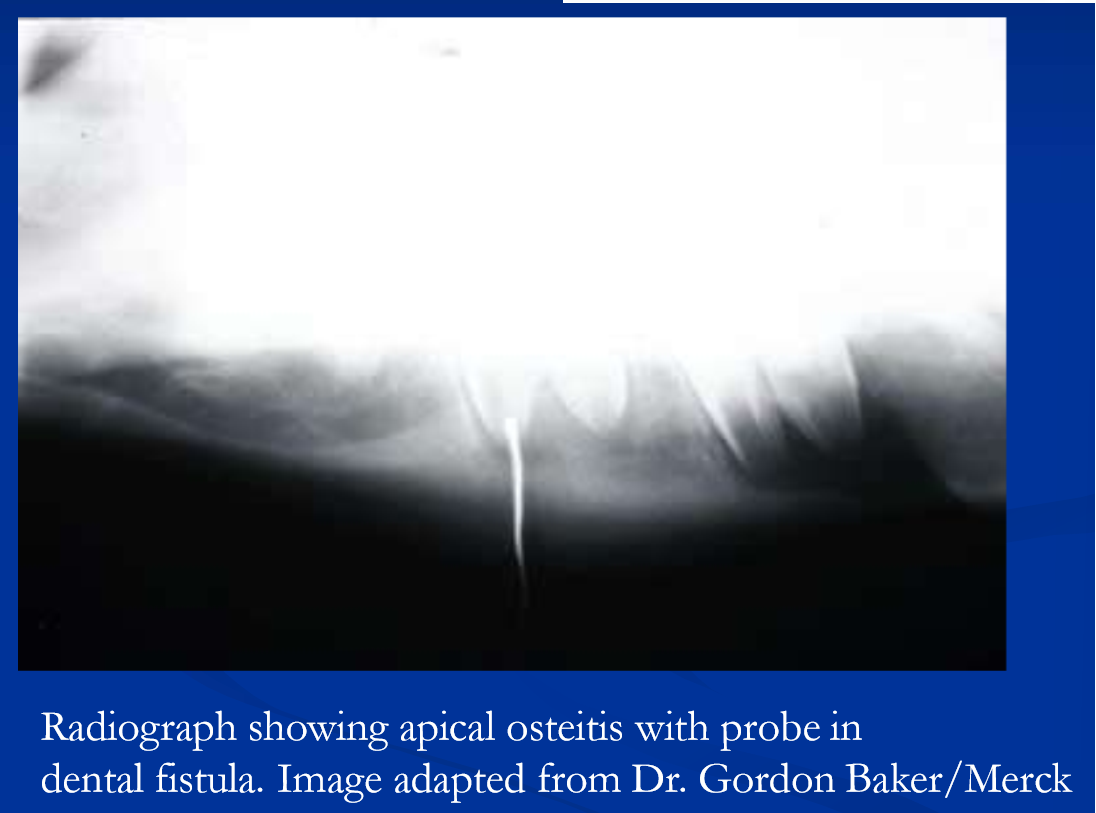
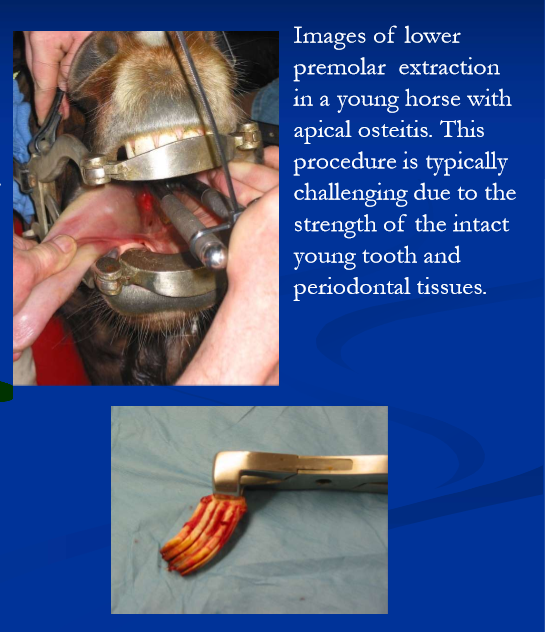
retained premolar caps and apical osteitis
persistently retained caps at P3/P4 can lead to impaction and or displacement of permanent P3/P4
with impaction there is expansion within the alveolus, lysis of supporting bone, and painful bony swelling around apex
with progression the apex and surrounding alveolar bone can become infected (apical osteitis) and eventually the pulp
management of retained caps and apical osteitis
remove retained cap(s)
± oral antibiotics based on presence / absence of painful bony swelling for example sulfas and metronidazole
advanced infection leads to draining tract (mandible) or sinusitis (maxilla) and requires more aggressive intervention
curettage of draining mandibular tracts
sinus irrigation with maxillary sinusitis
systemic antibiotics, often long term
root end resections and apical seal are options
extraction needed if fails to resolve
Dental decay / caries
occurs most commonly at the occlusal surfaces of the caudal upper cheek teeth within the infundibula
superficial decay at the surface of these teeth is common / typical generally non-problematic
horses with unusually deep infundibula are prone to more extensive caries that can weaken tooth, promote infection of pulp cavity
larger / persistent caries and infection
weakens the tooth, predisposes to splitting / cracking
infection may extend to root (apices)
endodontic techniques can be employed to seal caries
advanced dz requires extraction of tooth / fragments
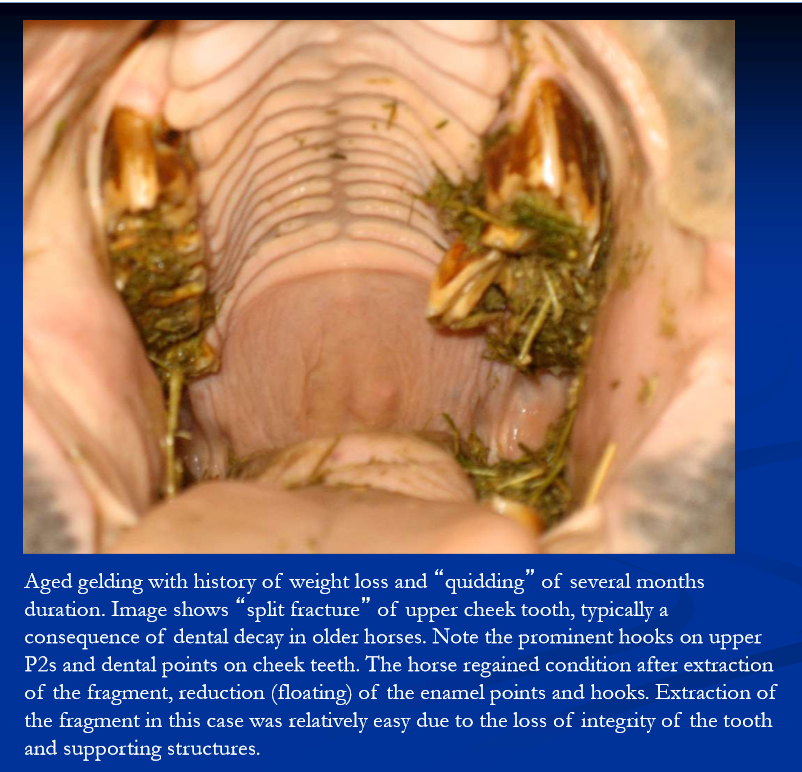
Extraction of cheek teeth
indications include infection, fracture, loose tooth, malposition, dental tumors
extraction can be challenging depending on age of horse, and nature extent and location of disease
intraoral extraction preferred; sinus trephination or sinus flap with repulsion, and lateral buccotomy, are more challenging and prone to complications
Malocclusions of the cheek teeth
wave mouth:
older horses, usually at P4-M1; manage with regular floating
step mouth:
“overgrowth” of cheek tooth because opposing tooth is absent; manage with cutting and or frequent rasping
shear mouth:
excessive angle of the upper and lower occlusal surfaces; related to narrow mandible; causes “tilt” profile of incisors
creates razor sharp teeth causing lacerations of tongue and cheeks; frequent floating of cheek teeth
smooth mouth
extreme wear of crown surfaces in older horses; pelleted feeds and removal of points
Periodontal disease
generally the result of malocclusions
missing teeth, mispositioned teeth, wave mouth, shear mouth, step mouth, large hooks
result in diastema, spaces between teeth that trap feed
progressive inflammation of the gingivae results in
resorption of alveolar bone, degeneration of periodontal membrane, pocket formation and loosening of the tooth
chronically there is tooth decay and tooth loss; also can lead to osteomyelitis of supporting bone
prevention: regular exams / dentistry to maintain normal occlusion
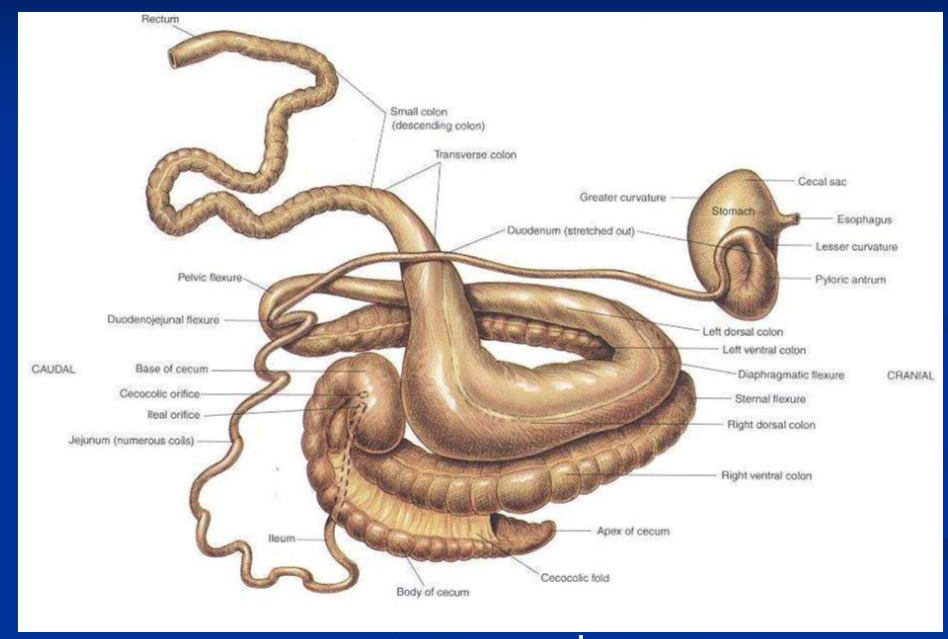
colic in horses
colic = abdominal pain
common but non-specific clinical signs in horses
multiple etiologies and severity
gastrointestinal: many conditions, stomach to rectum
non-GI: peritoneum, liver, urinary and repro tracts
“false colic” signs misinterpreted as abdominal pain, example rhabdomyolysis
accurate diagnosis requires
knowledge of GI structure and function
understanding of pathophysiology of intestinal diseases
systematic approach to examination
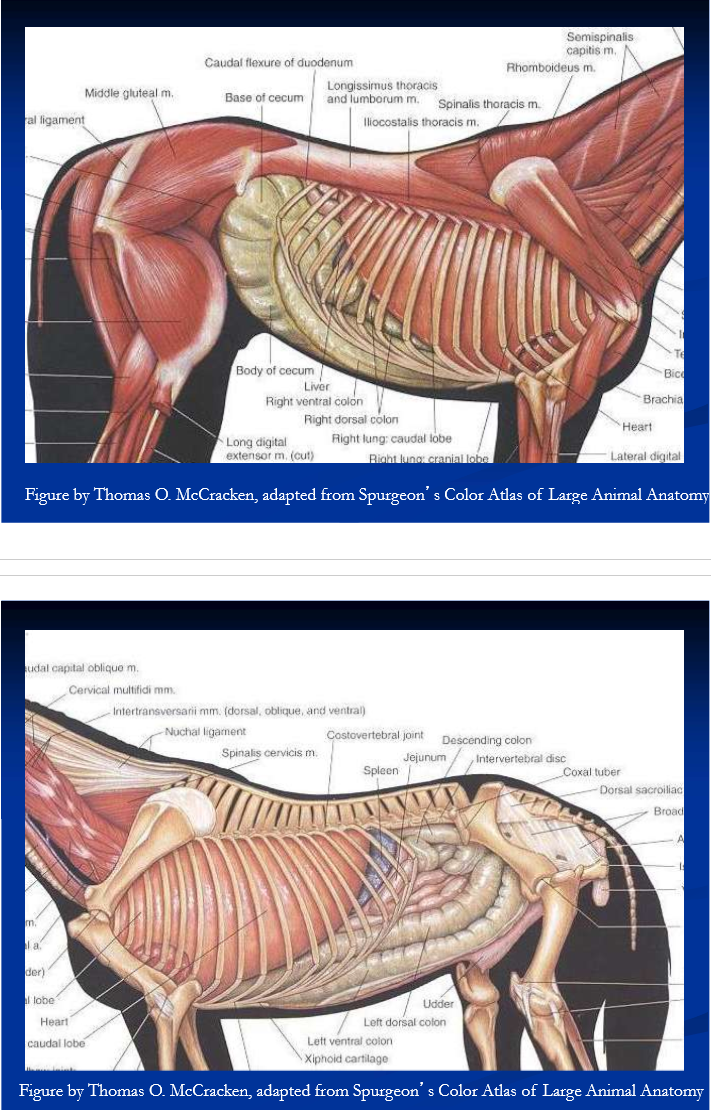
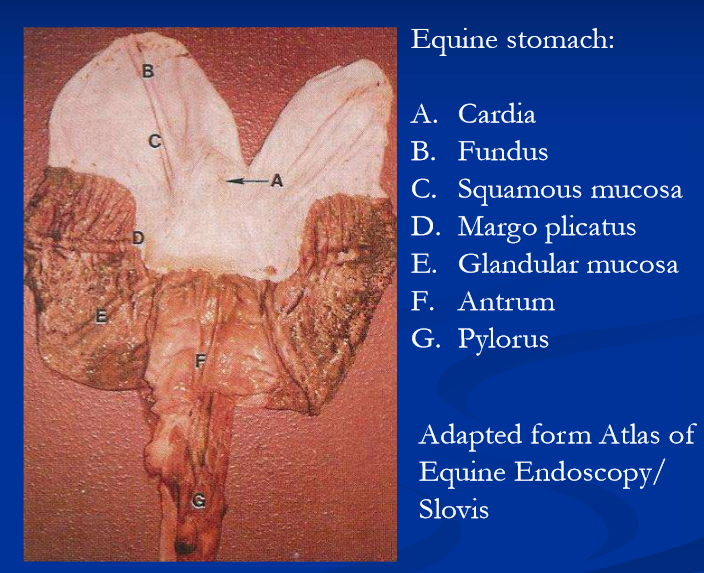
anatomic and physiologic predispositions to GI disease
the stomach is predisposed to gastric dilatation and rupture because the cardia is “one-way valve”
the small intestine is prone to incarceration and strangulating obstructions
large intestines:
important in water balance and nutrition, prone to acute inflammation leading to large fluid loses and PLE
prone to luminal obstruction, displacement, strangulation, and infarction
small colon: prone to intraluminal obstruction, vascular injury
motility patterns, natural openings and blood supply play roles in predispositions to obstruction and ischemic injuries
Mechanisms of intestinal pain
Distension / stretching of intestinal wall
gas, fluid or ingesta; pain receptors in wall
stretching / tension of the mesentery
ischemia
incarceration, strangulation
vascular spasm / thromboembolism / infarction
acute inflammation
intestinal mucosa / wall: enteritis (SI), typhylocolitis (LI)
serosa: peritonitis
mechanisms of intestinal injury: obstruction
anatomical obstructions
simple obstruction
intra-luminal blockage and non-strangulating displacements
causes intestinal distention, tension on mesentery
strangulating obstruction
simultaneous occlusion of the intestine and blood supply
ischemia is usually acute, severe and rapidly progressive, with loss of bowel integrity and progression to devitalization, perforation
torsion, volvulus and incarceration / strangulating entrapment
mechanisms of intestinal injury; inflammation
acute inflammation of the SI causes
Ileus (functional obstruction) fluid accumulation, SI distention, enterogastric reflux, gastric distension, abdominal pain, endotoxemia
acute inflammation of the LI is common and causes
Ileus, fluid leakage and or secretion into lumen, diarrhea and fluid loss, PLE, abdominal pain, endotoxemia
chronic inflammation of SI and or LI causes
malabsorption/ maldigestion, weight loss, sometimes hypoproteinemia
chronic, low volume diarrhea with LI
mechanisms of intestinal injury: non-strangulating ischemia and infarction
classic cause is verminous arteritis associated with S. vulgaris larvae in cranial mesenteric artery and branches
larval activity causes ischemia via arterial spasm, stenosis, and or thromboembolism
results in recurrent transient ischemia and pain or
infarction bowel injury, necrosis secondary peritonitis / perforation

pathophysiology of intestinal disease: cardiovascular compromise
persistent and or progressive intestinal injury and abdominal pain result in circulatory shock due to:
Hypovolemia*
cessation of fluid intake
increase in insensible losses
fluid loss into intestinal lumen
strangulation obstruction
endotoxemia: cardiovascular effects of endotoxin*
depression of myocardial fx, loss of peripheral vascular tone/control (capillaries) => distributive shock
prominent with acute inflammatory or ischemic conditions
Primary (intestinal) endotoxemia
endotoxin is the lipopolysaccharide (LPS) component of the outer cell membrane of gram-negative bacteria
LPS is released into the intestinal milieu during normal reproduction and death of G-negative enteric bacteria
in healthy animals, small amounts of endotoxin cross the GI mucosal barrier and enter the portal circulation
scavenged and eliminated by Kupfer cells in the hepatic sinusoids
Endotoxemia
Excess amounts of endotoxin in the systemic circulation (endotoxemia) occur via:
gram negative infection (G-neg sepsis)
primary / intestinal endotoxemia*
absorption of excess endotoxin and other bacterial products across damaged GI mucosal barrier, into portal circulation and or peritoneum
occurs especially when there is inflamed or injured bowel
primary / intestinal endotoxemia is common in horses
GI dzs leading to inflammation and or injury are common
horses are highly sensitive to the pathophysiologic effects of endotoxin
endotoxin interacts with mononuclear phagocytes and endothelial cells causing
widespread activation of the arachidonic acid cascade, massive release of pro-inflammatory cytokines, loss of vasomotor control and activation of the clotting cascade
results in a systemic inflammatory response syndrome
characterized by hypotension, poor tissue perfusion, lactic acidosis and coagulopathy
the terminal events are circulatory failure and DIC
primary (intestinal) endotoxemia
simple GI stasis increases the amount of endotoxin absorbed across the GI mucosa
GI distention, ischemia and or inflammation lead to
breakdown of the intestinal mucosa, resulting in
absorption of excess endotoxin across the bowel wall into the portal circulation
also enter peritoneal cavity when bowel wall is injured, taken up in circulation
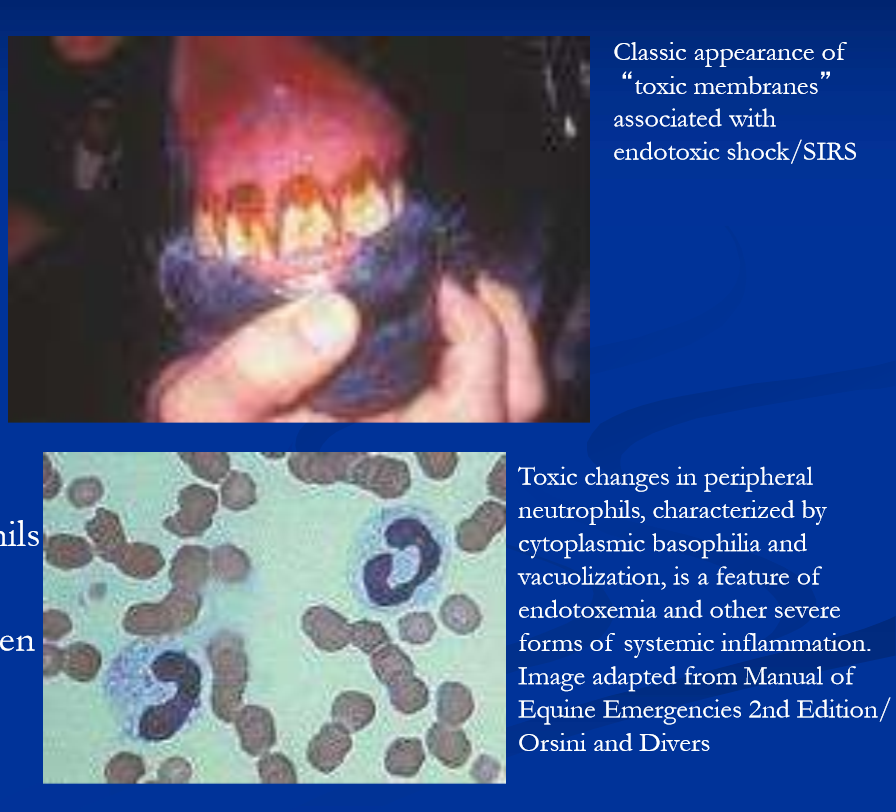
Clinical manifestations of endotoxemia
depression
fever
abdominal pain
tachycardia
increased CRT, weak pulses
“toxic “ membranes
hemoconcentration
neutropenia
left shift
toxic change in neutrophils
thrombocytopenia
consumption of fibrinogen
increased clotting times
clinical signs of abdominal pain
restlessness
curling the upper lip
stretching
looking at flank
pawing the ground
kicking at abdomen
crouching
dog sitting
lying down
rolling
tachycardia and tachypnea
sweating
fasciculations

Diagnosis for colic you need to do
thorough examination including
consideration of age, sex and breed
current and past medical history and preventive care
physical exam aimed at determining
the affected segment the intestinal tract
stomach, SI, LI, small colon or extra - intestinal
the nature and severity of the disease process
simple obstruction, strangulating obstruction, inflammation
cardiovascular status of the horse
Age, sex and breed predispositions with colic
Newborn foals
meconium impaction
enterocolitis
uroperitoneum
weanlings / yearlings
gastric ulcers
ascarid impaction
umbilical hernia
SI intussusception
foreign body
adult horses in general
spasmodic
flatulent
gastric ulcers
impaction of large intestine
large colon displacement / volvulus
SI strangulations
typhlocolitis
verminous arteritis
brood mares
parturition, uterine torsion, large colon displacement, large colon torsion / volvulus
stallions
inguinal hernia (common), testicular torsion (rare)
older horses, esp obese
strangulating pedunculated lipoma
miniature horses especially youngsters
large and small colon impaction with sand, dirt, hair and foreign material (bedding)
history for colic
history of current episode
duration, severity and progression of current signs
events surrounding the current episode
appetite, fecal production, water intake/access
response to treatment
prior history and management
use, housing / environment, diet and water source
preventive health care: teeth, parasite control / deworming
changes in management / environment
previous colic or other medical problems
drug history-examples NSAIDs, antibiotics
examination for colic
physical examination aimed at assessment of general condition, severity of pain, GI and cardiovascular status
nasogastric intubation
gastric dilatation and reflux are generally indicative of primary gastritis or SI obstruction
abdominal palpation per rectum can detect anatomical abnormalities
abdominal ultrasound to visualize abdominal structures
abdominal paracentesis can detect bowel compromise and or peritonitis (belly tap)
abdominal palpation per rectum
may differentiate between medical and surgical conditions
use a systematic approach
landmarks / normally palpable structures are the aorta, cranial mesenteric artery, cecal base and ventral cecal band, pelvic flexure, spleen, and left kidney, urinary bladder, inguinal rings in stallions and geldings, ovaries and uterus in mares, peritoneal surfaces
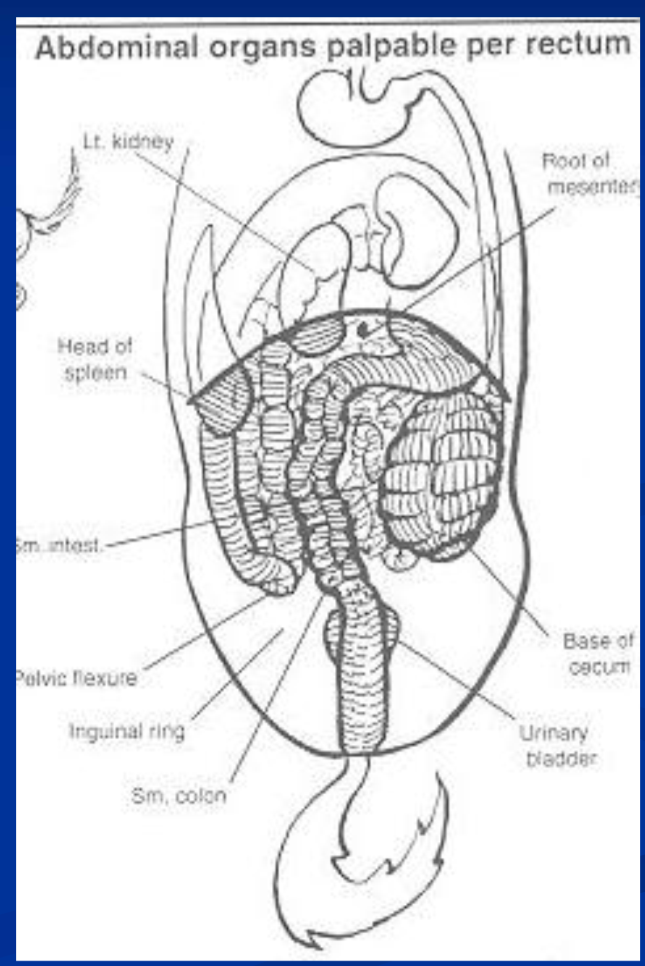
abnormalities seen with colic
dry or absent fecal balls in rectum / small colon
fecal masses of LI, cecum, or small colon
bowel distention; large versus small intestine
tight mesenteric bands
displacement of the spleen
large colon displacements and strangulations
abnormal peritoneal surfaces
abdominal masses
abdominal ultrasound
may differentiate between medical and surgical conditions
trans-abdominal and trans-rectal
detectable abnormalities include
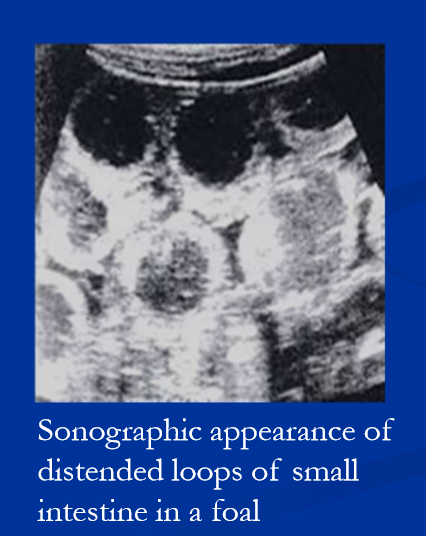
small or large intestinal distention
changes in wall thickness
large colon displacements
sand accumulation in the large colon
small intestinal intussusceptions
inguinal hernia
enterocolitis
right dorsal ulcerative colitis
peritonitis, abdominal hemorrhage
clinical pathology with colic
PCV and total solids help assess hydration / circulatory status; reflect protein losing enteropathy if present
WBC will indicate stress, inflammation, infection and or endotoxemia, aiding diagnosis
biochemical profile, electrolytes, blood gases, and lactate
provides assessment of circulatory status, guides fluid therapy
evaluation of organ function
peritoneal fluid analysis* to assess intestinal integrity; also reflective of extra-intestinal disease
peritoneal fluid analysis for assessment of bowel integrity / intestinal compromise
normal peritoneal fluid is light yellow and clear, WBC <5000/ul, protein <2.5g/dl
generally remains WNL with simple LI obstructions
vascular comprise (prolonged distention, incarceration, strangulation) leads to progressive changes
serosanguinous color (RBCs)
increases in WBC and protein (turbidity)
toxic changes in neutrophils as bowel wall becomes compromised (leakage of endotoxin)
dark fluid as bowel becomes necrotic, degenerate neutrophils
brown or green color, bacteria and plant material when bowel ruptures

principles of intervention with colic
relief from pain
analgesics: xylazine / butorphanol, flunixin; detomidine
gastric decompression, cecal trocharization
cardiovascular stabilization
volume expansion with IV fluids
counteract effects of endotoxin
fluids, flunixin, plasma, polymyxin B
ultimate goal: establish patent, functional intestine
fluids, laxatives and cathartics
surgical intervention (laparotomy)
Indications for surgical exploration with colics
Clinical signs and progression are monitored over time
duration, severity and progression of pain, response to analgesics, rectal examination findings, naso-gastric intubation, peritoneal fluid analysis, and cardiovascular status
surgical intervention is indicated with
progressive, severe and or unrelenting pain
obvious surgical lesion detected on rectal exam or US
progressive changes in abdominal fluid
progressive cardiovascular deterioration
unsatisfactory response to medical management
pre-surgical and anesthetic considerations
stabilize CV status prior to induction
horse is compromised, anesthesia causes further hypotension
volume expansion / perfusion
peri-operative antibiotics, anti-inflammatories
penicillin-gentamicin, flunixin
consider renal perfusion/function when giving these drugs
NG tube in place
Xylazine-ketamine-GG / diazepam induction, maintained on gas; goals are to maintain BP and limit time under anesthesia, myopathies are the primary risk
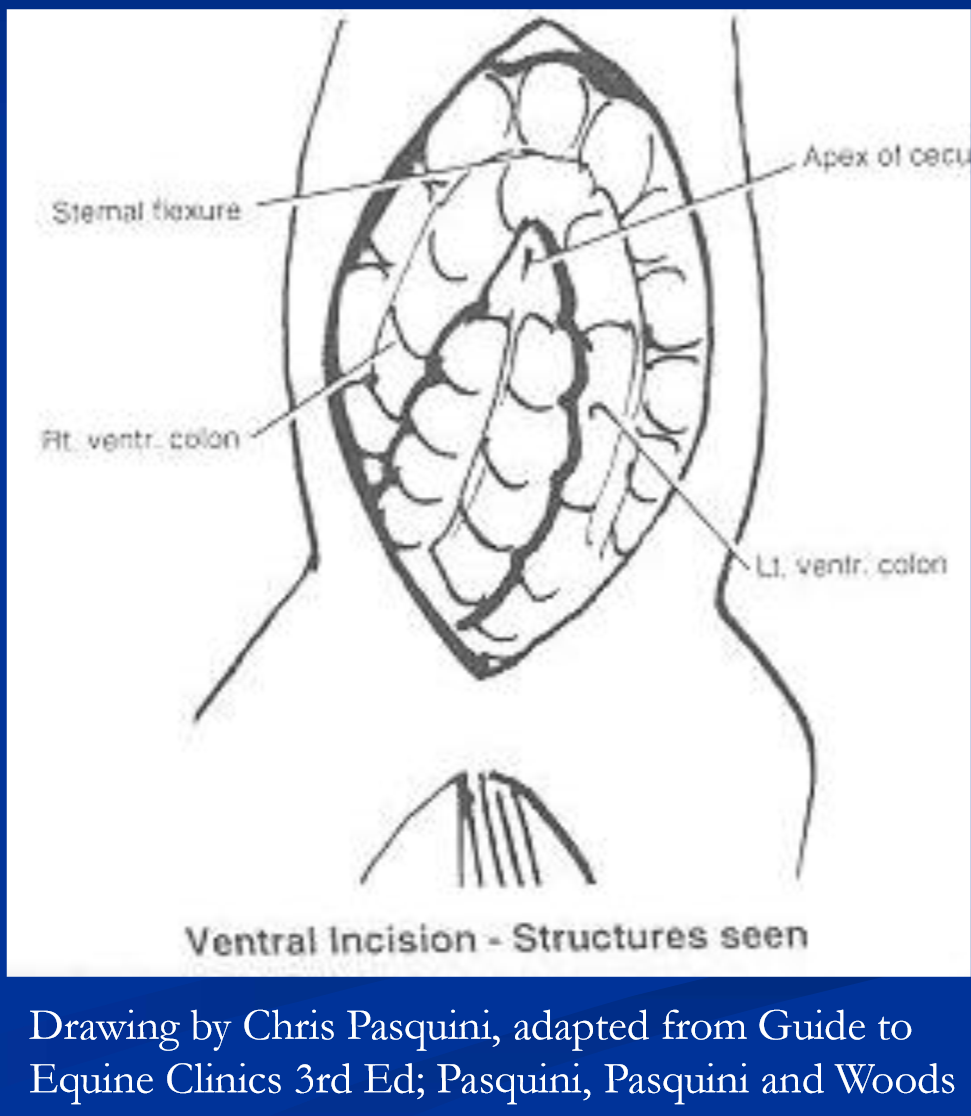
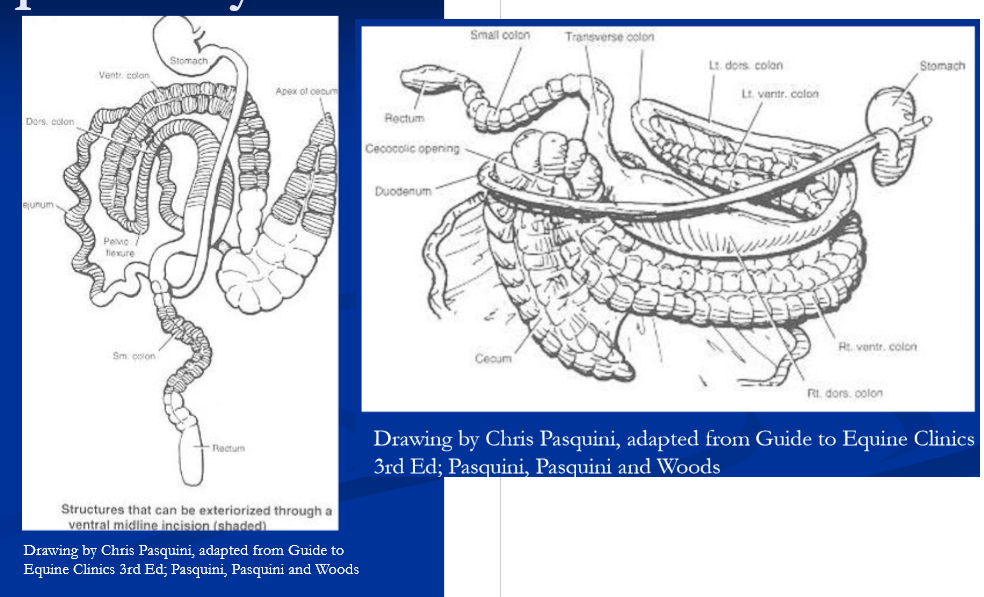
Exploratory laparotomy
ventral midline incision, xyphoid to umbilicus
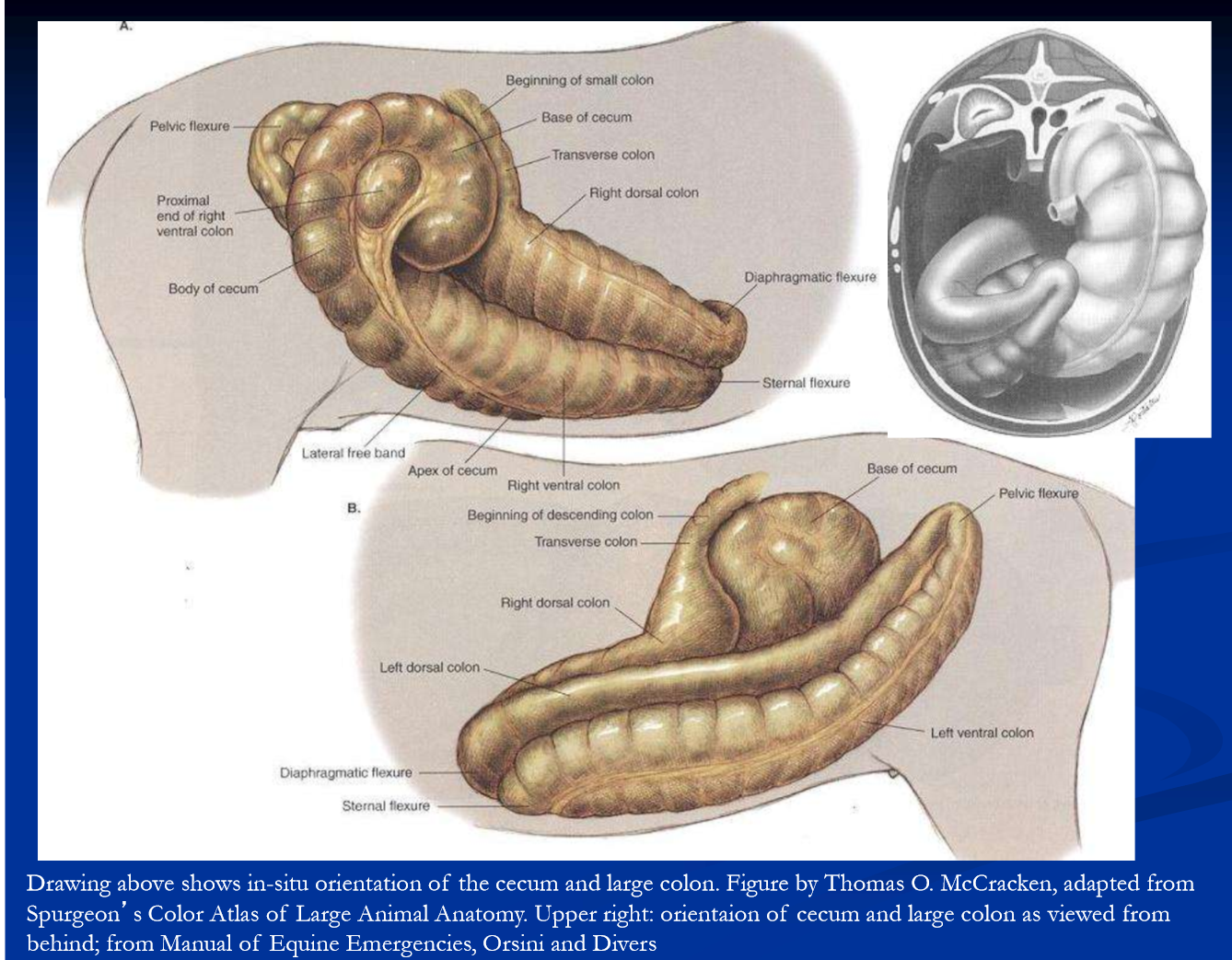
initial inspection: apex of cecum should be on ventral midline, surrounded by ventral colon / sternal flexure
look for discolored peritoneal fluid, fibrin on serosal surfaces, ingesta free in peritoneum
decompress any distended intestine
problem may be evident on initial inspection
explore further by sweeping hand over viscera in all quadrants
looking for distended loops of bowel, tight mesenteric bands, firm ingesta/fecal masses intra-abdominal masses
detailed exploration
feel root of mesentery and connections of cecum and colon for volvulus
LI: check position by starting at cecum → ventral colon → pelvic flexure; nephrosplenic space
run SI, palpate liver, right kidney, epiploic foramen
exteriorize the colon and examine
palpate / examine small and transverse colons
decompression of distended SI and
resection-anastomosis if needed
pelvic flexure enterotomy to evacuate colon
close abdominal wall with #2 absorbable (vicryl) methods vary; suture / staple skin; belly bandage
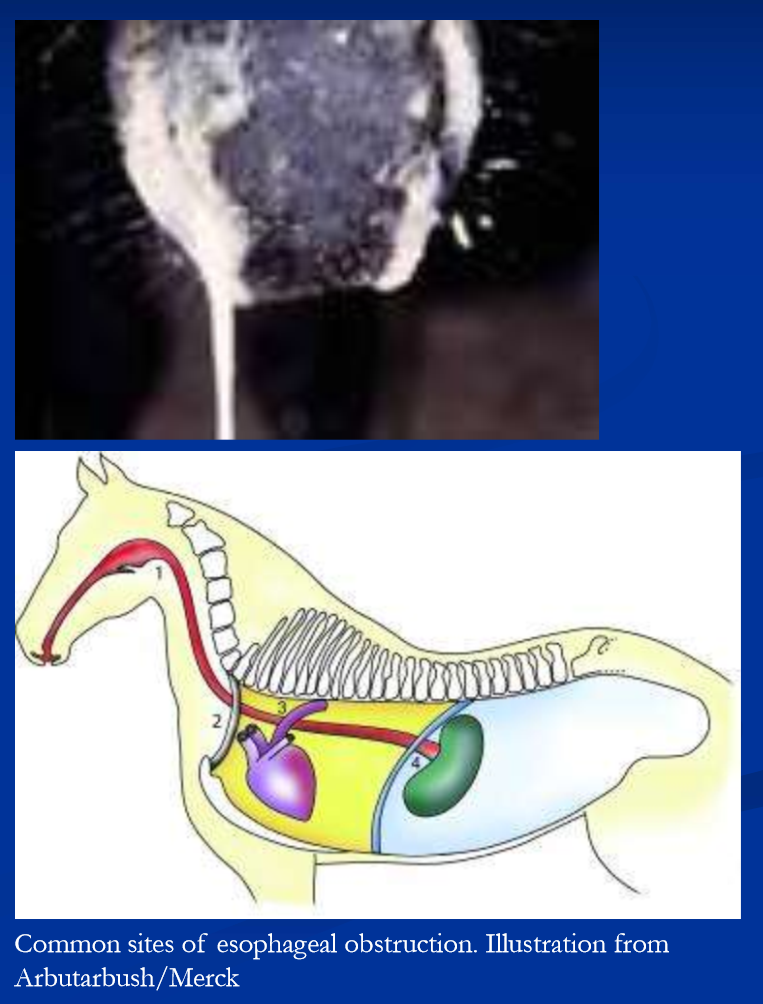
esophageal obstruction
primary obstruction = intraluminal obstruction with feed or foreign body
feed obstruction is the common form, referred to as “choke” or “simple choke”
causes / associations/ predispositions for simple choke are
dental problems
course hay
grain, pellets or beet pulp eaten greedily
physical exhaustion (feeding immediately after a workout)
any cause of generalized weakness (example botulism)
pharyngeal dysfunction
previous choke
additional causes of esophageal obstruction include
stricture
diverticulum
intramural masses example tumor (SCC), abscess/granuloma
extramural mass; cervical and mediastinal abscess, granuloma, or tumor
peri-esophageal scar tissue
functional obstruction: motility disorder and or mega-esophagus
primary obstruction with feed (simple choke)
signs: are saliva and or feed from nose after being fed, anxious expression, extended neck, gagging, retching, coughing
high cervical, thoracic inlet, heart base, cardia are common sites
site of obstruction identified by passing NG tube or endoscope
also can palpate cervical obstruction
endoscopy*, ultrasound, radiology to visualize
management of simple choke
goals are to resolve the obstruction, manage complications, determine and eliminate the cause
remove feed and water to avoid aspiration
mild choke may resolve spontaneously
sedation can relieve anxiety and promote relaxation to encourage spontaneous resolutions; ex xylazine / acepromazine
however, prolonged obstruction (>4-6 hrs) increases the risk of esophageal damage, perforation and aspiration
manual reduction via esophageal lavage is generally indicated (dont let the sun set on a choke)
lavage via stomach tube and warm water
requires a-traumatic approach and patience
sedate to relax horse and drop head to avoid aspiration*
with tube placed proximal to obstruction repeatedly administer and drain small volumes of water to break up feed
can massage bolus if in cervical esophagus
special double lumen tubes are available
can place cuffed naso-trahceal tube to avoid aspiration
*do not forcibly push the obstruction aborad
refractory / more severe impactions may require
irrigation under general anesthesia or
esophagostomy
after relieving obstruction endoscopic exam to evaluate the degree of mucosal/esophageal injury is ideal
for uncomplicated choke (minimal mucosal injury)
complete feed restriction for 24-48hours* (provide water
*esophageal motility is temporarily compromised subsequent to choke, predisposing to re-obstruction
re-feed with slurry initially for up to 7 days gradually return to normal diet depending on initial damage/progress
complications of simple choke
acute complications include
mucosal injury / ulceration (esophagitis)
perforation (these dont do well depending on location)
aspiration pneumonia
dehydration and electrolyte depletion with prolonged chocke
manage with fluids, antibiotics, anti-inflammatory drugs, surgery as needed
chronic complications are stricture, diverticulum, megaesophagus, recurrent obstruction
prevention
proper dental care; alternative diets for aged / poor dentition
dont feed horses immediately after workout
avoid competition for feed
Esophagostomy
employed rarely for cervical obstructions
refractory esophageal feed obstruction
foreign body retrieval
performed standing or under general anesthesia
place NG tube prior
longitudinal esophagotomy over or below obstruction
primary closure if esophageal tissue is healthy
otherwise, delayed closer / second intention, feed esophagostmy (stomach tube in place
antibiotic treatment indicated / necessary
can be employed for healing of esophageal injury, or perforation from choke or foreign body
also provides a means of enteral feeding in case of oropharyngeal disease that preclude oral intake
esophagostomy placed below damaged site
NG tube placed though esophagotomy site and sutured in place 2nd intention healing upon removal may fail to heal from fistula
esophageal perforation
result of long-standing obstruction with feed, intra-luminal foreign body, NG tube, external penetration
acute cervical perforation is potentially repairable if attended quickly and drainage established
diagnosis aided by endoscopy, US, radiographs, contrast
primary closure if possible
otherwise, must heal by 2nd intention, guarded prognosis; place esophagostomy tube below for feeding
intrathoracic perforation is fatal
severe, acute septic mediastinitis
Esophageal strictures
usually the result of acute obstruction
also external trauma, reflux esophagitis, congenital
signs are recurrent obstruction
diagnosis with endoscopy, contrast radiography
bougienage techniques, endoscopic and other
surgical techniques include
esophagomyotomy, partial or complete resection - anastomosis and patch grafting
prevention is
diligent management of primary obstruction thorough post-obstruction evaluation and prolonged feeding of low-bulk diet when indicated
Esophageal diverticulum
pulsion diverticulum
protrusion of mucosa and submucosa thru defect in the muscular wall, generally result of simple choke; has narrow neck / flask-like shape; fills with feed and leads to obstruction; diverticulectomy for correction
traction diverticulum
consequences of scar tissue from perforation or other cervical injury, or esophagotomy / ostomy
contraction of scar tissue and traction on esophageal wall
leads to localized shallow diverticulum with wide neck
signs are intermittent, usually transient obstruction
generally causes minimal difficulty cna live with it

Esophageal motility disorders
Megaesophagus is usually an acquired condition
prolonged obstruction (choke) may lead to permanent hypomotility and megaesophagus
can be a consequence of stricture or diverticulum
Idiopathic megaesophagus in Freisian horses
maybe as complication of neurological dz, example dysautonomia (grass sickness)
dilated, hypomotile esophagus on endoscopy
treatment options limited; elevate forequarters when feeding identify and treat any primary disease
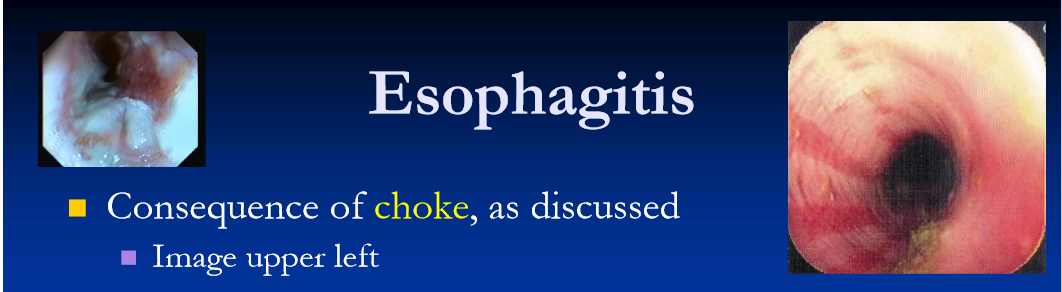
Esophagitis
Consequence of choke,
reflux esophagitis
chemical injury from reflux or gastric acid/bile salts, affecting lower esophagus
complication of gastro-duodenal ulceration in foals (mostly) causing pyloric stenosis and gastric outflow obstruction
other causes of RE are SI obstruction causing entero-gastric reflux, gastritis and or gastric dilatation of any origin esophageal and gastric motility disorders incompetence of lower esophageal sphincter
chemical injury from drugs (ex PBZ), toxicants, toxins (ex cantharidin)
other esophageal conditions
Neoplasia
squamous cell carcinoma (SCC)
occurs in association with stratified squamous epithelium of the esophagus and stomach; esophageal SSC may present as choke
congenital abnormalities
rare
idiopathic megaesophagus in Friesians
persistent right aortic arch vascular ring anomaly (stricture)
4th bronchial arch defect
Disorders of the stomach
gastric ulceration
gastric dilation
grain overload
gastric impaction
gastric rupture
neoplasia
Equine gastric ulcer syndrome
common condition and cause of poor performance and or ill-thrift across domestic equine populations
occurs in all ages, sexes, breeds and classes
performance horses are at highest risk
prevalence varies (11% go 90%)
etiopathogenesis is incompletely understood
multifactorial including confinement, feeding practices, NSAIDs and a variety of physiological and social stressors
clearly intensive management practices associated with training and performance are major contributors
clinical signs in adult horses for gastric ulcers
in adult horses, signs are vague and non-specific, and most cases go unrecognized; common complaints are
reluctance / refusal to work*
anxious demeanor “grouchy”
aversion to cinch, touching flank
diminished appetite
sometimes loss of condition
some (minority) show abdominal pain, typically as recurrent bouts of mild-moderate, intermittent colic
EGUS may be the most common cause of recurrent colic in adult horses
equine gastric ulcers syndrome in foals
very common and believed associated with illness, physiologic and or psychic stress in early life
common in neonates and suckling foals with diarrhea
lack of maternal interaction in neonatal period/ early life due to illness or death of dam, or illness of foal
stress of weaning psychosocial stress and disease
NSAIDs foals appear more sensitive to toxic effects
glandular and pyloric disease may be more common in foals vs adults
as with adults, most cases are subclinical
in clinically evident cases, signs and complications tend to be more pronounced / severe compared to adults
poor appetite / suckling behavior
abdominal pain*
colic after suckling
recumbence rolling up on back
abdominal pain can be marked and or persistent
Bruxism and ptyalism suggest advanced disease and many indicate ulcerative duodenitis
Diagnosis for equine gastric ulcers
clinical diagnosis response to treatment
condition is common, especially in athletes, stressed adn or sick horses, and horses on NSAIDs
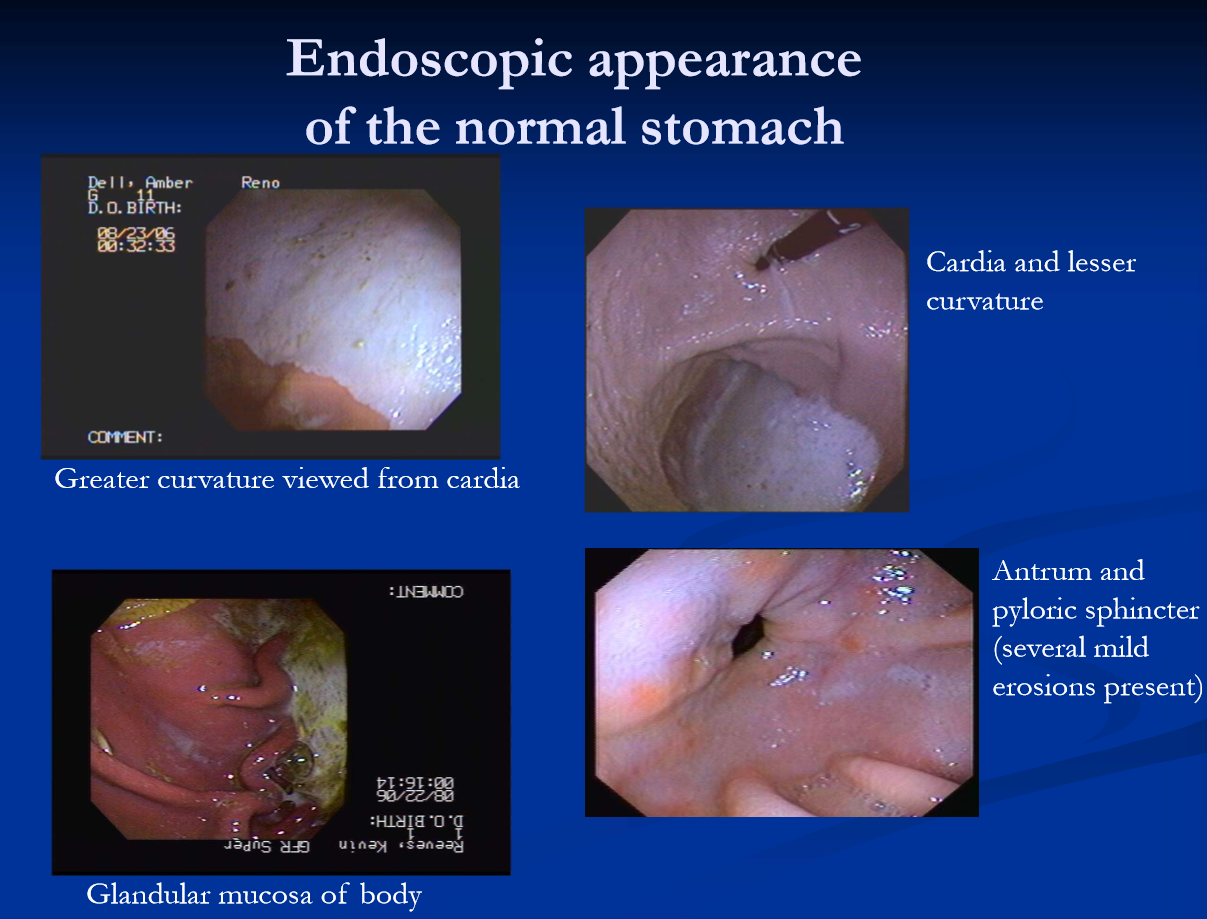
endoscopic examination of the stomach is definitive (and ideal)
requires 2.5-3m scope
graded based on severity
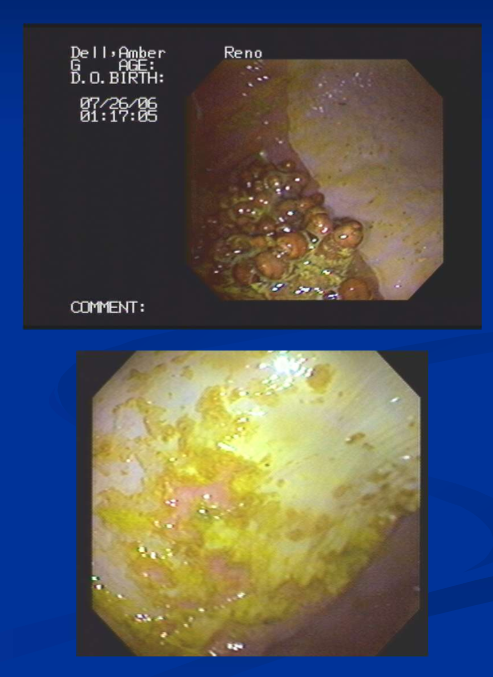
endoscopic appearance of gastric erosion and ulceration
top: mild hyperkeratosis of squamous mucosa adjacent to margo plicatus, indicating mild erosive disease (gastrophilus larvae are observed on the adjacent glandular mucosa)
below: extensive erosion of squamous mucosa with sloughing of epithelium
top: severe diffuse squamous ulceration involving lesser curvature
below: thickened, hyperkeratotic appearance of deep, focal squamous ulcers in the chronic phase

general principles of management of gastric ulcers
management changes****
take athlete out of work when possible
reduce confinement / increase turnout
change diet: free choice hay/pasture, stop grain
for non-athletes ID and eliminate stressors, illness
stop any NSAID use
pharmacologic suppression of gastric acidity
anti-ulcer drugs (acid suppressive therapy)
horses with clinical squamous ulceration uncomplicated by glandular disease
proton pump inhibitor omeprazole (Gastroguard, Boehringer-ingelheium)
4mg/kg q 24hrs for 28 days
recheck gastroscopy at 28 days
H2 receptor antagonists (ranitidine preferred, currently unavailable*)
off label use in US common
oral tablets
recheck gastroscopy at 4-6 weeks
H2 agonists work well and are inexpensive
off label pantoprazole and famotidine protocols also exist
injectable formulations very useful in managing EGUS in foals
horses with glandular disease
Omeprazole (gastroguard)
sucralfate 12mg/kg orally q12h
treat for 4 weeks, recheck gastroscopy
frequently need continued treatment and treatment failures are common after 8 wks consider alterantives
alternatives are injectable omeprazole and misoprostol these are off label usages
in refractory cases, management changes are critical including various means of enrichment to address psychosocial aspects
management of foals with EGUS, gastroduodenitis
foals with clinical signs (colic) often have extensive disease, including glandular ulceration adn or duodenitis; gastroscopy
treat any primary dz, identify adn eliminate physiologic and social stressors, eliminate any NSAID use
treat aggressively with anti-ulcer drugs, including injectable IV pantoprazole and oral sucralfate
with suspected duodenitis / gastric outflow obstruction, motility modifiers ex bethanicol, metaclopramide
some require pyloric bypass surgery to relieve outflow obstruction; gastroenterostomy; guarded prognosis
note: incidence and clincal consequences of ulcerative duodenitis in adults is not well documented
preventive use of ulcer drugs
intermittent use in performance horses
stressful events such as weaning, shipping
sick, hospitalized horses
maybe horses on NSAIDs
Gastric dilatation
primary gastric dilation: risk/ complication of carbohydrate overload “grain overload)
ingestion of excess amounts of highly fermentable feed
grain, extruded feeds, rich alfalfa, lush pasture
results in excessive gas production, gastritis and fluid production
Secondary gastric dilation: result of small intestinal obstruction
leads to enterogastric reflux
likely the most common cause of gastric dilation
in either case the risk is gastric rupture (fatal)
horses have small stomach relative to body size (8-10L) perhaps 20 liters when maximally distended
no mechanism for regurgitation / vomiting (lower esophageal sphincter is normally one way valve)
gastric dilatation clinical signs and diagnosis
signs are abdominal pain, NG reflux, caudally displaced spleen, gastric dilatation, distended SI with secondary
Dx/evaluation: nasogastric intubation, rectal exam, ultrasound
primary gastric dilatation / CHO overload may present with history of exposure, acute and progressive abdominal pain, gastric rupture or enterocolitis
horses with secondary gastric dilatation have distended small intestine and other signs of SI dz depending on cause/type
management of gastric dilation
gastric decompression via nasogastric tube
dilation secondary to SI obstruction recurs until SI problem is resolved
leave tube in place and work up case
grain overload (carbohydrate overload)
horses gains access to the grain bin
corn, barley, oats, sweet feed, commercial pellets
also rich alfalfa and lush pasture
may present as acute gastritis and gastric dilation
characterized by acute progressive abdominal pain and gastric reflux; gastric rupture is a major risk and fatal
severe cases evolve into a syndrome of enterocolitis, often severe with lactic acidosis, endotoxemia and laminitis
management of known or suspected grain overload
assess the situation critically / carefully in order to determine the level of exposure
pass NG tube to assess stomach contents / gastric pressure; attempt gastric lavage
with no clinical signs (colic/GD), treat as follows:
mineral oil under gravity flow
NPO for 24 hours; monitor closely for 72 hrs
if colic, reflux and or toxemia are present, decompress adn plan for intensive care
Gastric impaction
uncommon, poorly defined, fair to poor prognosis
defined as dehydrated mass of ingesta retained beyond 16 hours of abstinence
possible predispositions
poor dentition
course roughage (oat hay, straw), beet pulp, bran
possible sequelae to gastritis / grain overload
persimmon seed phytobezoars are a known specific cause
gastric squamous cell carcinoma (SCC)
Fresians appear predisposed via inherent motility issue
usually vague signs of poor appetite, maybe mild, intermittent colic; rarely acute abdominal crisis
gastric impaction: diagnosis and management
abdominal ultrasound: large radius of stomach curvature and splenic displacement; gastroscopy
medical tx for impacted feed is oral hydration with crystalloid solutions
oral infusion of carbonated beverage for persimmons
may be dx-ed at exploratory laparotomy; transmural hydration and massage of mass followed by medical tx
prognosis for idiopathic impaction with gastric enlargement is guarded risk of recurrence rupture

gastric rupture
terminal event of acute gastric dilation or gastric impaction
other possible causes and predispositions not clearly defined; perhaps mural disease ex stomach worms, gastric SCC
rupture results in acute septic peritonitis, rapid development of endotoxic shock and death
typically presented in severe endotoxic shock with history of abdominal pain or found dead
diagnosis on ultrasound, abdominocentesis, necropsy
euthanasia
Gastric neoplasia
squamous cell carcinoma is the most common form of gastric and esophageal neoplasia in horses
generally teen-aged and older
arises from the squamous epithelium of stomach / esophagus
may become transmural and invade adjacent organs
weight loss and or chronic colic; choke with esophageal
Dx: gastroscopy/biopsy, maybe peritoneal fluid analysis
poor prognosis
small intestinal obstruction
in general SI obstruction causes gas and or fluid distention of the SI, enterogastric reflux, gastric distension, and abdominal pain.
causes: adynamic ileus, intraluminal obstructions, incarcerations, intussusceptions, adhesions, and various strangulation obstructions
strangulating obstruction leads rapidly to bowel compromise, peritonitis, and CV compromise; prompt sx intervention is needed
further most simple SI obstructions eventually lead to bowl injury and usually require surgical intervention
signs of obstruction:
abdominal pain
nasogastric reflux
SI obstruction
adynamic ileus
inhibition of propulsive bowel activity results in functional obstruction
causes are:
post-operative complication of laparotomy, especially for SI dz
enteritis
peritonitis
neonatal weakness / hypoxemia syndromes
managed with treatment of any primary disease, decompression via NG tube, ± motility drugs
*without a specific diagnosis / functional cause, signs of SI obstruction should prompt exploratory laparotomy
simple intraluminal obstructions of the small intestine
ascarid impaction
jejunal obstruction in weanling aged foals
often precipitated by deworming foal with heavy burden
medical tx early is possible; guarded px for surgical dz
ileal impaction
coastal (Bermuda) hay and tapeworms are risk factors
gradual progression (hours) of SI distention and colic
generally a surgical condition, although medical management is possible with early diagnosis/intervention
foreign bodies
baling twine, plastic bags, more; surgical in most cases
SI incarcerations
epiploic foramen entrapment; cribbing is a risk factor
mesenteric rents: SI becomes incarcerated via teras in mesentery or gastrosplenic ligament becomes fluid filled and engorged prone to volvulus
inguinal entrapment in stallions (inguinal hernia): post breeding or heavy exercise; some breed predispositions
umbilical and inguinal hernias in foals, body wall defects, diaphragmatic hernia
these are surgical conditions presenting as gradually progressive (hours) SI distention and abdominal pain
SI intussusceptions and adhesions
Intussusceptions
jejunum, jeunual-ileal, ileo-ileal, ileo-cecal
perhaps more common in young
perhaps associated with hypermotility/enteritis
tapeworms may be associated with ileocecal intussusception
surgical and may require resection-anastomosis
intestinal adhesions
complication of laparotomy, esp SI obstruction / resection
any cause of peritonitis
localized or focal bowel injury ex infarction / parasites
post-surgical adhesions present later with colic / distended SI
surgical intervention; px depends on location and extent
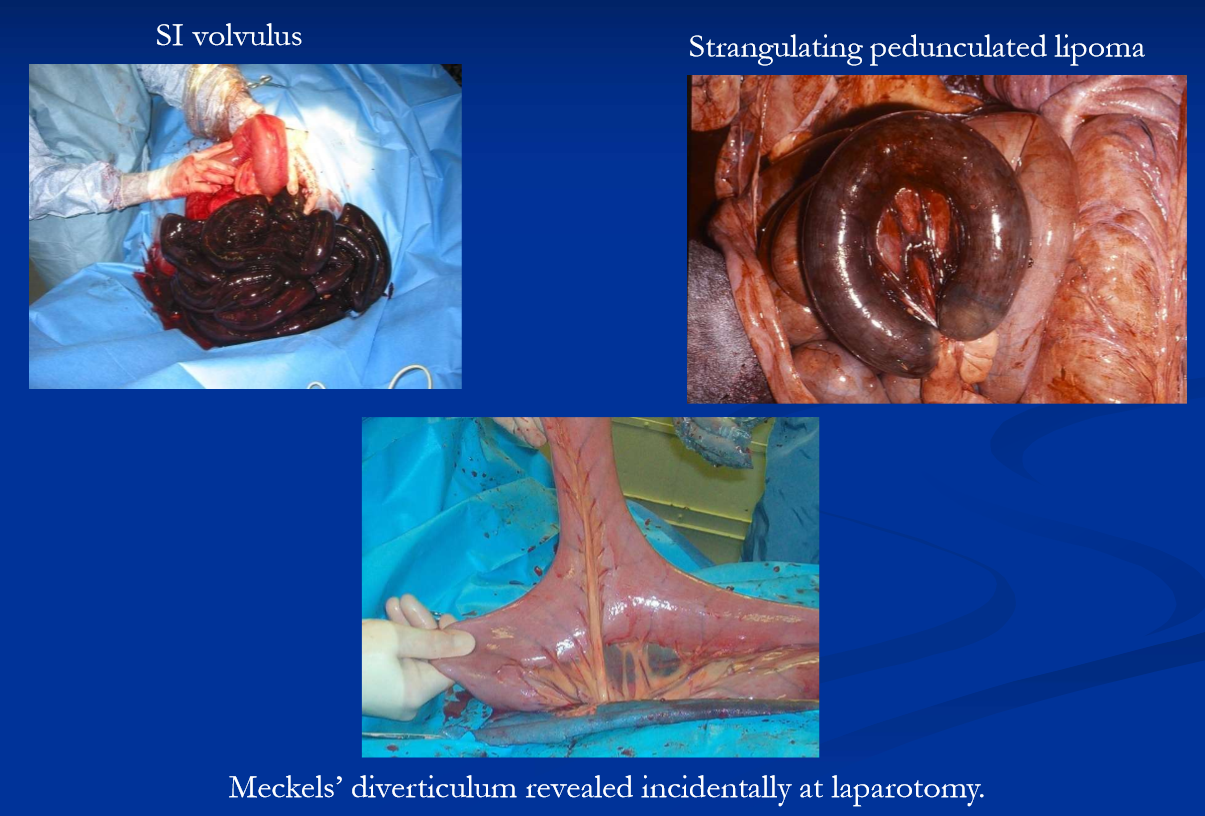
Strangulating small intestinal obstructions
strangulating pedunculated mesenteric lipoma
mature horses, especially older overweight mares
small intestinal volvulus; all ages, unknown etiology
strangulation / torsion / volvulus associated with Meckels diverticulum
these present as acute, persistent and progressive abdominal pain and require prompt surgical intervention
obstructive conditions of the large intestine
large colon and cecal impactions
sand accumulation
ureterolithiasis
LC displacement
large colon volvulus
intussusception
obstructive disease of the large intestine cause abdominal pain and include simple (intraluminal) obstruction, nonstrangulating displacements and strangulating obstructions (torsion, volvulus, intussusception). most intraluminal obstructions with course or dry ingesta (impactions) are treated medically. severe or persistent impactions, large accumulations of sand, enterolithiasis, most non-strangulating displacements and torsion/ volvulus require surgical correction
impactions of the large intestine
accumulation of firm desiccated ingesta in the lumen of the LC or cecum, resulting in physical obstruction
water restriction*, stall confinement, poor dentition, course roughage, sand, NSAIDs, and stress are predispositions
can occur as a complication of any disease that causes reduced fluid intake or fluid loss
LC impactions are most common, and initially arise at sites in where luminal diameter narrows, ie pelvic flexure and or transverse colon
impacted ingesta and gas accumulate orad to these sties, leading to gas distention of large intestine and thus pain
cecal impactions are less common; some may involve motility disorder
Large colon impaction
usually there is intermittent, mild to moderate abdominal pain and abdominal distention
mass of firm ingesta palpable when left colon involved
generally these horses remain physiologically stable and are managed medically
advanced cases may become complicated showing persistent / progressive pain and cardiovascular deterioration and may require surgical intervention
most can be managed medically
restrict feed and provide water
control pain
oral and IV fluids
laxatives and cathartics
mineral oil, DSS, psyllium, MgSO4 / NaSO4
surgery indicated with progressive pain and or failure of medical treatment (not typical)
evacuation of colon through pelvic flexure enterotomy
good prognosis in general; sx cases more complicated
cecal impaction
firm ingesta filling cecum
risk factors / predispositions as with LC impaction but
some are associated with orthopedic sx, prolonged hospitalization and NSAID use and
some may involve a primary motility disorder
diagnosis by abdominal palpation per rectum
medical tx if early; aggressive fluids and laxatives
surgery sooner rather than later; spontaneous perforation with minimal premonitory signs can occur
typhylotomy and evacuation
true motility disorder is considered a progressive condition that will culminate in cecal rupture without surgery; cecal bypass via ileocolostomy

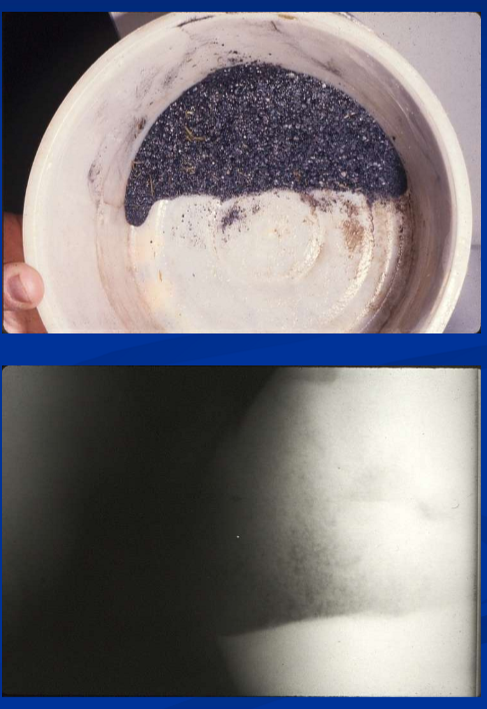
sand accumulation
sandy environments, bare pastures, feeding hay on the ground are predispositions to sand accumulation in LI
sand irritates the colonic mucosa
sometimes resulting in intermittent diarrhea (sand colopathy)
tends to accumulate in the RDC, resulting in
abdominal pain from tension on mesentery, large colon impaction and or obstruction of transverse colon
also predisposes to displacement, torsion / volvulus
diagnosis by
history of exposure, characteristic sounds on auscultation, detection of excessive sand in feces, abdominal ultrasound / radiography, and inadvertent enterocoentesis
medical tx: psyllium (sandrid pellet) hydromucilloid
400g/500kg in feed or via NG
protocol depends on amount of sand, clinical signs (colic or not)
IV fluids and analgesics as necessary
may require celiotomy; large sand accumulations, obstruction at transverse colon, failure of medical management; evacuation of sand via PF enterotomy
prevention: husbandry-avoid feeding on the ground; intermittent feeding of psyllium
Enterolithiasis
Mg-ammonium phosphate stones in large colon
regional; CA, AZ, IN and FL
associated with alfalfa hay, high mineral and pH in colon
can be single or multiple and quite large
chronic colic and or acute abdominal crisis by wedging in transverse colon / small colon
dx with abdominal x-ray, maybe US, or exploratory sx
surgical removal required
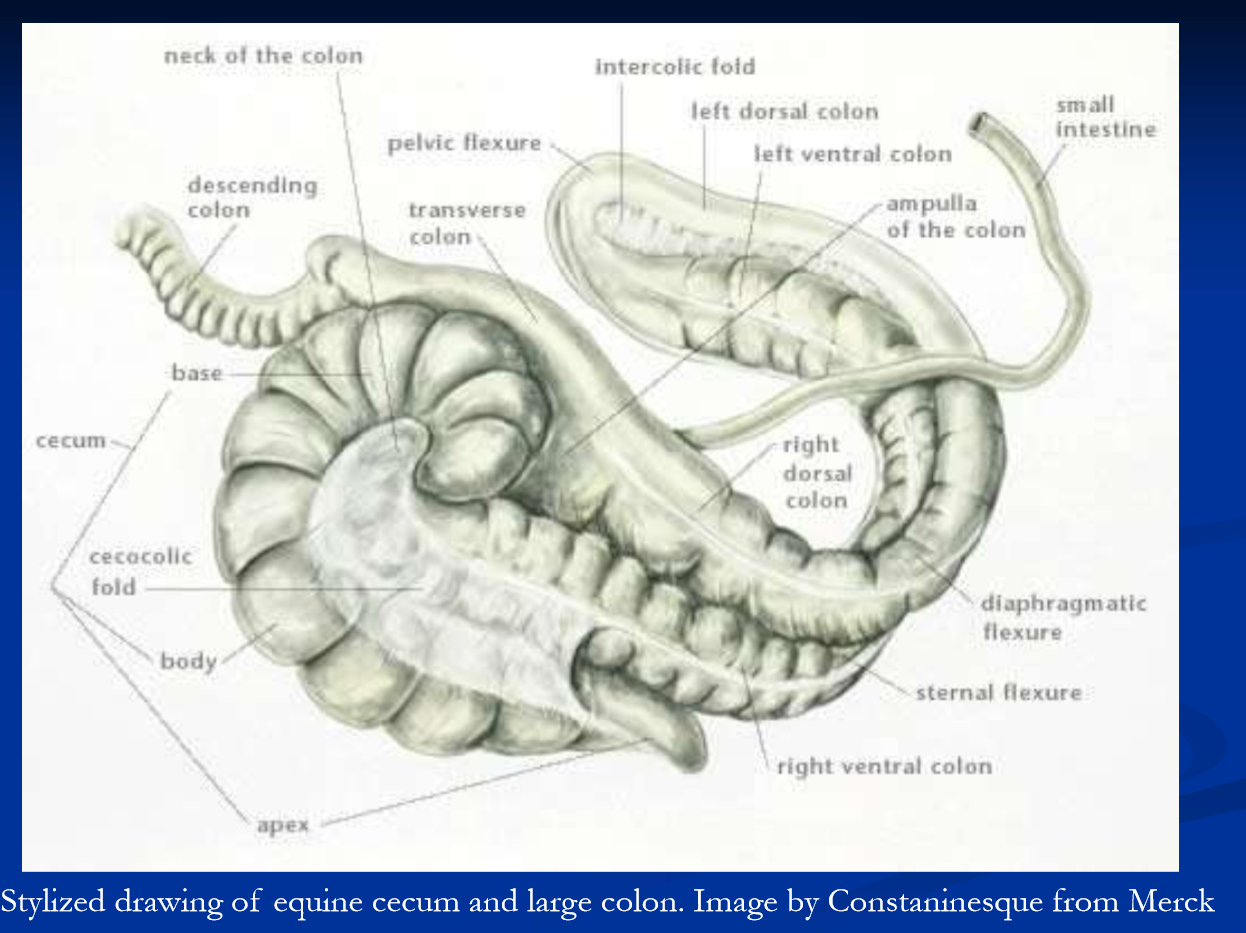
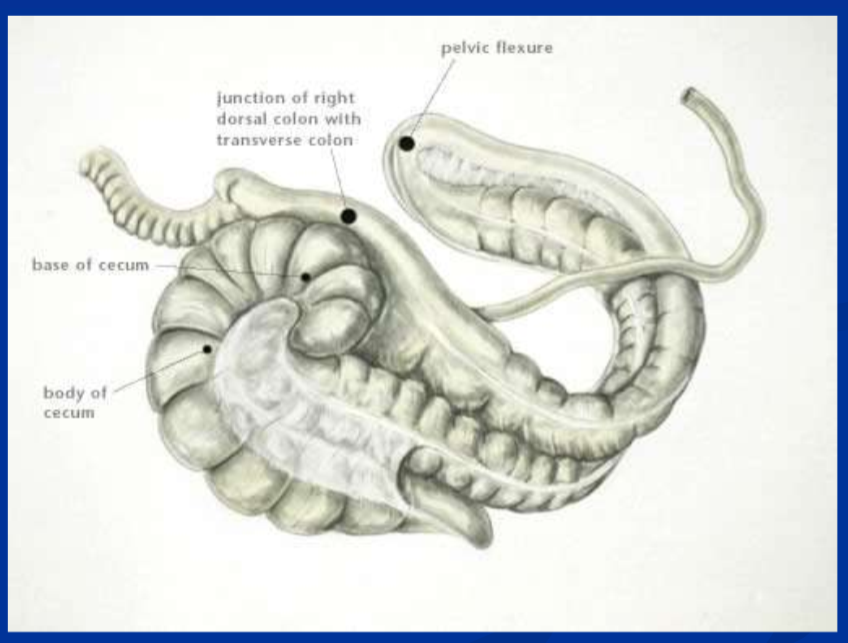
Large colon displacements, torsion, and volvulus
because most of the large colon is not directly attached to the body wall the left colon can move freely within the abdominal cavity (the floating colon)
predisposes the colon to several forms of entrapment, displacement, torsion and volvulus
primary affects adult horses; post-parturient mares particularly prone
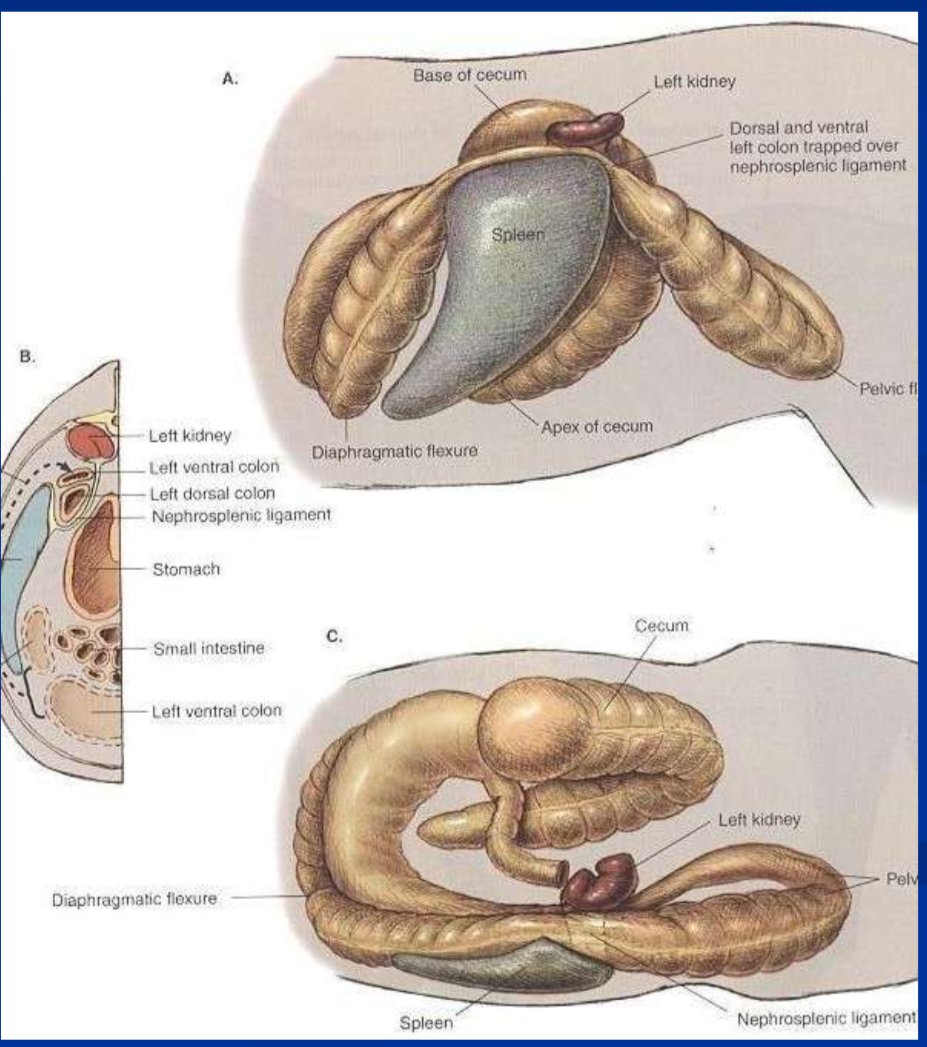
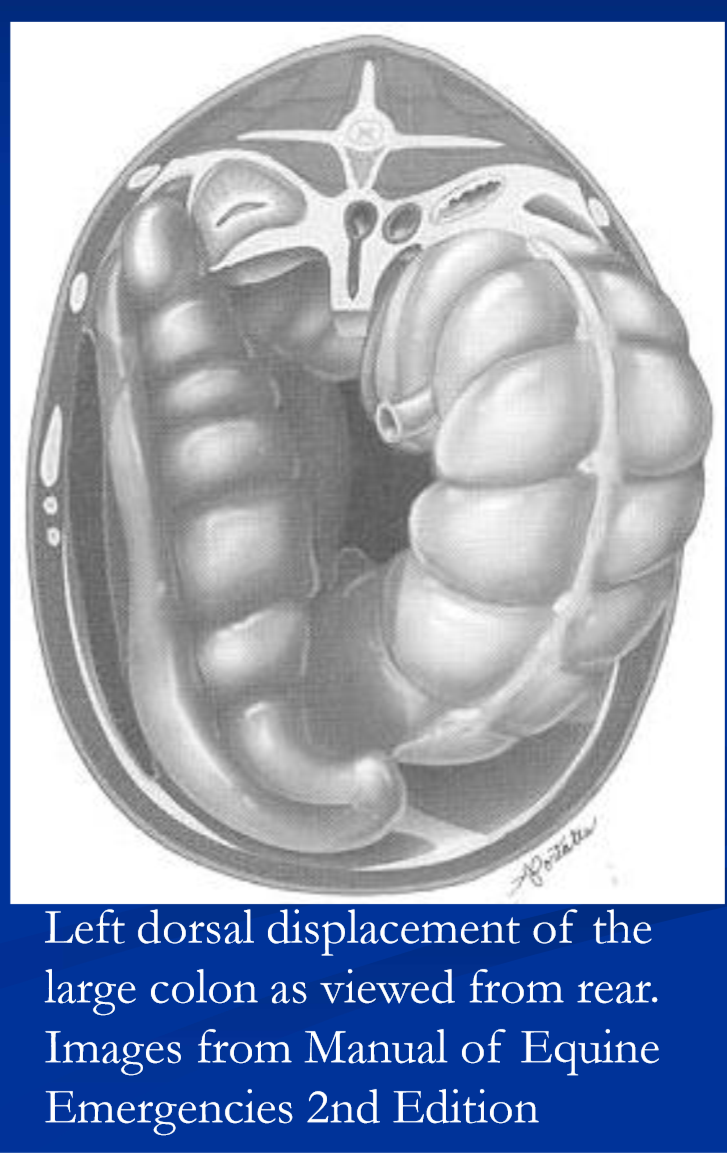
left dorsal displacement of the large colon
“nephrosplenic entrapment
non-strangulating displacement in which the left colon becomes incarcerated within the nephrosplenic space
lodged between the base of the spleen, left kidney, and neophrosplenic ligament
intermittent mild-moderate pain, depending on stage
dx by rectal exam, US
some resolve spontaneously
med txs: 1) controlled vigorous exercise 2) IV phenylpehirne or 3) anesthetize and roll
surgical correction via laparotomy often best option
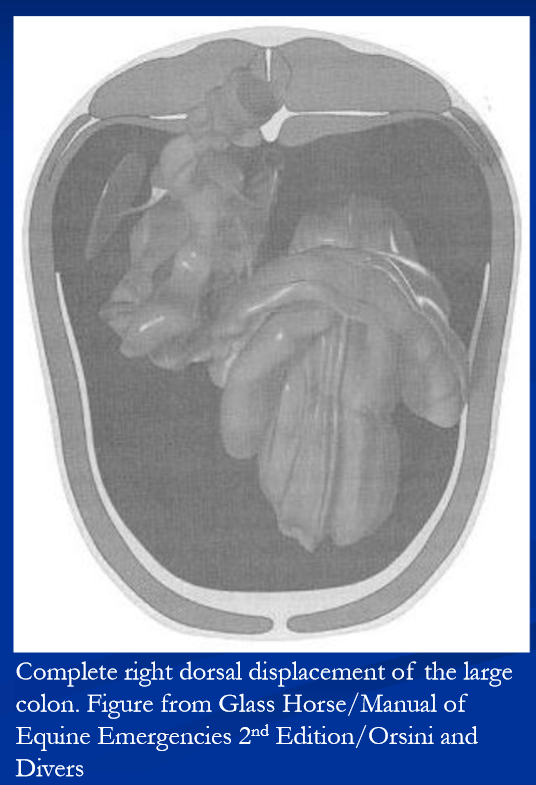
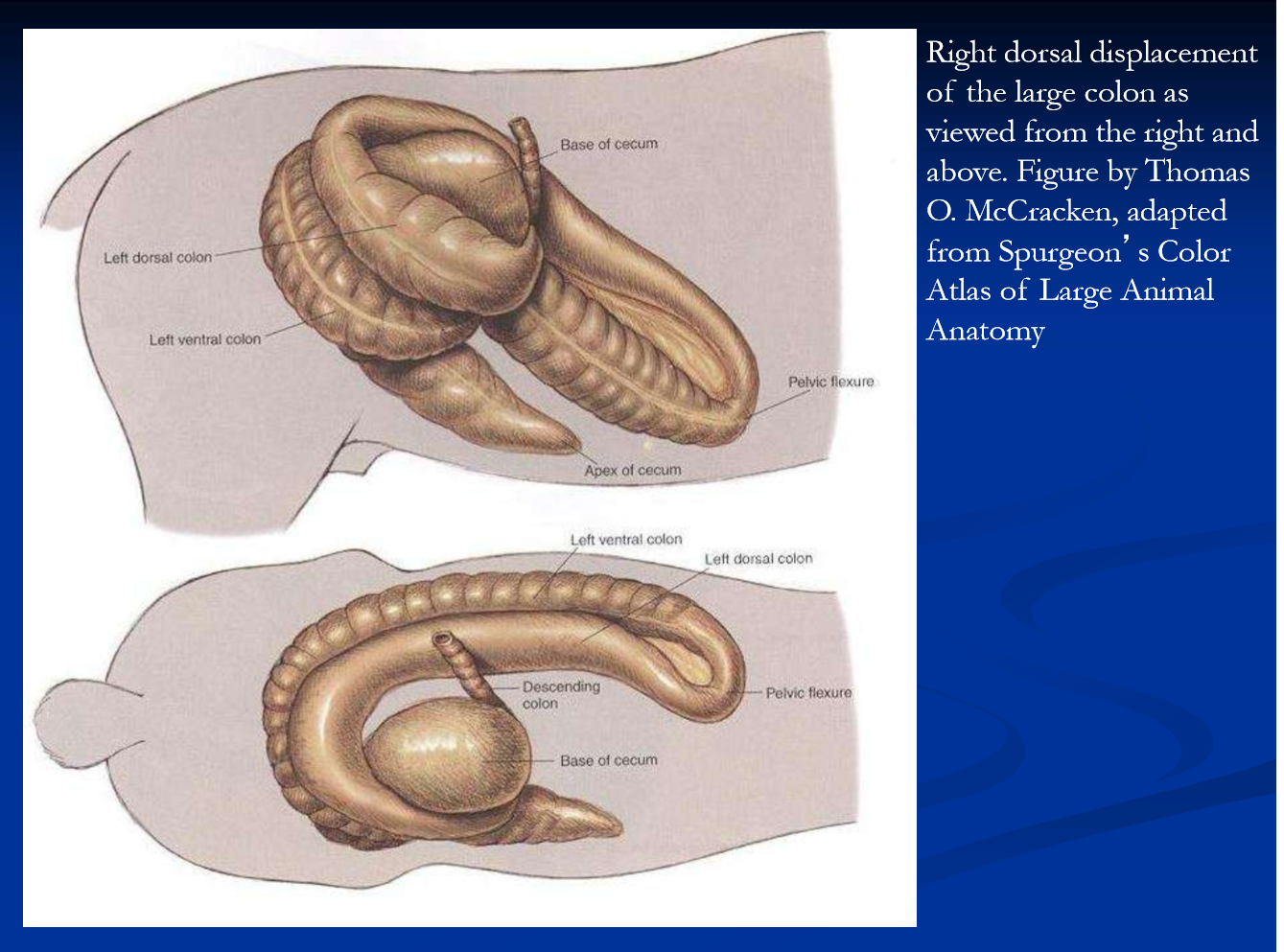
Right dorsal displacement of the large colon
the figure shows a complete right dorsal displacement of the LC
the large colon is displaced between the cecum and right body wall and wrapped around the back of the cecum, running transversally across the caudal aspect from right to left with the pelvic flexure directed forward
partial or incomplete displacements are often found at laparotomy
may possibly progress to torsion and or volvulus
a non-strangulating displacement resulting in progressive signs of pain and abdominal distention
pain varies depending on the position of the colon and degree of gas distention
over time, distention progresses, the levels of pain and cardiovascular compromise increase, and the colon is vulnerable to volvulus
dx: pain, distention, lack of fecal production, abnormal rectal exam; often the colon can be clearly felt passing across the caudal-dorsal aspect of cecum; ultrasound
surgical correction is required; generally good prognosis