Module 2: Cell Recognition and the Immune System
1/35
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
Pathogen definition
Disease-causing microorganisms
Antigen definition
Chemical markers found on the surface of all cells
Self vs non-self
Self antigens belong to oneself
Non-self are foreign
What do antigens help the immune system to detect (4 examples)
Pathogens
Cells from other organisms
Abnormal body cells
Toxins
Types of defence mechanisms and definition
Non-specific - same, immediate response for all organisms
Specific - slower, specific response to each pathogen
Non-specific mechanism examples (2)
Physical barriers
Phagocytosis
Specific mechanism examples (2)
Cell-mediated response
Humoral response
Phagocyte definition
A type of white blood cell involved in phagocytosis
Types of phagocytes (2) and their definitions
Neutrophils - engulf and digest pathogens (+ dead human cells/debris)
Macrophages - punch holes in bacteria/stick proteins onto surface of bacteria to make them more appealing
Phagocytosis definition
The cellular process of engulfing solid particles using the cell membrane
5 steps of phagocytosis
1. Phagocyte moves towards a pathogen along a chemical concentration gradient
2. Receptors on the phagocyte attach to antigens on the pathogen’s surface
3. Lysosome within the phagocyte migrate towards phagosome formed by engulfing a pathogen
4. Lysozymes are released by the lysosome, hydrolysing the pathogen
5. Hydrolysed products of the pathogen are either absorbed by the phagocyte or are egested/excreted by exocytosis
(6. Phagocytes may present antigens onto their cell surface to trigger an immune response)
T lymphocyte definition
A type of white blood cell involved in the cell-mediated immune response
Types of T lymphocyte (2) and their definition
T helper cells - stimulate cytotoxic T cell division, further phagocytosis, B cell division and develop into memory T cells for further division
Cytotoxic/killer T cells - seek out cells with foreign antigens/antigen-presenting cells and attach to them to release toxic substances to kill it
Which lymphocytes are used in cell-mediated immune response
T lymphocytes
5 stages of T lymphocyte response
1. Phagocytes take in invading pathogens
2. Phagocytes present antigens (from pathogens) on their cell-surface membrane (= antigen-presenting cells/APCs)
3. Receptors on a specific T helper cell fit onto the antigens
4. The T helper cell divides rapidly by mitosis and form clones of genetically identical cells
5. Cloned cells divide into memory cells, stimulate phagocytosis, stimulate B lymphocyte division or activate cytotoxic T cells
How do cytotoxic T cells work
The protein perforin makes holes in the cell-surface membrane so it becomes freely permeable and dies
Viruses are also prevented from multiplying and infecting other cells like this
steps in humoral response
1. B lymphocytes process and present antigens on their surface
2. T helper cells attach to processed antigens on the B cell
3. The B cell is activated so it divides rapidly by mitosis to give a clone of plasma cells
4. Cloned plasma cells produce and secrete antibodies complementary to the antigen on the pathogen’s surface, which destroys the pathogen
5. Some B cells develop into memory cells so that the secondary response is faster
What is this structure? Name all of the parts of it.
Structure: Antibody
A = antigen bonding sites
B = variable region
C = constant region
D = receptor binding site
E = heavy chain
F = light chain
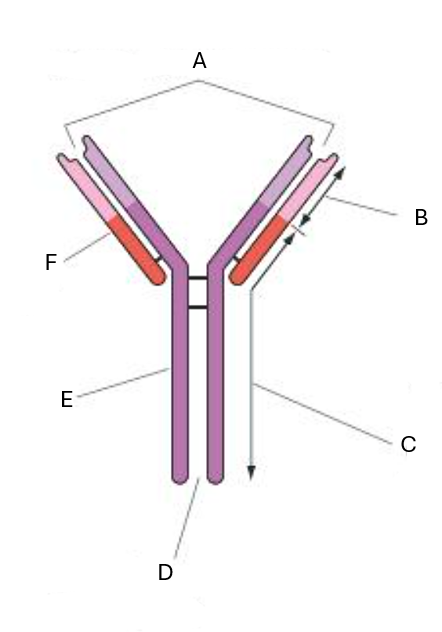
Antibodies are made of _ polypeptide chains that are connected by _____ ______
4
disulphide bridges
Describe the 4 regions of an antibody
heavy chain = longer
light chain = shorter
variable region = tertiary structure is complementary to antigen
constant region = same for all antibodies and is where a receptor can bind to
What are the 3 ways an antibody can work (brief description)
Agglutination - antibodies clump antigens together so phagocytes can engulf them at once
Neutralising toxins
Preventing viruses from entering host cells - bind to proteins on viruses that may usually bind to receptors on host cells
What is antigenic variability and what does this mean
Different strains (caused by mutations) have different antigens so memory cells won’t identify them, meaning that new antibodies must be made in a primary immune response
Name 2 viruses in which antigenic variability is common
HIV and influenza (flu)
What is HIV
Human immunodeficiency virus a type of retrovirus that infects humans by infecting T helper cells
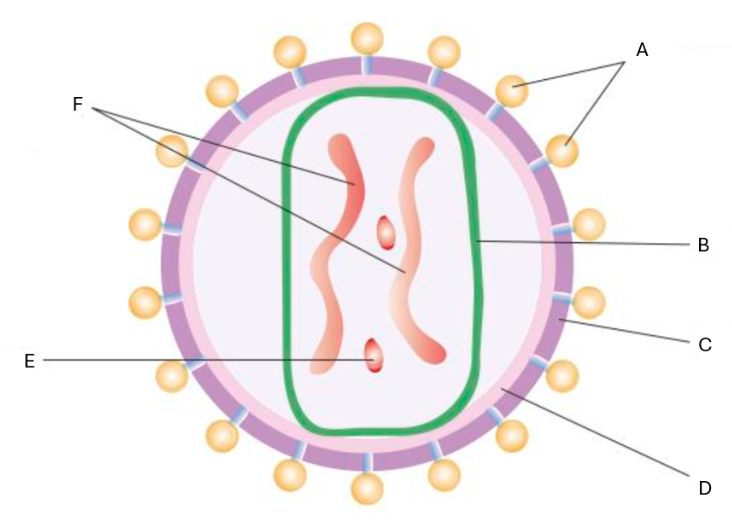
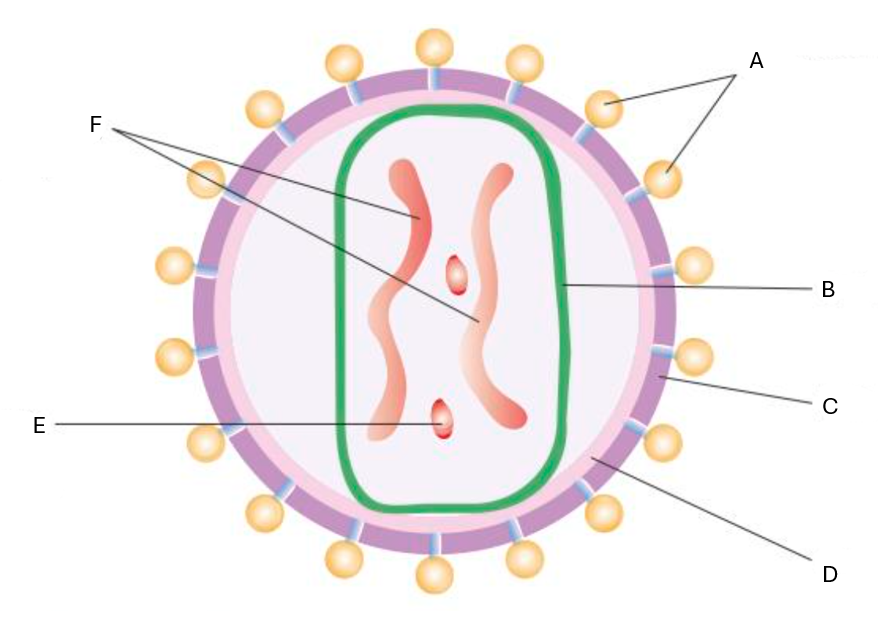
Label the diagram of the HIV virus
A = attachment protein
B = capsid
C = lipid envelope
D = matrix
E = reverse transcriptase
F = genetic material - RNA
Process of HIV replication
1. A protein on the HIV surface binds to a protein called CD4 (mostly attaches to T helper cells but other cells do have this protein)
2. The virus capsid fuses with the cell-surface membrane of a cell and allows RNA, reverse transcriptase and other HIV enzymes to enter the cell
3. Reverse transcriptase converts RNA into DNA
4. HIV DNA enters the nucleus of the cell and is inserted into the host cell DNA
5. HIV DNA makes mRNA that contains instructions on making viral proteins and RNA for new HIV molecules
6. HIV proteins and RNA are made at the ribosomes
7. HIV particles break away, taking some of the host cell’s cell-surface membrane
What does AIDS stand for
Acquired Immune Deficiency Syndrome
How is AIDS acquired
Low numbers of T helper cells mean that B cells and cytotoxic T cells can’t be stimulated in an immune response
Memory cells may also become infected
How does HIV spread
With an infected person, it can be caused by
unprotected sex, close contact or using their blood in a blood transfusion
Treatments for HIV
Antiretroviral drugs - slow down replication by blocking reverse transcriptase
PrEP - taking antiretroviral drugs
2 cases of chemotherapy killing WBCs and transplanting bone marrow from a person with a natural CD4 mutation
Monoclonal antibody definition
antibodies produced by a single clone of cells
Monoclonal antibody uses (3)
- Using cancer cell-specific monoclonal antibodies to attach to cancer cells and block release of chemical signals that stimulate uncontrollable cell growth
- Attaching radioactive or cytotoxic drugs to monoclonal antibodies
- medical diagnosis - pregnancy tests and detecting prostate-specific antigens (a protein) in blood of men who may have prostate cancer
ELISA test definition
Enzyme Linked ImmunoSorbent Assay tests test for the presence of an antigen/antibody and are very sensitive
Steps in ELISA test (direct + starting of indirect) for an antigen
1. Apply sample to surface
2. Wash the surface to remove excess antigens
3. Add antigen-specific antibody to the surface and leave to bind together
4. Wash surface to remove excess antibody
Rest of steps for ELISA test for an antigen
5. Add a second antibody that binds to the first antibody and has an enzyme attached to it
6. Wash the surface
7. Add a colourless substrate (of the enzyme)
The substrate will change colour when acted upon by the enzyme (greater intensity of colour = more antigen present)
Use of ELISA tests (3)
Detect HIV and other pathogens
Measure the quantity of an antigen
Test for drugs or allergies