Unit 6 - Craniomandibular
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
83 Terms
Pathoanatomy: Temporomandibular Joint Pain with Mobility Deficits
What is the proposed underlying cause of the condition?
Arthralgia (capsulitis/synovitis)
Capsular fibrosis
Osteoarthritis
Disk displacement without reduction
Pathoanatomy: TMJ Pain with Mobility Deficits
What is the proposed underlying cause of the condition?
Arthralgia (capsulitis/synovitis)
Inflammatory condition of the capsule and extracapsular articular soft tissue
Pathoanatomy: TMJ Pain with Mobility Deficits
What is the proposed underlying cause of the condition?
Capsular fibrosis
Loss of capsular mobility
Pathoanatomy: TMJ Pain with Mobility Deficits
What is the proposed underlying cause of the condition?
Osteoarthritis
Progressive degeneration of the articular cartilage
Pathoanatomy: TMJ Pain with Mobility Deficits
What is the proposed underlying cause of the condition?
Disk displacement without reduction
Displacement of the articular disk anterior to the condyle blocking further anterior translation
Progressed from disk displacement with reduction and hypermobility
Medical Screening: TMJ Pain with Mobility Deficits
What other conditions should be considered with this patient presentation?
Viscerogenic
Neoplastic conditions
Inflammatory or systemic disease
Cardiopulmonary conditions
Cervical vascular pathology
Medical Screening: TMJ Pain with Mobility Deficits
What other conditions should be considered with this patient presentation?
Neuromusculoskeletal
Spinal fracture
Cervical myelopathy
Upper cervical ligamentous instability
Medical Screening: TMJ Pain with Mobility Deficits
What other conditions should be considered with this patient presentation?
Psychological
Anxiety
Depression
Differential Diagnosis: TMJ Pain with Mobility Deficits
What other conditions should be considered with this patient presentation?
Neuromusculoskeletal
Neck pain with headache
Trigeminal neuralgia
Trigeminal neuralgia
condition that leads to neuropathic symptoms in the face, in the distribution of the trigeminal nerve, and should be considered
Differential Diagnosis: TMJ Pain with Mobility Deficits
What other conditions should be considered with this patient presentation?
Primary headache
Migraine
Tension-type
Differential Diagnosis: TMJ Pain with Mobility Deficits
What other conditions should be considered with this patient presentation?
Dental conditions
might require outside referral
Subjective Examination: TMJ Pain with Mobility Deficits
What system, structure, pain mechanism, and phases of healing are unique to this patient presentation?
System
Neuromusculoskeletal
Structure
Temporomandibular joint and periarticular soft tissue
Pain mechanism
Nociceptive, nociplastic
Phase of healing
Muscle strain 2-4 weeks, capsule sprain and cartilage injuries 10-12 weeks
Subjective Examination: TMJ Pain with Mobility Deficits
What are common subjective reports for patients with mobility deficits?
Arthralgia
Recent history of parafunctional oral habits or trauma
May be gradual or immediate onset
May report tenderness to palpation
Symptom reproduction with biting on the contralateral side
No current joint sounds if in isolation
Subjective Examination: TMJ Pain with Mobility Deficits
What are common subjective reports for patients with mobility deficits?
Capsular fibrosis
History of trauma, disk displacement without reduction, or immobilization
Gradual onset
Will report limited mouth opening
No current joints sounds, may have a previous history of end rage or mid range clicks
May be pain-free
Subjective Examination: TMJ Pain with Mobility Deficits
What are common subjective reports for patients with mobility deficits?
Osteoarthritis
History of trauma, disc displacement without reduction
Older age with gradual onset
Crepitus currently, may have a previous history of end rage or mid range joint sounds
May report tenderness to palpation and limited mouth opening
Radiographic evidence of osteoarthritis
Subjective Examination: TMJ Pain with Mobility Deficits
What are common subjective reports for patients with mobility deficits?
Disk displacement without reduction
History of disc displacement with reduction and hypermobility
Previous history of reciprocal mid range and end range joint sounds
No current joint sounds
History of joint locking or catching
Acutely will have a sudden loss of range of motion
Chronically range of motion may be normal
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Systems Review: Cardiopulmonary
Vitals – BP, HR, auscultate
Assess for mechanical reproduction of symptoms and/or adverse response to movement
AROM, PIVM, compression/distraction
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Systems Review: Neuromusculoskeletal
Cranial nerves
Reflexes/pathological reflexes
Dermatomes/myotomes
Upper cervical ligamentous testing
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Structural examination
Dental occlusion
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Palpation examination
Tenderness to palpation of the lateral condyle and/or posterior compartment
Point tenderness may include myofascial trigger points if concurrent myalgia
Increases resting tone of superficial cervical muscles and muscles of mastication
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Specific Tests and Measures: Movement and provocation examination
Cervical clearing examination
TMJ active range of motion
TMJ passive accessory testing
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Cervical clearing examination
Active range of motion
Passive intervertebral motion
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
TMJ active range of motion
May see limited range of motion due to pain and/or joint hypomobility
Deviation towards ipsilateral side with opening and protrusion
Limited contralateral lateral excursion
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
TMJ passive accessory testing
Possible reproduction of symptoms and joint hypomobility
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Specific Tests and Measures: Orthopaedic examination tests
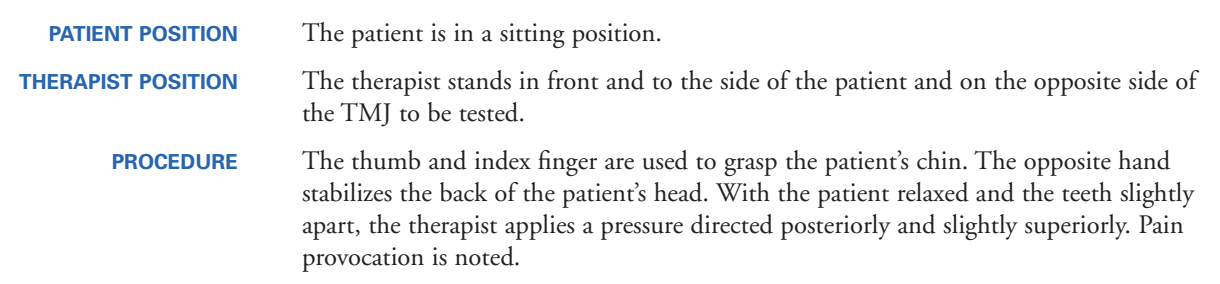
Forced retrusion (compression) TMJ provocation test
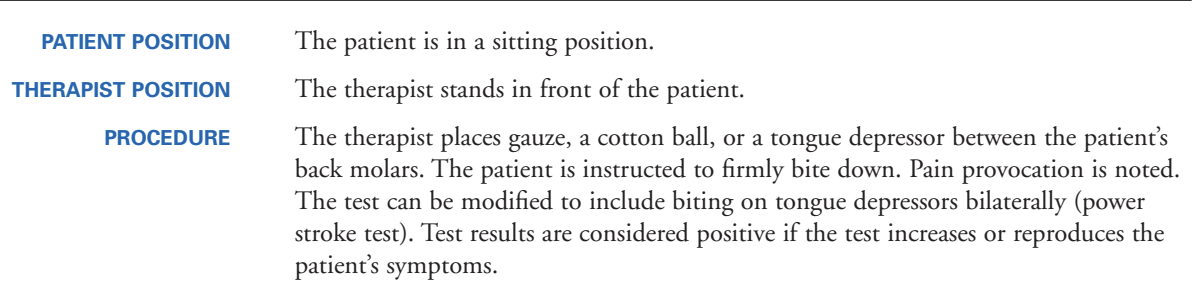
Forced biting provocation test (dental stick test)
Auscultation of the TMJ
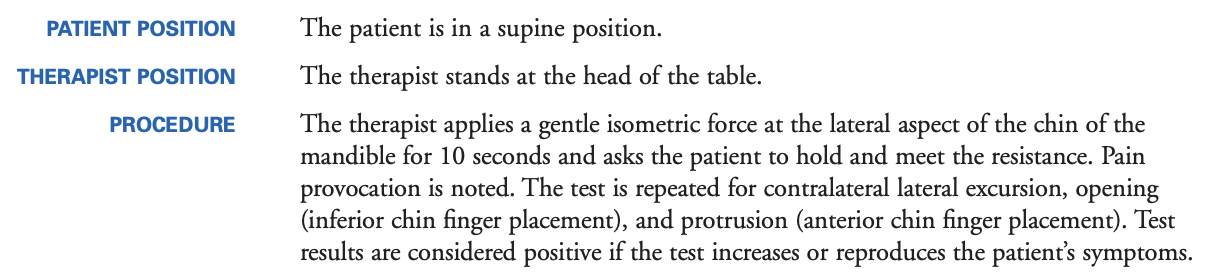
Muscles of mastication isometric resistive provocation test
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Forced retrusion (compression) TMJ provocation test
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Forced biting provocation test (dental stick test)
Arthralgia, osteoarthritis
Reproduction of symptoms – contralateral side
Sn 0.71, Sp 0.77; +LR 3.09
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Auscultation of the TMJ
Osteoarthritis
Sn 0.70, Sp 0.43; +LR 1.23 –LR 0.70
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Muscles of mastication isometric resistive provocation test
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Specific Tests and Measures: Muscle performance examination
Muscle recruitment and endurance
Muscle length testing
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Muscle recruitment and endurance
Deep neck flexors and extensors
Parascapular muscles
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Muscle length testing
Cervicoscapulothoracic muscles
Objective Examination: TMJ Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Test-item cluster (Disk displacement without reduction)
Dental stick test
Isometric test
Joint provocation test
Joint sound test (crepitus)
Deviation with mandibular opening
Limited contralateral lateral excursion
Limited anterior glide accessory test
5/7 positives Sn 0.71, Sp 0.91; +LR 7.89
Prognosis: TMJ Pain with Mobility Deficits
What is the prognosis of the condition?
Clinical course and prognosis
Minimal evidence to project clinical course and prognosis for conservative management
Intraoral devices demonstrate inferior effectiveness to manual therapy
Only 50% of patients after TMJ arthroplasty report a favorable outcome
Interventions: TMJ Pain with Mobility Deficits
What are interventions recommended for mobility deficits?
Education
Exercise
Manual therapy
Interventions: TMJ Pain with Mobility Deficits
What are interventions recommended for mobility deficits?
Education
Cessation of parafunctional oral habits
Mouth resting position
Limit positions that load the joint
Soft diet and small bites
Interventions: TMJ Pain with Mobility Deficits
What are interventions recommended for mobility deficits?
Exercise
Exercises that promote range of motion and mobility of the TMJ
Impairment-based approach to address cervicoscapulothoracic mobility, flexibility, endurance, neuromuscular control, and strength
Rocabado 6x6
Rocabado 6x6
a common set of exercises that ask the patient to perform six cervical spine and timber temporomandibular joint exercises, six times per day for six repetitions
Interventions: TMJ Pain with Mobility Deficits
What are interventions recommended for mobility deficits?
Manual therapy
Mobilization of the TMJ
Mobilization and manipulation of the cervicothoracic spine
Interventions: TMJ Pain with Mobility Deficits
When should we consider interprofessional or intraprofessional referral and what are other treatment options?
Imaging
Medical Intervention
Psychological
Interventions: TMJ Pain with Mobility Deficits
When should we consider interprofessional or intraprofessional referral and what are other treatment options?
Imaging
Radiograph necessary to confirm osteoarthritis
Indicated only when a non-musculoskeletal condition is suspected to failure of conservative management where imaging may change the course of care
Interventions: TMJ Pain with Mobility Deficits
When should we consider interprofessional or intraprofessional referral and what are other treatment options?
Medical Intervention
Medications
Injections
Intra-oral appliances
Arthroplasty
Interventions: TMJ Pain with Mobility Deficits
When should we consider interprofessional or intraprofessional referral and what are other treatment options?
Psychological
Counseling
Meditation
Biofeedback
Pathoanatomy: TMJ with Movement Coordination Impairments
What is the proposed underlying cause of the condition?
Hypermobility
Disk displacement with reduction
Mylagia
Pathoanatomy: TMJ with Movement Coordination Impairments
What is the proposed underlying cause of the condition?
Hypermobility
Increased extensibility and laxity of the passive stabilizing elements of the joint
May be congenital or acquired through repetitive strain to the capsule and posterior and collateral ligaments
Pathoanatomy: TMJ with Movement Coordination Impairments
What is the proposed underlying cause of the condition?
Disk displacement with reduction
Displacement of the articular disk anteriorly that reduces
Progression from hypermobility
Pathoanatomy: TMJ with Movement Coordination Impairments
What is the proposed underlying cause of the condition?
Mylagia
Painful guarded muscles of mastication (masseter, temporalis, lateral pterygoid) with taut bands and myofascial trigger points
Parafunctional habits, joints conditions, stress and anxiety, nociplastic pain
Medical Screening: TMJ with Movement Coordination Impairments
What other conditions should be considered with this patient presentation?
Viscerogenic
Neoplastic conditions
Inflammatory or systemic disease
Cardiopulmonary conditions
Cervical vascular pathology
Medical Screening: TMJ with Movement Coordination Impairments
What other conditions should be considered with this patient presentation?
Neuromusculoskeletal
Spinal fracture
Cervical myelopathy
Upper cervical ligamentous instability
Medical Screening: TMJ with Movement Coordination Impairments
What other conditions should be considered with this patient presentation?
Dental conditions
need to be screened
might mimic temporomandibular dysfunction
Medical Screening: TMJ with Movement Coordination Impairments
What other conditions should be considered with this patient presentation?
Psychological
Anxiety
Depression
Differential Diagnosis: TMJ with Movement Coordination Impairments
What other conditions should be considered with this patient presentation?
Neuromusculoskeletal
Neck pain with headache
Trigeminal neuralgia
Differential Diagnosis: TMJ with Movement Coordination Impairments
What other conditions should be considered with this patient presentation?
Primary headache
Migraine
Tension-type
Subjective Examination: TMJ with Movement Coordination Impairments
What system, structure, pain mechanism, and phases of healing are unique to this patient presentation?
System
Neuromusculoskeletal
Structure
Temporomandibular joint and periarticular soft tissue
Pain mechanism
Nociceptive, nociplastic
Phase of healing
Muscle strain 2-4 weeks, capsule sprain and cartilage injuries 10-12 weeks
Subjective Examination: TMJ with Movement Coordination Impairments
What are common subjective reports for patients with movement coordination impairments?
Hypermobility
May have history of parafunctional oral habits
During end range opening may report a click
Generally asymptomatic unless combined with a myalgia or arthralgia
Can report pain with end range opening activities like eating or yawning
Subjective Examination: TMJ with Movement Coordination Impairments
What are common subjective reports for patients with movement coordination impairments?
Disk displacement with reduction
History of joint hypermobility
Presence of reciprocal mid range click
Previous history of reciprocal end range joint sounds
No report of range of motion loss unless combined with myalgia or arthralgia
Subjective Examination: TMJ with Movement Coordination Impairments
What are common subjective reports for patients with movement coordination impairments?
Mylagia
May have a history of parafunctional oral habits, stress and anxiety, or nocipalstic pain conditions
May have history of other temporomandibular joint conditions with associated symptoms
No joints sound if occurring in isolation
Pain with palpation of the involved muscles or eating and chewing
May have painful, limited opening if masseter and temporalis are involved
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Systems Review: Cardiopulmonary
Vitals – BP, HR, auscultate
Assess for mechanical reproduction of symptoms and/or adverse response to movement
AROM, PIVM, compression/distraction
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Systems Review: Neuromusculoskeletal
Cranial nerves
Reflexes/pathological reflexes
Dermatomes/myotomes
Upper cervical ligamentous testing
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Structural examination
Dental occlusion
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Palpation examination
Tenderness to palpation of the lateral condyle and/or posterior compartment
Point tenderness may include myofascial trigger points if concurrent myalgia
Increases resting tone of superficial cervical muscles and muscles of mastication
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Movement and provocation examination
Cervical clearing examination
TMJ active range of motion
TMJ passive accessory testing
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Cervical clearing examination
Active range of motion
Passive intervertebral motion
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
TMJ active range of motion
End range or reciprocal click possible
Aberrant motions common
May see limited range of motion due to pain or could be full to hypermobile
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
TMJ passive accessory testing
Possible reproduction of symptoms and joint hypermobility
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Orthopaedic examination tests
Forced retrusion (compression) TMJ provocation test
Forced biting provocation test (dental stick test)
Auscultation of the TMJ
Muscles of mastication isometric resistive provocation test
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Forced retrusion (compression) TMJ provocation test
Reproduction of symptoms – Joint
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Forced biting provocation test (dental stick test)
Pain on opposite side – Joint
Pain on same side or bilateral – Muscle
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Auscultation of the TMJ
Joint sounds during midrange or end range active range of motion
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Muscles of mastication isometric resistive provocation test
Masseter and temporalis
Limited, painful opening and pain with power stroke
Pain-free resisted lateral excursion and protrusion
Lateral pterygoid
Full, pain free opening
Pain with resisted protrusion and power stroke
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Muscle performance examination
Muscle recruitment and endurance
Muscle length testing
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Muscle recruitment and endurance
Deep neck flexors and extensors
Parascapular muscles
Objective Examination: TMJ with Movement Coordination Impairments
What are the key examination procedures for patients with movement coordination impairments?
Muscle length testing
Cervicoscapulothoracic muscles
Prognosis: TMJ with Movement Coordination Impairments
What is the prognosis of the condition?
Clinical course and prognosis
Minimal evidence to project clinical course and prognosis for conservative management
Intraoral devices demonstrate inferior effectiveness to manual therapy
Only 50% of patients after TMJ arthroplasty report a favorable outcome
Interventions: TMJ with Movement Coordination Impairments
What are interventions recommended for movement coordination impairments?
Education
Exercise
Manual therapy
Interventions: TMJ with Movement Coordination Impairments
What are interventions recommended for movement coordination impairments?
Education
Cessation of parafunctional oral habits
Mouth resting position
Limit positions that load the joint
Soft diet and small bites
Interventions: TMJ with Movement Coordination Impairments
What are interventions recommended for movement coordination impairments?
Exercise
Exercises that promote proprioception and neuromuscular control
Impairment-based approach to address cervicoscapulothoracic mobility, flexibility, endurance, neuromuscular control, and strength
Rocabado 6x6
Interventions: TMJ with Movement Coordination Impairments
What are interventions recommended for movement coordination impairments?
Manual therapy
Soft tissue manipulation and dry needling
Joint mobilization and manipulation of the TMJ and cervicothoracic spine
Interventions: TMJ with Movement Coordination Impairments
When should we consider interprofessional or intraprofessional referral and what are other treatment options?
Imaging
Medical Interventions
Psychological
Interventions: TMJ with Movement Coordination Impairments
When should we consider interprofessional or intraprofessional referral and what are other treatment options?
Imaging
Radiograph necessary to confirm osteoarthritis
Indicated only when a non-musculoskeletal condition is suspected to failure of conservative management where imaging may change the course of care
Interventions: TMJ with Movement Coordination Impairments
When should we consider interprofessional or intraprofessional referral and what are other treatment options?
Medical Intervention
Medications
Injections
Intra-oral appliances
Arthroplasty
Interventions: TMJ with Movement Coordination Impairments
When should we consider interprofessional or intraprofessional referral and what are other treatment options?
Psychological
Counseling
Meditation
Biofeedback