Rational Antimicrobial Therapy - PK/PD and Dosage Regimen Design
1/27
Earn XP
Description and Tags
Flashcards covering fundamental PK concepts, loading dose, half-life, dosing regimens, formulation effects, and duration of antimicrobial therapy based on the notes.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
28 Terms
What is the fundamental tenet of clinical pharmacokinetics?
There is a relationship between pharmacological effects and an accessible plasma concentration of the drug.
Name the key pharmacokinetic parameters that govern drug disposition.
Volume of distribution (Vd), Clearance (CL), and Elimination half-life (t½).
What order process describes the typical movement of drug molecules?
First-order (movement is a constant proportion, not a constant amount).
How is clearance defined and expressed?
Total systemic clearance; elimination of drug from all organs; expressed as the amount removed from plasma per unit time (e.g., mL/min/kg).
What is the clinical use of clearance in dosing?
Used to calculate the dosing rate and maintenance dose to maintain the target concentration (TC).
What is the relationship between dosing rate, clearance, and target concentration?
Dosing rate = Clearance × Target Concentration (TC).
What is Volume of Distribution (Vd) and what does it represent?
A proportionality constant relating the amount of drug in the body to its concentration in blood; not a literal anatomical volume.
Which compartments are included in Vd for water-soluble drugs?
Plasma space (~7% of total body water) and interstitial fluid (~20% TBW); intracellular fluids are usually not included (~30-40% TBW).
Which drugs tend to have high Vd values?
Lipid-soluble drugs and drugs that bind extensively to tissue sites outside the plasma.
What is the loading dose equation?
Loading Dose = Vd × Target Concentration (TC).
What is elimination half-life (t½) and what determines it?
The time required to reduce the amount of drug in the body by half; depends on Vd and CL
t½ = 0.693 × Vd / CL. → half life is directly proportional to the distribution and inversely related to the clearance
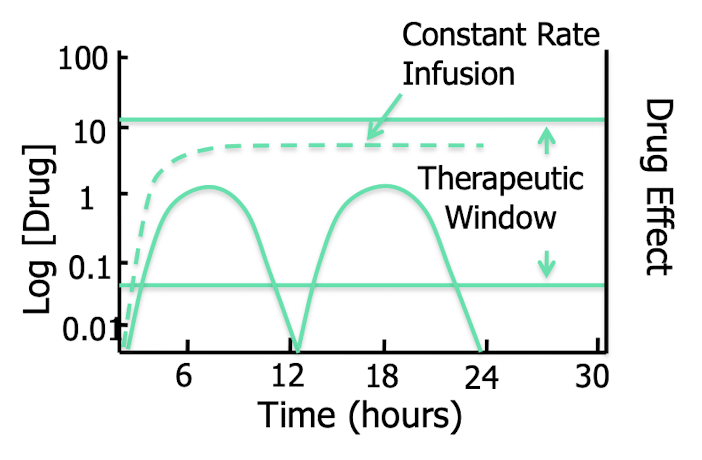
How long does it typically take to reach steady-state with continuous dosing?
Approximately 3–5 half-lives → drug input = drug elimination
What is a key use of t½ in dosing planning?
Guides dosing interval and prediction of drug accumulation.
What are the pharmacodynamic targets for concentration-dependent antibacterials?
Cmax/MIC 8–10×; AUC0–24/MIC 125–250×; presence of a post-antibiotic effect (PAE).
Name examples of concentration-dependent antibacterials.
Aminoglycosides, fluoroquinolones, and metronidazole.
For time-dependent antibacterials, what percentage of the dosing interval above MIC is needed for efficacy and for minimizing resistance?
Efficacy: >50% of the dosing interval above MIC; to minimize resistance: 80–100% of the dosing interval above MIC (as with beta-lactams).
What is Cmax/MIC and AUIC/MIC used for?
Pharmacodynamic indices used to design dosing regimens; Cmax/MIC for concentration-dependent drugs; AUIC (AUC/MIC) for overall exposure.
If MIC = 3 µg/mL and Cmax = 17 µg/mL, what is the Cmax/MIC ratio?
Approximately 5.7 (17 ÷ 3).
Why are drugs formulated in different dosage forms?
To improve ease of administration/compliance, allow controlled rate delivery, and accommodate husbandry constraints.
How does dosage form influence absorption and pharmacokinetics?
The formulation affects the rate and extent of absorption, influencing onset, duration, and intensity of action.
What factors influence the choice of formulation regarding route of administration?
Availability of formulations for the drug; owner compliance; cautions with compounded products; work with a reputable pharmacist.
What is bioequivalence in generic vs proprietary drugs?
Generic drugs are bioequivalent to proprietary products; similar PK/PD profiles.
What is the status of veterinary transdermals?
Few veterinary-approved transdermal products exist; compounded transdermals are not recommended without supportive PK data.
How should duration of therapy be determined for infections?
Depends on location and chronicity; longer for chronic/inaccessible infections; treat until healing with restoration of local immunity.
What are typical durations for acute infections?
7–10 days overall; uncomplicated UTI 3–5 days; neutropenic or immunocompromised 10–14 days.
What duration is typical for chronic or serious infections?
4–6 weeks; 7–10 days past resolution of clinical signs; pyrexia until afebrile for 4–5 days.
Why is owner compliance important in duration and dosing?
Ensures therapeutic levels are maintained and reduces risk of treatment failure and resistance.
How are PK/PD targets related to MIC in dosing design?
Dosing regimens are designed to achieve PK/PD targets relative to MIC to maximize efficacy and minimize resistance.