Week 5 - SA Ortho, Bandaging
1/171
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
172 Terms
1) Observation (Stance/posture while sitting and standing; Gait at walk/trot)
2) Joint and long bone palpation (Range of motion; Joint stability (e.g., cranial drawer test))
3) Discomfort response tests
4) Sedated orthopedic exam (Recheck joint stability without competing muscle tension as in the Ortolani or shoulder abduction angle tests)
5) Follow with site specific diagnostics
Radiographs, US, CT, MRI, arthrocentesis
What are the steps/components of a thorough orthopedic exam?
- Painful in the hind end (likely right hind given toe touching); Shifting weight to the front
What does this patient's stance tell you?

- False
True or false: It is best to assess a dog's gait while putting tension on the leash.
- Trot
For a gait analysis, the _____________ is the best gait.
- Caused by difficulty flexing a joint
- Infraspinatus contracture
What causes circumduction? Provide an example of a specific etiology which would cause circumduction.
- Sound
- Painful
When observing for forelimb lameness, if a head bob is noted, the head will be down when the ____________ leg hits the ground and up when the __________ leg hits the ground. This decreases weight on the painful limb.
- Elevates hip when painful hind limb touches the ground
- May increase weight bearing on forelimbs (dropping the forequarters)
- Hind leg spends less time on the ground
- Head bob: head down on diagonal painful hind leg
What are some signs of hindlimb lameness when assessing a patient's stance/gait?
- Hip dysplasia (it hurts on extension so rather than fully extend the limb they hop forward from a partially extended position)
Bunny hopping is indicative of what orthopedic abnormality (most commonly)?
- Joint subluxation or luxation
During palpation, an out of place joint landmark would indicate what?
- True
True or false: During long bone palpation, one should palpate firmly rather than gently.
- Squeezing over muscles and nerves will get you false + response
Why is it important to know the anatomy of vessels/nerves in the limb when performing a long bone palpation?
- Fractures
- Panosteitis
- Bone tumors
- Osteomyelitis
Long pain palpation can assist in the diagnosis of what pathologies?
- Hold the bones proximal and distal to the joint
How does one isolate a joint being examined?
- Isolate the joint being examined
- Examine range of motion (flex, extend, abduct, adduct; may increased in some directions but decreased in others)
- Check for joint instability (cranial/caudal and medial/lateral)
How does one generally perform a joint palpation?
- Signs of an osteoarthritic joint on physical exam
- Joint capsule hypertrophy
- Periarticular osteophytes
- Crepitus (sensation when joint capsule is rubbing over periarticular osteophytes)
- Pain
- Reduced ROM
- Infilling
What are signs that a joint is in distress? (Know for exam)
- Joint effusion
- Arthritis joints "hate" full range of motion (pain at full extension/flexion)
- Palpation of periarticular osteophytes
What are signs of an osteoarthritic joint on physical exam? (Know for exam)
- Acromial process of the scapular spine
- Greater tubercle of the humerus
What are the joint landmarks for the shoulder? (Know for exam)
- Acromial head of the deltoid muscle
- Supraspinatus
- Scapular head of the deltoid muscle
Which muscles of the shoulder can be palpated?
- Shoulder muscle atrophy
If the scapular spine is palpable, what does this indicate?
- False; Generally will not be able to feel joint effusion
True or false: If present, one can palpate shoulder joint effusion
- OCD of the humeral head
- Biceps tenosynovitis
Commonly, resistance to shoulder extension indicates _______________________________ while resistance to shoulder flexion indicates _____________________ (not always for either).
- Flex the shoulder, extend the elbow, and palpate the biceps tendon medial to the humeral greater tubercle (this works by maximizing the tension on the biceps brachii muscle, which crosses both the shoulder and elbow to extend the shoulder and flex the elbow)
How does one perform a biceps tenosynovitis test?
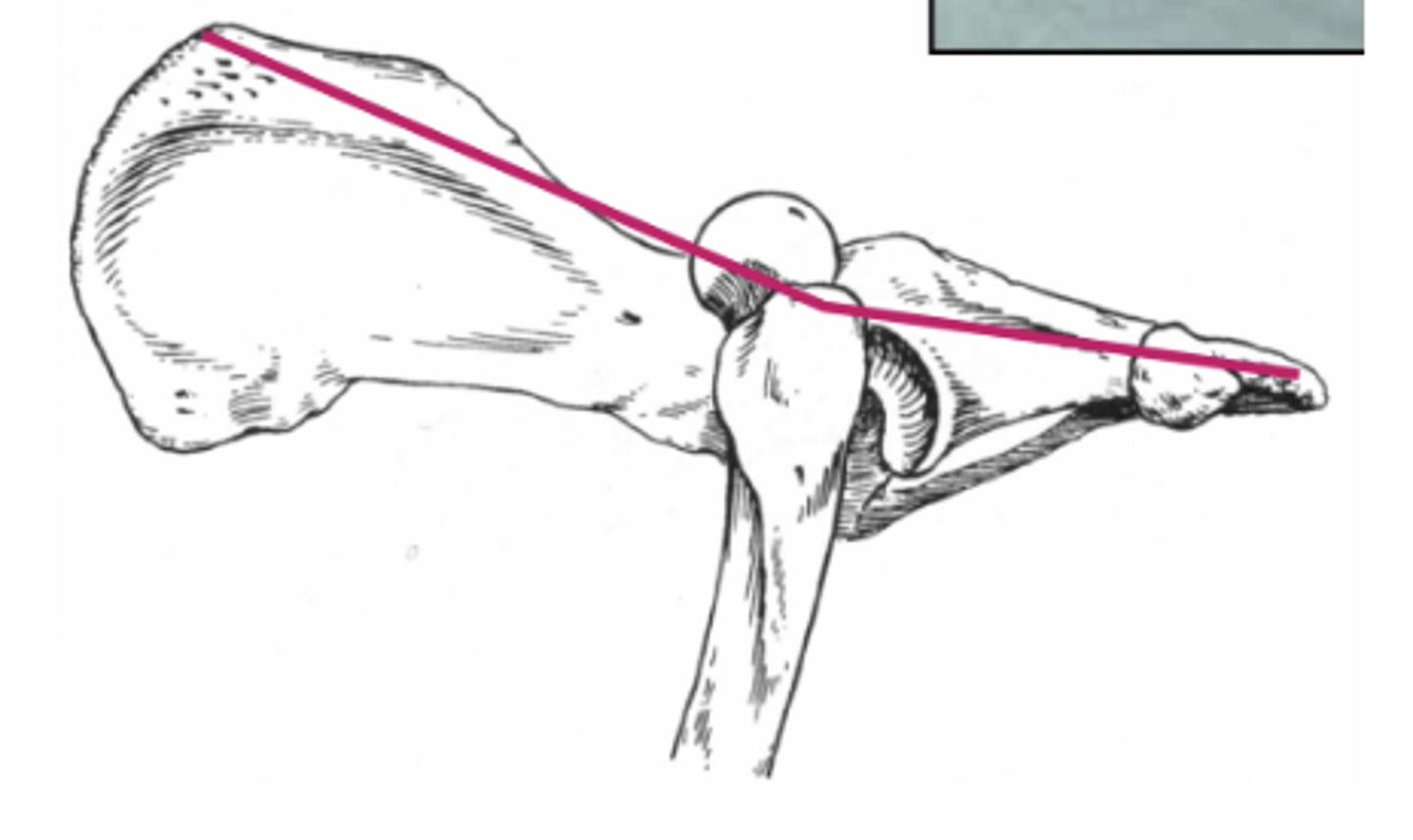
- Tests integrity of medial joint stabilizers (> 32 degree -> Medial shoulder instability)
What is the purpose of a shoulder abduction test?
- Pain and/or swellings
Generally, one palpates the brachium/humerus for what?
- Tough to find a window to palpate without accidentally squeezing muscle or nerves (try distal and medial)
What is a limitation to palpating the brachium/humerus?
- Elbows abducted and paws externally rotated (often to reduce loading on the medial side of the joint due to fractured medial coronoid processes)
- May keep elbows in extension when laying down (flexion is painful)
- Skinny forearms/atrophied forearm muscles
What are some observational signs of elbow pain?
- Olecranon
- Medial and lateral epicondyles
- Triceps muscles
- Joint
What are palpation landmarks of the elbow? (Know for the exam)
- False
True or false: The anconeal process is palpable.
- Normal dogs will have a "valley" between the epicondyles and the olecranon. Dogs with joint effusion will have thickening or a "water balloon" filling effect in the "valley".
How does one palpate for elbow joint effusion?
- Anconeus muscle
When palpating the elbow for joint effusion, what can sometimes be confused with swelling in the region laterally?
- Elbow arthritis (Such as caused by elbow dysplasia)
Resistance to flexion of the elbow often indicates what?
- Ulna
What is the most common/easiest to palpate bone in the antebrachium?
- Antebrachium
What is a good location to palpate long bones for panosteitis in the forelimb?
- Problem with the carpal joint -> Likely requiring surgical intervention
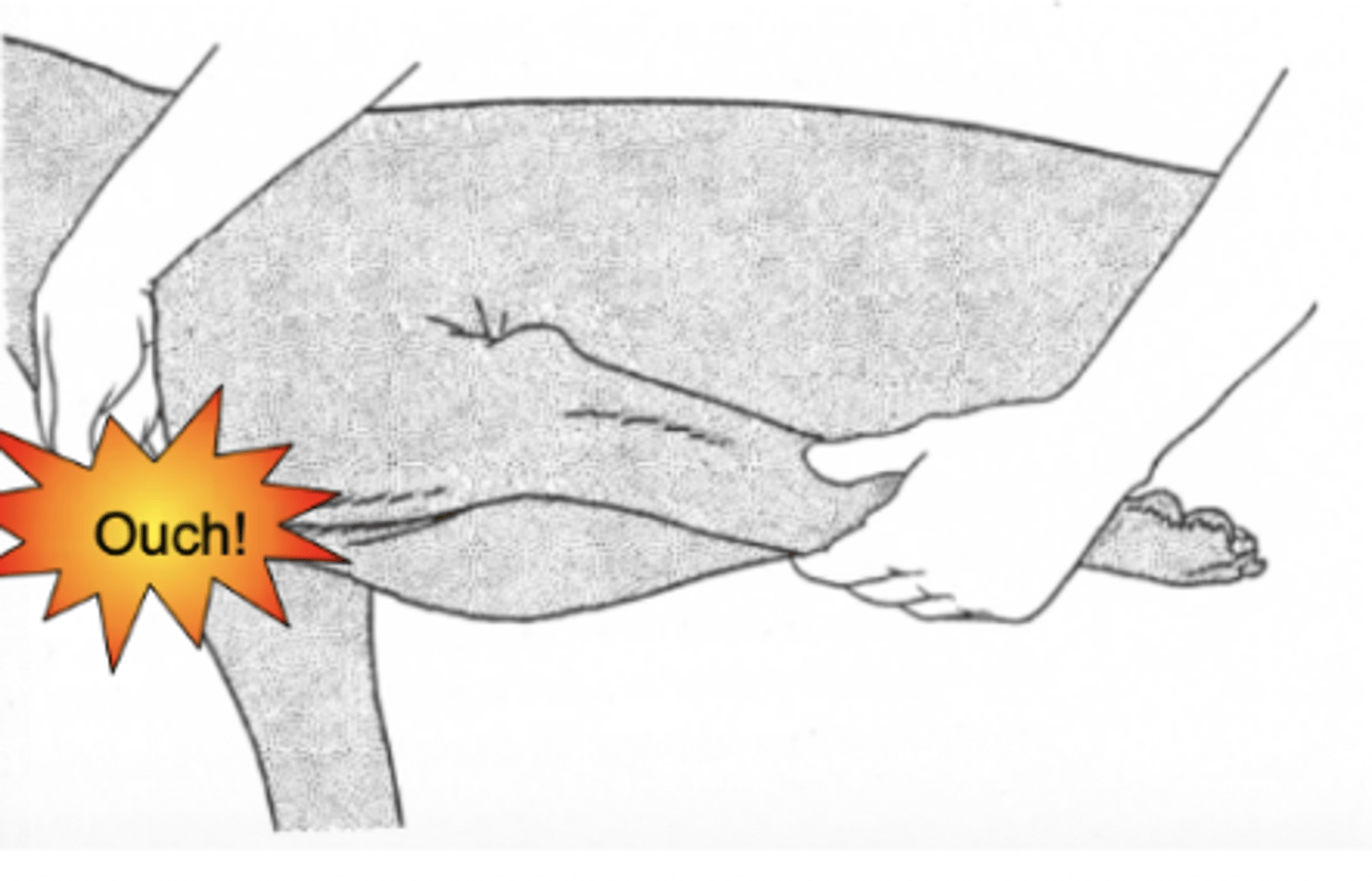
If an animal presents with a palmagrade stance/palmar hyperextension, what does this most often indicate?
- A pathology which commonly occurs in growing dogs in shelter populations resulting in hyperflexion and/or hyperextension of the carpus and "bucked" carpi. It resolved with time but may require splinting.
Briefly describe puppy carpal laxity syndrome.
- Arsenic
Radial hemimelia is related to _______________ toxicity.

- Medial and lateral styloid processes
- Accessory carpal bone
- Antebrachiocarpal joint
What are the palpation landmarks for the carpal joint? (Know for exam)
- In strong flexion, palpating cranially just distal to the radius (If there is joint effusion you won't be able to feel the "dimple" that is normally there)
How is the carpal joint most easily palpated?
- The paws
What is the most common source of lameness?
- Extension: 5 to 10 degrees beyond vertical
- Flexion: Almost touches the toes to the caudal antebrachium
What should be the maximum ROM for the carpus in flexion and extension?
- SDF
- DDF
A "Dropped toe" is caused by a torn ____________ while a "knocked up toe" is caused by a torn _____________.

- False
True or false: A broken toe will heal on its own.
- True
True or false: Dogs and cats do not have "growing pains"
- Ileopsoas tendinopathy (pelvis flexed, hind limbs extended)
This stance is highly indicative of what pathology?

- Their weight shifts to the thoracic limbs, resulting in hypertrophy of the shoulders and atrophy of the gluts.
Why do dogs with bilateral hip dysplasia develop a "body builder appearance"?
- Shortened leg
- Externally rotated and adducted limb
What are signs of a craniodorsally luxated hip?

- Iliac crest
- Ischiatic tuberosity
- Greater trochanter of the femur
- Normally, these landmarks should make a triangle (when feeling this triangle, the middle gluteal muscles should fill the curve of your hand - otherwise they are atrophied)
What are the joint landmarks for the hip joint? (Know for exam)
- They form a line
Describe the position of the landmarks of the hip joint in craniodorsal hip luxation.
- True
True or false: One cannot palpate joint effusion in the hip joint.
- Pain on extension usually indicates hip disease. However, extreme hip extension will also extend the lumbosacral joint and elicit a pain response in patients with lumbosacral disease.
Why must one be careful to diagnose hip disease when the patient is painful on full hip extension?
- Hip OA (usually secondary to hip dysplasia)
- Femoral head and neck fractures
- Lumbosacral disease
- Iliopsoas tendinopathy
What are some causes of pain on hip extension?
- Sedation
Tests for hip laxity should be performed with _________________.
1) Hip and stifle flexed at 90 degrees
2) Subluxate the hip joint by adducting the femur and pushing dorsally (A normal hip won't do this. This part is also called the Barlow test.)
3) While maintaining dorsal pressure on the femur, slowly abduct the femur.
4) You will feel and hear a "clunk," "click," or "thud" as the femoral head slips back into the acetabulum (Dogs with normal hips or advanced arthritis from hip dysplasia will have a negative Ortolani)
How does one perform/interpret an Ortolani's Test?
- GSDs
Which dog breed tends to get Gracillis and semitendinosus fibrotic myopathy?
- Commonly indicative of a CCL tear
What does medial buttress of the stifle joint/proximal medial tibia indicate?

- Patella
- Patellar ligament
- Joint space (just caudal to patellar tendon with a "valley" medially; With stifle joint effusion this "valley" will fill, making it hard to palpate the caudal border of the patellar ligament)
- Tibial tuberosity
- Fabellae
- Fibular head
What are the palpation landmarks for the stifle joint? (Know for exam).
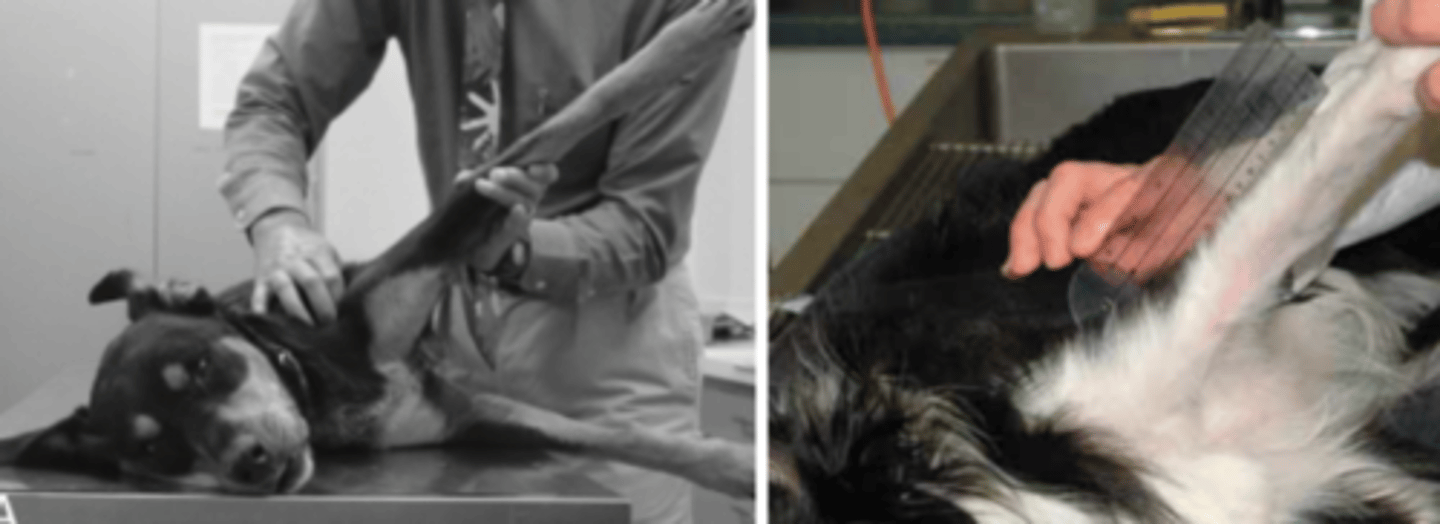
1) Recumbent or standing
2) Easier to learn on a sedated or very relaxed dog
3) Grasp the lateral side of the stifle
4) Index finger on the patella, thumb on the femur fabella
5) Other index finger on the tibial tuberosity, thumb on the fibular head
6) Push the proximal tibia cranially with your thumb
How does one palpate for cranial drawer?
- False; Test in both (flexion will detect partial tears)
True or false: The cranial drawer test should only be performed in stifle flexion, not extension.
- Sedation
Ideally, the cranial drawer test should be performed with _____________.
- Keep stifle and hock extended, then flex the hock
- Watch/feel for cranial displacement of the tibial tuberosity
- In complete tears the knee will buckle forward
How does one perform a tibial compression test?
- Medially: Extend the stifle, rotate the toes medially, and push the patella medially
- Laterally: Partially flex the stifle, rotate the toes laterally and push the patella laterally
How does one palpate for patellar luxation medially and laterally?
- Tibia
Which bone in the hindlimb is easy to palpate for long bone pain?
- Left: Normal
- Middle: Plantigrade stance (common calcaneal tendon rupture)
- Right: Plantrigrade stance with flexed toes (Gastrocnemius avulsion with SDF intact)
Describe each stance and a common cause of each (if they are pathologic).
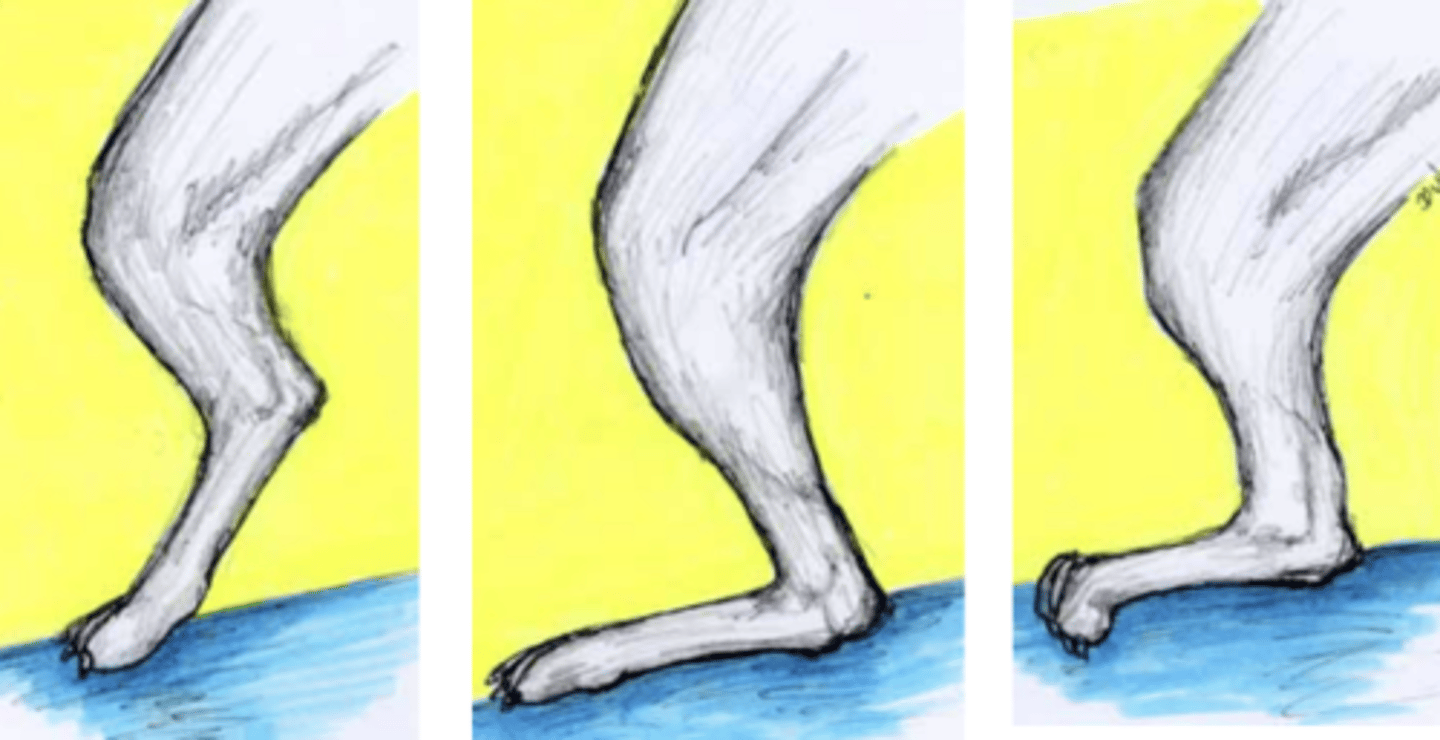
- Plantigrade means the hock has increased flexural instability with weight bearing (In severe cases the calcaneus touches the ground and surgical intervention is usually required)
What does a plantigrade stance of the hock joint indicate?
- Calcaneal fracture
- Talocrural joint luxation/ fractures
- Intertarsal joint luxations/ fractures
- Tarsometatarsal joint luxations/ fractures
- Rupture of Gastrocnemius or Common calcaneal tendon
- Fractures of all metatarsals
- Polyneuropathy secondary to diabetes or endocrinopathy
- Collagen synthesis disorders
- CATS: Sciatic neuropathy/ palsy/ weakness
What are some causes of a plantigrade stance of the hock joint?
- Medial and lateral malleoli
- Calcaneus
- Common calcaneal tendon
- Talocrural joint space: Valley between the malleoli and calcaneus
What are the hock joint palpation landmarks? (Know for exam)
- Hock OCD (common in labs and rotties)
What is the most common cause of hock joint effusion?

- Often hyperextended hocks and very lame
Describe the typical stance/degree of lameness in dogs with hock OCD.
- Hemostasis/coagulation
- Inflammation
- Proliferation
- Remodeling
What are the phases of wound healing?
- Hemorrhage -> peripheral vasoconstriction -> hypoxia -> platelet activation, adhesion, aggregation -> coagulation cascade -> blood clot formed
- Blood clot is scaffold for migrating cells
- Degranulating platelets release chemoattractants, stimulates migration of cells to promote healing
What is involved in the hemostasis/coagulation phase of wound healing?
- Early phase = neutrophil recruitment (peaks 1-2 days)
- Late phase = monocytes appear and transform (days to weeks)
What is involved in the inflammation phase of wound healing?
- Fibroplasia
- Angiogenesis
- Epithelialization
What is involved in the proliferation phase of wound healing?
- Wound contraction
- Maturation
What is involved in the remodeling phase of wound healing?
- Protect from environment
- Absorb exudate
- Prevent/reduce edema
- Eliminate dead space, prevent seroma formation
- Keep topical medications/dressings in place
- Facilitate debridement
- Support/stabilization/immobilization
- Improve aesthetics
What are some reasons for bandaging a wound?
- Primary (contact layer)
- Secondary (padding layer)
- Tertiary (outer layer)
What are the general layers of a bandage?
- Holds dressing in place, absorbs exudate, and provides padding
What is the function of the secondary/padding layer of a bandage?
- Hold padding in place, provide compression/stabilization, and prevent contamination
What is the function of the tertiary/outer layer of a bandage?
- Wound dressing (+/- topical medications)
- A light layer to secure the dressing
What makes up the primary contact layer of a bandage?
- Absorbent/adherent
- Hydrophilic
- Semi-occlusive synthetic
- Antimicrobial
- Biologic
What are the various types of wound dressing?
- Gauze (dry or as wet-to-dry for heavily contaminated, necrotic, exudative wounds)
- Hypertonic saline dressing (2% NaCl impregnated)
What are some absorbent/adherent dressings?
- Usually only used in the bandage for the first few days -> strong osmotic draw leading to aggressive debridement and edema reduction (As it dries, the salt sticks to necrotic tissue and when it is pulled off the next day, it will pull off the necrotic tissue and leave healthy tissue)
- Aggressive form of debridement which is not fit for exposed bone (kills periosteum)
Describe how hypertonic saline dressing is used for debridement.
- Highly absorbent dressing used in the inflammatory phase of wound healing
When is a hydrophilic dressing used in a bandage?
- A hydrophilic wound dressing which absorbs up to 20-30 times its weight in fluid
- Used for exudative wounds in the inflammatory and early repair phases -> Calcium ion release promotes prothrombin activation
What is calcium alginate? What is it used for>
- Fabric synthetic dressings which can be petroleum impregnated or telfa pads
What are some semi-occlusive synthetic wound dressings?
- Perforated polyester film filled with compressed cotton
What is a Telfa pad?
- Vaseline petroleum gauze are adaptive and used in the repair phase once a healthy bed of granulation tissue is present and epithelialization is beginning
When/why are petroleum impregnated fabric synthetic dressings used for a wound?
- An antimicrobial wound dressing which has antimicrobial activities that are more compatible with tissues compared to chlorhexidine (sponge or roll)
What is Kerlix AMD?
- Use during inflammatory phase and when an open synovial cavity is present; Good for packing deep contaminated wounds for debridement, drainage, and reduction in bacterial numbers
- Resists bacterial penetration of wound site
When/why is Kerlix AMD used as a wound dressing?
- Barrier to protect from infection
- Maintains moist wound environment
- Discourages EGT formation
- Designed to become incorporated into wound (Scaffold for adhesion and migration of fibroblasts, vascularization, epithelialization)
What are the benefits of a biologic wound dressing?
- Amnion
What is an example of a biologic wound dressing?
- HA
- Cytokines
- Growth factors
What does amnion contain?
- Availability concerns
- Time consuming to harvest and process
What are the limitations of using amnion as a biologic wound dressing?
- Varies with type of wound, dressing used, and external factors, but considering the dressing used remember the inflammatory/debridement phase lasts 1-3 days and the repair phase lasts 4-7 days
When should a primary layer be changed?
- Iodine-containing dressings
- Antimicrobial gauze (I.e., Kerlix AMD)
- Silver-impregnated dressings/topicals
- Medical grade honey
What are options for management of a wound with a persistent/resistant microbial infection?
- Conforming gauze (brown gauze, soft roll gauze - remember these are abrasive)
- Cast padding (ideally sterile)
How is a dressing secured in the primary layer of a bandage?
- Elastikon (stretch prior and never place under tension)
What composes the "inner sanctum portion" of a primary bandage layer?
- Cotton roll
- Quilt padding
- Gamgee
- Cast padding
What materials can be used for a secondary (intermediate) bandage layer?
- +/- brown gauze
- Vet Wrap
- Elastikon
What materials can be used for a tertiary (outer) bandage layer?
- Porous
Materials used for a tertiary (outer) bandage layer should be _________________.
- Added compression
- Immobilization
- Additional protection
- Use under splints
What are the purposes of a Robert-Jones bandage?