11 - Motor Systems 2
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
53 Terms
what provides proprioception and kinesthetic awareness?
proprioceptors, exteroceptors
other sensory input includes vestibular, visual and auditory
proprioceptive information is used by CNS for
sensory awareness in cerebral cortex, motor control and planning in cerebral cortex and cerebellum, reflex responses in spinal cord and brainstem
where are mechanoreceptors located?
joint capsules, ligaments, menisci, tendon, muscle, skin and subQ tissue
what are the types of joint receptors?
Type I-IV
Type I joint receptors type, adaptation, information?
Ruffini-like ending
slow adapting
extremes of motion, stretch of capsule, sustained
Type II joint receptor type, adaptation, information?
lamellated corpuscle/Pacinian corpuscle-like
rapid adapting
changes in direction and speed, start/stop
Type III joint receptor type, adaptation, information?
GTO-like
slow adapting
extreme stretch, ligament of horns of menisci
Type IV type, adaptation, information?
FNE - C and A-delta
slow adapting
mechanoreceptors and nociceptors, mechanical and chemical
joint receptors respond to _______.
specific arc of motion
T/F most joint receptors have high density.
F, varies with location
what receptors are specific vs general?
general: FNE, Ruffini’s endings, Pacinian corpuscles
specific: golgi tendon organ, muscle spindles
what is an extrafusal fibers? intrafusal fibers?
skeletal muscle, contractile elements in the skeletal muscle
what attaches to a single golgi tendon organ? what does it consist of? what kind of nerve fiber in GTO?
around 20 muscle fibers
thin nerve fibers intertwined with collagen strands
Ib afferent fiber - heavily myelinated fast axon
what is the stimulus for a golgi tendon organ?
muscle tension
what is the sequence of golgi tendon organ reflex?
force → stretches GTO → Ib afferent fiber → (+) interneurons → (-) motoneurons of same muscle
muscle spindle function
gives signals of static muscle length, changing dynamic muscle length, and limb position (with info from other receptors)
CNS can adjust gain or sensitivity of muscle spindle
what are the contractile and noncontractile regions of a muscle spindle?
contractile: ends of the muscle spindle
noncontractile: center of the muscle spindle
what happens during change in muscle length?
spindles are in parallel with muscle and would shorten
what are the 2 types of intrafusal muscle fibers?
nuclear bag and nuclear chain
both carry different kinds of information back to the CNS
contractile ends are innervated by? what do they do?
noncontractile centers are innervated by? respond to? what do they contain?
gamma-motoneurons, carry information to contract/relax muscle. they adapt to the length of extrafusal fibers; by working with alpha-motoneurons in extrafusal muscle to maintain/alter sensitivity
Ia or II sensory afferent endings, respond to stretch, contain nuclei
nuclear chain and static nuclear bag (bag2) fibers respond to? type of MN?
sensitive to change in length only
static gamma-motoneurons
dynamic nuclear bag (bag1) fibers respond to? type of MN?
sensitive to rate of change in length
dynamic gamma-motoneurons
how do nuclear chain and static nuclear bag fibers and dynamic nuclear bag fibers differ?
contractile properties, passive mechanical properties
sensory fibers terminate on _______ of intrafusal fibers (IFF)
central region
what happens when muscle is stretched?
whole muscle stretch → stretch of intrafusal fibers (IFF) → stretch of central region → depolarization of afferent endings
where do primary endings (Ia) fibers (afferent) terminate? what fiber do they have the greatest response to?
all types of IFF
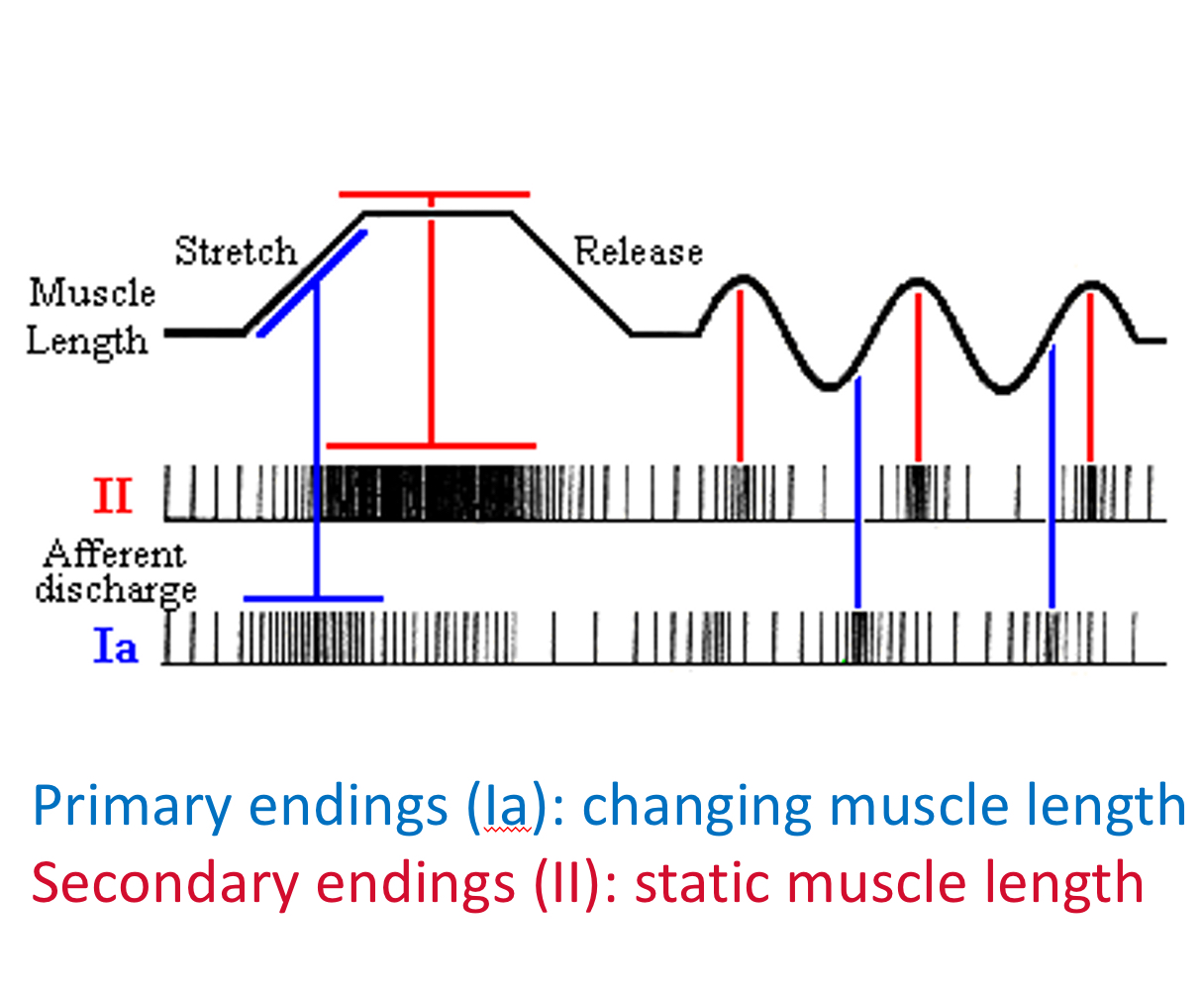
greatest response to stretch of dynamic nuclear bag fibers, changing length
where do secondary endings (II fibers) terminate?
nuclear chain and static nuclear bag fibers
static (absolute) length
what is alpha/gamma coactivation?
simultaneous activation of both alpha and gamma motoneurons in the CNS, helps with adjusting length of muscle spindle to length of surrounding muscle
visual of response to stretch
T/F intrafusal and extrafusal fibers generally contract simultaneously
T, CNS activates both alpha and gamma motoneurons, adjusts lengths of muscle spindle to length of surroudning muscle
often referred to as alpha/gamma coactivation
which motoneuron is task specific?
gamma motoneurons, the degree of gamma-mn activation is greater with tasks that require more precise movement
where are the control centers of gamma motoneuron activation?
near red nucleus - UE flexion
reticular formation
vestibular nuclei - LE extension
substantia nigra pars compacta
what is the “gamma loop”?
gamma-motoneurons activated by CNS → intrafusal fiber contraction → AP along Ia fiber endings → enhance excitation of a-motoneurons → increase extrafusal muscle contraction
GTO vs muscle spindle
GTO (Ib) - muscle tension, force of contraction, tension on tendon and passive stretch
muscle spindle (Ia, II) - primary endings Ia are responsible for changing muscle length and speed of movement and secondary endings are responsible for muscle length, joint position and static position
reflex definition
involuntary stereotypes responses to specific sensory stimuli - the locus of stimulus determines the muscles that will contract, the strength of the stimulus will determine the strength of the response
spinal reflexes - all circuitry for the reflex is located in the spinal cord
why are spindle fibers important
help with proprioception
reflex def
involuntary stereotyped responses to specific sensory stimuli
the locus of stimulus determines the muscles that will contract, the strength of the stimulus will determine the strength of the response
what are spinal reflexes
all circuitry for the reflex is located in the spinal cord
what modulates the reflex response?
descending influences
what is the stretch reflex? what is the phasic component of a stretch reflex?
deep tendon reflex, muscle stretch leads to Ia afferent sending signal to alpha motoneuron for muscle contraction (homonymous/synergistic muscles)
rapid, brief muscle contraction that occurs in response to a sudden stretch
how does a stretch reflex work?
a muscle is stretched, Ia afferents travel to SC and synapse with alpha motoneuron which then sends signal back to muscle to contract homonymous and synergistic muscles
reflex categories
absent or weak
hyperactive/excessive
muscle spindle reflex connections
type Ia afferents have monosynaptic EPSPs and multisynaptic IPSPs
monosynaptic EPSPs have homonymous muscle α-motoneuron and synergistic muscle α-motoneuron
multisynaptic IPSPs have α-motoneuron of antagonist
type II afferents have multisynaptic EPSPs
multisynaptic EPSPs have homonymous and synergist muscle α-motoneuron
are golgi tendon organ segmental alpha-motoneurons multi or mono synaptic? do they use EPSP or IPSP?
multisynaptic
EPSP to antagonist motoneuron to prevent damaging amounts of tension developing in the muscle
IPSP to homonymous and synergist motoneuron
flexor withdrawal and crossed extension reflexes
stepping on glass analogy
why are “upper” and “lower” motoneuron no longer neuroanatomical terms?
it implies direct connections between long tract cells and motoneurons in the spinal cord
however, they are frequently used clinically
alpha-motonuerons get input from
cerebral cortex, brain stem (vestibular nuclei, reticular formation, red nucleus, tectum), SC interneurons (including Central Pattern Generators)
what happens with a lesion to motoneurons?
weakness, flaccidity, atrophy, fibrillation potentials, fasciculation, decreased or absent reflexes
what happens with a lesion to descending pathways?
initially paralysis/paresis, flaccid muscles
develop spasticity/hypertonicity, hyperreflexia and possibly clonus, Babinski sign - upward big toe, synergistic movement -patterns of groups of muscles
what happens with a lesion to the posterior limb or genu of internal capsule?
lesion to lenticulostriate arteries (branch of MCA)
corticospinal - contralateral hemiplegia, spasticity - hyperreflexia, Babinski, increased resistance to passive movements
corticonuclear - facial motor nuclei
thalamocortical fibers - sensory loss, contralateral hemianesthesia
what happens with an M1 lesion?
paresis of voluntary movements, generally initially flaccid limbs
often regain movements of the proximal limbs but movements are not smooth and distal muscles may remain paralyzed
some return of stretch reflex (what causes spasticity from flaccidity), but not to extent as widespread stroke
review: what happens with a lesion to preMC an SMC?
decreased ability to coordinate bilateral movements
apraxia - difficulty appropriately using the limb during tasks despite ability to use limbs
review: what happens with a lesion to the PPAC?
tactile agnosias (like astereognosis)
deficits in association of tactile and visual image, initiation of contralateral movements, attention to contralateral world, visually and tacitly guided movements
most significant in non dominant side