All equations and Conversions (from RxPrep Formula Sheet)
1/135
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
136 Terms
1 tsp = ? mL
5 mL
1 tbsp = ? mL
15 mL
1 fl oz = ? mL
30 mL (29.5 ml/fl oz)
1 cup = ___ oz
8 oz
1 pint = ? oz = ? mL
16 oz, 473 mL (2 cups)
1 quart = ? pints
2 pints (32 oz, 4 cups)
1 gallon = ? quarts
4 quarts (3840 mL)
1 kg = ? lbs
2.2 lbs
1 oz = ? g
28.4 g
1 pound = ? g
454 g
1 grain = ? mg
65 mg (64.8 mg exact)
K+, Na+, monovalent ions: 1 mEq = ? mmol
1 mEq = 1 mmol (for monovalent ions)
Ca++, divalent ions: 1 mEq = ? mmol
1 mEq = 0.5 mmol (for divalent ions)
Weight in volume (%w/v)
X g/100 mL
volume in volume (% v/v)
X mL/100 mL
weight in weight (% w/w)
X g/100 g
NS w/v
0.9 g/100 mL
Ration strength -> % strength
% strength = 100/ratio strength
Ex: 1:2500 to % strength
% strength = 100/2500= 0.04%
% strength -> ratio strength
Ratio strength = 100 / % strength
Ex: 0.04% to ratio strength
ratio strength = 100/0.04 = 2500, so 1:2500
PPM to percentage strength
Move decimal left 4 places
Ex: 2.2 PPM = 0.00022%
Percent strength to PPM
Move the decimal right 4 places
Ex: 0.00022% = 2.2 PPM
Specific gravity equation
SG = g/mL
When to use C1V1 vs alligation
C1V1: use with 2 concentrations
Alligation: use with 3 concentrations
1 gallon = ? mL (approx)
3840 mL
1 quart = ? mL
960 mL
1 pint = ? mL
480 mL
1 cup = ? mL
240 mL
Osmolarity
the concentration of a solution expressed as the total number of solute particles per liter.
Osmolality
A measure of the number of particles per kilogram of water
How many particles does sodium acetate disassociate into?
2
How many particles does magnesium sulfate disassociate into?
2
How many particles does calcium chloride disassociate into?
3
How many particles does sodium citrate disassociate into?
4
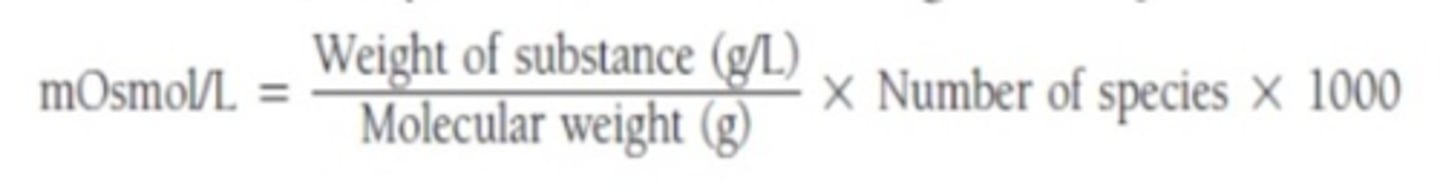
Osmolarity Equation (mOsmol/L)
mOsmol/L = (weight (g/L)/MW (g/mol)) x # particles x 1000
1) add up the number of disassociation particles
2) Calculate # of g in 1L
3) use MW to solve the problem
Always normalize to 1 L (miliosmoles don't do this)
If there are multiple things in solution, solve for the mOsmol of each separately then add together at the end (see page 143, #53 of book for example)
E value equation
E = 58.5 (i) / MW of drug (1.8)
*multiply the E-value of a number times the amount of that product to see the amount of sodium chloride represented from that product
(1) calc how much NaCl will come from the sodium product (NS, 1/2NS)
(2) calc how much product you will need then multiply it times the E value; this gives you the sodium equivalent of the product
(3) subtract product equivalent to NaCl from amt NaCl needed for isotonicity
Dissociation (i) factors (based on # of dissociation ions)
1 ion: i = 1
2 ions: i = 1.8
3 ions: i = 2.6
4 ions: i = 3.4
5 ions: i = 4.2
Mol equation
mols = g/MW
mmol equation
mmol = mg/MW
mEq equation
mEq = (mg x valence)/MW
or
mEq = mmol x valence
(so basically the equation for mmol but multiplied by valence)
Valence is the charge associated, so KCl has a valence of 1 b/c K and Cl only have 1 charge. Ca (Ca++) has a valence of 2 because it has a 2+ charge
Molecules with a valence of 2
Ca carbonate
Ca chloride
Ferrous sulfate
Magnesium sulfate
(these are a lot of the same drugs that chelate)
KCl mEq to percent strength conversion
KCl 10% = 20 mEq/15 mL
After how many days of being unable to absorb enteral nutrition is parenteral nutrition considered?
> 5 days of inadequate absorption
2-in-1 vs 3-in-1 TPN
2-in-1: Dextrose and protein
3-in-1: Dextrose, protein, and lipid
Estimated BEE
15-25 mg/kg (adults)
Dextrose monohydrate provides _____ kcal/g
3.4 kcal/g
Amino acid solutions provide _____ kcal/g
4 kcal/g
10% lipid emulsion provides ___ kcal/ml
1.1 kcal/mL
20% lipid emulsion provides ___ kcal/ml
2 kcal/mL
30% lipid emulsion provides ___ kcal/mL
3 kcal/mL
Enteral dextrose and protein provide ____ kcal/g
4 kcal/g
Enteral lipids provide ____ kcal/g
9 kcal/g
1 gram of Nitogen = ____ g of protein
1 g Nitrogen = 6.25 g protein
(e.g. for every 6.25 g of protein given to a patient, it will be broken down into 1 g of Nitrogen)
Calculate the number of grams of protein given then divide by 6.25 to find g of N
Non-protein to nitrogen ratio
First calculate g of Nitrogen (1 g N = 6.25 g protein)
Then divide total non-protein calories by g of N
Equation for fluid needs
Fluids needed = 1500 mL + 20mL (# kg over 20 kg)
Estimate using 30-40 mL/kg/day
Total Energy Expenditure (TEE) equation
BEE x activity factor x stress factor
Aminosyn, FreAmine, Clinisol
Amino acid solutions for TPN
What filter do lipids require?
1.2 micron filter
What are some medications that provide fat calories when infused?
Propofol
Clevidipine
Formulations of sodium that can be added to a TPN
Sodium Chloride
Sodium Acetate
Sodium Phosphate
What formulation of sodium should be added if a patient is acidotic?
Sodium acetate (converted to bicarb and can help)
Formualations of K that can be used in TPN
KCl
KPO4
K acetate
How to reduce risk of percipitation with Ca and Ph
1) use Calcium gluconate instead of CaCl (less reactive, lower risk of percipitation due to lower dissociation constant with Ca gluconate)
2) Add phosphorus first after dextrose and amino acids, then add everything else except Ca, agitate, and then add Ca to give it the largest volume to disperse in
3) Keep refrigerated until use (keeps dissociation of ions low)
4) Keep total Ca and Ph below 45 mEq/mL
What type of insulin is given in TPN?
Regular insulin
How to prevent drug and enteral feeding interactions
Hold feeding one hour before and 2 hours after the drug is administered
How long should enteral tube feeds be separated from warfarin?
Hold feeding for 1 hour before and 1 hour after administration of warfarin
How do levothyroxine, quinolones and tetracyclines interact with enteral tube feeds?
Chelate, seperate administration
What formulations of ciprofloxacin are and are not used for enteral tube feeding?
Cipro oral solution is NOT used because it adheres to the tube
Use IR tablets crushed and mixed in water instead
Flush line with water before and after administration
How should phenytoin be separated from enteral tube feeds?
Seperate feeds by 2 hours before and 2 hours after phenytoin
BMI equation
BMI = weight (kg) / height (m^2)
OR
BMI = (weight (lbs)/height (inches^2)) x 703
BMI classifications
underweight: <18.5
normal: 18.5-24.9
overweight: 25-29.9
obese: >30
IBW equation for women
IBW = 45.5 + 2.3 * (inches over 5 feet)
IBW equation for men
IBW = 50 + 2.3 * (inches over 5 feet)
Adjusted Body Weight Equation
AdjBW= IBW + 0.4 (TBW-IBW)
If a patient's TBW < IBW what dosing weight should be used?
TBW (for all medications)
If a patient's TBW is about equal to IBW (< 120% of IBW), which dosing weight should be used?
TBW for most medications
What medications only use IBW for dosing, unless TBW is < IBW?
Aminophylline
Theophylline
Acyclovir
Levothyroxine
(most narrow therapeutic index drugs use IBW for dosing to minimize risk of toxicity in normal weight and obese patients)
What dosing weight is used for LMWH, UFH and vacomycin if TWB is ≥ 120% IBW?
TBW (basically, always use TBW for these)
What dosing weight is used for aminoglycosides if TBW is ≥ 120% IBW?
AdjBW
CrCl equation
CrCl (mL/min) = (140 - age)(weight) / ([SCr](72))
x 0.85 if female
When calculating CrCl, if TBW < IBW, what weight should be used?
TBW
When calculating CrCl, if TBW is about equal to IBW, what weight should be used?
IBW
When calculating CrCl, if someone is overweight or obese (TBW > IBW) what weight should be used?
Depends on BMI:
BMI < 25: use IBW
BMI > 25: use AdjBW
pH < 7.35
acidosis
pH > 7.45
alkalosis
What BUN:SCr ratio indicates dehydration?
> 20:1
pCO2 range
35-45 mmHg
HCO3 range
22-26 mEq/L
Anion gap equation
AG = Na - Cl - HCO3
Causes of gap acidosis (CUTE DIMPLES)
Cyanide
Uremia
Toluene
Ethanol
Diabetic ketoacidosis
Isoniazid
Methanol
Propylene Glycol
Lactic acidosis
Ethylene Glycol
Salicylates
What does it mean when pH = pKa
It means that 50% of the drug is ionized and 50% of the drug is nonionized.
pH > pKa
More of the acid is ionized
pH < pKa
More of the acid is un-ionized
Differences in characteristics of an ionized vs. non-ionized drug
Ionized: more soluble but cannot cross lipid membranes
Non-ionzied: not soluble but can cross membranes to reach receptor site
Are most drugs weak acids or weak bases?
Weak acids
Weak acid formula
pH = pKa + log (salt/acid)
Weak base formula
pH = pKa + log (base/salt)
(flip the fraction from weak acid formula)
How much elemental calcium is in calcium carbonate?
40%
How much elemental calcium is in calcium citrate?
21%
How should calcium carbonate be taken?
Take with food (acid dependent absoprtion)
How should calcium citrate be taken?
With or without food (acid independent absorption)