Ocular Diagnostics Midterm
1/165
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
166 Terms
Case History purpose
establish a caring relationship with patient
-gather information about patient's chief complaint, visual function, ocular and systemic health, risk factors, and lifestyle
-begin process of differential diagnosis and patient education
what is the most important procedure of the examination?
obtaining a thorough case history
Case history components
1. Introduction
2. Chief Complaint/History of present illness
3. Past medical History and Review of Systems
4. Family History
5. Summary
when does the clinician begin diagnostic thought process?
by asking appropriate questions during case history
Chief complaint
the main reason for the patient's visit
-use open ended questions
History of preset illness (HPI)
elaborate on CC
use FOLDARQ
Background information
Ocular history, medical history, medications, family medical history, family ocular history, social history and review of systems
questions for patients who smoke
-for how long?
-how many per day?
can be used to determine whether the patient is a heavy or light smoker
commonly missed items (during case history)
-inquire about any other complaints, in addition to chief complaint
-compliance with current medication
-any other medications
4 components of history
1. Chief Complaint
2. History of Present Illness
3. Review of Systems
4. Past, Family, and Social History
several reasons for visit
list them in order of importance
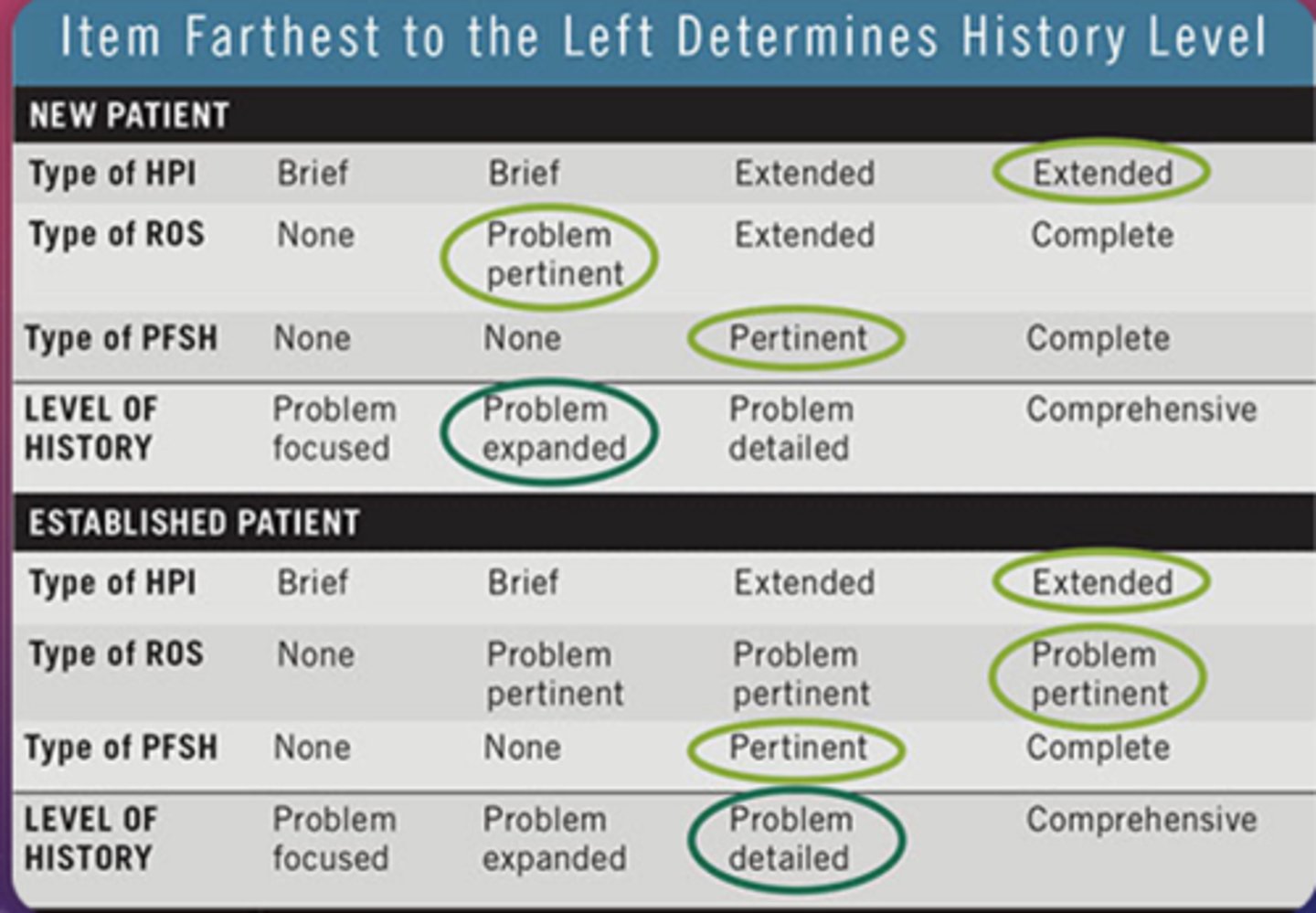
case history and coding
-level of history that is involved in an office visit is one of the three criteria that determine which E&M code can be billed
finding history level
1. determine the type of HPI, ROS, and PFSH
2. Circle the appropriate HPI, ROS, and PFSH
3. Criterion that is farthest to left determine level of history
positives marked on ROS
must be accompanied by a statement of treatment plan; otherwise, they won't necessarily count
-If patient states they have asthma, you might document that she controls it with an inhaler
PFSH elements
1. Past history, which focuses on prior major illness, operations, current medications, and allergies
2. Family history should document members of the family who have disease that may be hereditary
3. Social history focuses on smoking, drinking, and drug uses, as well as employment or job duties
when does patient communication occur?
-Before
--scheduling, appointment reminders, history forms
-During
--case history, elements of the exam, pt education
-After
--post-exam education, referrals, follow-up appointment scheduling
Verbal communication
face to face, telephone, video
nonverbal communication
facial expression, body language, hand movements
written communication
email, report, chat
listening communication
active act of absorbing verbal communication
-required for effective communication
visual communication
imagery through platforms, videos, memes
patient greeting
Part of patient interaction- make eye contact, introduce yourself, speak clearly, verify patient identity
understanding patient's emotions
anxiety
-towards "1 or 2" and puff of air test
Fear
-vison loss, mental health problems, vision symptoms "floaters", and loss of independence
Financial considerations
patient education
discuss in layman's terms, check for understanding and provide additional educational resources
delivering bad news
make eye contact, be frank but understanding and empathetic, provide resources
exam flow
1. case history
2. eye health
3. refractive status
4. functional vision
5. assessment/plan/Rx/PT. ED
Eye health
-general medical observation (observe pt as a whole)
-Ocular health assessment
-Ancillary testing
Refractive Status
-Obtained by performing manifest refraction (goal is 20/20)
-Refractive errors are corrected with refractive corrections
-Some patients are not correctable to 20/20
functional vision
-assessment of the patient's accommodative system and vergence system
-an assessment of how well the eyes work together
endpoint of functional vision
clear, comfortable, binocular vision for all visual tasks
assessment and plan
the conclusion to the clinical examination
Assessment refers to the pertinent diagnoses made.
Plans refer to the decisions made for each diagnosis.
differences in exam types
depends on the reason for the visit
-Vison or medical
-comprehensive or wellness
Confrontation Visual Fields
Assessment of peripheral vision
-conducted 60-80cm in front of the patient at eye level
-patient does not wear SRx
-monocular
-bright illumination
-examiner closes eye opposite to pt
finger counting
examiner presents 1, 2, or 4 fingers approximately 20 to 30 degrees from fixation
-ensure hand is perpendicular to the patients visual axis
-be sure to present fingers halfway between examiner and patient
-do not present finger on horizontal midline
advantages of CVF
simplicity, flexibility, requires no specialized instrumentation (can be performed in any setting)
disadvantages of CVF
-can not determine the exact size of field loss (qualitative not quantitative)
-lack of standardization
-not sensitive enough to detect subtle defects
recording CVF
full to finger count
-shading in restricted areas on field
ex. OD: no defects (or full) OS: superior nasal restricted field
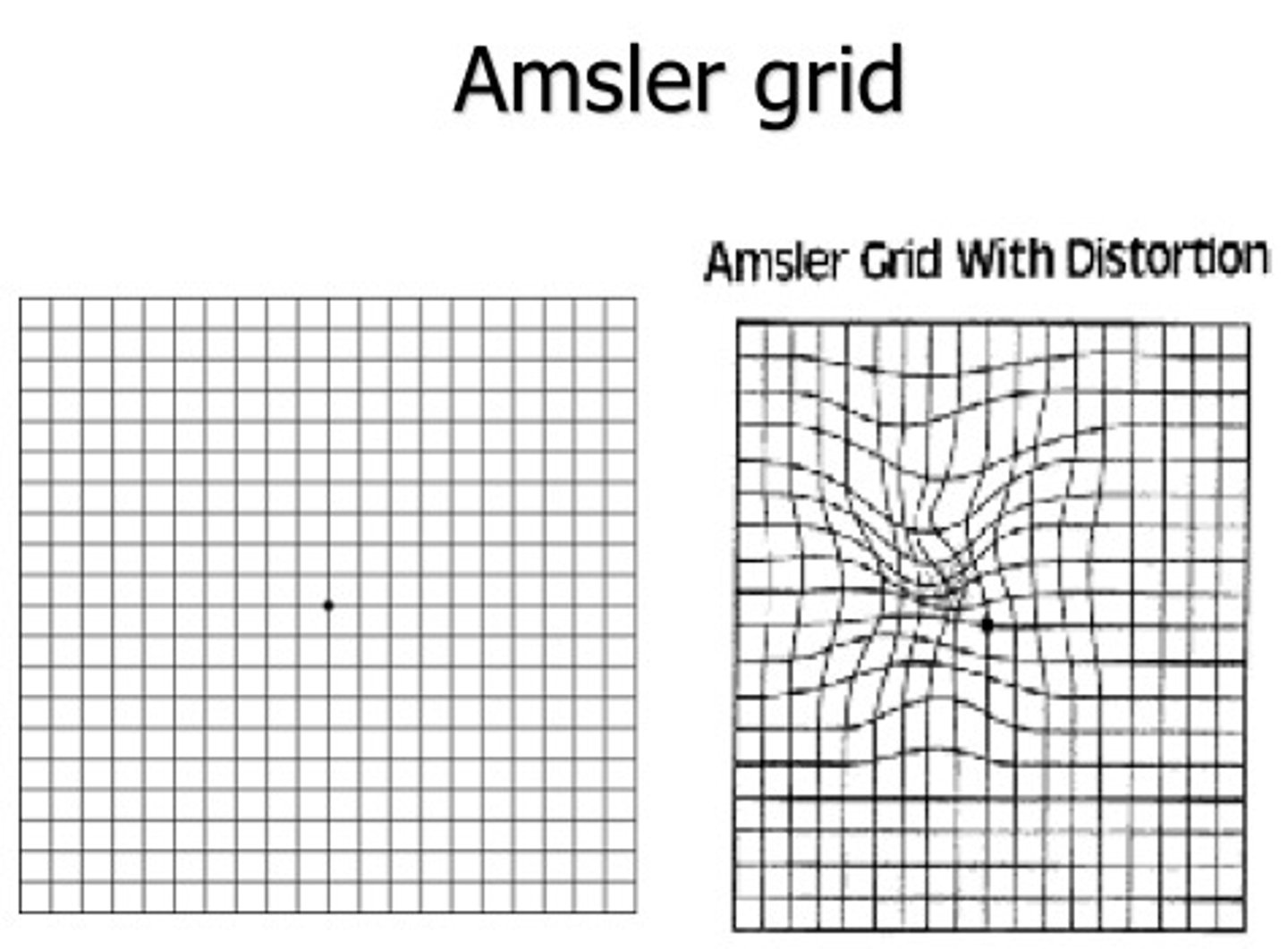
Amsler grid test
test to assess central vision and to assist in the diagnosis of age-related macular degeneration
-monocular
-ask pt if any squares within the grid are missing or blurred or if the lines are appear wavy or distorted
-record findings on recording sheet; patient can draw what they see
visual acuity purpose
measure the clarity of vision or the ability of the visual system to resolve detail
numerator of VA
test distance
-typically 20ft or 6 meters
a patient's VA depends on
the accuracy of the retinal focus, the integrity of the eye's neural elements, and the interpretive faculty of the brain
denominator of VA
distance at which the smallest discernable letter subtends 5 minutes of arc
-also stated: distance at which a person with 20/20 acuity would discern the same letter
when should VA be done?
the first procedure following the case history
setting up VA
-pt wears habitual correction for the distance being tested
-acuity chart shown with multiple lines
-room illumination should maximize contract on the VA chart used
-occluder to cover eye
what should the examiner observe when performing VA?
always the patient
-make sure they have eye covered properly
-not squinting
when should the examiner stop the pt during VA?
when more than half the letter son a line have been missed
what should happen when the pt can not see the largest letter on the chart?
have the pt walk toward chart until they can just make out the largest letter
-not the distance
tests for dVA (after walk-up testing)
-finger counting
-hand motion
-light projection
-light perception
-no light perception
near VA
-provide high illumination on near point card
-card at appropriate distance for which it is calibrated
16 in (40 cm) for reduced Snellen Acuity Card
types of near VA charts
-reduced snellen
-logMAR
-Tumbling E
-Reduced LEA symbols
-Cards with words or paragraphs
-Samples of newsprint, playing cards, the Bible, or musical staff notation
recording nVA
can be recorded in Snellen notation, logMAR, N units (used by printers), decimal notation or M units
what notation should be avoided for recording nVA?
Jaeger notation
-since the difference between the sizes of letters on different lines is not consistent
M units
used for assessing near visual acuity in low-vision patients and increasingly used for primary car patients
20/20 is recorded as 0.4/.4M
20/50 is 0.4/1.0M
cc
with correction
sc
without correction
cCL
visual acuity take through contact lenses
recording VA
record the Snellen fraction or print size for smallest (lowest) line in which more than half the letter were correctly identified
-record quality of pt's response
LogMAR chart
the incremental size of letter is determined according to the base 10 logarithm of the critical detail in minute of arc of the letters
LogMAR charts should be used when
a precise, quantitative assessment of VA is needed
-VA in logMAR should be used in all research studies where VA is a dependent variable
logMAR scoring
circle each letter correct and put a X through incorrect letters
-proceed until pt incorrectly identifies at least 4 of 5 letters
logMAR formula
multiply number of letter read correctly by 0.02 and subtract this product from 0.10 more than the LogMAR of the first line read
ex. pt began reading at 0.10
logMAR VA= 0.20 - (0.02 x # of letters correctly read)
expected findings for logMAR
VA of 0.0 or better (-0.01) is considered normal
-the difference between the two eyes should be no greater than 0.16
pinhole VA purpose
to determine if a decrease in vision is correctable by lenses
-taken when the VA is worse than 20/30 at both distance and near through habitual or induced correction
anterior
toward the front
posterior
toward the back
superior
toward top of the head
inferior
away from the head
nasal
toward the nose
temporal
toward the temple
inner
toward the center
outer
away from the center
fick's axes
all eye movements can be described as rotation about one or more axes, around a center of rotation
-x-axis (horizontal/transverse)
-y-axis (sagittal
-z-axis (vertical)
x-axis rotation
elevation and depression
y-axis rotation
extorsion and intorsion
z-axis rotation
adduction and abduction
vergences
moving against each other
-convergence
-divergence
versions
moving with each other
-right gaze (dextroversion)
-left gaze (levoversion)
-up gaze (supraversion)
-down gaze (infraversion)
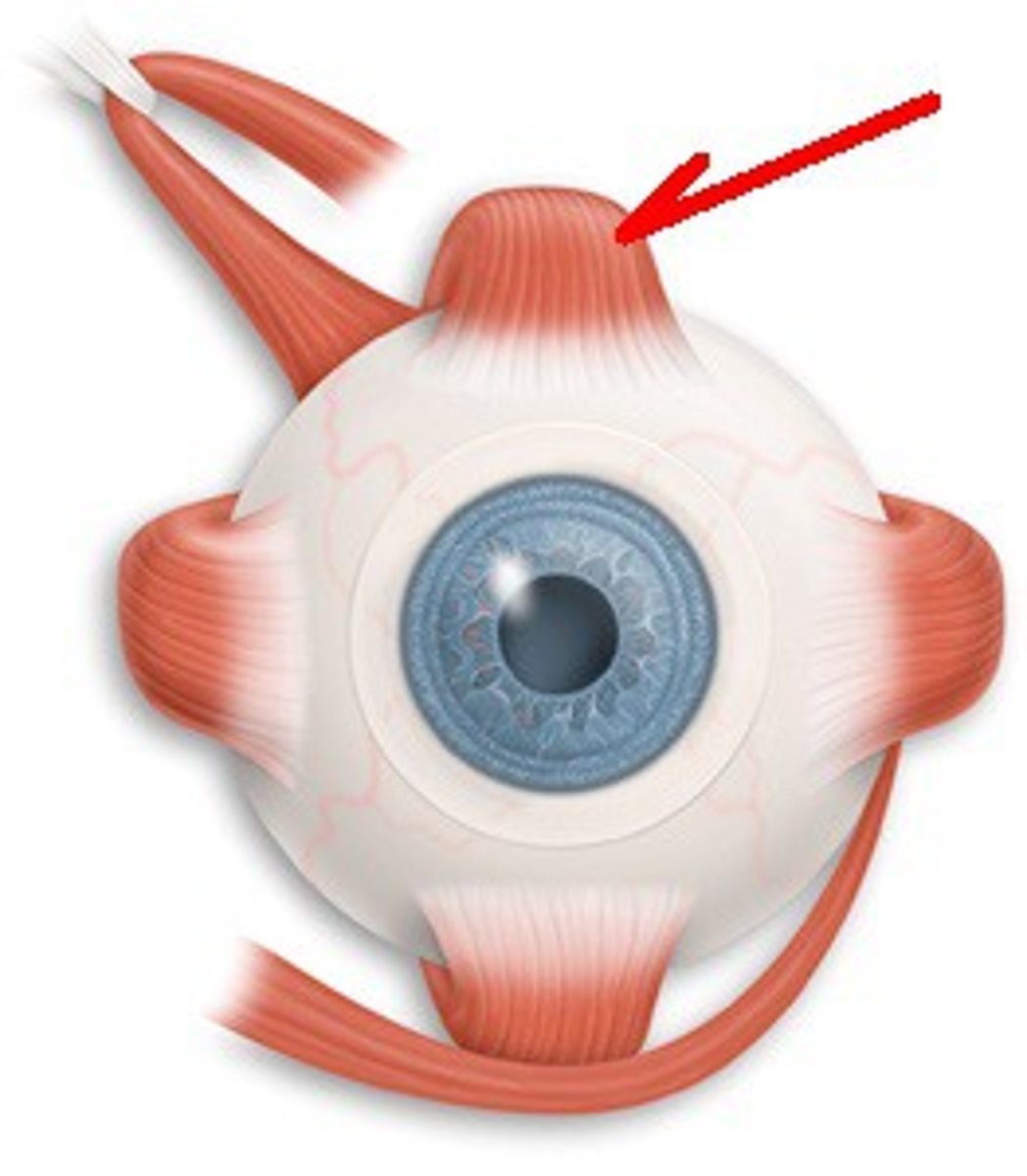
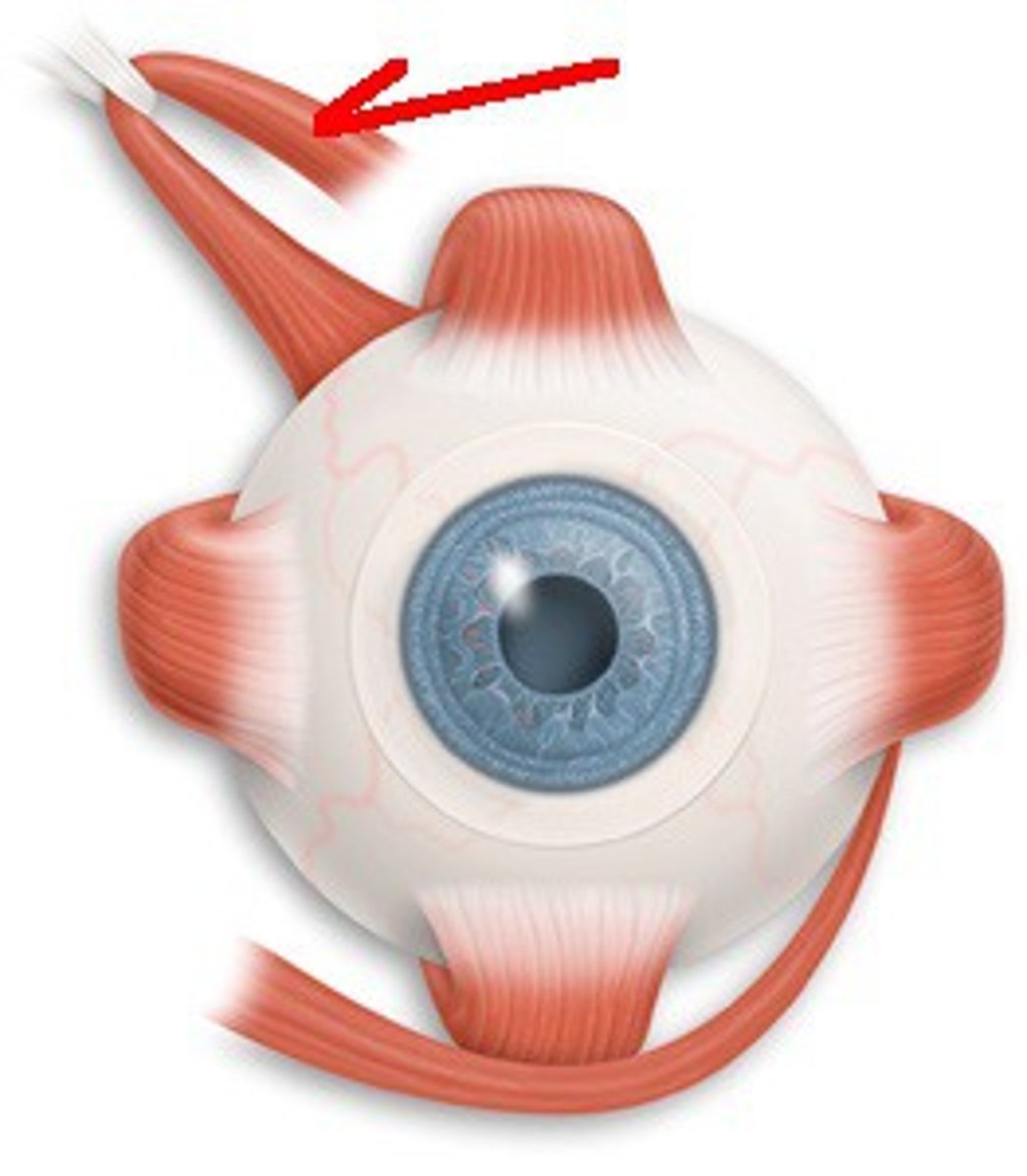
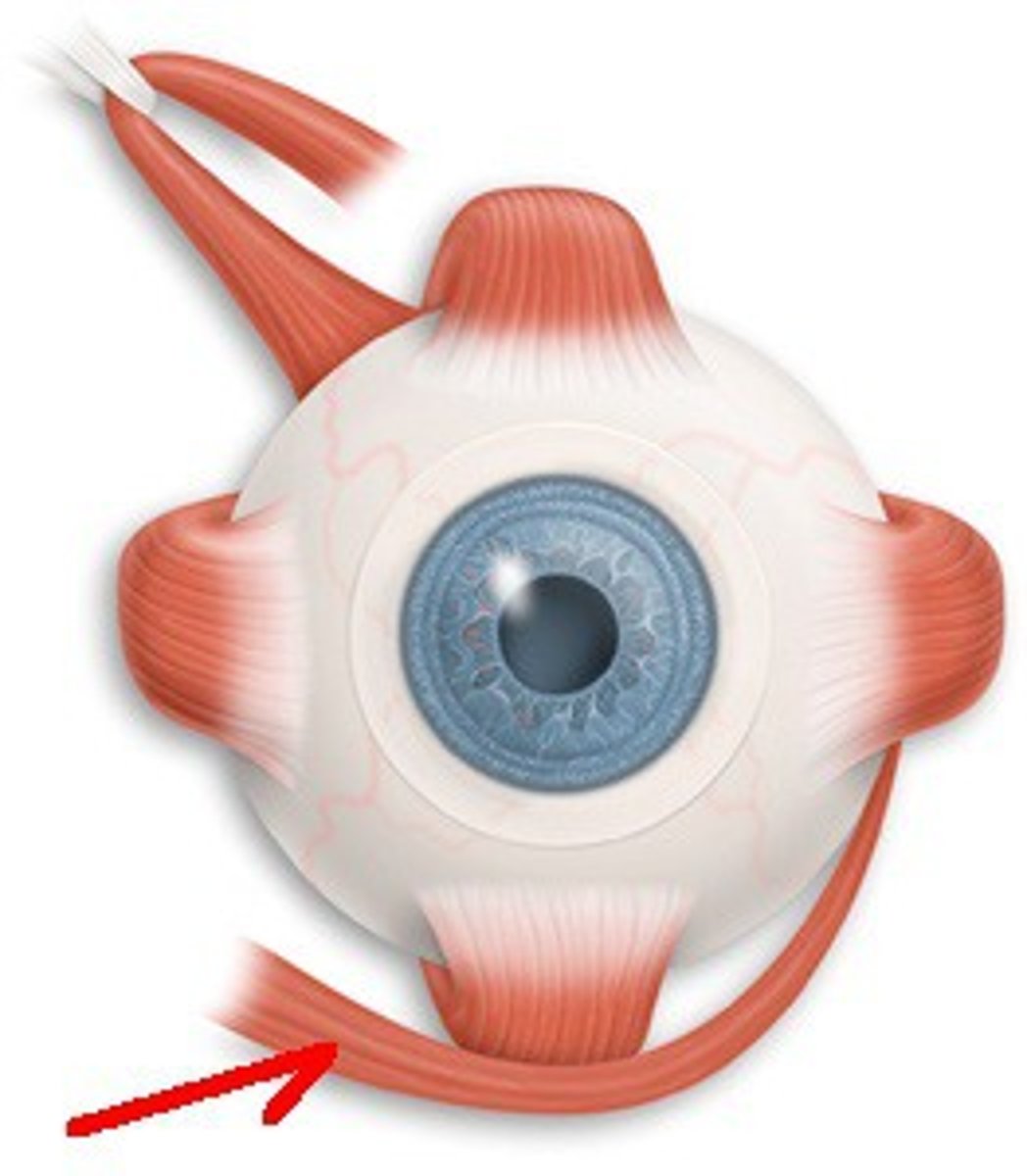
extraocular muscles
-striated muscles
-6 per eye
-each is innervated by a cranial nerve
-each has a least one action
-most have multiple actions
lateral rectus
primary: abduction
secondary: none
Cranial Nerve 6
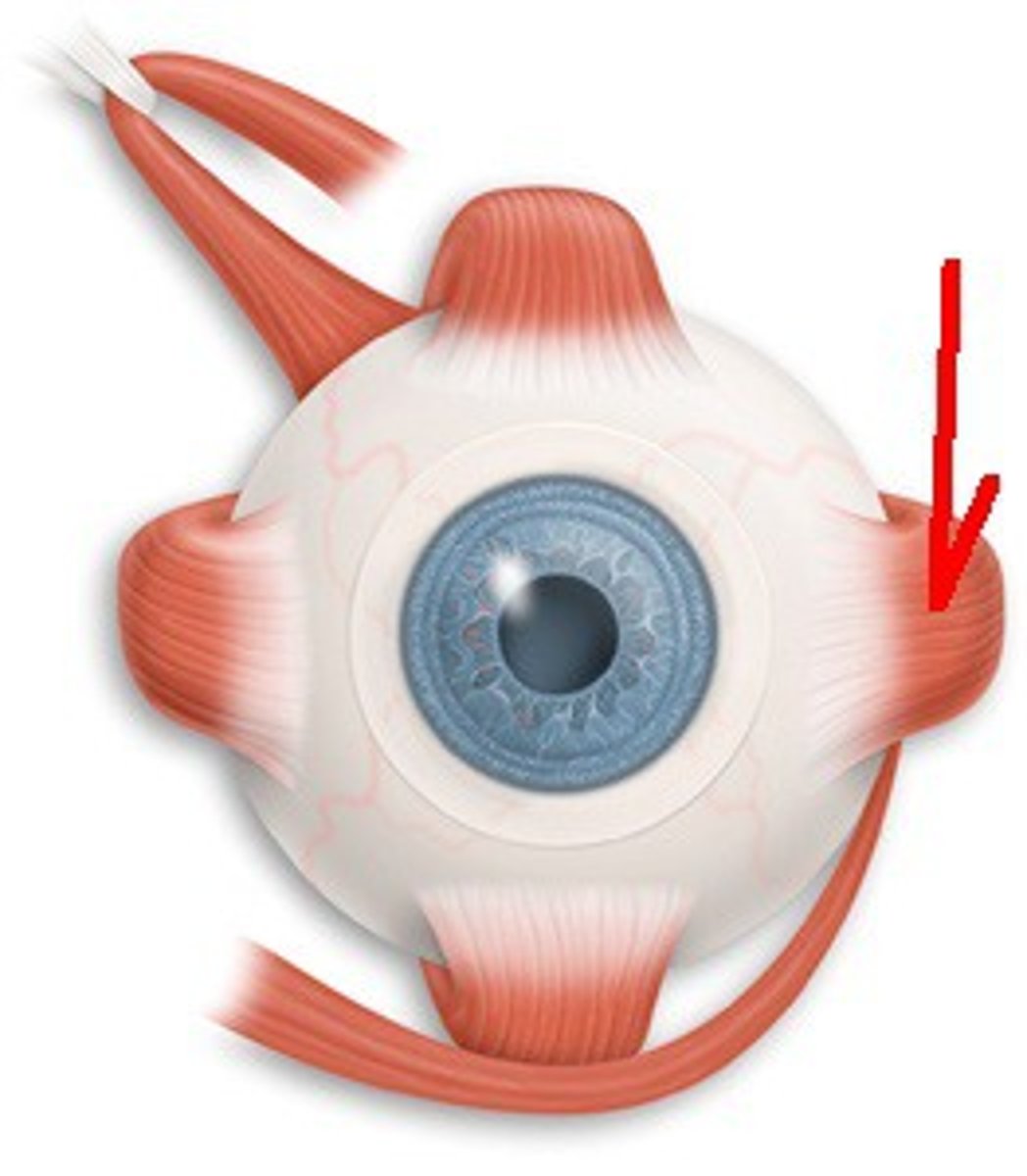
Medical Rectus
primary: adduction
secondary: none
Cranial Nerve 3
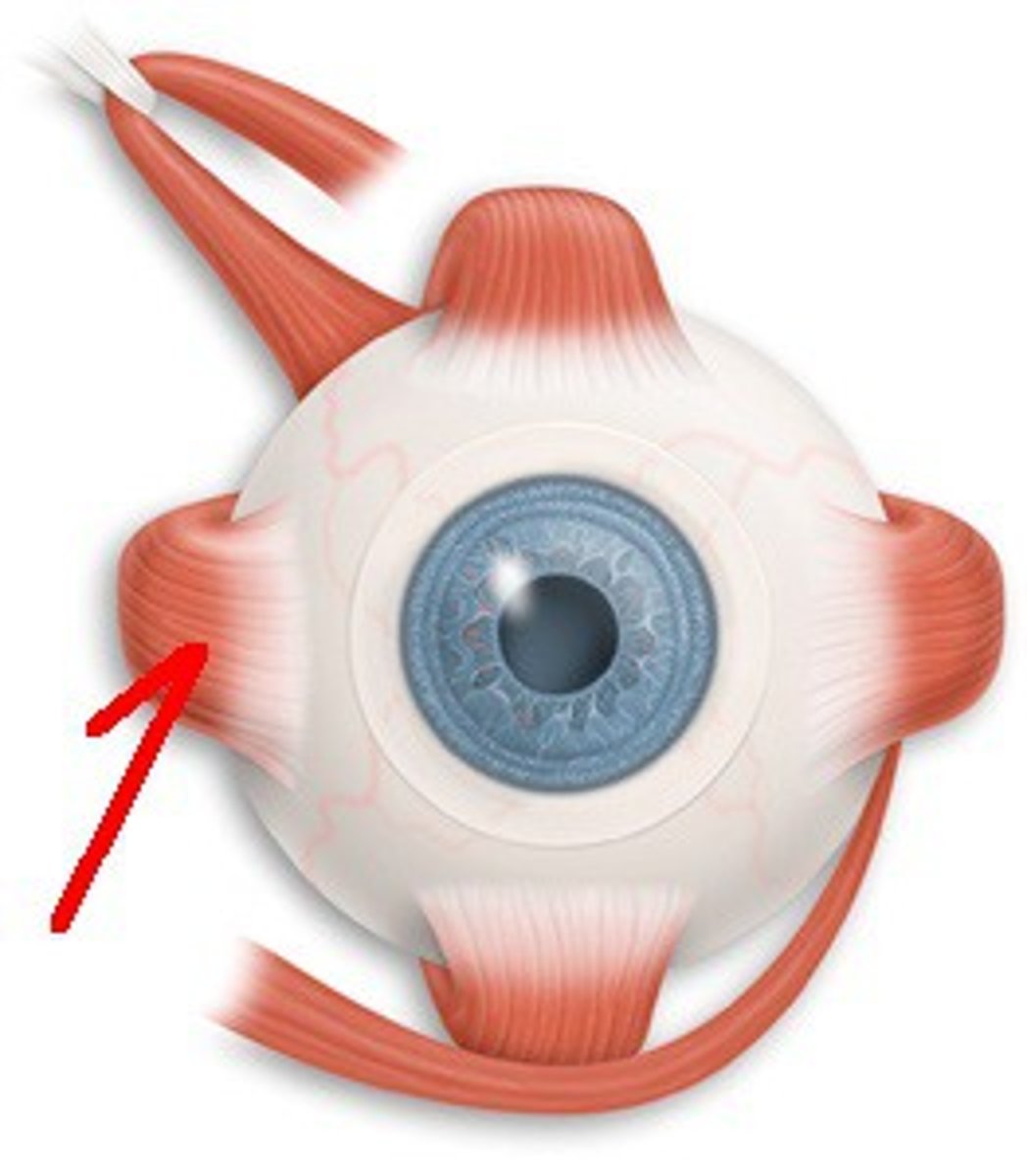
Superior Rectus
primary: elevation
secondary: adduction and intorsion
Cranial Nerve 3
Inferior Rectus
primary: depression
secondary: adduction and extorsion
Cranial Nerve 3
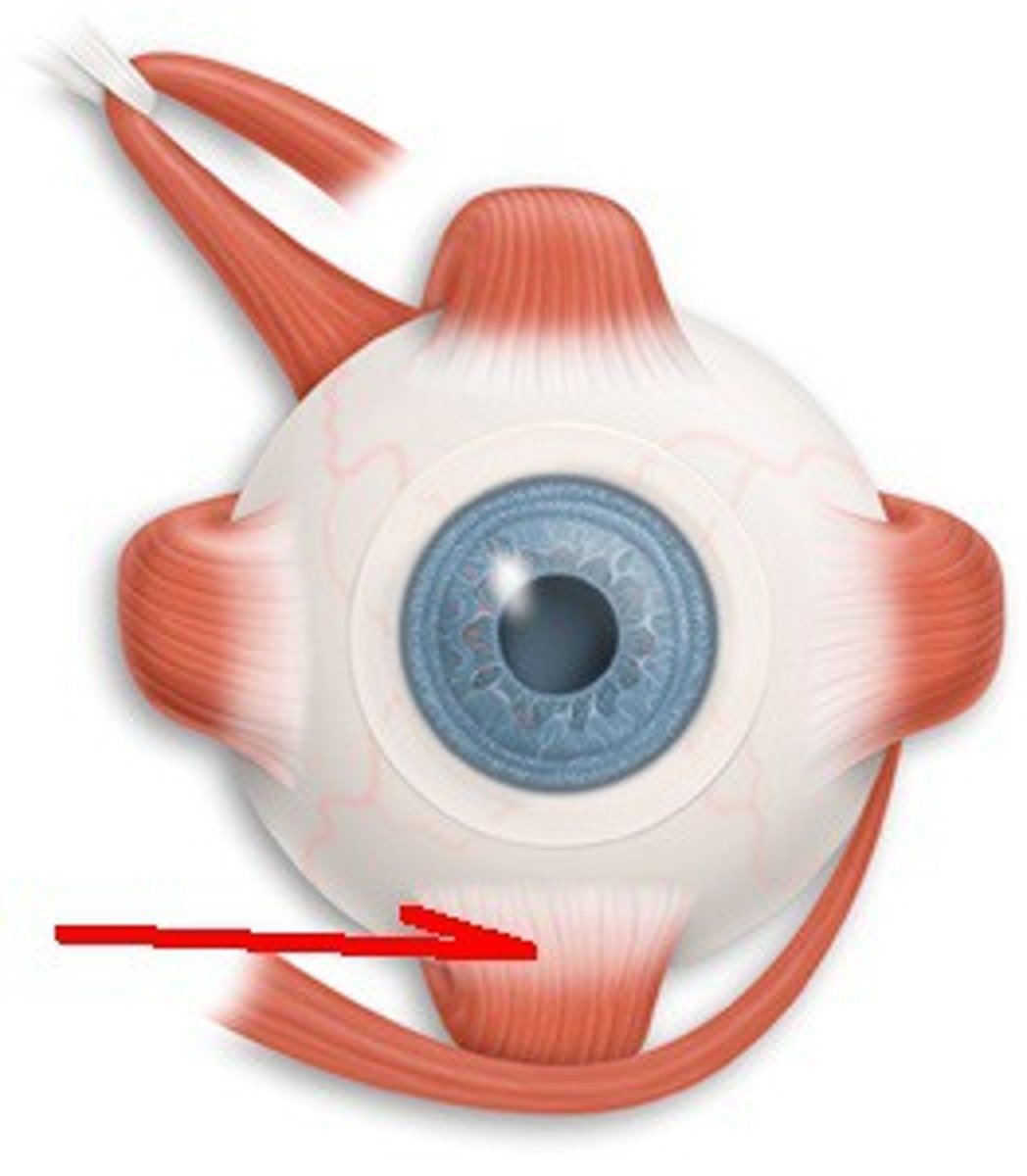
Superior Oblique
primary: intorsion
secondary: depression abduction
Cranial Nerve 4
Inferior oblique
primary: extorsion
secondary: elevation and abduction
Cranial Nerve 3
how many cranial nerves relate to the eye?
6
extraocular motilities
access the ability to perform conjugate eye movements
EOM instructions
follow the light with your eyes without moving your head. Tell me if you ever see two lights instead of one or if you feel any pain or discomfort
EOM procedure
-glasses off and transilluminator
start with light on primary gaze, move to 6 other positions in an H pattern
Observe smoothness, accuracy, fullness, and extent of movements
EOM recording
Normal:
FROM (full range of motion)
SAFE (smooth, accurate, full, extensive)
USA (unrestricted, smooth, accurate)
reported for each eye
abnormal:
describe the abnormality
and which eye
-diplopia upper right gaze
-pain OD on left gaze
-50% restriction on downgaze OD
Near point convergence
subjective and objective assessment of the ability to converge
NPC setup
habitual near correction, target 1-2 lines larger than best corrected VA of worse-seeing eye, near lamp on target
NPC instructions
follow the target and keep it clear and single. Let me know if the target ever splits into two
NPC procedure
move the target toward the patient and observe their eyes
move the target away from the patient and observe their eyes.
break
distance at which the patient reports diplopia or at which you observe one eye lose fixation
recovery
distance at which the deviated eye regains fixations or at which the patient reports regaining single vision
recording NPC
record correction, break/recovery distances and eye that deviated (leave blank if diplopia)
normal:
NPC (cc) 4cm/7cm OS out
NPC (sc) 5cm/7cm diplopic response
NPC TTN
Abnormal NPC
break/recovery worse than 5cm/7cm
Saccades
quick eye movements from one fixation point to another
pursuits
smooth eye movements that involve following or tracking a moving target
purpose of saccade and pursuits
assess the quality of refixation and smooth eye movements