10. Overview of Adaptive Immunity
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
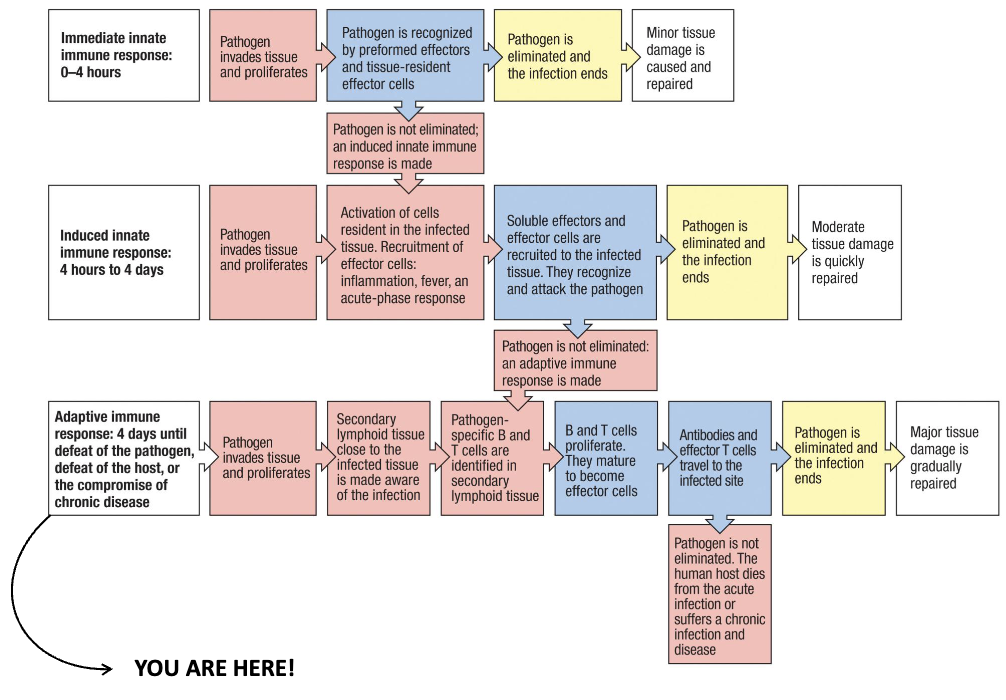
What are the main stages of the adaptive immune response?
Pathogen invades and proliferates in tissue
Nearby secondary lymphoid tissue detects infection
Pathogen-specific B and T cells are activated
B/T cells proliferate and mature into effector cells
Antibodies + effector T cells go to infection site
→ Outcomes:
Pathogen eliminated → tissue repairs
Pathogen persists → death or chronic infection
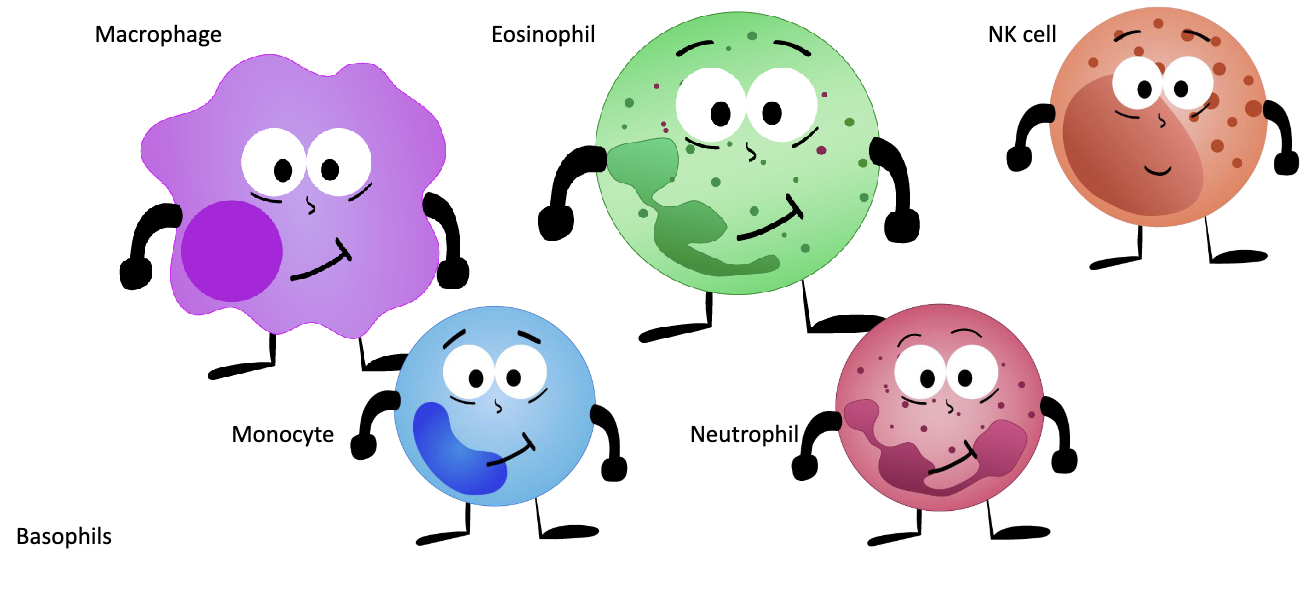
What are the main innate immune cells?
Macrophage
Monocyte
Neutrophil
Eosinophil
Basophil
NK cell
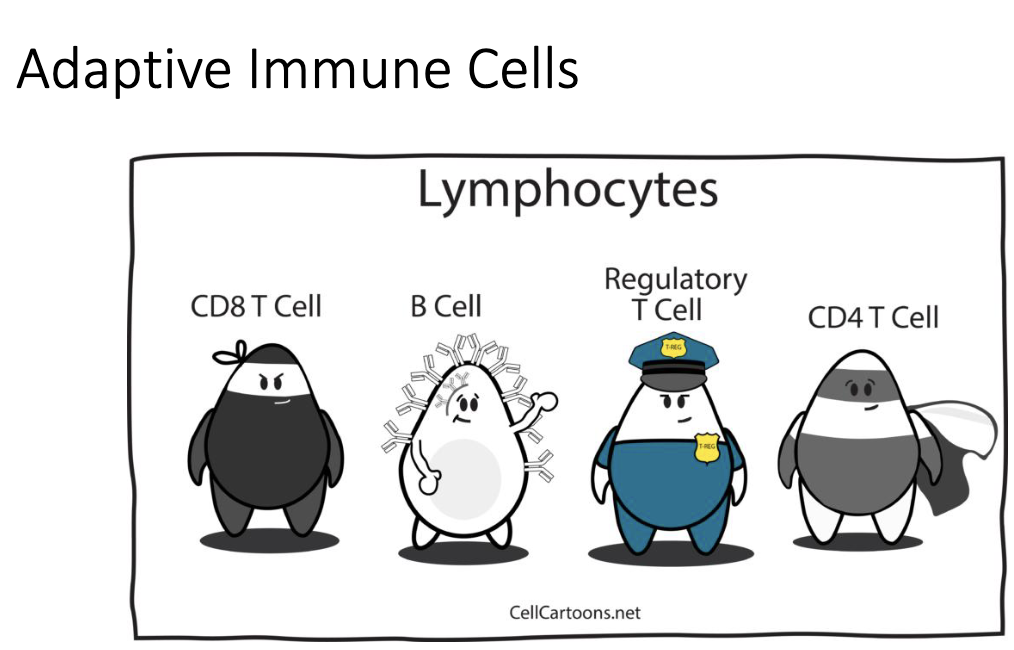
What are the main adaptive immune cells?
Lymphocytes:
CD4+ T cell (helper)
CD8+ T cell (cytotoxic)
B cell
Regulatory T cell
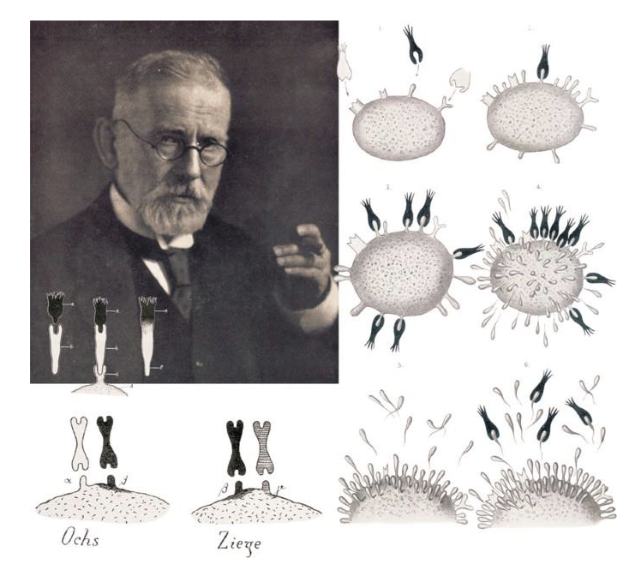
What makes adaptive immune cells adaptive?
They react and adapt to specific pathogens
Their functions are not innate — they are instructed during infection
(Linked to Paul Ehrlich’s idea of specificity and instruction = side-chain theory → antibodies)
What are the three key principles of immunity?
Immune recognition – Detect the invader
Immune protection – Mount a killing response
Immune regulation – Limit the response to prevent damage
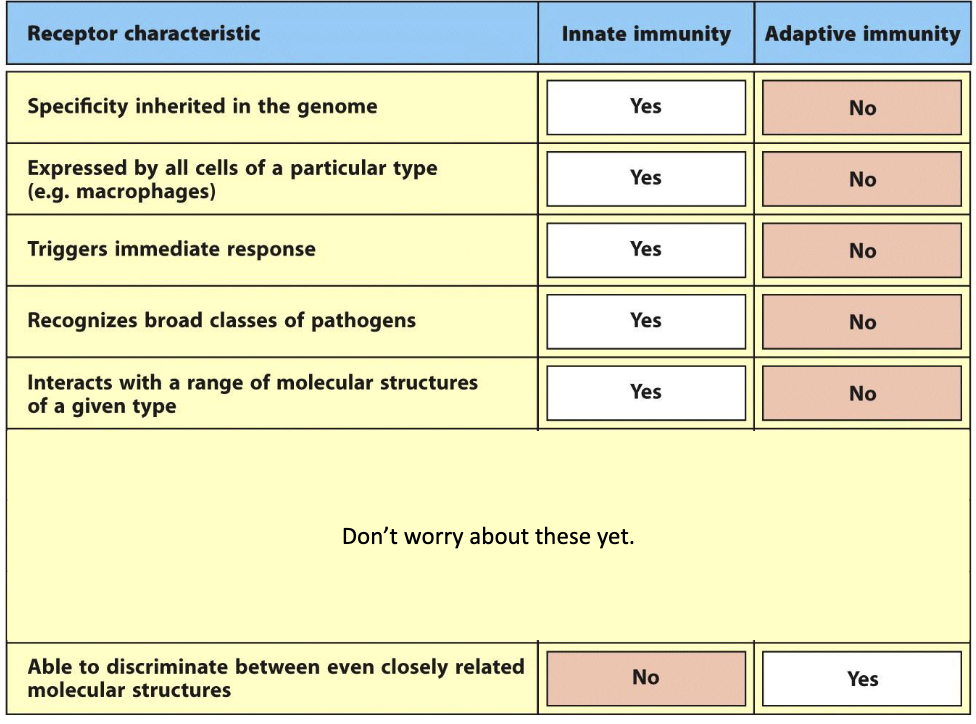
How does adaptive immune recognition differ from innate recognition?
Adaptive receptors:
❌ Not inherited in genome
❌ Not expressed by all cells
❌ No immediate response
✅ Highly specific — can distinguish closely related molecules
What are adaptive immune receptors specific to?
They are antigen-specific (“ANTIbody GENerating” substances)
Almost anything can be an antigen:
Proteins
Carbohydrates
Nucleic acids
Some small molecules
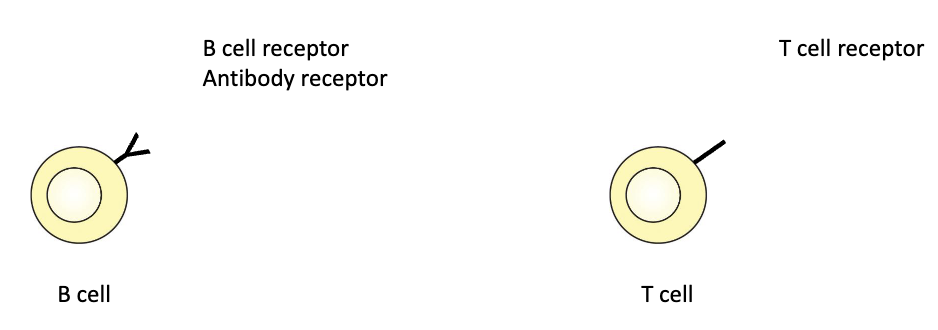
What receptors do B and T cells have?
B cells: B cell receptor (BCR) / antibody receptor
T cells: T cell receptor (TCR)
These receptors are ONLY found on B cells or T cells. Unlike TLRs which can be found on many immune cells.
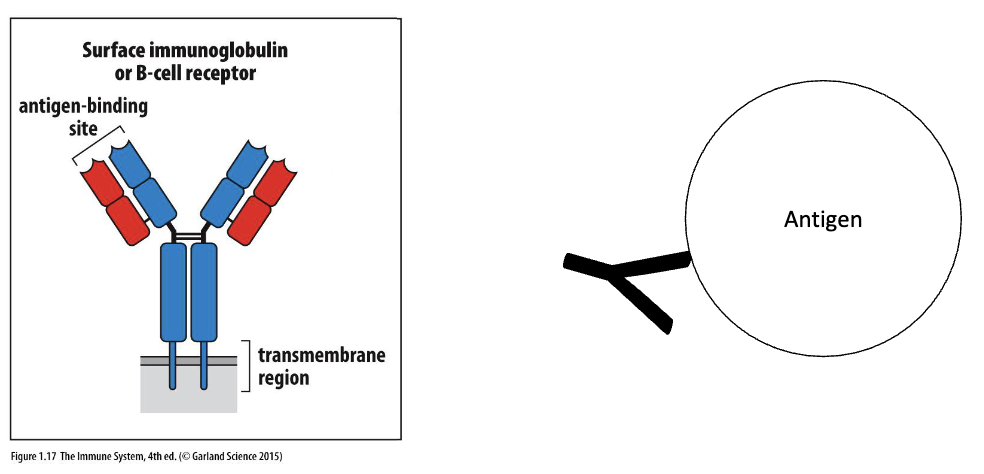
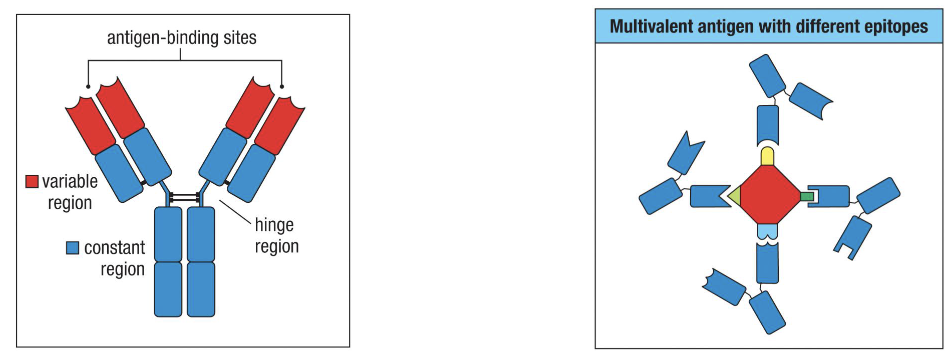
How do B cell receptors recognize antigens?
BCR = immunoglobin = antibody
BCRs bind whole, intact antigens
Bind to whole antigen’s in their natural conformation
No need to process antigen
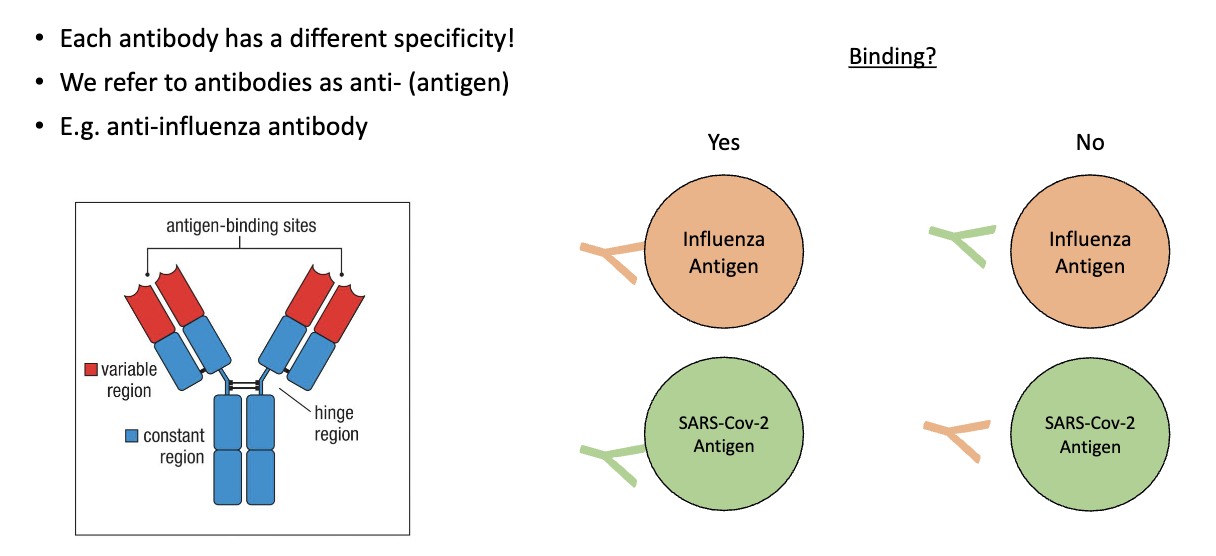
What determines antibody specificity?
Each antibody binds only one specific antigen
“Anti-X” = antibody against antigen X
e.g., anti-influenza antibody binds influenza antigen, not SARS-CoV-2
What is an epitope?
A small part of an antigen that a B cell, T cell, or antibody recognizes and binds to.
Example: A multivalent antigen can have several different epitopes (e.g., circle, triangle, square, butt), each recognized by a different antibody.
Tip of the antibody is called the paratope which binds to the epitope
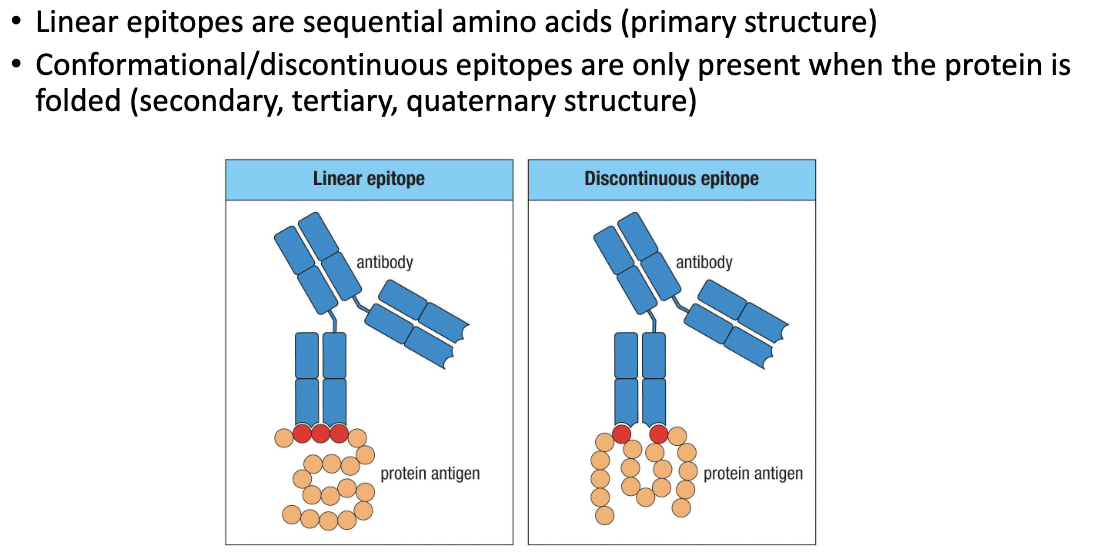
What are the two types of epitopes made during immune response?
Linear epitope: Sequence of amino acids (primary structure).
Antibody still binds even if the protein is denatured.
Conformational (discontinuous) epitope: Formed only when the protein is folded (secondary/tertiary/quaternary structure).
How do T cell receptors detect antigens?
TCRs do not bind whole antigens
They bind processed antigen fragments
Fragments are presented by antigen-presenting cells (APCs) using MHC molecules
Summarize how T cells recognize antigens.
Pathogen protein → broken down → peptide displayed by MHC molecule → recognized by T cell receptor (TCR)

Immune Protection: Compare innate and adaptive immune responses.
Killer T-cells → direct killing (similar to NK cells but antigen specific receptor)
Helper T-cells, B cells → indirect killing (secrete antibodies)

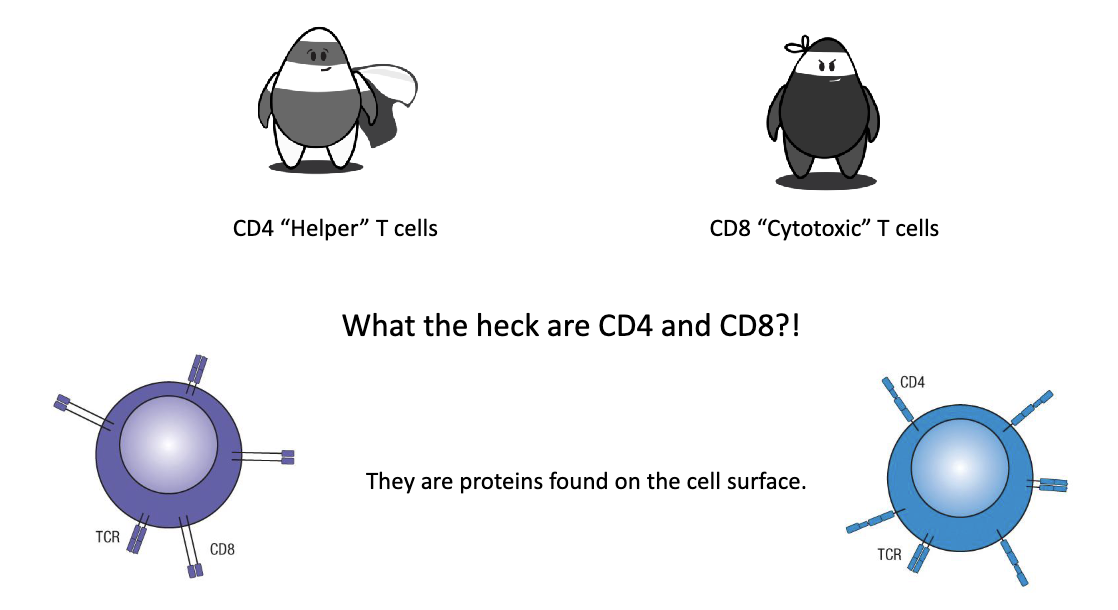
What are the two main T cell types and their roles?
CD4+ “Helper” T cells: Provide signals which help other immune cells perform functions
CD8+ “Cytotoxic” T cells: Directly kill infected or mutated cells (cancer cells)
CD4 and CD8 are proteins found on the cell surface.
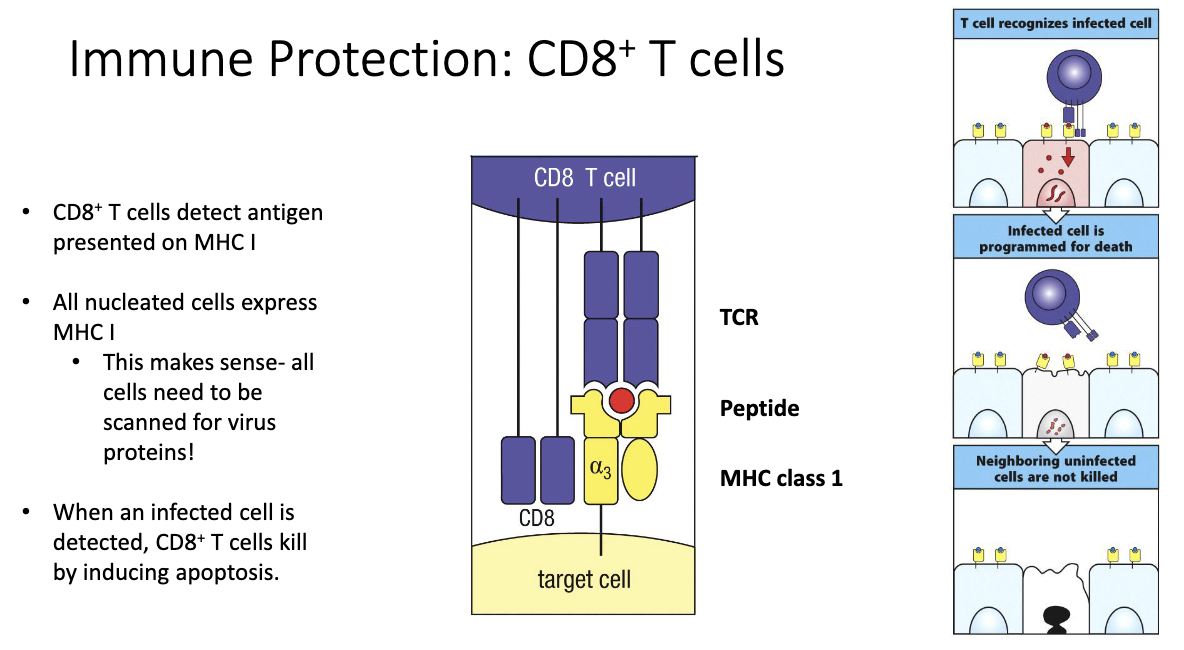
How do CD8+ T cells detect and kill infected cells?
CD8 = co-receptor for MHC class I.
MHC I is expressed on all nucleated cells → allows surveillance of proteins made inside the cell.
CD8+ T cells scan for foreign (viral or abnormal) peptides displayed on MHC I.
If MHC I is missing, NK cells will target and kill that cell instead.
When CD8+ T cell recognizes an infected cell:
TCR binds the antigen–MHC I complex.
The infected cell is programmed to undergo apoptosis (cell death).
Only infected cells are killed — neighboring healthy cells are spared.
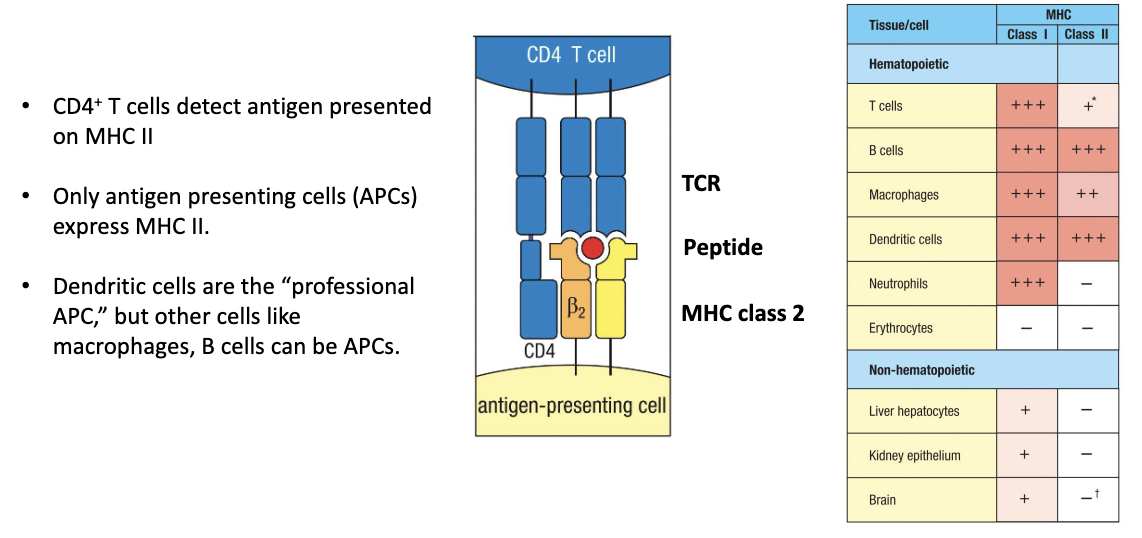
How do CD4+ T cells detect antigens and what cells express MHC II?
CD4 = co-receptor for MHC class II.
MHC II is expressed only on antigen-presenting cells (APCs):
Professional APC: dendritic cells
Others: macrophages, B cells
CD4+ T cells recognize antigens presented on MHC II.
Function: Enables helper T cells to “talk to” APCs and coordinate immune responses.
(Extra note: T cells can sometimes express MHC II to interact with other T cells — advanced, not covered here.)
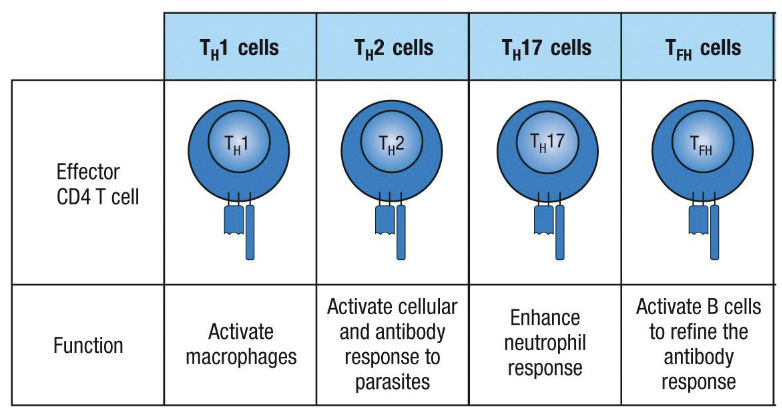
What are the main CD4+ T helper (Th) cell subtypes and their roles?
Th1: Activate macrophages → antiviral and antimicrobial
Type 1 response: IL-12 → Th1 → IgG
Th2: Activate responses to parasites (cellular + antibody)
Type 2 response: IL-4, IL-5 → IgE → mast cells, basophils, eosinophils
Can drive allergies if response misfires
Th17: Enhance neutrophil response → antibacterial
Type 3 response: IL-17 → neutrophils
Involved in autoimmune responses
Tfh (follicular helper T cells): Help B cells refine antibodies
Can specialize for antiviral or antiparasitic responses
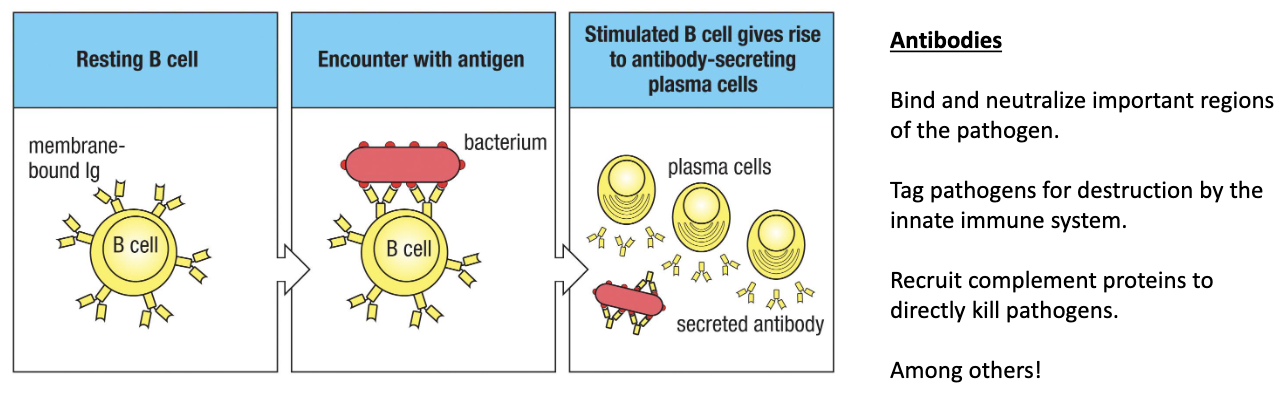
What do B cells do after activation?
Resting B cells: Have surface antibodies but don’t secrete them yet
Activation: Triggered by adaptive immune response
Differentiate into: Plasma cells
Plasma cell functions:
Secrete antibodies that:
Bind & neutralize key parts of pathogens
Tag pathogens for destruction by innate immune cells
Recruit complement proteins (classical pathway) to directly kill pathogen
Where are adaptive immune responses activated?
Origin: Adaptive immune cells come from bone marrow
Naïve B/T cells: Reside in secondary lymphoid tissues (lymph nodes, spleen)
Activation site: Secondary lymphoid tissues
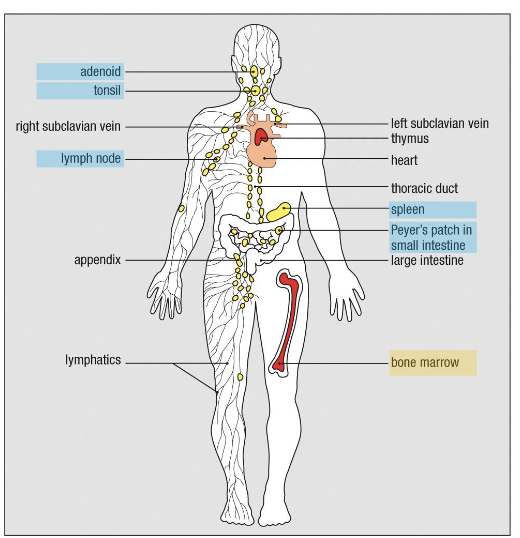
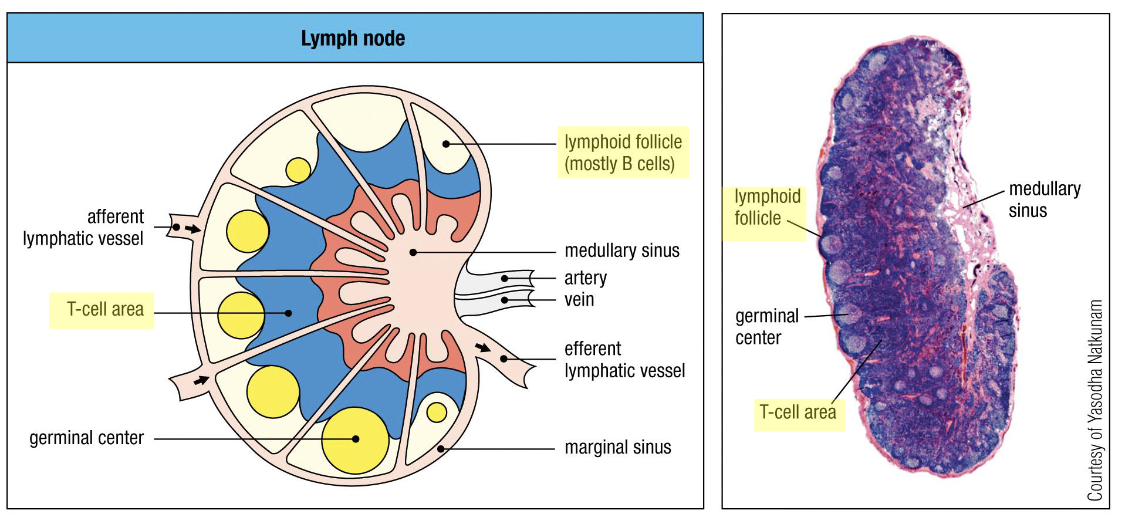
How does the immune system take advantage of space to activate itself?
Lymph node structure:
Follicles at edge: B cells
Inside wing: T cells
Medullary sinus: exit for immune cells/lymph
Process:
Lymph node collects fluid from tissues → brings antigens to lymphocytes
B cells capture antigen → present to T cells → determine activation → initiate adaptive response
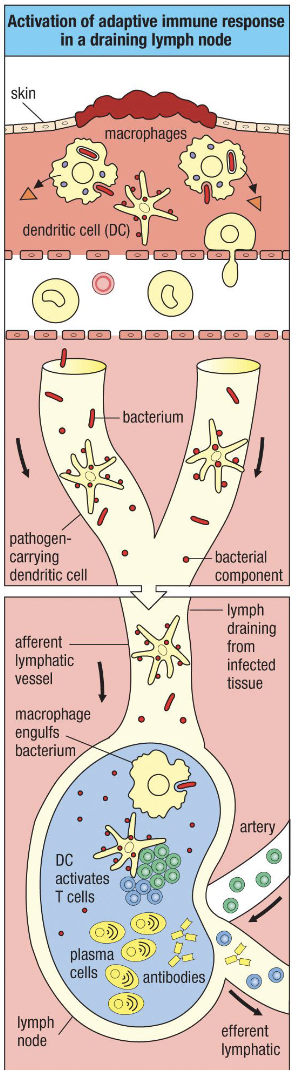
How does an adaptive immune response get activated in a tissue infection?
Battleground: Infection site → macrophages, dendritic cells, neutrophils respond
Dendritic cells:
Capture antigen/bacterial pieces → become activated
Enter lymphatics draining the tissue → travel to lymph node
Go to T cell area → find antigen-specific T cells → activate them
B cells:
Antigens filter through B cell follicles
Bind antigens in native conformation → present to T cells for help → get activated
Activated lymphocytes:
Exit lymph node via lymphatics → enter circulation → protect whole body
Example: Infection in left ear → immunity extends to other sites (toe, etc.)
What cell type regulates the immune response?
Regulatory T cells (Tregs)
Function: suppress and limit immune responses to prevent tissue damage
