SARREEE SARREE HCS MODELS
1/113
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
114 Terms
What are the 2 theories of early childhood development?
Piagets theory
Vygotsky’s theory of social development
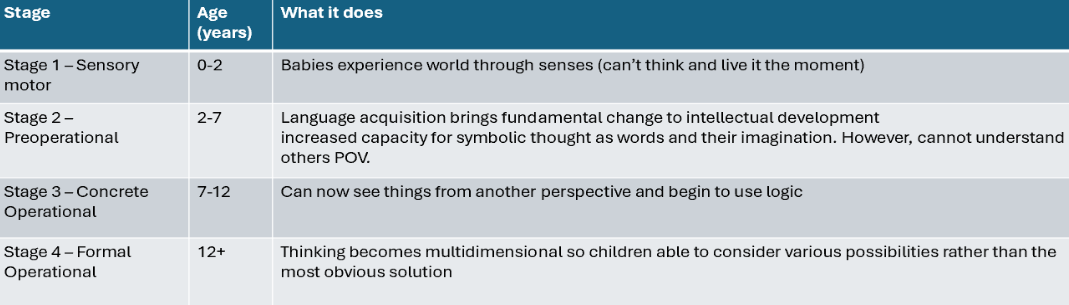
Outline piaget’s theory and how it works
Children’s brains aren’t mini adult brains and go through 4 developmental stages
Piaget theories suggest that Children aren’t passive learners—they’re active explorers. They interact with their environment and construct knowledge through experience. This learning process is centered around schemas, which are mental frameworks or “blueprints” for understanding the world. They build on information schemas by adapting what they know to accommodate new information.This is done via 2 mechanisms:
Accommodation (modify existing schema or create new schemas)
Assimilation (fit into existing schema)
🔄 Two Key Processes for Adapting Knowledge??? Kya hain bolo bolo samjhao
1. Assimilation
New experiences are interpreted using existing schemas.
It’s like fitting new info into old mental folders.
✅ Used when the new info is similar to what they already know.
Example:
A child sees a zebra for the first time and calls it a "horse" because they already have a schema for horses.
2. Accommodation
The child changes or creates a new schema when the info doesn’t fit.
This happens when they realize the new experience doesn’t match what they already believe.
Example:
The child learns that a zebra is different from a horse and creates a new schema for zebras.
Flaws with piaget’s theory
Actual development and learning are a lot smoother (not concrete stages)
Underestimation of child's capacity & overestimation of adults capacity
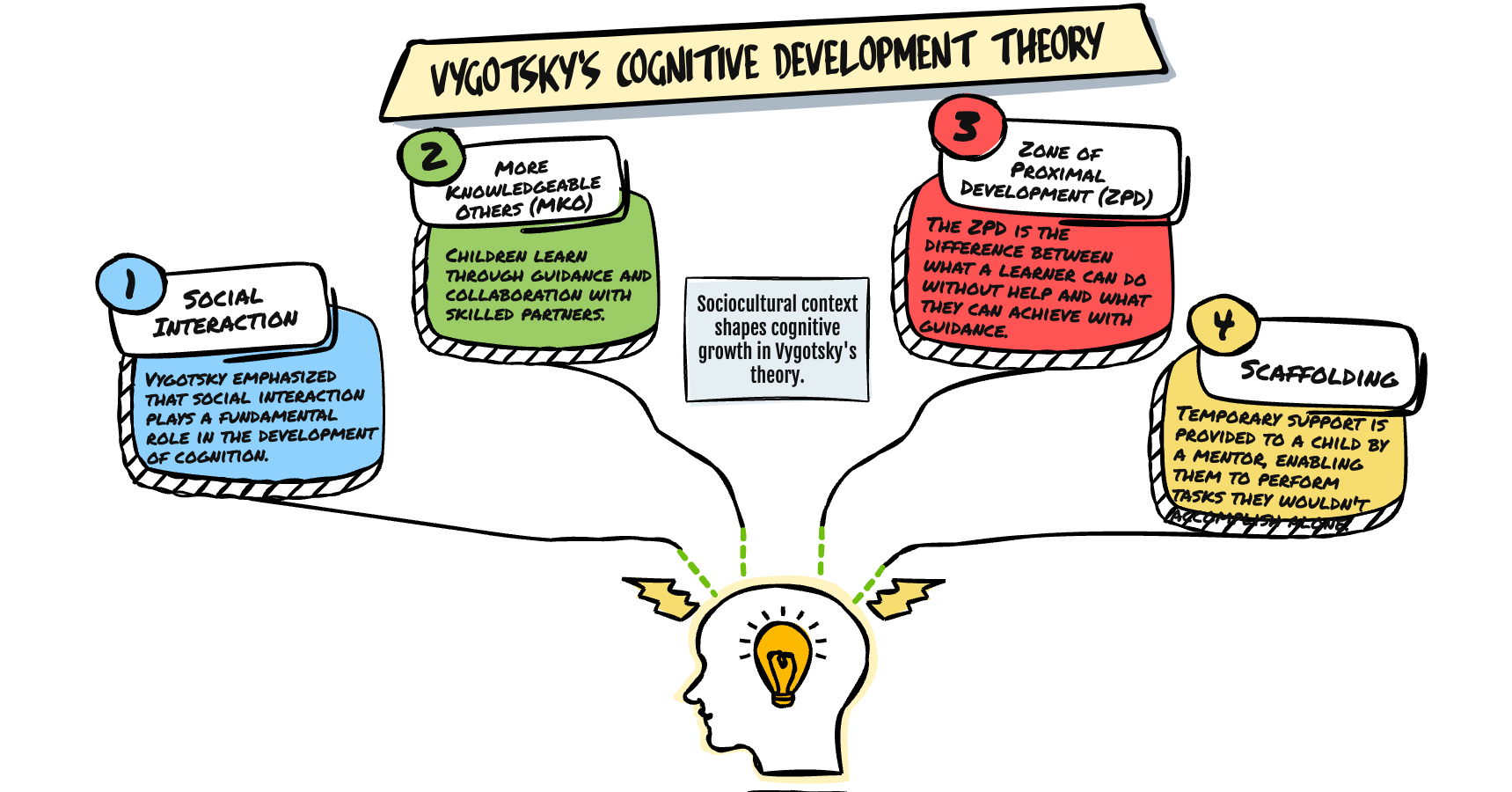
Outline Vygotsky’s theory of social development
•Full cognitive development requires social interaction.
•Culture teaches children how to think and what to think.
•Argued that language = crucial for collaborative problem solving
•collaborative problem solving = vital for children’s cognitive development
• Learning happens in the “zone of proximal development” = The gap between what a child can do without help and what they could do with appropriate guidance or collaboration
The zone of proximal development is why social interaction is important in this theory as help from adults or peers can help children complete tasks they can’t do by themselves.
What are the two theories of adolescent identity formation?
Eriksons Theory
Marcia’s theory
Explain Eriksons theory
•Central Conflict: Adolescents struggle to form a theory of self and become confused about their roles and values.
•Exploration and Commitment: Erikson highlighted the importance of adolescents exploring different roles, values, and beliefs, and making commitments to those that resonate with them.
•Successful Resolution: A strong sense of identity provides direction and purpose, while unresolved conflict leads to role confusion and a lack of self-understanding.
Explain Marcia’s theory
•Said that adolescent stage doesn't involve identity resolution or confusion
•Involves the degree to which one has explored and committed to an identity in a variety of life domains (religion, gender roles etc)
•Exploration - Time to explore and re-evaluate values and choices
•Commitment - Commitment to a particular role or value
•Adolescents classified into 4 statuses based on whether they have explored various alternatives and made firm commitments to a life domain
•Identity Diffusion – these adolescents have not yet thought about or resolved identity issues and future life decisions
•Identity Foreclosure – These adolescents are committed to an identity but didn’t experience or explore the identity
•Identity Moratorium – These adolescents have explored options but not yet committed
•Identity Achievement - These adolescents have explored options and found what suits
Outline Physical Changes in adolescence - Tanner’s stages
Rowe and Kahn’s model
Rowe and Kahn defined successful aging as ‘high physical, psychological, and social functioning in old age without major diseases’
Three main components:
Low probability of disease and disease related disability.
Refers to less disease and less risk of disease.
High cognitive and physical functional capacity.
Includes both physical and cognitive capacities and potential for activity.
Tell us what a person CAN do not what they DO do.
Active engagement with life.
Interpersonal relations – contacts and transactions with others and exchange of information.
Productive activity – an activity is productive if it creates societal value.
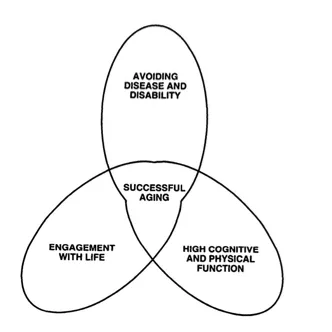
Biomedical model for successful aging
Optimising life expectancy and minimising physical and mental deterioration.
Importance of maintaining good health, no chronic conditions and maintaining independence.
Focus on how your body is able to adapt to aging.
Biopsychosocial Model for successful aging
Outcomes of one’s development over life and their ability to grow.
Importance of life satisfaction, personal growth and psychological resources.
Focus on what you get out of life – have you lived a good life?
Fair Innings Theory
older patients have already benefited from a longer life and so have less claim to scarce treatment resources than younger patients who have not yet lived their “fair innings.
Pros - Older people want to look ‘youthful’ – invest in botox, relief of symptoms of menopause, treatment for baldness etc.
Cons - Risk of infection upon hospitalisation, inappropriate use of tranquilisers, overprescribing
BREAKING BAD NEWS - SPIKES
S – Set up the consultation
Private, uninterrupted, sat down, warm, offer tissues at the side, and be attentive and ready to listen
P – Perception
Establish the patient’s perception and their understanding so far, ask how the patient is feeling, if they need to time to register the information.
I – Invitation
How much to they want to know? Invite them to ask questions
K – Knowledge and Information
Avoid using jargon, understand how much the patient knows and go off that, check the patient’s understanding
E – Emotion
Be empathetic, don’t downplay it and make sure to validate their emotions.
S – Summarise
Check understanding and make a plan
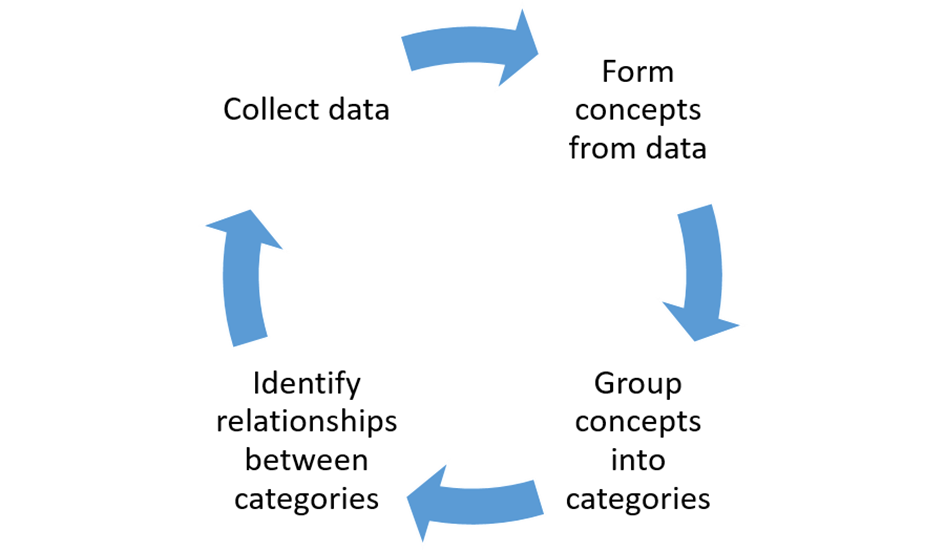
GROUNDED THEORY RESEARCH
Inductive research approach where you have a question or a bunch of qualitative data and you need to develop a hypothesis from it.
Formation of new theories using qualitative data.
Findings tightly connected to data.
Great for new theories.
Offers strategy for analysis.
Stops confirmation bias.
Difficulty collecting data.
Long process.
6 key hurdles for psychological adjustment to bad news
-managing uncertainty
-looking for meaning
-dealing w/ loss of control
-having a need for openness
-needs for emotional support
-needs for medical support
Substantive Theory of Caregiving
Purpose of caregiving varies over time
Gives insight into when and how family caregivers accept, reject or seek assistance with their caregiving efforts.
Purpose of caregiving related to decisions about maintaining, sharing, relinquishing care and accepting/rejecting help
Focuses on:
WHO is going to provide care (formal vs informal caregivers)
WHERE the care is going to be provided (home, day centre, nursing home)
HOW the care is going to be provided (exclusive to family or shared/delegated roles)
Outlined that caregivers went through two phases: interrelational and pragmatic – not necessarily in a linear format.
Interrelational phase happened early on and focused a lot more on what the care recipient needs and wants.
Pragmatic occurs later on and focuses on the effects on the caregiver and how to provide the best quality of care for the care recipient.
Potential third stage: care giving recedes from being the centre of the care givers life – so they become detached form their role as a care giver.
During each phase, caregivers made decision based on the purpose of that phase
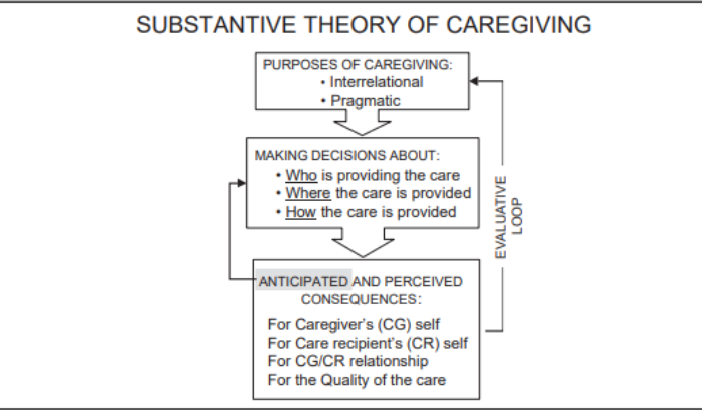
Interrelational Caregiving
Usually when the person being cared for experiences a cognitive loss.
Carers work to strengthen and support the recipient’s sense of self to way things ‘had always been’.
Ensure the recipient has a sense of worth and is able to reciprocate in the relationship – do something for the carer too.
Maintain past role – even if they are unable to complete some tasks.
Pragmatic Caregiving
Sharing the care more – so now the interrelational aspect is handled by HCP.
Now, the carer’s main focus is that the recipient is emotionally and physically comfortable.
Ensures high quality care, lessens the cost of care giving, and ensures the recipient is getting cared for properly (preventing pressure sores, eating well, emotionally happy).
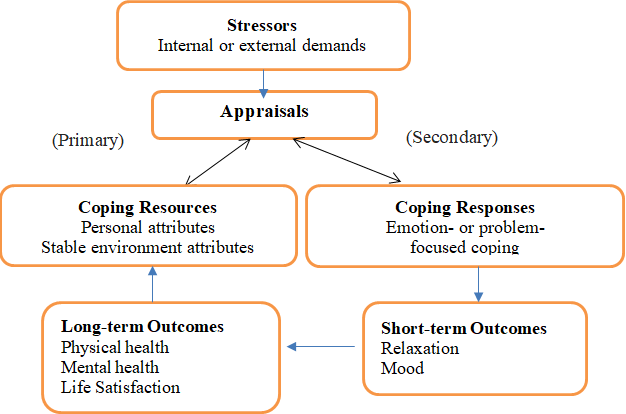
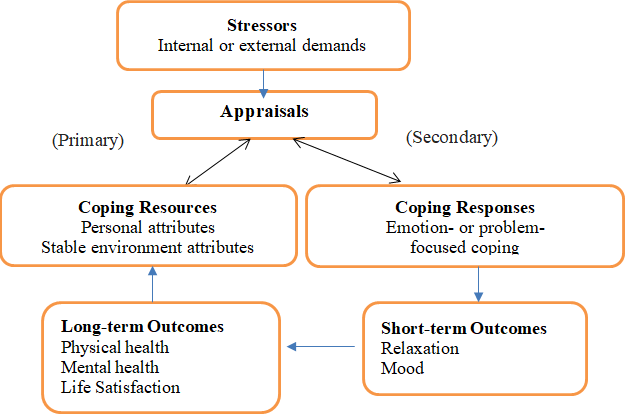
Transactional Model of Stress & Coping (Lazarus & Folkman)
Stress is a dynamic relationship between a person and their environment.
Become stressed when the demands outweigh the resources.
Primary Appraisal (is anything at risk? How bad is it?)*
Secondary Appraisal (Internal coping options and external coping)**
Coping (Problem Focused/Emotion Focused)
What is the biomedical model of pain?
Treating the pain as a pathology itself
What is the Biopsychosocial model of pain?
Origin of pain is complex and multifactorial.
Takes into consideration the psychological and social impact of pain.
What is Operant Conditioning in terms of pain?
Learning through consequences.
Through the concept of negative reinforcement – avoid what gives you pain in order to not feel the pain.
WHat is Psychophysiological Reactivity?
When you feel pain, your body has a physiological response to overcome it.
Tensing muscles in order to stop pain – can be debilitating if continued for too long
Treat with relaxation techniques
WHat is the Cognitive Theory of pain?
Making sense of pain in the surroundings
Pain demands attention and interrupts ongoing activity.
Attempts to prevent pain may result in anxiety = more pain.
As this is a vicious cycle – patients more likely to catastrophise their pain – make it out to be a disaster and so it leads to more pain, more hypervigilant of pain too. Think panic attacks.
Outline the Developmental Model for EMOTION REGULATION AND EATING BEHAVIOURS
Exposure: Exposure to different types of food as kids – lessen neophobia.
Social Learning: Observational learning – children see role models engaging with different food and they too will be likely to engage in eating different foods.
Association: Rewarding eating behaviours seem to increase food preference.
Outline the Weight Concern Model for EMOTION REGULATION AND EATING BEHAVIOURS
Associated with the meanings attached to food, weight, body dissatisfaction and dieting.
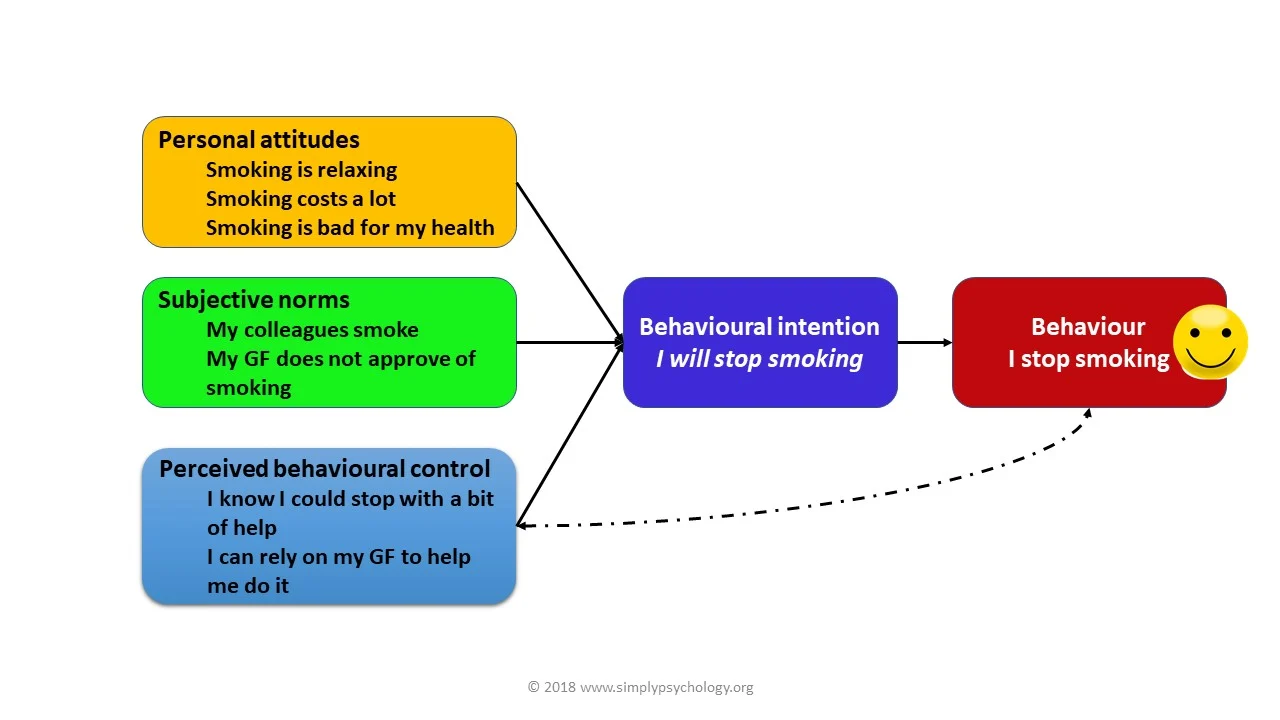
THEORY OF PLANNED BEHAVIOUR
1) Starts from the assumption that the strongest determiner of your behaviour is your intentions.
How you intend to behave will be how you actually behave
2) Intentions affected by three factors
Attitudes:
Influenced by beliefs about the outcomes of the behaviour
Evaluation of outcomes.
Subjective norm:
Influenced by perceived beliefs of others
How much the person wants to comply.
Perceived behavioural control:
Determines how easy or difficult it is for the person to complete the task
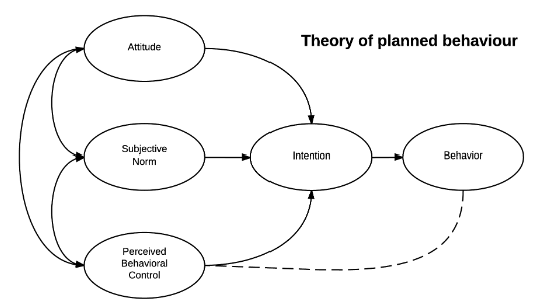
Some pros and cons of the Theory of planned behaviour
Pros:
Takes account the importance of social pressures + norms as well as how much control a person believes they have
Cons:
Focuses more on intentions than behaviours
Assumes you have the opportunities and resources to be successful in that behaviour
Fear, threat, mood and past experience.
HEALTH BELIEF MODEL
1) Perceived Threats:
Perceived threat for chronicity was high, cyclical nature was low and consequences were moderate.
Perceived personal control was high and were usually unaware of the severity of threat.
2) Perceived Benefits:
Compared to non-attenders, high attenders and low attenders still perceived a greater physiological and functional benefit from participating in programmes
Greater social benefits
3) Perceived Barriers:
Accessing health programmes
Travel barriers
4) Cues to Action:
Worry for health
Peer pressure
Family Is a strong cue for action
Emphasise benefits and modify barriers
TRANSTHEORETICAL MODEL OF CHANGE
Model of change that encourages people to change chronic detrimental lifestyles.
Longstanding and addictive behaviour.
Not a linear model of change – can enter and exit any part at any point.
Stage 1: Pre-contemplation
Patient not considering changing behaviour.
Stage II: Contemplation
Patient realises some changes need to be made.
Stage III: Preparation
Patient prepares to change.
Stage IV: Action
Makes change for the short-term.
Stage V: Maintenance
Change for the long-term.
Stage VI: Relapse
Relapse at any time and go through the cycle a few times.
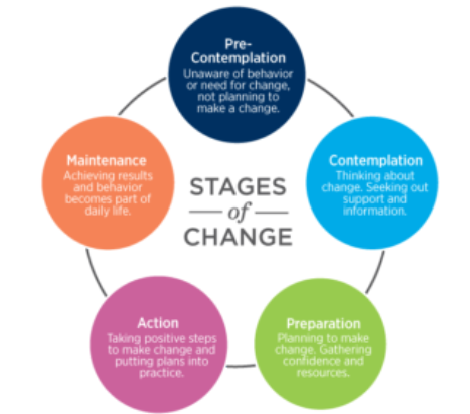
Advantages and disadvantages of the Transtheoretical model of behaviour change
Advantages of the Transtheoretical Model of Change
Recognises that changing behaviour is different for everyone and not a linear process – can move in and out of different stages at any time.
Recognises relapse as part of the process and does not blame person for it.
Disadvantages of the Transtheoretical Model of Change
Precontemplation and contemplation might just be the same.
Go through it many times – time consuming and might get tired of trying.
Requires a motivation.
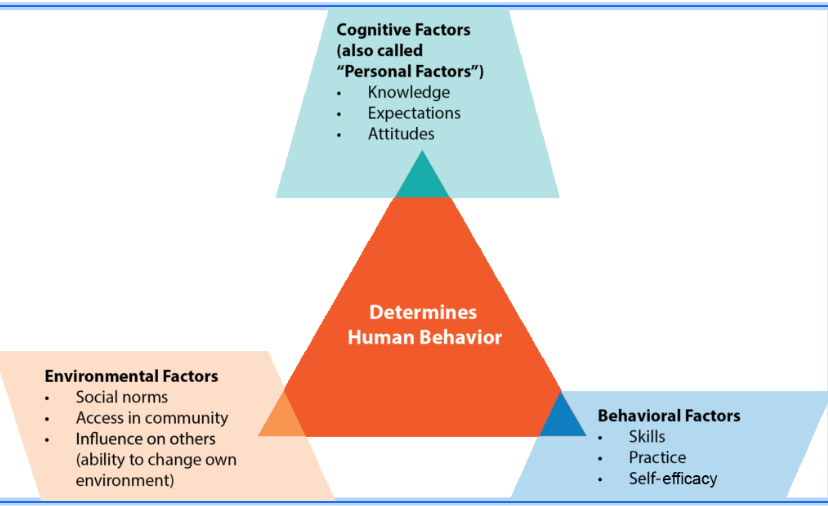
What is the SOCIAL COGNITIVE THEORY?
a framework for understanding how people learn by observing others and how personal, behavioral, and environmental factors interact to influence learning and behavior.
1. Cognitive (Personal) Factors
These include:
Knowledge – What a person knows.
Expectations – What outcomes they expect from their actions.
Attitudes – How they feel or think about certain behaviors or situations.
These internal processes influence how a person perceives and responds to their environment.
🔶 2. Environmental Factors
These are external influences such as:
Social norms – What’s considered acceptable behavior by society or peers.
Access in community – Availability of resources or opportunities (e.g., access to healthy food, education).
Influence on others – How a person can shape their environment or social surroundings (e.g., peer influence, role models).
🔷 3. Behavioral Factors
These are related to the individual’s actual actions or capabilities:
Skills – The ability to perform certain behaviors.
Practice – Experience gained through repetition.
Self-efficacy – Confidence in one’s ability to perform a behavior successfully.
🔁 The Core Idea:
All three factors interact and influence each other—this is called reciprocal determinism.
For example:
Your beliefs (cognitive) affect how you act (behavior).
Your behavior can change your environment (e.g., joining a group).
Your environment then feeds back and affects your beliefs and actions.
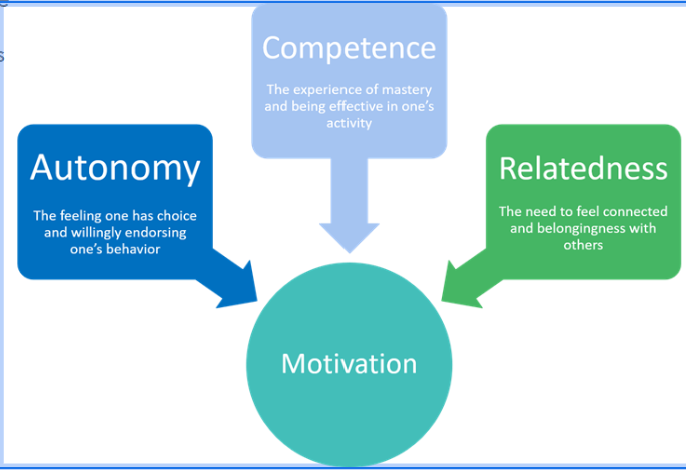
SELF-DETERMINATION THEORY
Suggests that people are motivated to grow and change by three innate and universal psychological needs.
People are able to become self-determined when needs for competence, connection/relatedness and autonomy fulfilled.
Competence:
Sufficient qualities to perform a given task or to describe the state of having sufficient intellect, judgement, skill and strength.
When you are competent, you are able to interact effectively within their environment – environmental mastery.
Relatedness:
Sense of belonging to a social group.
Autonomy:
Able to have choice and govern own behaviour.
Outline Selye’s GAS Model of Stress
Alarm: Activation of the SNS – short term stressor.
Resistance: Activation of HPA axis – long term stressor (chronic illness).
Exhaustion: Depletion of bodily resources (long term affects of cortisol).
There are two parts of the cycle of stressor-disease relationship
Influence of stress on disease
Disease disrupting the neural and endocrine circuits that mediate the stress response.
Neuropsychiatric symptoms come to light – depression, anxiety, insomnia.
Stress leads to disease and disease leads to stress
Explain Critical Theory
Critiquing and changing socitey as a whole. Focuses on how knowledge and organisation of power can lead to certain groups being subjugated or oppressed. It is concerned with equity and justice.
Explain Professionalism Theory
How occupational groups have exclusive ownership of specific areas of knowledge and expertise. Entry regulations and maintaining standards.
Explain Labelling Theory
Placing a label on someone and understand their deviant behaviours
Negotiated order Theory
Maintains social order with an organisation. Emphasises negotiation through bargaining and compromising which helps create rules and structures.
Name determinants of mental well being
- Under employment
- Food insecurity
- Poor access to healthcare
- Low education
- Poverty
- Poor neighbourhoods
- Social exclusion and inclusion
- Housing instability
- Adverse life experiences
What are the 3 factors that contribute to coping
Individual factors
Family Factors
Environmental Factors
Cognitive Behavioural model of depression
Cognitive Model of Health Anxiety
A previous experience forms a bad memory
You create a schema of that memory – a pocket of information.
Schema affects your view of yourself, the world and the future (Beck’s Cognitive Triad)
When faced with a critical ‘incident’ that coincides with your schema i.e. failed an exam = feeling worthless- this activates your automatic negative thoughts
Negative automatic thoughts lead to behavioural, emotional, cognitive and somatic symptoms.
The more negative you become, the more depressed you become.
Beck’s Cognitive Triad
Kubler-Ross 5 Stages of Grief (DABDA)
Denial
Anger
Bargaining
Depression
Acceptance
Pros and cons of DABDA Kubler-Ross 5 Stages of Grief
Pros:
Understanding AND coping with loss.
Cons:
Assumes set pattern – this is not like the real experience of grief.
Too linear, rigid and passive to be used to describe grief.
Usually used in life-limiting illness and NOT in bereavement.
Freudian Theory of Grief
Grief is a solitary process where mourners withdrew from the world so detachment from the deceased could be a gradual process.
Concept of ‘Grief Work’ where you detach from the deceased and focus on letting them go.
Freudian theory of Grief
Cons:
Only studied people who were depressed so his explanation can only be used with depressed people.
Not applicable to wider population.
Pros:
Confronting grief to allow detachment has remained a feature of subsequent theory and practice.
Lindemann’s 5 Stages of Grief
Somatic distress – Physical symptoms like tightness in the chest, shortness of breath, or loss of appetite.
Preoccupation with the image of the deceased – Constantly thinking about or seeing the lost person in your mind.
Guilt – Feelings of guilt or self-blame (e.g., "I should have done more").
Feelings of hostility and anger
Difficulty carrying out daily activities
Bowlby’s Theory of Attachment
Emphasises the importance of human attachments and bonds formed in early life.
Involves four overlapping, flexible phases:
Shock
Yearning and Protest
Despair
Recovery
Parkes Theory of Grieving
A process rather than a state. Each stage morphs into each other; a continuum.
Shock or numbness
Yearning and pining
Disorganisation and despair
Recovery
Understood that process of grieving is not linear
Recognised grief is not a state, but a process – you cannot be cured from grief, but rather the phases merge and replace one another.
Emphasises emotional and physical effects of anxiety.
Focuses on adults
What is worden AWAW model of grief
Setting tasks that need to be achieved in order to work through grief.
Passive phases replaced by active tasks of mourning.
Task One: Accept reality of loss
Task Two: Work through and experience the pain of grief
Task Three: Adjust to an environment without the deceased person.
Task Four: Withdraw emotionally from or relocate the deceased and move on – relocation focuses on having memories of deceased in a way that you can go about daily life.
Evaluation of Stage Models
Pros
Understand grief in an active way.
Helps understand WHY we grieve – attachment theory in particular.
Patterns and similarities in human behaviour.
Comfort knowing experience is shared by others.
COns:
Grief is a complicated process and there is not one way of feeling grief.
Grief is explained in a linear fashion.
Is there a wrong and right way to grieve?
Western culture – different cultures have different bereavement processes.
Explain the dual process model
The Dual Process Model of Coping with Bereavement, developed by Margaret Stroebe and Henk Schut (1999), describes how people adapt to the loss of a loved one by oscillating between two types of stressors:A bereaved individual as to cope with the experience of death as well as the lifestyle changes that result from it
1. Loss-Oriented Coping
This involves facing the grief directly and dealing with emotions related to the loss.
Activities:
Yearning, remembering, and crying
Talking about the deceased
Experiencing sadness, anger, or guilt
Visiting places or keeping items associated with the person
2. Restoration-Oriented Coping
This involves adjusting to life without the deceased, focusing on practical changes and new roles.
Activities:
Taking on new responsibilities (e.g., finances, childcare)
Forming new routines or identities
Reinvesting in life or forming new relationships
Distraction from grief
3. Oscillation (Key Concept)
The model emphasizes that healthy grieving involves moving back and forth (oscillating) between these two types of coping.
Constant focus on either can be overwhelming or unhealthy.
Oscillation allows for balance—some days are filled with emotional reflection; others are about getting on with life.
Evaluation of the Dual Process Model
Pros and cons
Pros:
Culturally sensitive and flexible – allows an individual experience of grief.
Understand you can move between loss orientated and restoration orientated.
Degree of emphasis on loss orientated or restoration orientated depends on individual.
COns:
Emphasis on coping and adjustment – if this takes long or you are unable to cope or adjust is it abnormal?
No focus on interpersonal relationships within grieving process – how do families interact?
WHat are the 2 ways people adapt to chronic illness?
Illness Related
Dealing with symptoms, disability, medical regimens
Good rship with staff
General
Coping with illness diagnosis
Maintaining a good self image
Keeping social relationships
Preparing for uncertain future
Key aspects of adjustment:
Chronic illness necessitates adjustment in multiple life domains
Involves positive and negative outcome dimensions
Dynamic process
Can be viewed only from within an individual context
Heterogeneity is the rule not the exception
Stress & Coping Model
Adjustment in the face of external stress is influenced by
The individual’s appraisals of stressors
The coping strategies they use for managing these stressors
Their appraisal of the efficacy of the coping strategies used
Processes of adjustment are measured separately from their outcomes
Transactional Model of Stress & Coping (Lazarus & Folkman)
Stress is a dynamic relationship between a person and their environment.
Become stressed when the demands outweigh the resources.
Primary Appraisal (is anything at risk? How bad is it?)*
Secondary Appraisal (Internal coping options and external coping)**
Coping (Problem Focused/Emotion Focused)
Engel’s Biopsychosocial Model
Giving the patient the sense they are being understood by examining the biopsychosocial dimensions of their illness
Livneh & Antonak
Variables associated with chronic illness and disability
Disability related (type/severity)
Sociodemographic factors (age/sex/ethnicity)
Personality (coping mechanisms/locus of control/meaning of condition)
Physical and social environment (social support/stigma)
What are zola’s 5 triggers? name them
These are events/factors which influence individuals to seek medical consultation. They are dependent on daily demands or interpretation of bodily symptoms. Zola’s 5 triggers are:
Interpersonal crisis
Perceived interference with physical or vocational activity
Perceived interference with personal or social relations
Sanctioning e.g. others pressure you to seek medical help
Temporalising (setting time limit before seeking help)
What are Mechanic & Volkart’s triggers? Name them
Describes a different set of factors which encourage patients to seek medical consultation. The triggers are:
Frequency of illness in the population
Familiarity of symptoms
Predictability of outcome
Amount of threat and loss likely to be suffered from illness
What is Lazarus transactional model of stress
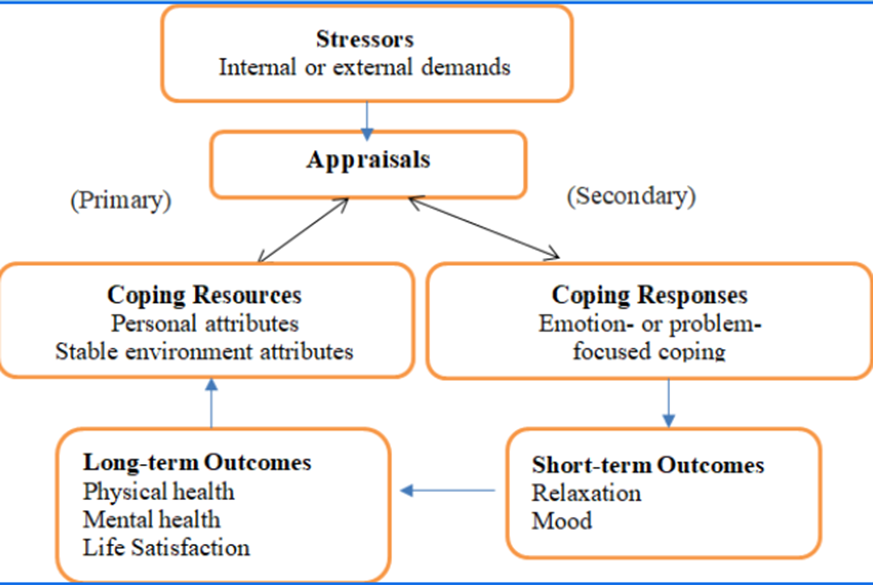
Primary Appraisal: “Is this a threat or challenge?”
Secondary Appraisal: “Do I have the tools/resources to deal with this?”
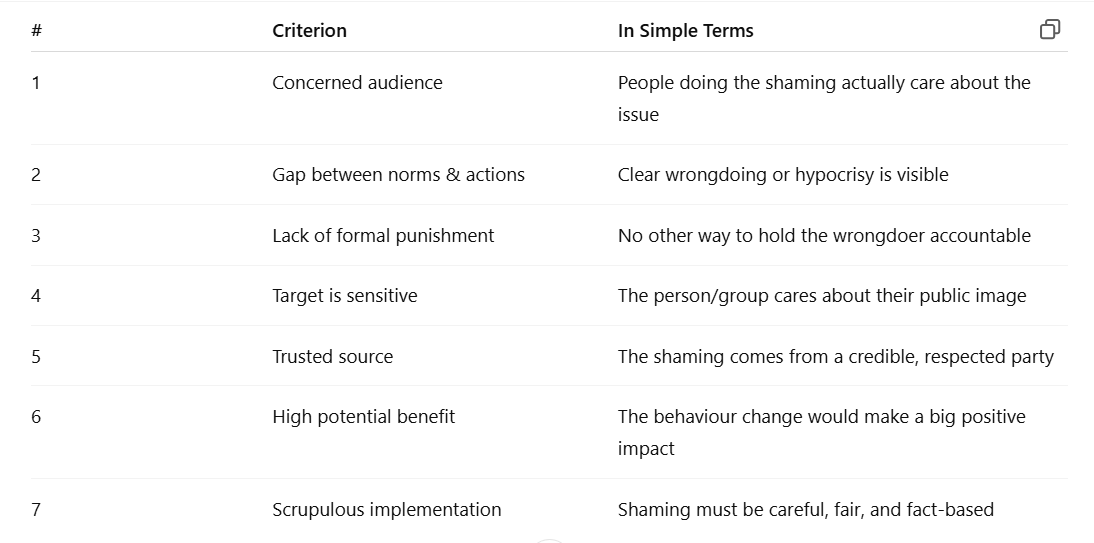
What are Jacquet’s 7 Criteria for Effective Stigmatisation?
The audience responsible for the shaming should be concerned with the transgression
There should be a big gap between the desired and actual behaviour
Formal punishment should be missing
The transgressor should be sensitive to the source of the shaming
The audience should trust the source of shaming
Shaming should be directed where possible benefits are greatest
Scrupulous implementation
Outline the Transtheoretical model of behaviour change PCPAMR
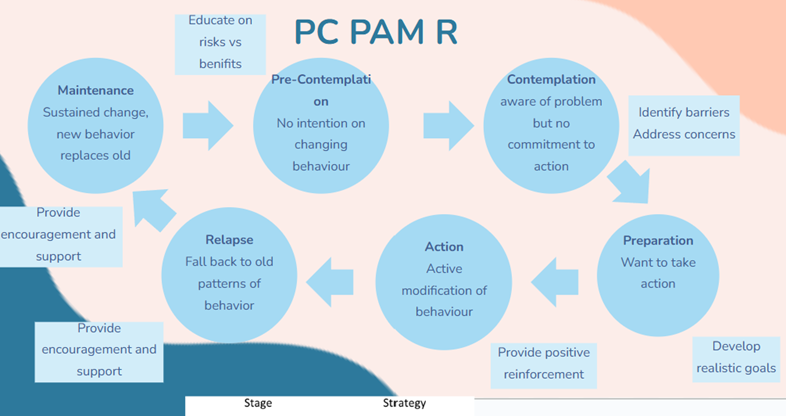
What are the pros of the transtheoretical model of behaviour change?
+ realistic as it acknowledges that change is not a linear process and that people go through stages in different ways and may relapse
+ recognises that relapse is a normal part of changing behaviour
It is important for HCPs to emphasise this and explore what a person has learned from a relapse and how this can be used to increase chances of success next time
+ useful in practice when dealing with smoking/alcohol/food/drug addictions etc, allows doctor to see if the patient is ready to change
What are the cons of the Transtheoretical model of behaviour change
could potentially become too much as a person may go through the cycle many times
- requires motivation from the patient
-not always a sequential process
-Ignores social context
- may be too late before a person enters the contemplation stage
What is the health belief model used for and what are the 5 factors part of it?
1) Perceived Susceptibility= belief of the chances of getting the illness
2) Perceived Severity= belief of the severity of the illness
3) Perceived Benefits= beliefs about what can be gained from taking action
4) Perceived Barriers= beliefs about the negative consequences of taking action
5) Self-Efficacy= confidene in their own ability to take action
What are the pros of the health belief model?
Includes common-sense constructs easy for non-psychologists to assimilate and apply
Has focused research attention on modifiable psychological prerequisites of behavior
Makes testable predictions
What are the Limitations of the health belief model?
Its common-sense framework simplifies health-related representational processes
Its theoretical components are broadly defined, and therefore different specific behaviors may not be strictly comparable
Lack of specification of a causal ordering
Neglects social factors
Name the big 5 personality traits (Psychological reasons why people respond differently to health) and what they mean
The Big Five personality traits, also known as OCEAN (Openness, Conscientiousness, Extraversion, Agreeableness, and Neuroticism), play a significant role in influencing how individuals respond to health-related situations.
Openness (O):
High Openness: Individuals with high openness are often more receptive to new information and experiences, including health-related information. They may be more likely to adopt alternative or unconventional health practices.
Low Openness: Those with lower openness might be more skeptical of new health approaches, preferring traditional or well-established methods.
Conscientiousness (C):
High Conscientiousness: Individuals high in conscientiousness tend to be organized, responsible, and disciplined. They are more likely to adhere to health regimens, follow medical advice, and engage in preventive health behaviors.
Low Conscientiousness: Those with lower conscientiousness may struggle with maintaining consistent health habits, missing appointments, or neglecting prescribed treatments.
Extraversion (E):
High Extraversion: Extraverted individuals may seek social support and engage in group activities that promote health and well-being. They might be more inclined to participate in group fitness classes or team sports.
Low Extraversion: Introverted individuals may prefer more solitary health activities or self-directed exercises. They may also be more reserved about discussing health concerns openly.
Agreeableness (A):
High Agreeableness: Agreeable individuals are generally cooperative and empathetic. They may be more likely to comply with medical advice and work collaboratively with healthcare professionals.
Low Agreeableness: Individuals with lower agreeableness may be more skeptical, independent-minded, and may question health recommendations. They might seek multiple opinions before committing to a health plan.
Neuroticism (N):
High Neuroticism: Neurotic individuals may be more prone to stress and anxiety, which can affect their health. They might engage in health behaviors as a way to alleviate anxiety or may be more vigilant about potential health threats.
Low Neuroticism: Those with lower neuroticism may be more resilient to stress and less likely to worry about health issues. However, they might also be less likely to seek help when needed.
Sociological reasons why people respond differently to health
Cultural influences: Cultural norms and values shape health behaviors. For example, some cultures may prioritize holistic approaches to health, while others may rely more on medical interventions.
Social support: The presence or absence of a strong social support system can significantly impact health behaviors. Individuals with supportive networks may be more motivated to adopt and maintain healthy habits.
Socioeconomic status: Access to healthcare resources, education, and economic factors can influence health behaviors. Lower socioeconomic status may limit access to healthcare and healthy lifestyle options.
What are the 2 Models of disability
social model of disability
medical model of disability
What is the social model of disability
The social model of disability views disability as a result of the interaction between individuals with impairments and societal barriers that hinder their full participation in society. This model emphasizes that disability is not an inherent attribute of the individual but rather a socially constructed phenomenon.
What is the medical model of disability?
The medical model of disability perceives disability primarily as a problem or deficiency within the individual that needs to be cured or managed through medical intervention.
Differences between the disability models
1. Conceptual Framework:
Medical Model: Disability is a problem of the individual, requiring medical treatment.
Social Model: Disability is a social issue, arising from environmental and attitudinal barriers.
2. Focus of Intervention:
Medical Model: Focuses on curing or managing the individual's impairment.
Social Model: Focuses on changing society to be more inclusive and removing barriers.
3. View of Disability:
Medical Model: Views disability as a negative condition that should be mitigated.
Social Model: Views disability as a natural part of human diversity and emphasizes acceptance and inclusion.
4. Role of Professionals:
Medical Model: Doctors and healthcare providers play a central role in "fixing" the disability.
Social Model: Emphasizes the role of policymakers, architects, educators, and the community in creating an inclusive society.
Pros and cons of the social model of disability
Social Pros:
Reduces stigma
Empowers disabled
Focuses on barriers
Social Cons:
Denies link between physical impairment & social disability
Reduces urgency to find cures in disabled patients
Not all disability can be helped by removal of societal barriers
Outline the Implications of these disbaility models on care
Patient centred care:
Medical Model: Health care often focuses on treating the impairment, which can lead to overlooking the broader needs and rights of the individual.
Social Model: Encourages health care providers to consider the person's social context and work to reduce barriers, promoting a more holistic approach to care.
Accessibility and Inclusion:
Medical Model: May not prioritize making healthcare facilities and services accessible.
Social Model: Stresses the importance of accessible healthcare environments and services, ensuring that all individuals can receive care without facing physical or systemic barriers.
Empowerment and Participation:
Medical Model: Can sometimes lead to a paternalistic approach, where healthcare providers make decisions on behalf of the patient.
Social Model: Advocates for the empowerment of individuals with disabilities, encouraging their active participation in healthcare decisions and promoting autonomy.
Policy and Advocacy:
Medical Model: Policy may focus more on funding medical treatments and rehabilitation services.
Social Model: Advocates for policies that address social determinants of health, such as accessible housing, education, and employment opportunities, and that promote equality and non-discrimination.
What is Maslow's hierarchy of needs? Relate this to QoL (5+1)
1. Physiological needs
2. Safety and Security needs
3. Love and Belonging Needs
4. Self esteem
5. Self actualization
-the higher up you go, the more likely QoL will be increased
What is the model of responsiblity?
1. Awareness of risk: By being aware of the risk, parents are more likely to address themselves and redefine their responsibilities
2. Reproduction seen as problematic
3. Redefining elements: Situation is perceived differently, especially within the family, which can lead to decreased support. Responsibility becomes problematic.
4. Establishing self as responsible decision maker: Parents have a choice to accept the risk, modify the risk, or avoid the risk. This depends on the relationships which are prioritised.
What are the different models of addiction?
Disease Approach
Moral Code
Genetic approach
Choice model
Exposure Model
Experimental Model
What is the disease approach to addiction?
Progressive & chronic disease which is uncontrollable & requires treatment – aims to reduce stigma.
What is the Moral Code to addiction?
Result of weakness and people are addicted due to a matter of choice → increases stigma.
What is the Genetic Approach to addiction?
Genetically predisposed to certain addictive behaviours. Excludes environmental & social influence
What is the choice model of addiction?
Refers to addiction as an action of choice meaning people can choose to stop & start as they decide.
What is the Exposure Model to addiction?
Regular consumption has led to metabolic dependency & so need to use with increasing dose to receive effect.
What is the Experimental Model of addiction?
Phase of experimenting
Outline the PRIME theory?
-brings together what we know about motivation in one model
-includes our innate reactions, habits, drives, desires, goals, plans and so on
-goal is to improve our ability to explain, predict and influence behaviour
-'p.r.i.m.e', which stands for plans, responses, impulses, motives and evaluations
· PLANS- Your intention to do something - Mental representations, future action, degrees of commitment
· EVALUATION- Evaluate beliefs to make a decision
· MOTIVES- Conscious desires - what you want
· IMPULSES/INHIBITIONS- Conscious urges
· RESPONSES- Start / stop / modify actions

What are the 3 central ideas of the prime theory?
-it is wants and needs at each moment that drive our behaviour.
-our intentions and beliefs about what is good or bad only influence our actions if they create sufficiently strong wants and needs at the relevant moment.
-our image og our ourselves and how we feel about that, our identity, is a potentially very strong source of wants and needs which can be enough to overcome ones arising from biological drives such as hunger
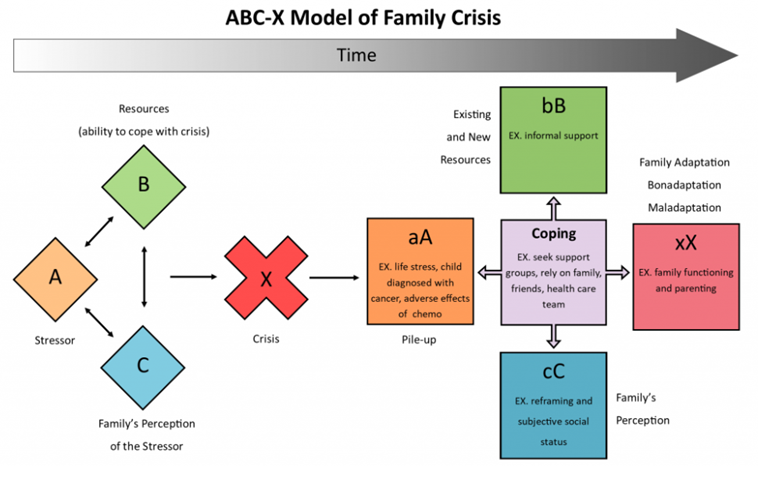
Outline the ABCX model of family crisis
Outline Transactional Model of Stress & Coping (Lazarus & Folkman)
Stress is a dynamic relationship between a person and their environment.
One becomes stressed when demands outweigh resources.
1. Primary Appraisal - is anything at risk? How bad is it?
2. Secondary Appraisal - internal & external locus coping options.
3. Coping - problem/emotion-focussed.
Name and explain 5 Stages of Grief
5 Stages of Grief - DABDA
1. Denial: patient does not want to acknowledge what is happening; protective emotion.
2. Anger: acknowledges illness but anger persists; “why me?”, “why now?”.
3. Bargaining: making deals with self to feel better; “what if I didn’t do X?”, “if I act this way I’ll feel better.”
4. Depression: crushing sadness; diagnosis no longer denied.
5. Acceptance: Illness is accepted and incorporated within life and self-identity.
Outline DNARA
1. Denial: denies having the illness.
2. Normalising: classes symptoms as normal which neutralises threat but not disease.
3. Avoidance: avoids situation which may exacerbate problem; potentially causes social exclusion.
4. Resignation: totally consumed by illness; highly dependent on others.
5. Accommodation: patient acknowledges and deals with problems illness presents.
Cognitive -Behavioural Model
1. Previous experience forms a bad memory.
2. Create a dysfunctional schema of that memory – negative assumptions about health.
3. When faced with critical ‘incident’, i.e. sharp chest pain = overthink.
4. Negative automatic thoughts:
a. Probability – perceived likelihood of illness.
b. Awfulness – perceived cost and burden of illness.
c. Coping – perceived ability to cope with illness.
d. Rescue – perceived extent to which external factors will help
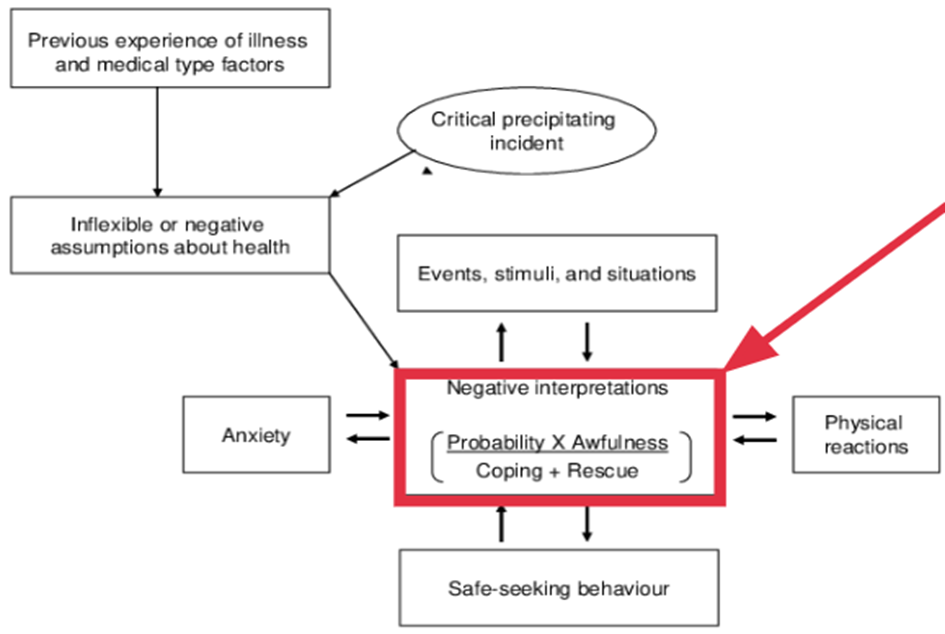
.
theory of planned behaviour
States that people’s behavioural intentions and behaviours are determined by their attitudes, social pressure (i.e. Subjective norms) and the amount of control they perceive to have over their behaviour
- Behavioural intentions determined by attitude, social pressure and amount of control exerted over behaviour.
- Highlights predictive value of attitudes and norms in intentions to quit smoking.
Socioecological Model
- Environment plays a role in order to encourage behaviour.
- Target population not individuals; be mad at fag companies, not smokers themselves
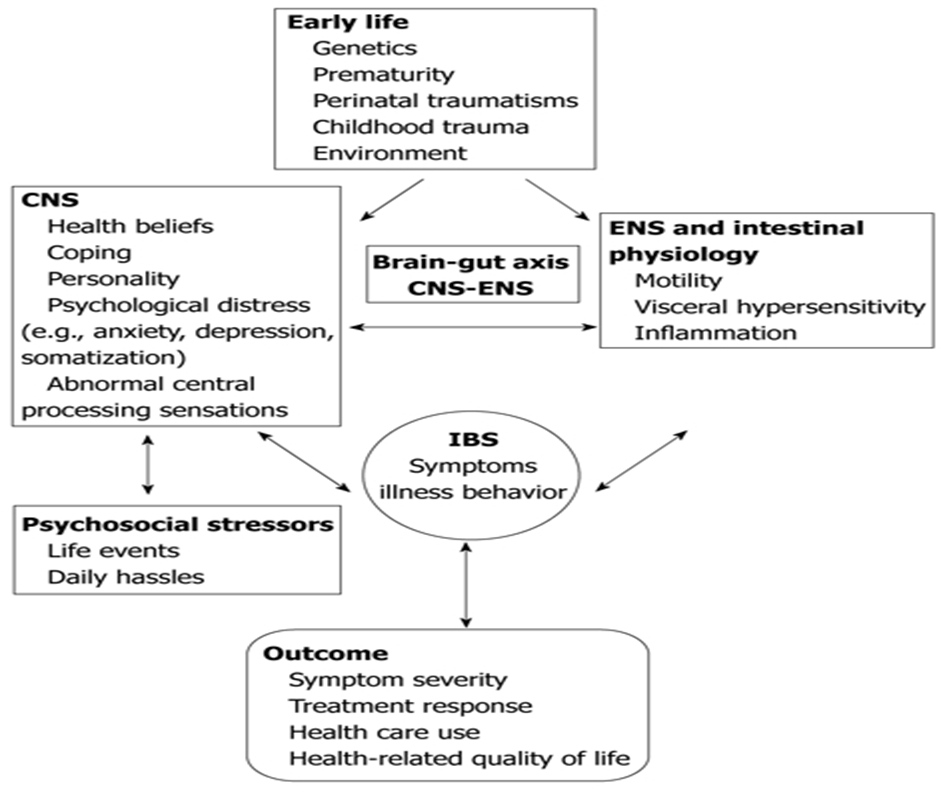
IBS
Drive Theory
- Increased arousal and determination to reach a particular goal; ‘drive’ to do something.
- Primary drives – directly related to survival.
o Food, water, oxygen.
- Secondary drives – acquired and culturally determined or learned.
o Money, intimacy, social approval.
- People have a higher drive to do better when they are being judged or looked at by others – social facilitation effect.
- Pros:
o Takes into account the importance of social pressures + norms as well as how much control a person believes they have.
- Cons:
o Focusses more on intentions than behaviours.
o Assumes you have the opportunities and resources to be successful in that behaviour.
o Fear, threat, mood and past experience.
Grounded Theory Research
- Inductive research approach where you have a question or a bunch of qualitative data and you need to develop a hypothesis from it; collect, analyse data & create hypothesis.
- Used where no existing theory is related; existing theory incomplete.
o Unlike research where researchers choose a theory and only collect data that supports that theory.
Steps of grounded theory approach:
1. Determine initial research question.
2. Collect and review data – theoretical sampling.
3. Repeated ideas are tagged with codes.
4. Codes are grouped into concepts and then into categories.
5. Constant comparison!!!
6. Eventually these categories may become basis of new theory.