FINAL EXAM: Assessment and Health Promotion
1/120
Earn XP
Description and Tags
4/29 @0800
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
121 Terms
Steps of the nursing process (review)
Assessment
Analysis (Nursing dx)
Planning
Implementation
Evaluation
Nonmaleficence (review)
Do no harm
Beneficence (review)
Promoting good for patients
Justice (review)
Be fair when providing care
4 types of assessment
inspection- looking carefully at pt
Auscultation
Palpation
Percussion
Tools needed for inspection
Penlight
Tape measure
Pulse ox
Items for height and wt measurement
Types of Involuntary movements
• Fasciculation-twitch/quivering
• Myoclonus- muscle jerks/spasms
• Tic
• Tremors
BMI classifications
Underweight less than 18.5 kg/m
Healthy weight 18.5 to 24.9 kg/m
Overweight 25 to 29.9 kg/m
Obesity 30 and above
Calculation for BMI
BMI = weight (kg) / height (m)²
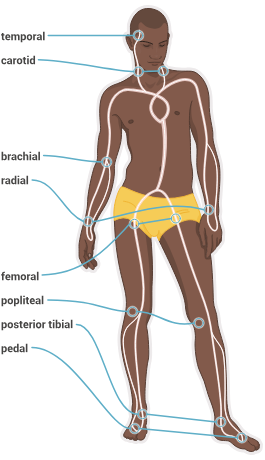
Pulse locations
Pulse strength scale
0 = an absent, impalpable pulse
+1 = a weak, thready, diminished pulse
+2 = a normal, brisk pulse (expected finding)
+3 = an increased, strong pulse
+4 = a bounding, full volume pulse
Visceral pain
in organs, deep cramping, squeezing (appendicitis) (colitis)
Somatic pain
MS system, muscles, bones, tendons
throbbing/aching
broken bones
trauma
Acute pain
Less than 6mo
AKA transient pain
PQRST for pain assessment
Provocation/Palliation. What were you doing when the pain started? What makes it better? What makes it worse? What triggers the pain? What relieves it?
Quality. Describe the pain. Is it dull or sharp? Is it stabbing, throbbing, or cramping?
Region. Where is the pain? Does it radiate? Is it localized?
Severity. How severe is it? Does it interfere with activities? How long does it last?
Timing. What time did it start? How long does an episode last? Is it sudden or gradual onset? Occur during day? Night?
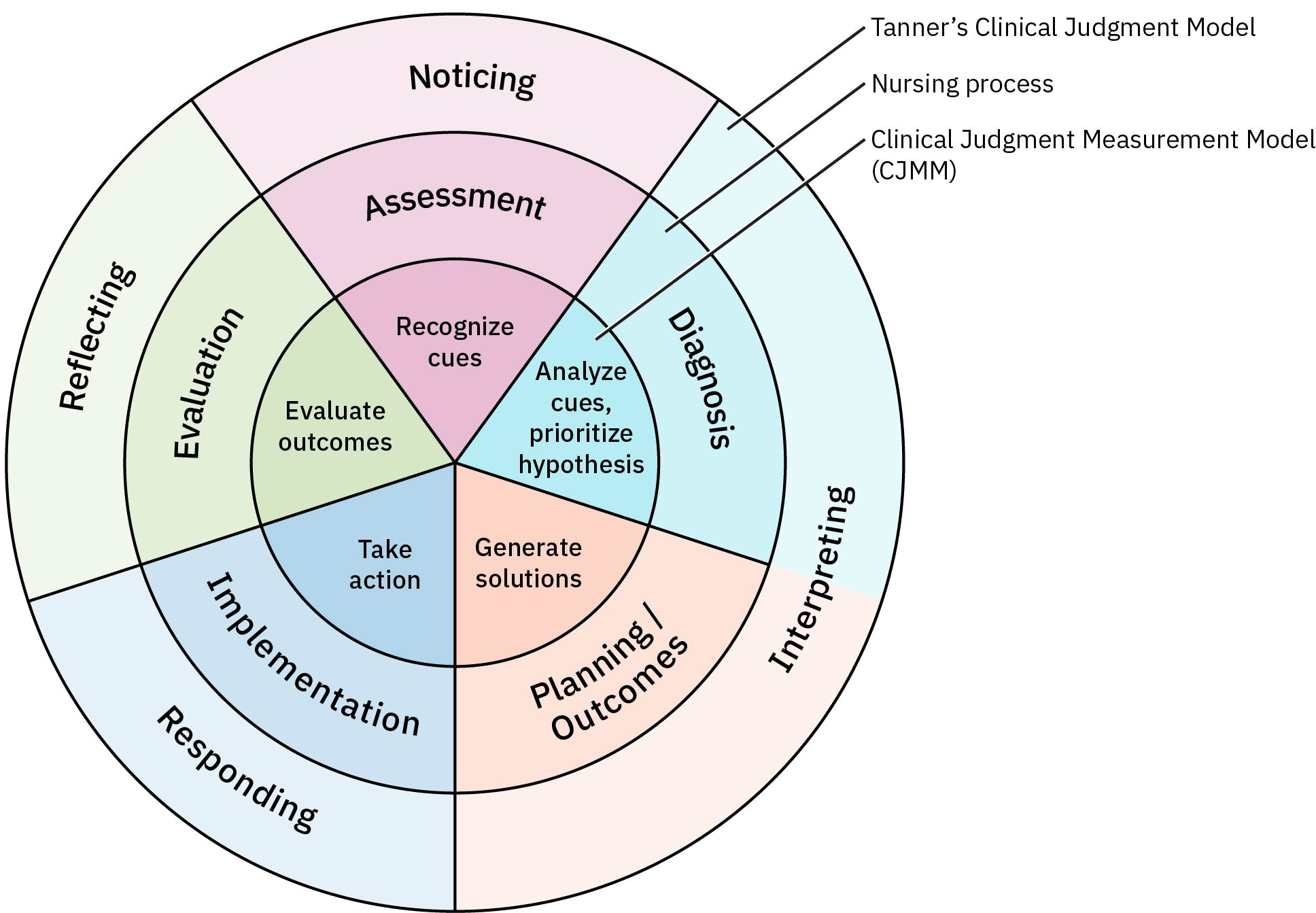
Tanner’s Clinical Judgment Model
Background - on the situation
Noticing - what was initially noticed about the situation/as time went on (assessment of skin, ect)
Interpreting - what do you think about the situation? Have you ever been in a similar one? What other data do you need (Ex. pt has RLQ pain, you think it is appendicitis)
) Responding: What is your goal for the patient/family/staff? Interventions and nursing response (ex. Applying O2 to a pt with low sat)
Reflection in action: What happened? What was the response? (Ex. Pt oxygen improved)
Reflection on action: What did you learn from the experience that could improve future practice?
Functional assessement
Determined patients ability to care for self when not experiencing an acute illness
lifestyle
living environment
ADL ability
Internal factors (stress, activity, sleep, ADLs, spirituality, substance abuse)
External factors (occupational health, living environment, relationships, maltreatment)
Where to assess for cyanosis on darker skin
Oral mucosa and nail beds, palms and soles
Ecchymosis
A discoloration of the skin resulting from bleeding underneath, commonly known as a bruise.
Expected variations of skin assessment
acne
wrinkles
scars
What might velvety skin be indicative of?
Thyroid disease
Purpura
petechiae and ecchymosis covering an area
bleeding disorder
ABCDs of skin lesion assessment
Asymmetry: Compare one side of the lesion with the other side. The two halves of the lesion do not look the same. They are not a simple round circle or an oval shape. They look radically different from each other.
Border: The Lesion has an irregular outline
Color: Color variation within the lesion (areas of brown, tan, black, blue, red, white, or a combination of those colors.
Diameter: Diameter of the lesion greater than 6 mm (the size of a pencil eraser) at its largest dimension.
Evolving: Lesions change rapidly in size
Stage 1 pressure ulcer
Non-blanchable reddened area of epidermis
do NOT rub
Stage 2 pressure ulcer
Partial loss of dermis
pink wound bed
Stage 3 pressure ulcer
Full thickness tissue loss involving subcutaneous tissue, may expose fat.
Stage 4 pressure ulcer
Full thickness tissue loss with exposed bone, tendon, or muscle.
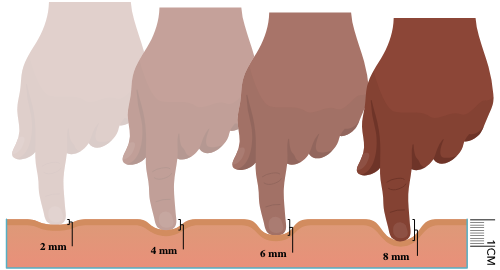
Assessment of edema
To palpate for pitting, use your thumb or index finger to apply pressure for 3 to 4 seconds
1+ denoting a barely detectable indentation
4+ denoting a depression of 8 mm or more that persists for a long time.
Primary prevention
An intervention completed before there is evidence of injury or disease, reduce risk factors
Ex: encouraging exercise and healthy eating to prevent obesity
Ex vaccine clinics
Secondary prevention
During disease process, early screenings
Ex. check BMI during well checks to determine weight status
Tertiary prevention
After the injury or disease is established. Stop bad from getting worse (sick care, hospitals)
Ex. help individuals lose weight to prevent long term effects of obesity
Beck-depression inventory
Self screens for depression (17-20=borderline clinical depression and higher is worse)
AUDIT form
Alcohol screening form
15-20=moderate to severe use
DAST
Drug abuse screening - no alcohol or tobacco use
3-5=moderate… higher is worse
Edinburg scale
For postpartum depression
10 or higher=pp depression
Normal resting pupil size
3-5mm
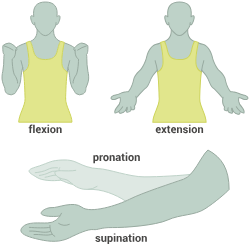
Define flexion, extension, hyperextension, adduction and abduction of the upper extremities
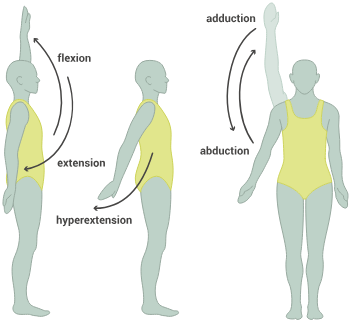
Define flexion, extension and pronation/supination of arms/elbows
Define flexion, extension, hyperextension and lateral flexion of the torso

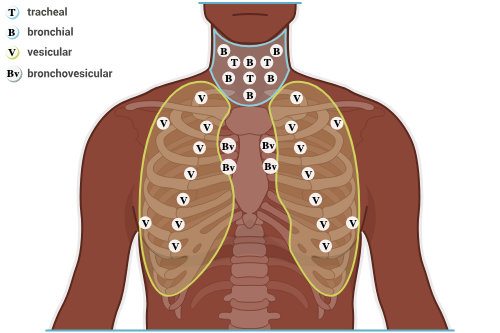
Describe dorsiflexion, plantar flexion, inversion, eversion, flexion and hyperextension of the feet
How much calcium should one intake per day
1000-1200 mg daily
How much vitamin D should one intake per day
600-800 IU
GCS scale
Eyes: 4
Verbal: 5
Motor: 6
Total: 15
Steps of abdominal assessment
Inspection, auscultation, palpation.
listen to right lower quadrant first
How many BS per min
5-34
Is voluntary guarding an expected variation
Yes typically caused by lack of relaxation, involuntary guarding is when there is rigidity even with relaxing (for abd assessment)
have pt exhale
Male v Female urethra lengths
Male: 20 cm (8 inches)
Female: 3-4cm (1-1.5 inches)
Types of feeding tubes
Nasogastric - goes into stomach
Nasojejunal - goes past stomach into jejunum
Nasointestinal - for high aspiration risk pts- short term, usually less than 4 weeks
For duodenal and jejunal feeding tubes, how much extra tubing would you add?
20-30cm (8-12 inches)
How often should the nurse check residual volumes on a feeding tube?
q4-6 hours
If using bag for formula administration through feeding tube, how much formula should you add at one time?
Enough to last about 4 hours
change the bag every 24 hours
How often should the nurse flush the feeding tube?
Before and after each feeding, after med admin/residual checks and every 4 hours to maintain patency
30-50 mL of water
Thoracic vs diaphragmatic breathing
Thoracic breathing involves using the upper chest and is more common in women
diaphragmatic breathing engages the diaphragm for deeper, more efficient breaths and is more common in males
orthopnea
Difficulty breathing while laying supine
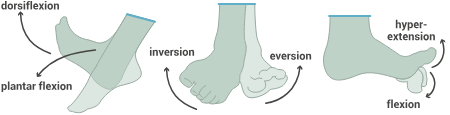
Barrel chest occurs with what dx
COPD
Cheyene-stokes breathing
“ Start stop” breathing
The pt will have deeper breathing that may quicken, followed by hypoventilation and progress to apnea, a lack of respirations.
Ataxic breathing
unexpected pattern with periods of apnea and irregular breathing at varying depths
brain injury, meningitis, resp. depression
Pleural friction rub
May be felt on palpation of respiratory system, felt as a “grating” sensation
can also be heard on auscultation
How often should the pt perform TCDB and IS
TCDB q1h or q2 hours when asleep
IS 4-10 times per hour
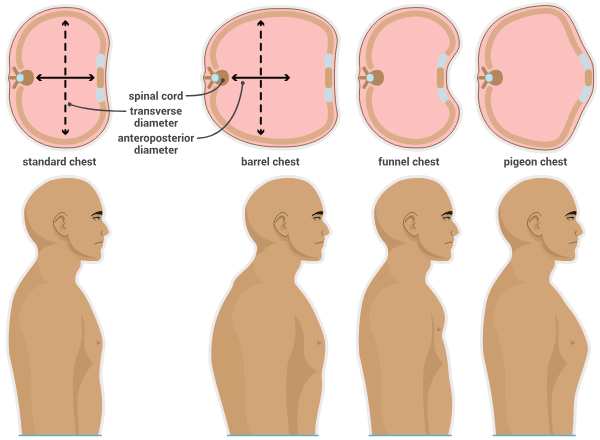
Types of breath sounds
tracheal - high pitch/loud intensity
bronchial - high pitch/loud intensity
vesicular - intense and loud airflow in the upper anterior lobes but have a softer intensity with a low pitch throughout the other lobes. These breaths are soft-sounding like wind blowing through trees
bronchovesicular - especially on the right—have a moderate intensity and pitch
Crackles
fine pops like a rice crispy treat
wheezes
whistling sound
Rhonchi
Low pitched bubbling/snoring sounds
Stridor
High-pitched sound during breathing, often indicating airway obstruction.
Assessment of jugular and carotid arteries
HOB @ 35° to 45° angle
Position yourself on the pts right side and inspect the neck for its tone, symmetry, veins, and pulsations.
Ask the pt to turn their head away from you and use your penlight to inspect the jugular vein area for pulsations (located on top of the sternocleidomastoid muscle). It is expected to observe a slight visible pulsation in the jugular area without distention of the veins.
absent pulsation of the carotid arteries is abnormal
What does JVD indicate?
R sided heart failure
Are visible pulsations in the PMI area normal?
Yes but may not be
should not be prominent and thrusting (heave/lift)
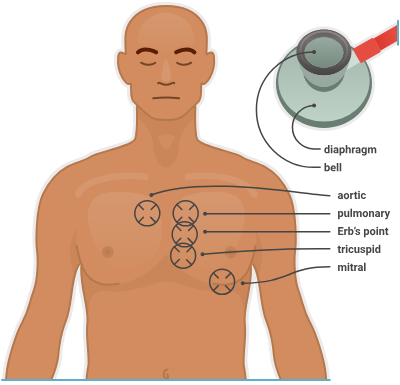
What should you use the bell vs diaphragm for? (stethoscope)
The diaphragm is used to listen to high-pitched heart sounds such as S1, S2, and some murmurs.
The bell of the stethoscope is used to identify unexpected lower-pitched sounds, such as S3 and S4.
Auscultation pattern for heart sounds
APe To Man
Normal nail bed curve
160 degrees
Peripheral arterial disease (PAD)
Reduced blood flow to the limbs (arteries carry blood AWAY from the heart)
pain with activity
skin is cool and shiny, pale, hairless
weak or absent pulses
Peripheral venous disease (PVD)
Veins not taking blood back to heart (blood pooling)
edema
skin is warm, thick, brownish, tough
pulses are present
pain is worse when standing and improves when sitting or elevating the legs.
Unexpected findings for breast tissue
Thickened rough skin, unilateral dilated veins, dimpling of the skin, edema, inflammation, or a unilateral rash are all findings associated with breast cancer.
Peau d’orange is when the breast tissue resembles the skin of an orange. It is caused by edema, which dilates the hair follicles. This finding is associated with breast cancer.
An inflamed, warm, edematous breast can indicate the presence of an infection in the breast tissue.
Screening for breast cancer
Self exams: should be done 4-7 days after start of menstrual cycle
Mammograms: beginning at age 50 q2 years for average risk and 40 for increased risk
done until age 74
congenital dermal melanocytosis
Often appears in infants with darker skin on lumbosacral area/near the shoulders… should not be mistaken for bruising.
When are tonsils able to be visualised in children
The tonsils are not usually able to be visualized until 6 to 9 months of age and will appear enlarged throughout childhood.
What pulse should you assess in patients less than 2 years of age instead of the carotid?
Brachial
Heart murmurs in children
In addition to S1 and S2, S3 may be heard in some children.
An S3 sound occurs during ventricular filling, sounds like the word Kentucky, and can be considered normal in children.
The presence of S4 on auscultation is always a pathologic finding, and sounds like the word Tennessee.
Types of pain scales for infants
neonatal infant pain scale (NIPS) (birth-12mo)
Riley infant pain scale (RIPS) (up to 12 mo)
r-FLACC (infant-7 years and for non-verbal)
Types of pain scales for children
FACES (3-8 years)
Visual analog scale (7+ years)
Numerical scale (8+ years)
Palmar grasp reflex
A reflex in infants that causes them to grasp objects placed in their palms
should be gone by 3mo of age
normal newborn HR
110-160 BPM
normal newborn RR
30-60 breaths per minute
count for 1 full min
Ear placement on infants
The pinna of the ears should be aligned with an imaginary line drawn horizontally from the outer eye canthus; ears set lower than that line may be associated with genetic disorders.
Ronchi in the newborn
rhonchi presents immediately after delivery and should clear by 48 hr of age
Murmurs in newborns
A soft murmur is expected for the first 24 hr of the newborn’s life
Moro (startle reflex)
With the newborn in the supine position, holding the newborn’s hands, pull the newborn up about 1 to 2 cm from the surface, then quickly let go. The arms abduct, at the shoulder, then extend outward with fingers spread, followed by flexion and abduction.
This reflex should disappear by 6 months of age.
Rooting reflex
With stroking of the cheek, the newborn turns to that side and makes a sucking motion
(should disappear by 3 months of age).
Stepping reflex
Hold the infant in a vertical position with the feet in contact with a flat surface. The infant lifts the feet alternately as if stepping
(disappears by 1 to 2 months of age).
Tonic neck reflex
With infant in supine position, turn the head to one side—the upper and lower extremity on that side extend, while the contralateral extremities flex (fencing posture).
This reflex disappears by 6 months of age.
Nevus simplex
‘stork bites’ common in infants, not abnormal
Fine pincer grasp
Usually occurs by 12 mo of age
Fontanel closure times
The posterior fontanel closes between 6 weeks to 2 months of age.
The anterior fontanel will close on average in the majority of infants by 18 months of age.
Babinski reflex
Stroke along the lateral portion of the sole of the foot, up across the plantar area. With a positive sign, the toes splay and extend with the particular extension of the great toe.
This reflex is a typical finding in infants to 1 year of age
flexion is a negative babinski, should occur s/p 1 year
Nagels ’s rule for determining due date
LMP - 3mo + 7 days
Classic manifestations of preeclampsia
Headache, vision changes, epigastric pain, abd pain, edema of face and hands
With false labor the cervix does not __
Dilate or efface
Fundal height measurment
From weeks 18-30, the fundal height (in cm) is the same as the weeks of gestation
have pt empty bladder first!
Symphysis pubis to top of fundus (measure)
Latent phase of labor (1st stage of labor)
Cervix softens/effaces to allow for dilation
Active phase of labor (1st stage of labor)
Cervix dilates, fetal presenting part descends