Pathology Midterm
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
What is the mechanism by which neutrophils kill bacteria?
activation —> increase ability of integrins to recruit cells to site of inflammation —> opsonization —> phagocytosis & eradication
once phagocytosed, bacteria combines with phagolysosome to destroy it using reactive oxygen & nitrogen intermediates
Bacterial sinus infection: when a bacterium is present in the mucosa, neutrophils can aggregate and ingest the bacterium. What helps the neutrophil kill the bacterium?
production of reactive oxygen and nitrogen molecules
what are the causes of chronic inflammation?
prolonged exposure to tissue injury, irritants, or potentially toxic agents - infection won’t go away; ill fitting dentures
immune mediated diseases (autoimmune)
allergic diseases (asthma)
persistent infections
which white cells secrete antibodies?
B cells
Mechanism of complement MAC
attack wall of bacteria and create holes in the wall
Chronic inflammatory condition examples
rheumatoid arthritis, atherosclerosis, crohn’s disease
What is a histologic characteristic of a granuloma?
multi nucleated giant cells
In an allergic reaction, the development of symptoms such as nasal congestion and wheezing is primarily the result of what circulating factor?
histamine
an acute inflammatory exudate is rich in what kind of white blood cell?
neutrophils
What is the definition of hyperemia?
dilated blood vessels (part of inflammatory response)
what are the 4 cardinal signs of acute local inflammation?
redness, swelling, heat, pain
why does inflammation get red?
bringing more blood to area
what kind of inflammation is produced by infection with tuberculosis?
granulomas
which cells produce histamine?
mast cells
what is purulent exudate and what does it contain?
pus; contains neutrophils & protein. large concentration of neutrophils usually due to bacteria that attract neutrophils. cloudy appearance due to the many cells
what is the difference between an exudate and a transudate?
exudate: high concentrations of protein and inflammatory cells; implies damage of inflammatory changes to the vascular endothelium.
transudate: low concentration of protein and inflammatory cells; implies that the endothelial barrier to the passage of plasma proteins is intact although endothelial cells may have retracted. may occur due to increased hydrostatic pressure or reduced oncotic pressure
what’s the difference between humoral and cellular immunity?
humoral: antibody mediated. soluble proteins that are part of immune system (antibodies - from adaptive immune system, fragments of complement system - from innate immune system, and cytokines).
cellular: may also be either innate or adaptive. T cell mediated.
what is hyperplasia?
increase in number of cells causing increase in volume/size of organ or tissue. only in cell populations capable of division (i.e. glandular tissue & smooth muscle cells)
what is hypertrophy?
increase in size of cells (increased synthesis of cellular components) causing increase in convolute/size of organ or tissue. can occur in fully mature non-dividing cells (usually caused by increased functional demand)
muscles getting bigger when working out
what is fibroplasia?
proliferation of fibroblast as they lie down fibrous tissue
what is metaplasia?
cells change phenotype - a reversible change. one adult cell type replaces another. induced by cytokines and growth factors in response to stress or persistent injury. tissue and circulating stem cells.
commonly columnar —> squamous
what is hydropic degeneration?
cellular swelling
what is liver cirrhosis?
healthy cells replaced by scar tissue (fibrosis)
what is angiogenesis?
formation of new blood vessels by mobilization of EPCs from the bone marrow or from pre-existing vessels. occurs in wound healing
what is atrophy?
reduction in size of cells (protein degradation exceeds synthesis) causes decrease in volume/size of organ or tissue.
increase autophagic vacuoles and residual bodies
what happens to heart muscle when it undergoes infarct?
coagulative necrosis
T/F: gangrenous necrosis is a type of coagulative necrosis
true
what are the 2 types of gangrenous necrosis?
dry gangrene (arterial obstruction; bacteria fail to survive, better prognosis) and wet gangrene (venous obstruction; numerous bacteria, poor prognosis due to toximeia)
as an enlarged lymph node regresses, what process accounts for the lymphocyte cell loss?
follicular hypoplasia —> apoptosis
a middle aged woman with a smoking habit presents with a chronic cough. the columnar upper respiratory epithelium is replaced with squamous epithelium. what is this phenomenon called?
metaplasia
A 4 year old male patient presents with a history of recent weight loss, abdominal distention, and skin changes. on physical exam, patient has markedly distended abdomen with thinning of subcutaneous fat and a yellow discoloration of the skin. patient has generalized edema and skin desquamation with areas of hyperpigmentation and hypopigmentation. what is most likely diagnosis?
kwashiokor (protein deprivation)
which vitamin deficiency can manifest as gingival swelling?
vitamin C
anti epileptic drugs can cause gingival hyperplasia
electrolyte imbalance associated with bulimia
loss of potassium
can result in encephalopathy, confusion, cardiac arrhythmia
pathophysiology of autoimmune disease
loss of tolerance against self antigens
using same mechanism and machinery, the immune system attacks our cells and tissues
results from multiple factors: susceptibility genes that may interfere with self tolerance or environmental triggers ( infections, tissue injury, inflammation)
underlying cause of numerous human diseases
estimated to affect 2-5% of population and tend to be more common among women
What are the different types of autoimmune disease?
lupus: multisystem disease w/ autoantibodies directed against a number of nuclear antigens as well as antigens of blood elements and phospholipid protein complexes; acute onset followed by chronic phase. failure of mechanisms that maintain self tolerance
type I diabetes: autoantigen ( pancreatic beta-cell antigen); T cell mediated destruction; consequence - beta-cell destruction; associated with higher rate of recurrent aphthous stomatitis (canker sore)
rheumatoid arthritis: inflammation of multiple joins, joint deformity, pain (arthralgia), dysfunction. T cell mediated inflammation and destruction.
MS: strong effect of MHC. autoantigen - myelin basic protein, proteolipid protein. consequence - demyelination, brain degeneration, paralysis. demyelinated axons are vulnerable to atrophy
graves disease: single organ system affected ( thyroid gland)
56 year old female patient presents with one year history of dry eyes and dry mouth. reports difficulty producing tears and saliva, and her eyes and tongue often feel uncomfortably dry and scratchy. also noticed increase in joint pain and fatigue. salivary glands are tender and swollen. what is the most likely diagnosis?
Sjorgens syndrome
what is treatment of choice for end stage kidney disease?
kidney transplant
what is the most common cause of end stage kidney disease?
diabetes
what effect can NSAIDs have on the kidney?
causes drug induced interstitial nephritis in which afferent arteries are constricted which causes reduced GFR
nephrotoxic effect:
tubulointerstitial nephritis
minimal change disease
prerenal acute kidney injury
membranous nephropathy
what are the functions of the kidney?
maintain body homeostasis
filters blood/rids of waste, regulates acid base balance, secretes hormone (EPO), regulates plasma osmolarity
what are the laboratory parameters that define nephrotic syndrome?
proteinuria (> or = 3.5g; mostly albumin)
hypoalbuminemia (serum albumin < 3g/dL)
generalized edema
hyperlipidemia and lipiduria
± hypercoagulability
what is creatinine level used for clinically?
GFR efficiency - reflects level of kidney function
what is the role of telomerase in tumorigenesis?
helps tumors achieve immortality
replicative immortality through activation of telomerase - maintains telomere length by adding DNA sequences to ends of chromosomes
what’s the difference between an oncogene and a tumor suppressor gene?
oncogene: genes that when activated/overexpressed promote cancer (ex. cyclin D overexpression)
tumor suppressor gene: functional loss promotes cancer (ex. p53)
how often is a new mutation introduced every time a cell divides?
~3
What is cyclin D and what pathway turns on transcription of cyclin D?
a regulator of cell growth and proliferation
mitogen-activated protein kinase (MAPK) pathway turns on transcription of cyclin D
cyclin D fast facts
elevated cyclin d proteins bind and activate Cdk4/6 kinases (cyclin dependent kinases)
active cyclin d:cdk 4/6 complexes phosphorylates Rb protein, which sequesters E2F transcription factors
phosphorylated Rb releases E2Fs, which drive expression of genes necessary for S phase
cell is now committed to cell division
54 year old male has a non-healing ulcer on right buccal mucosa with severe pain. patient was edentulous and a denture wearer for 12 years. his denture was loose for several months. well defined ulcerproliferative lesion - primary cancer was diagnoses. statistically, what type of cancer is most likely ?
squamous cell carcinoma
what are the risk factors for the development of lung cancer?
smoking and radon
what is the presentation of horner’s syndrome?
invasion of neural structures around the trachea by a tumor located in the superior pulmonary sulcus (pancoast tumor) resulting in:
enophthalmos
ptosis
mitosis
anhidrosis
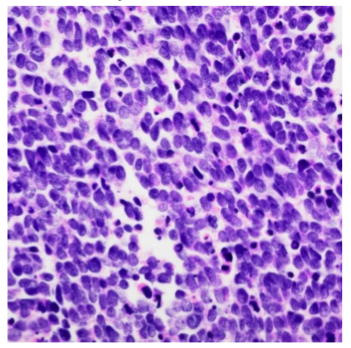
what histologic pattern is this
small cell carcinoma
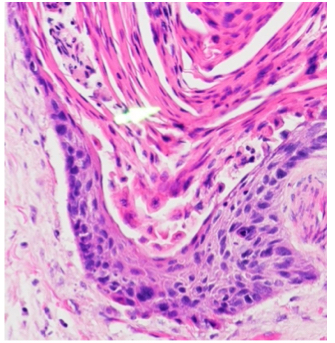
what histologic pattern is this?
squamous cell carcinoma
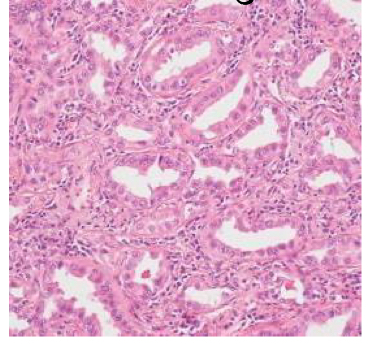
what histologic pattern is this?
adenocarcinoma (forming glands)
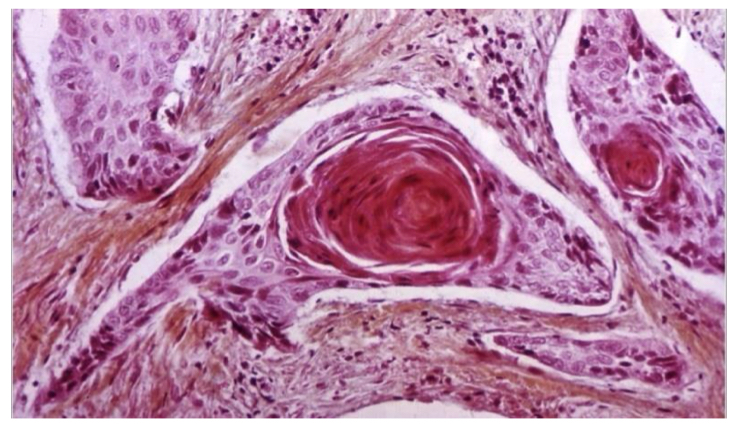
what kind of lung tumor is this?
squamous cell
what is the typical appearance of a melanoma on the skin?
irregular border and pigmented
what is the typical appearance and cause of cutaneous warts?
multiple papules with rough surfaces (papillomatous epidermal hyperplasia)
caused by HPV (viral cause)
What kind of pathogen causes CJD (creutzfeldt-jakob disease)?
prion protein
T/F: psoriasis is not an autoimmune disease
false - it is
what is the typical clinical appearance of basal cell carcinoma?
pearly telangectatic nodule
nests of basaltic cells within dermis
blood vessels running through nodule
what is the of gene variant that predisposes individuals to late-onset Alzheimer disease?
ApoE
variant E4 increases risk for AD
what is the clinical presentation of parkinson’s disease?
hypokinesia/bradykinesia (slow movements)
resting tremor
postural instability
rigidity
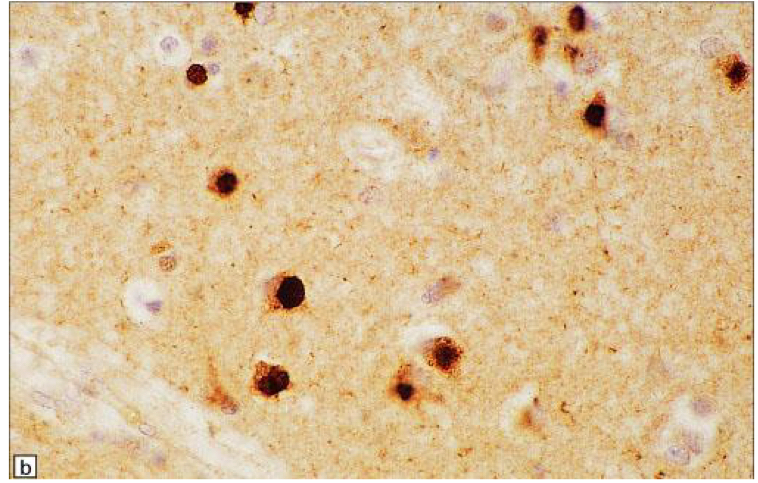
What is this image?
Tau protein immunohistochemical staining of tissue from a patient with pick bodies associated with frontotemporal lobar degeneration (FTLD)
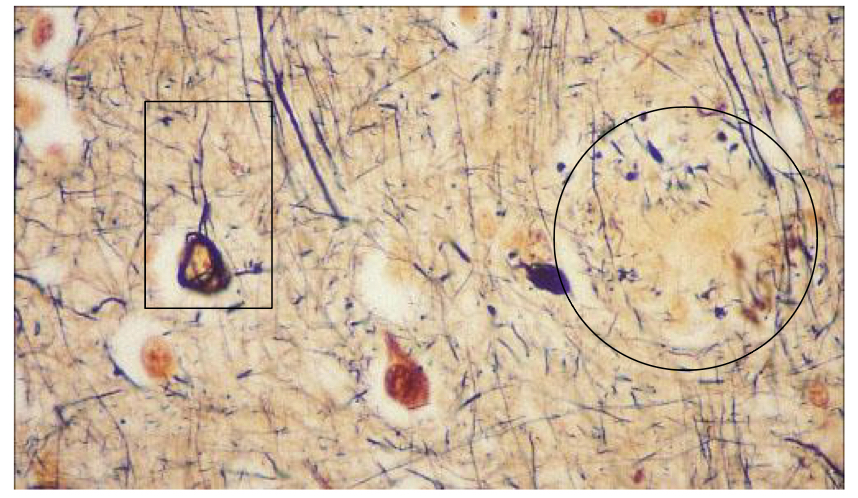
In this silver stain of tissue from a patient with alzheimer disease, what is circled?
senile plaques
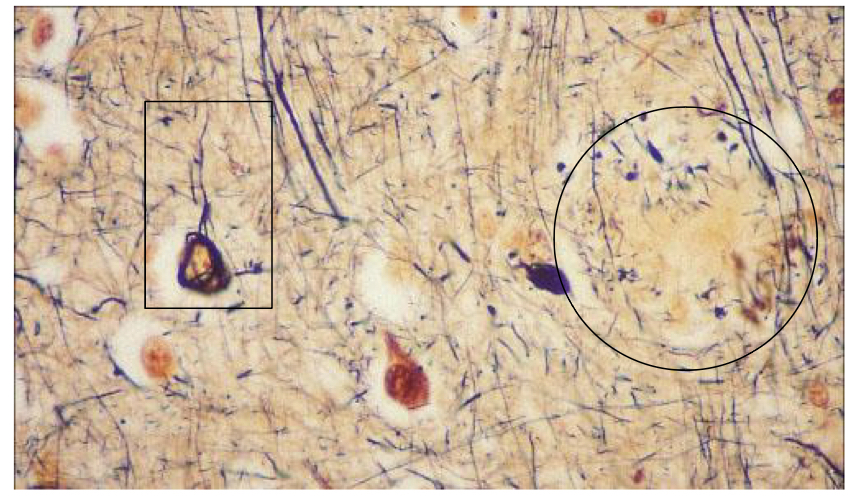
In this silver stain of tissue from a patient with alzheimer disease, what has a rectangle around it
tau positive tangle
65 year old woman is brought to clinic for difficulties with memory, resting tremor, shuffling gait, and visual hallucinations. at night she thrashes violently as she dreams. her symptoms fluctuate during the day. What disease is this and what protein aggregates in this disease?
dementia with lewy bodies
alpha synuclein aggregates