Kidneys Review
1/21
Earn XP
Description and Tags
BILD 2
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
22 Terms
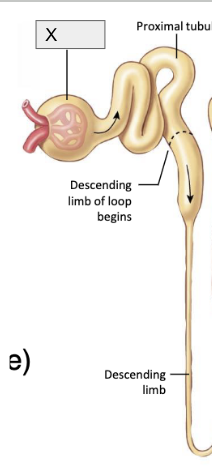
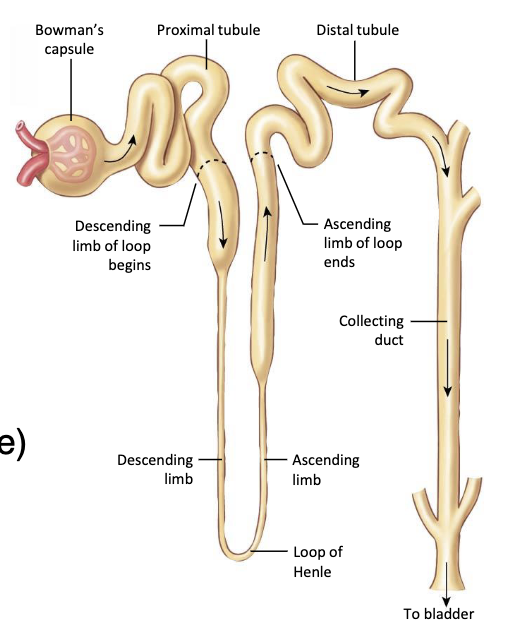
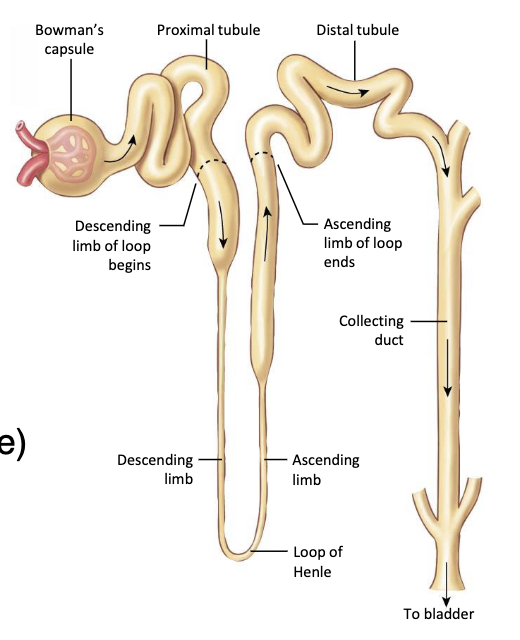
Label parts of the nephron and their function in absorption in filtration
RENAL CORPUSCLE- ONLY PLACE where filtration happens, dependent on blood pressure and PRESSURE GRADIENT
glomerulus - Filters blood b/c H2O follows Na+ through capillary wall = filtrate
Bowman’s capsule - where filtrate is taken from glomerulus
ISOSMOTIC (same osmolarity) to plasma which is 93% water
fluid and solutes move from blood in afferent arteriole → glomerulus → Bowman’s capsule
afferent arteriole has Juxtoglomerular cells → produces renin
Blood that DID NOT get filtered leaves through EFFERENT arterioles → renal veins
What’s the GFR?
Glomerular filtration rate = volume of filtrate made per unit of time by both kidneys
regulated by BP
HIGH BP → HIGH capillary pressure → more blood coming in to glomerulus through afferent arteriole →HIGH BV in glomerulus → INCREASED leaking in glomerulus → INCREASED filtration rate
REGULATED by RADIUS of afferent (the ones that bring blood) and efferent arterioles (the ones that take blood out)
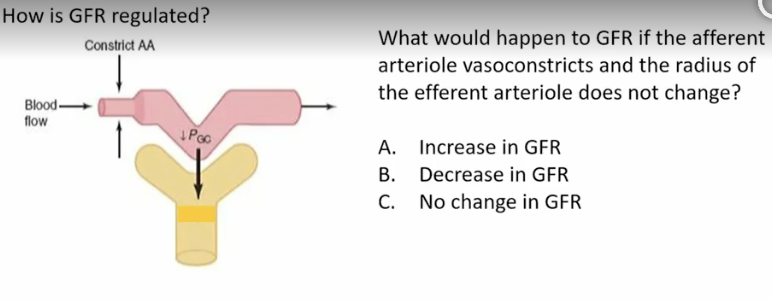
GFR would DECREASE because less blood would be coming IN, since the afferent arteriole’s lumen radius is decreasing →INCREASING resistance → reducing blood flow → reducing blood volume → decreasing capillary pressure
regulated by contracting or relaxing smooth muscle of efferent and afferent arterioles and blood pressure
How is GFR regulated by arteriole vasoconstriction and vasodilation?
regulated by CHANGING the size of AFFERENT and EFFERENT arterioles
HIGHER cap pressure → INCREASED radius → DECREASED resistance → INCREASED blood flow → INCREASED GFR
positively correlated, as capilalry pressure icnreases, so does glomerular filtration rate
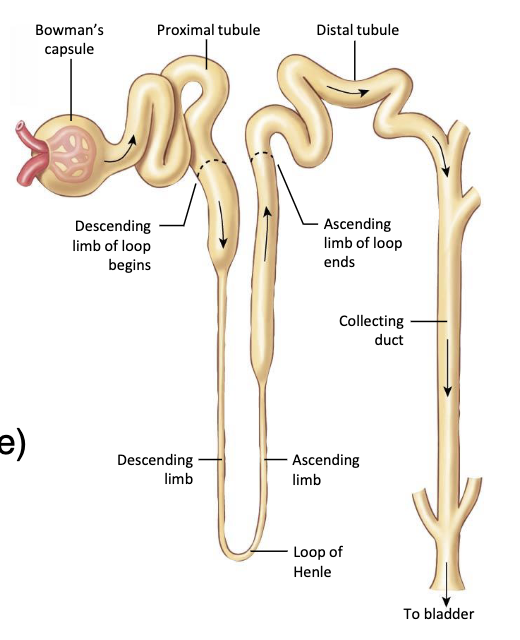
What’s the function of the proximal tubule? remember that the proximal tubule and the rest of the nephron are in the MEDULLA
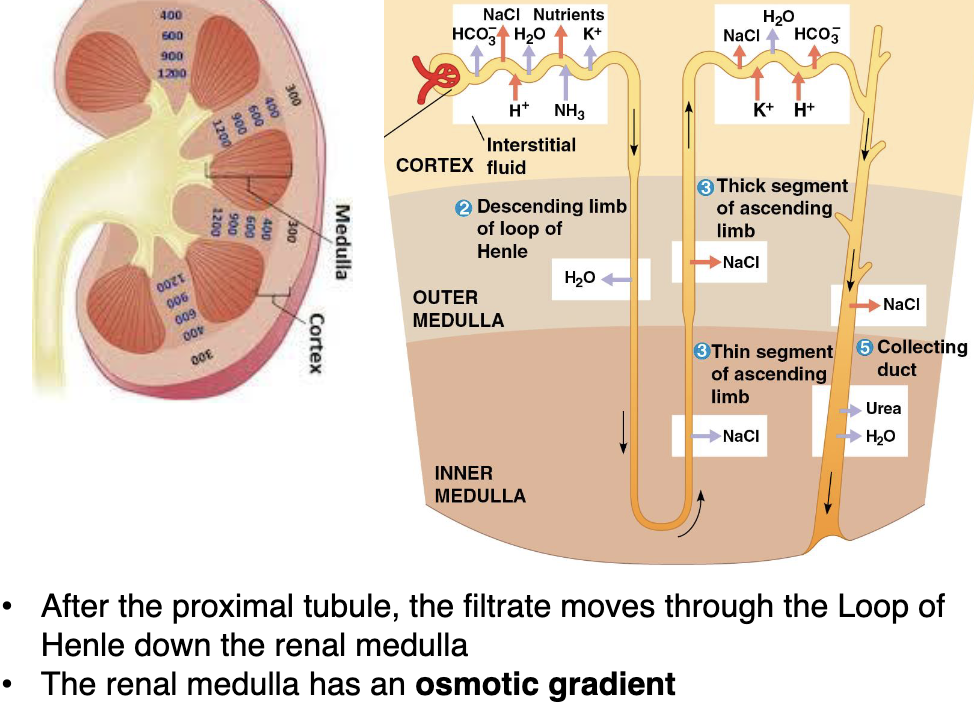
Medulla has an OSMOTIC GRADIENT where the outer medulla has an osmolarity (# of particles per solute) of 300 mOsm and inner medulla has an osmolarity of 1200 mOsm
Proximal Tubule: where REABSORPTION happens
b/c Na+’s driving force created by the Na/K pump OUT of lumen → capillaries = free ride for other molecules to be REABSORBED into blood through capillaries
water has fomo, wants to be where all nutrients and solutes are
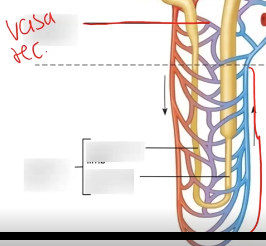
What’s this?
VASA RECTA; the network of peritubular capillaries around loop of hnle
What parts of the nephron are in the renal medulla, which haev an osmotic gradient?
Loop of henle and collecting duct
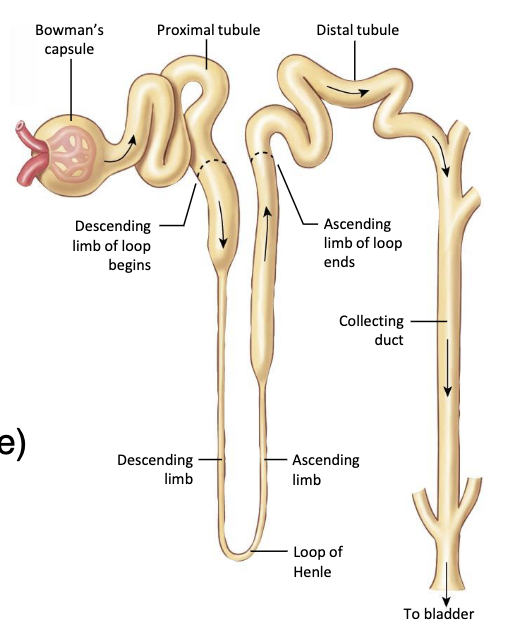
What’s the function of the descending loop of Henle? remember that it’s still in the medulla
Descending Limb to loop of Henle: only permeable to H2O
AQ 1 = pathway
Osmotic gradient b/c its in the medulla = driving force
H2O is going to move from LOW osmolarity to HIGH osmolarity in order to reduce the concentration of particles per volume (osmolarity) OUTSIDE
bottom of loop of Henle is VERY concentrated b/c water left but solutes particles did not since the loop is only permeable to h20
At the bottom of the loop of henle, Filtrate is ______ to plasma
HYPEROSMOTIC (has a higher osmolarity)
What’s the function of the ascending loop of Henle? remember that it’s still in the medulla
ASCENDING Limb of loop of Henle: NOT permeable to H2O
NO pathway b/c there are NO AQ1 = non-permeable to H20
REABSORBS Na+ Cl- and urea
At the top of the loop of henle, Filtrate is ______ to plasma
HYPOSMOTIC (lower osmolarity relative to plasma)
What are the functions of the loop of Henle?
PRODUCE HYPOSMOTIC filtrate (100 msm) at end of loop of henle (main funttion)
maintain isosmotic gradient in renal medulla
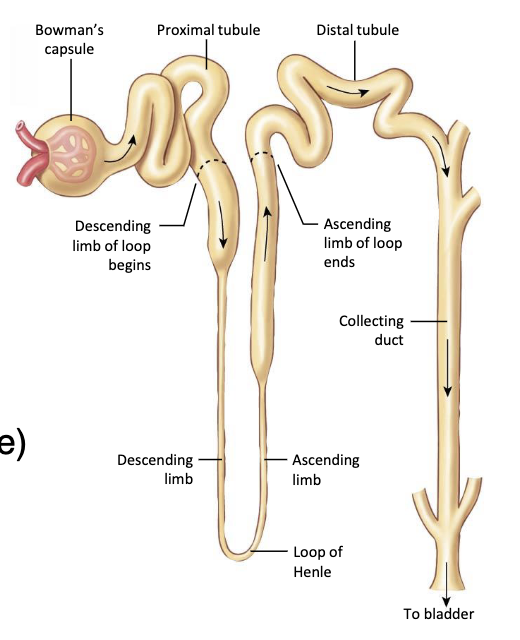
What’s the function of the Distal tubule and collecting duct?
dilute filtrate from ascending limb → distal tubule and collecting duct, reabsorption of H2O and solutes depend on HORMONE REGULATION, permeability is affected by insertions of channels (ADH → AQ2 channels to move out
Distal tubule:regulates sodium, chloride, and potassium reabsorption, as well as calcium handling and pH balance DEPENDING ON PRESENCE OF ADH
Whats the function for the collecting duct?
collecting duct: collects filtrate, reabsorbs water → CONCENTRATES filtrate and regulates fluid and electrolyte balance= FORMATION OF URINE
influenced by ALDOSTERONE, which affects sodium and water reabsorption, and potassium EXCRETION
collecting duct connects nephrons to renal pelvis → secretion
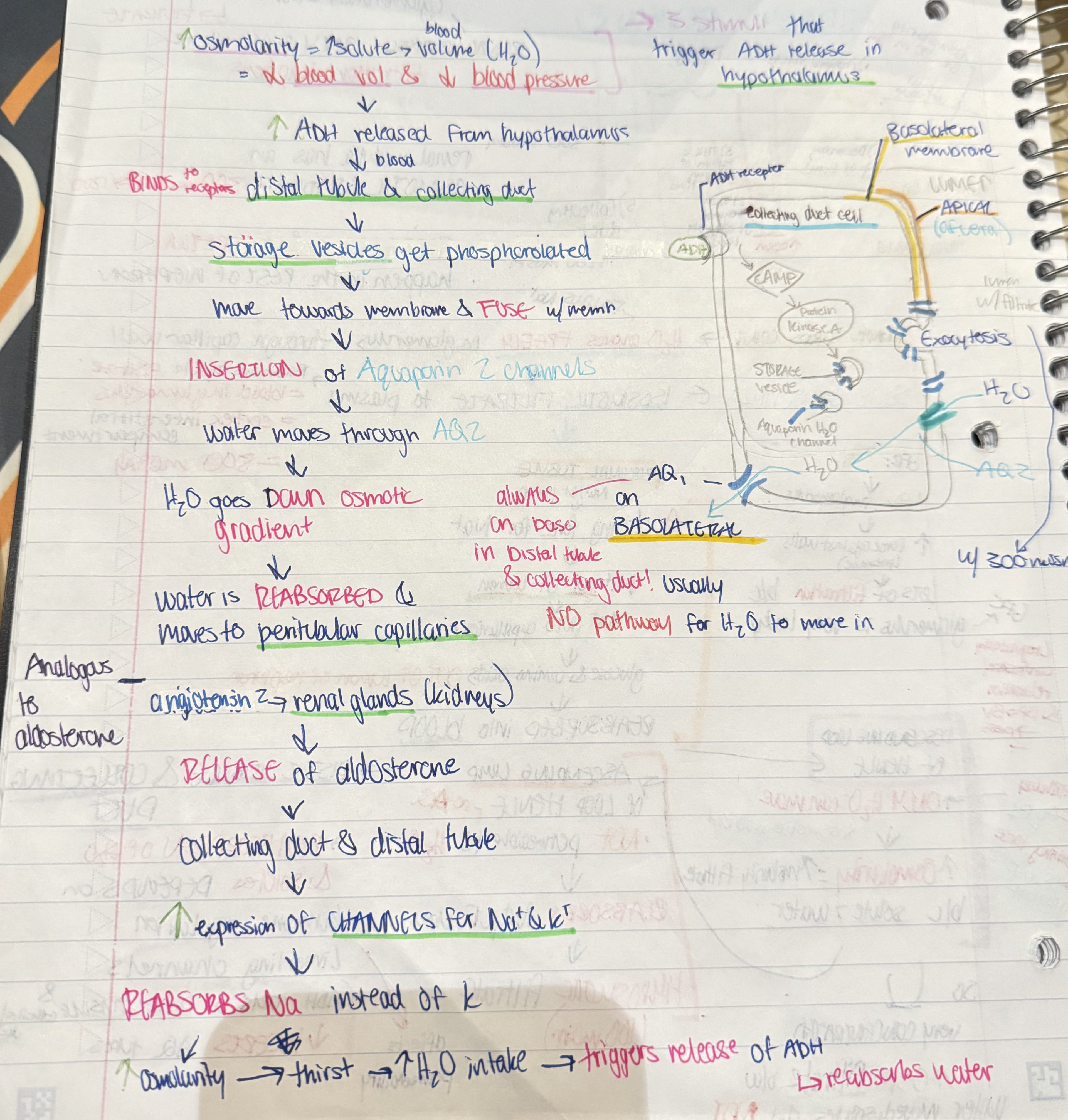
What’s the cascade for ADH release in the hypothalamus that eventually results in REABSORPTION
HIGH osmolarity → LOW blood volume and blood pressure → ADH RELEASED from hypothalamus → ADH BINDS to receptors in distal tubule and collecting duct → AQ2 channels INSERTED on APICAL membrane → water moves, it has a pathway now → water is REABSORBED and moves to peritubular capillaries
role of ADH: insert AQ2 channels on apical membrane to allow water to move and be reabsorbed in order to release urine
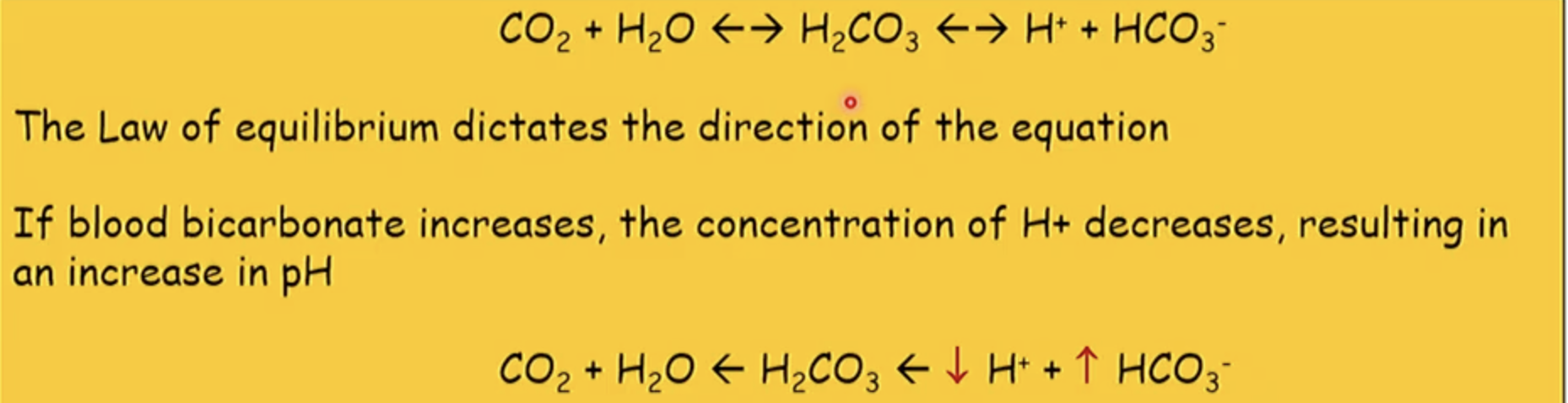
What parts of the kidney are responsible for maintaining pH within the homeostatic range? What ions are absorbed or secreted?
proximal tubule and collecting duct by either REABSORBING OR SECRETING HCO3- OR H+ ions
slower effect on pH b/c processes must be done
If HCO3- is reabsorbs into peritubular capillaries, how will blood pH be affected?
*keep this equation in mind!!
more HCO3- ions → less H+ ions → less acidic , more basic→ pH will INCREASE → alkalosis
How does the Na+/K+ pump relate to solute/water reabsorption at different parts of the nephron?
CREATES a concentration gradient for sodium to facilitate diffusion for other particles, including water to be absorbed
When Na is permeable and crosses the membrane, it allows for water to follow it into the glomerulus
allows for other materials to be reabsorbed in proximal tubule etc.
What’s reabsorptiona nd where does it happen?
molecules are moved from filtrate → blood of peritubular capillaries
**. happens in renal tubule: everything after renal corpuscle:
proximal tubule
loop of henle
distal tubule
Where is the filtrate ISOSMOTIC to plasma?
the proximal tubule b/c water wants to go to higher osmolarity
What causes the release of renin?
DECREASE in blood pressure
LESS blood → afferent arteriole
lower capillary pressure → lower GFR → decreased flow of filtrate through nephron
SYMPATHETIC output
baroreceptors if BP is high or low, depends on stretch and action potentials fired
MACULA DENSA CELLS
on DISTAL tubule, stimulated to release paracrine signal to neighboring cells (JGA)
antisinogen → angiotensin 1 → angiotensin 2 →increase sympathetic - > INCREASED ADH → insertion of AQ2 on apical membrane → water reabsorption because
ADH ALSO causes aldosterone to be released → sodium reabsorption → triggers thirst → increases blood volume and blood pressure