Exercise Test & Rx in Pulmonary Patients
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
20 Terms
pulmonary diseases
-Significant causes of morbidity and mortality
-Pulmonary rehabilitation (PR): improves exercise tolerance, reduces symptoms, and improves quality of life
oKey focus: long-term behavior change for continued participation in PA and exercise
-How assessed?
*better at treating asthma now; know exercise good
*multiple types: chronic and episodic
*misdiagnose=vocal cord disruption
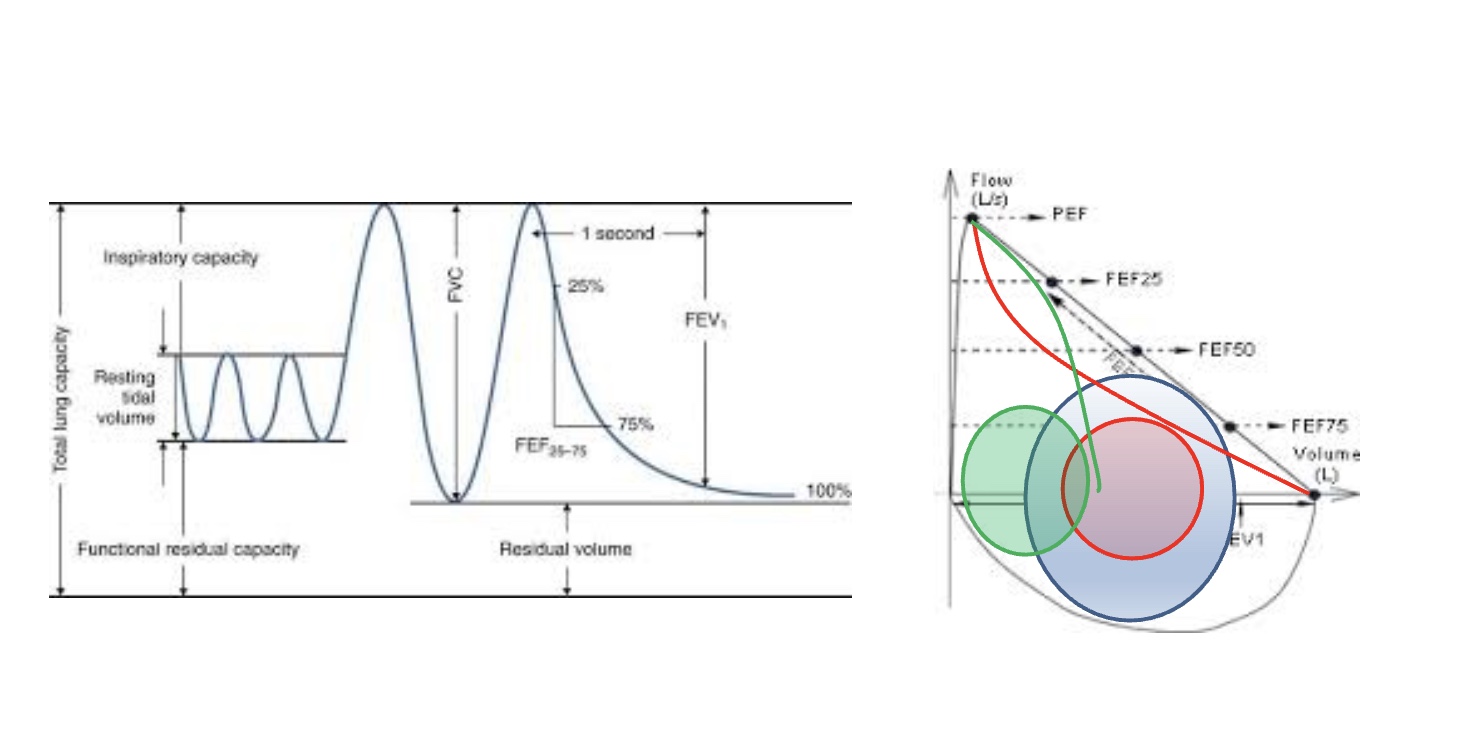
Pulmonary Function: (static) Normal, obstructive, restrictive
-big breathe in, blast out
-elasticity=ability to force air out
-total lung capacity=size of lungs; high TV means don’t have to breathe as fast
-restrictive: size of lungs smaller (ex: pneumothroax)
-obstructive: longer ait to come out, thing airway but lung same size; limits TV so breathe faster/short of breath (ex: asthma)
*either or disrupts TV; ex COPD
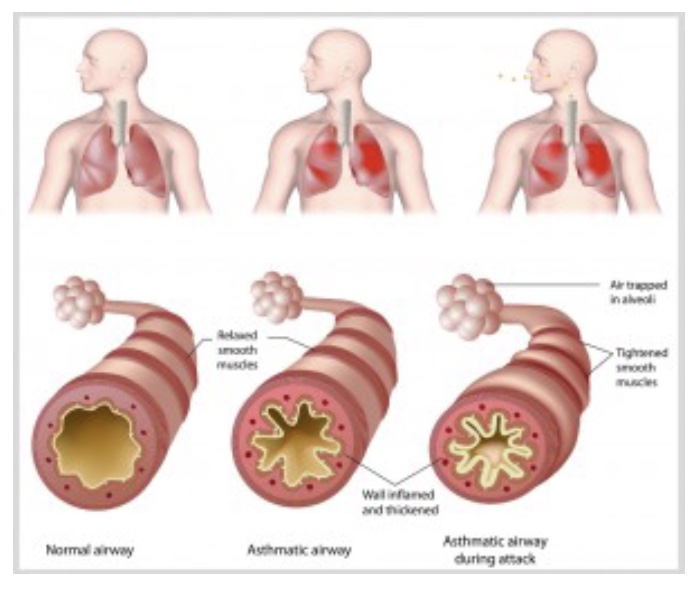
asthma: characterization
-Multi-factorial chronic inflammatory disorder of the airways
irritation from violant airfflow cause mucus narrows airway
-Characterized by:
oHistory of episodes of bronchial hyperresponsiveness; variable airflow limitation;
oRecurring wheeze, dyspnea, chest tightness, and coughing that occur particularly at night or early morning
-Variable and reversible symptoms
typically, but not always
bronchodilation so better airflow
-Provoked or worsened by exercise
-Deconditioning --> downward cycle or “spiral”
don’t exercise bc astham attack risk, but then ADL hard
mike Asthma review
-disrupts TV, so shut of breath and increase RR
-airway inflation → obstructive pattern in lungs
-Pulmonary function test=classic diagnostic tool
-reversible w/ meds, but not perfect (still some inflammation)
-asthma attack=narrow airways and mucus secretion
asthma & exercise Rx
-No conclusive evidence-based guidelines for exercise as effective therapy
*Mike disagrees: can’t cure asthma, but lower if PA (lower TV)
-Strong evidence for recommending regular PA
oGeneral health benefits and reduced incidence of exacerbations
oImprovements in days without asthma symptoms, aerobic capacity, maximal work rate, exercise endurance, and pulmonary VE
*intensity exercise=trigger, so better in shape=less risk
Exercise-induced bronchoconstriction (EIB)
-airway narrowing that occurs as a result of exercise
oExperienced in a substantial proportion of people with asthma, but people without a diagnosis of asthma may also experience EIB
oManaged with pharmacotherapy
*ex trigger: cold air
asthma and exercise testing
-Assessment of physiologic function should include evaluations of cardiopulmonary capacity, pulmonary function (before and after exercise), and oxygen saturation.
-Administration of an inhaled bronchodilator prior to testing may be indicated to prevent EIB, thus providing optimal assessment of cardiopulmonary capacity.
oDiagnosis vs. Management
-Typically performed on a motor-driven treadmill or an electronically braked cycle ergometer
oTargets for high ventilation and HR are better achieved using the treadmill.
oSports-specific mode for athletes
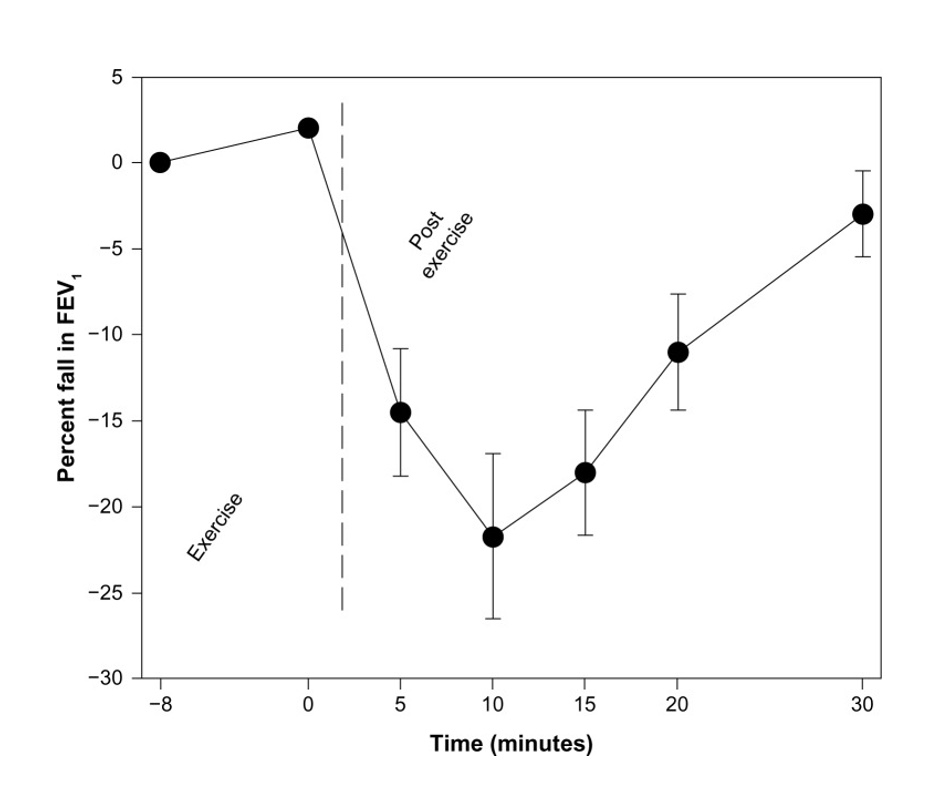
asthma and exercise testing criteria
-The degree of EIB should be assessed using vigorous intensity exercise achieved within 2–4 minutes and lasting 4–6 minutes with the individual breathing relatively dry air. (Rapid Acceleration Protocol)
oAccompanied by a spirometric evaluation of the change in (FEV1) from baseline and the value measured at 5, 10, 15, and 30 min following the exercise test.
oThe criterion for a diagnosis of EIB varies, but many laboratories use a decrease in FEV1 from baseline of ≥15% because of its greater specificity.
*test to provoke asthma; *not much warm up, get 85% HR quickly and stay there 6-8 mmin to induce asthma
*low FEV1=EIA
*treat w/ a bronchodialaltor
asthma and exercise testing physician supervision
-Physician supervision is warranted when testing higher risk individuals because severe bronchoconstriction is a potential hazard following testing.
oIf incident occurs--> Immediate administration of nebulized bronchodilators in addition to supplemental oxygen
-Evidence of oxyhemoglobin desaturation <80% should be used as test termination criteria in addition to standard criteria.
-The 6-MWT may be used in individuals with moderate-to-severe persistent asthma when other testing equipment is not available.
FITT for asthma
-goal: eliminate asthma much as can/control asthma
-should be relaxed when take inhaler
-begin with moderate intensity; time based on what can tolerate
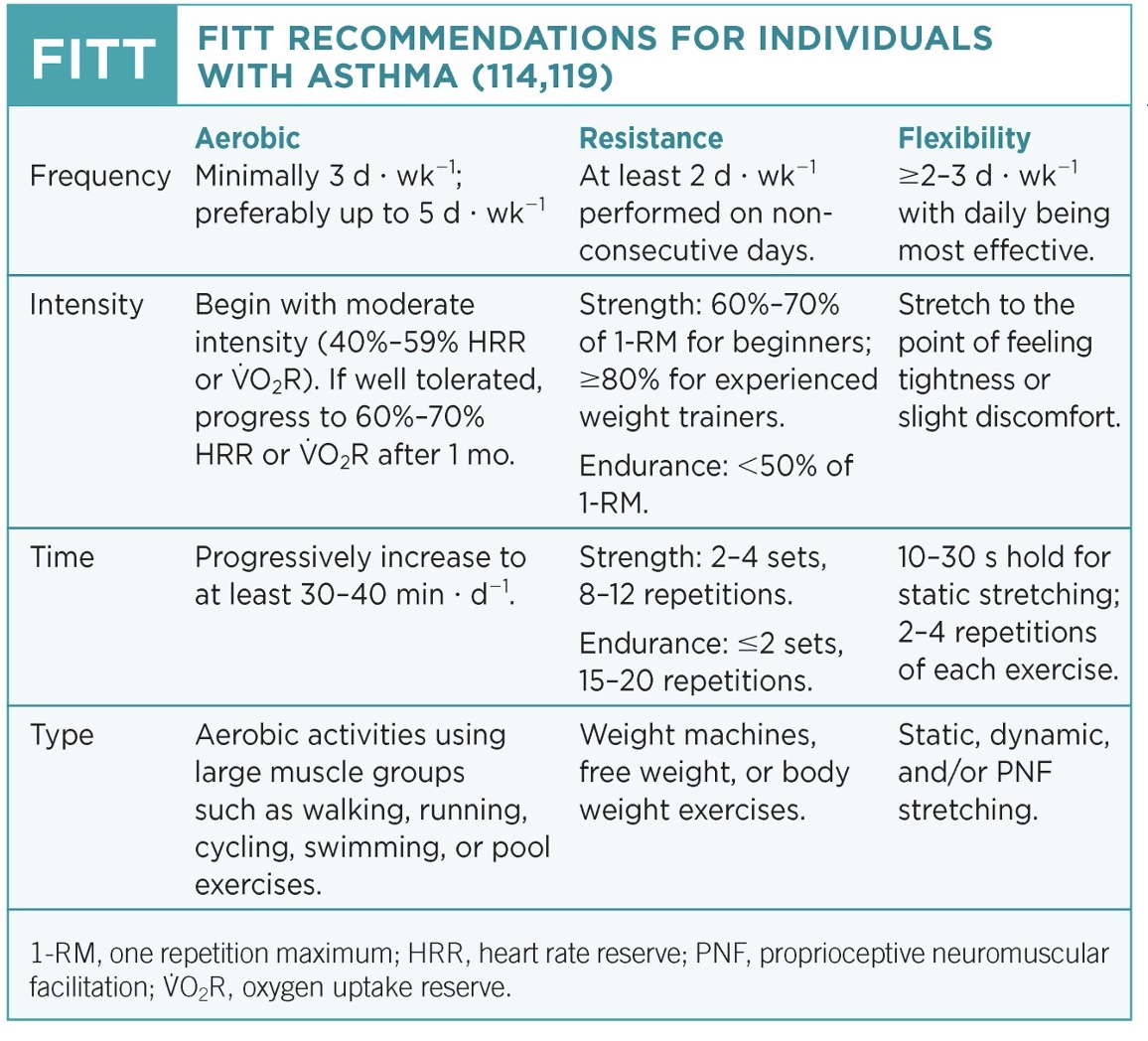
asthma and special considerations
-Caution is suggested in using intensities based on prediction of maximal heart rate (HRmax) because of the wide variability in its association with ventilation and the potential HR effects of asthma control medications.
*inhaler increases HR/SNS
-Individuals experiencing exacerbations of their asthma should not exercise until symptoms and airway function have improved.
-Use of short-acting bronchodilators may be necessary before or after exercise to prevent or treat EIB.
-Individuals on prolonged treatment with oral corticosteroids may experience peripheral muscle wasting and may benefit from resistance training.
-Exercise in cold environments or those with airborne allergens or pollutants should be limited to avoid triggering bronchoconstriction in susceptible individuals.
oEIB can also be triggered by prolonged exercise durations or high intensity exercise sessions.
*persistant in severe patient, but can be envionrmentally triggered as well
key points asthma exercise Rx
-try to control asthma, if so can do standard ACSM Rx
-if not controlled, change strategy or pre-treatment options (ex: agressive warm-up and BD)
Chronic Obstructive Pulmonary Disease
-Fourth leading cause of death and a major cause of chronic morbidity throughout the world
*smoking #1 cause, so highly preventable
-Characterized by chronic airway inflammation due to exposure to noxious gases and particles, especially tobacco smoke and various environmental and occupational exposures
*more permanent; difficult to treat; FEV1 to test; might need lung transplant
-Common symptoms: dyspnea, chronic cough, and sputum production
-Systemic effects: weight loss, nutritional abnormalities, sarcopenia, and skeletal muscle dysfunction (*bc higher metabolism)
-Encompasses chronic bronchitis and emphysema
*inflammation of airway w/ excess mucus OR chronic inflammation breaks down alveolar membrane so lower SA and lung hyperinflation
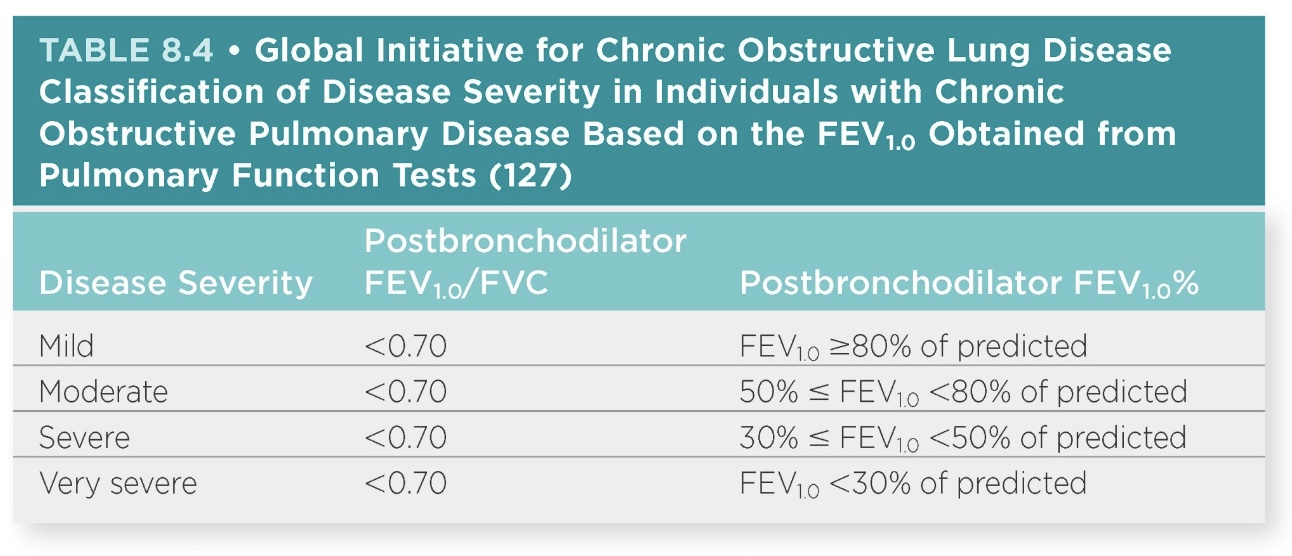
COPD and FEV1
->80%=normal
-severe=30%; ability to help them here is difficult
-likely asymptomatic if mild or moderate
COPD and exercise testing
-Evidence confirms the utility of cardiopulmonary exercise testing in adults with COPD as well as other chronic lung diseases (*but clinically significant?)
oRationale: Objective measure of exercise capacity, mechanisms of exercise intolerance, prognosis, and disease progression and treatment response
-Modifications of traditional protocols (e.g., smaller work rate increments) may be warranted depending on functional limitations and the onset of dyspnea.
oTest duration of 8–12 minutes in those with mild-to-moderate COPD
oTest duration of 5–9 minutes for individuals with severe and very severe disease
*can use BD, but have emphysema too
-Age-predicted HRmax may not be appropriate criteria for terminating a submaximal GXT. (*limited respiratory symptoms)
-A constant work rate (CWR) test using 80%–90% of peak work rate achieved from the GXT approximates the type of work-related activity levels likely to be encountered in everyday life. (*oxygen kinetics increase COPD (transit delay)
-The 6-MWT is a widely used exercise assessment tool for cardiorespiratory function in PR. (*look at O2 saturation)
oMinimal clinically important difference (MCID): mean of 30 m (98.42 ft)
-Incremental (ISWT) and endurance (ESWT) shuttle walk tests are also used to assess cardiopulmonary function in individuals with chronic lung disease. (*like pacer test have breaks)
-In addition to standard termination criteria, exercise testing may be terminated because of severe arterial oxyhemoglobin desaturation (i.e., SaO2 ≤80%).
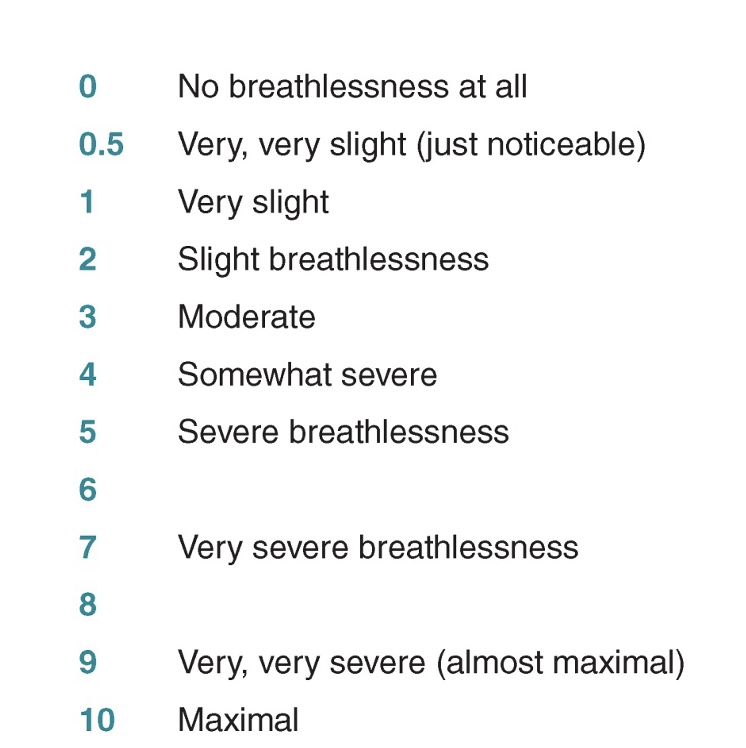
-Exertional dyspnea is a common symptom in people with many pulmonary diseases.
oModified Borg Category-Ratio 0–10 (CR10)
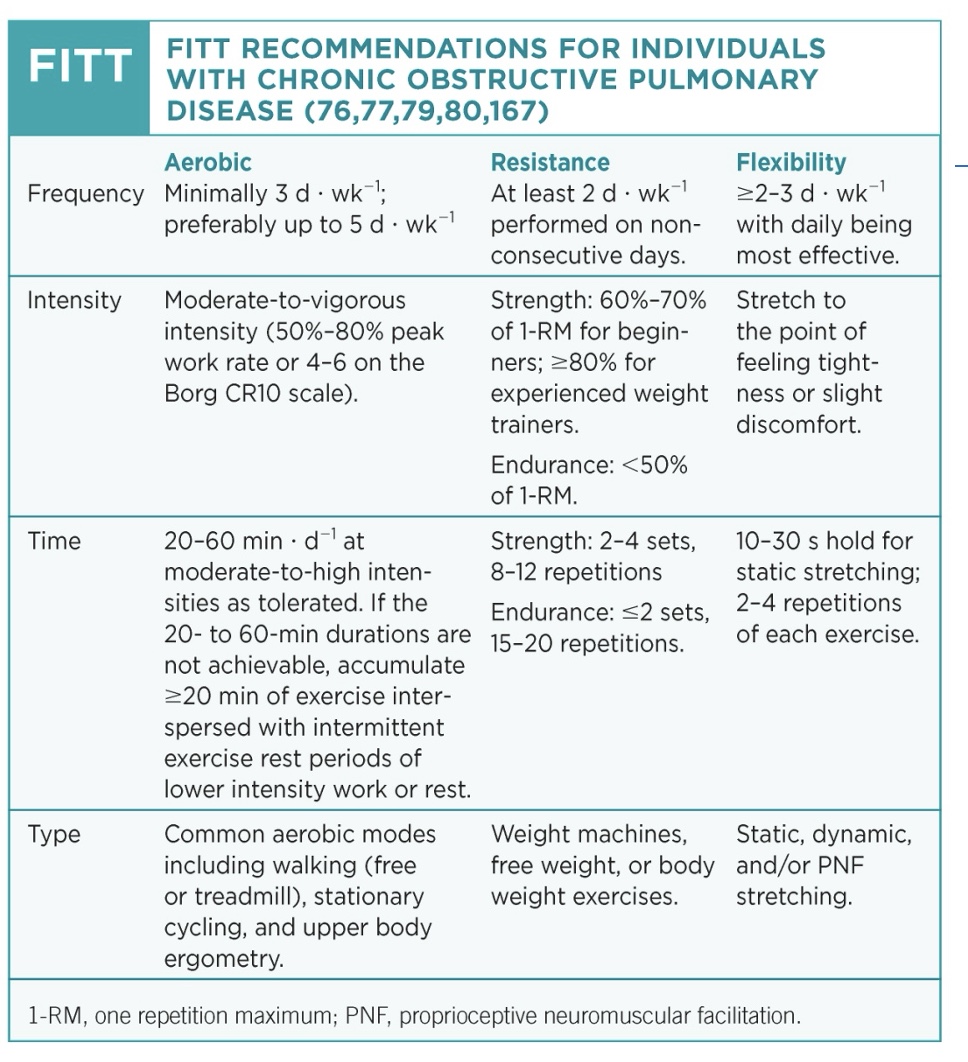
FITT for COPD
-dif than asthma; can do normal Rx but tend to have low body comp but normal BMI, so RT good
-aerobic: limited, so do to improve ADL; prefer everyday; not too formal
-resistance: do UB, Respiratory muscle training (use higher pressure so use accessory muscles/chest/diagram)
-flexibility: do UB so improve UE motion; expand/contract theory
*supplemental O2 also an option
COPD exercise considerations
-Higher intensities yield greater physiologic benefits (e.g., reduced minute ventilation and HR at a given workload) and should be encouraged when appropriate.
-For individuals with mild COPD, intensity guidelines for healthy older adults are appropriate.
oModerate-to-severe COPD: intensities representing >60% peak work rate
-Severe COPD or very deconditioned individuals: light intensity aerobic exercise
-Ventilatory limitation at peak exercise in individuals with severe COPD coincides with significant metabolic reserves during whole body exercise.
oMay allow these individuals to tolerate relatively high work rates that approach peak levels and achieve significant training effects.
-Dyspnea ratings of between 3 and 6 on the Borg CR10 Scale may be used
oCorrespond with 53% and 80% of VO2peak, respectively
-Intensity targets based on percentage of estimated HRmax or HRR may be inappropriate.
-The use of oximetry is recommended for initial training sessions to evaluate possible desaturation and to identify the workload at which desaturation occurred.
-Flexibility exercises may help overcome the effects of postural impairments that limit thoracic mobility and therefore lung function.
-Dyspnea or breathlessness may supersede objective methods of Ex Rx
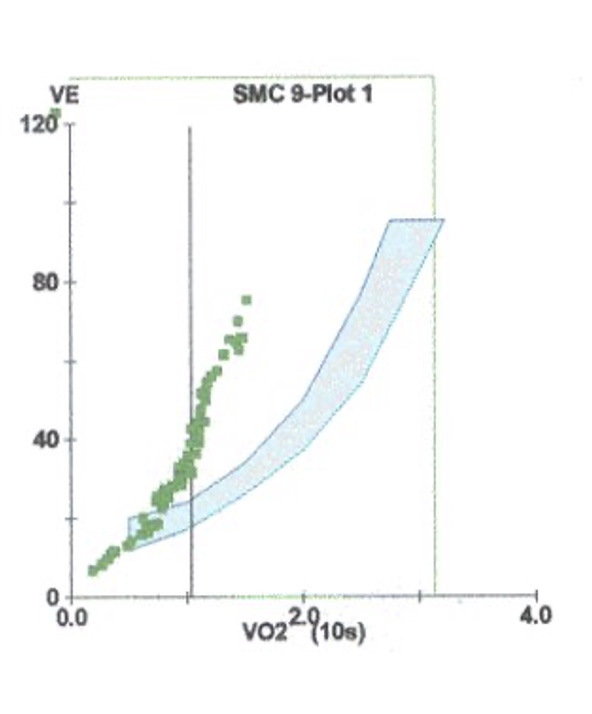
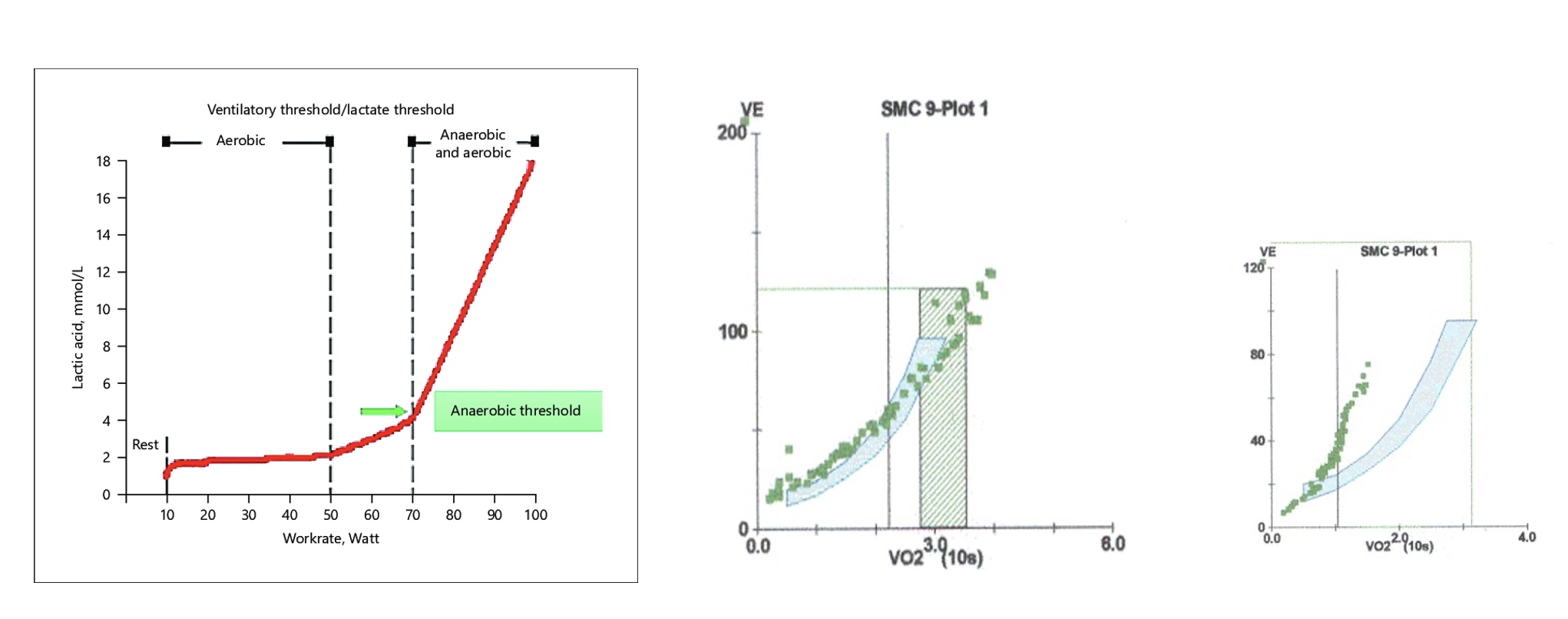
graphs OBLA normal person vs COPD person
-Rx below OBLA
*normal in middle, COPD far right
-COPD breathes twice as much
-increase ADL if can breathe easier; most efficent
COPD special considerations
-Peripheral muscle dysfunction contributes to exercise intolerance and is significantly and independently related to increased use of health care resources, poorer prognosis, and mortality.
oMaximizing pulmonary function (bronchodilators) before exercise in those with airflow limitation can reduce dyspnea and improve exercise tolerance.
-Because individuals with COPD may experience greater dyspnea while performing ADL involving the upper extremities, include resistance exercises for the muscles of the upper body.
-Inspiratory muscle weakness is a contributor to exercise intolerance and dyspnea in those with COPD.
oInspiratory Muscle Training (IMT) may prove useful in those unable to participate in exercise training; Improving inspiratory muscle strength and endurance, functional capacity, dyspnea, and quality of life may lead to improvements in exercise tolerance.
-No clear guidelines for IMT
oRecommendation: intensity of the training load of ≥30% of maximal inspiratory pressure
-Supplemental oxygen is indicated for individuals with a PaO2 ≤55 mm Hg or an SaO2 ≤88% while breathing room air.
oIn individuals using ambulatory supplemental oxygen, flow rates will likely need to be increased during exercise to maintain SaO2 >88%.
oEvidence suggests the administration of supplemental oxygen to those who do not experience exercise-induced hypoxemia may lead to greater gains in exercise endurance (particularly during high intensity exercise).
-Individuals suffering from acute exacerbations of their pulmonary disease should limit exercise until symptoms have subsided.
Exercise testing for Pulmonary diseases other than COPD
-Other pulmonary diseases will be covered in EXPH 3200
-Conditions that could benefit from exercise training:
oPulmonary artery hypertension
oInterstitial lung disease
oCystic fibrosis
oLung transplantation