Pharmacology Exam #1 Study Guide
1/75
Earn XP
Description and Tags
*NOTE - if the content is highlighted in red or the flashcard has a 🛑 - THAT MEANS SHE EMPHASIZED WE NEED TO KNOW THE INFORMATION FOR THE EXAM.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
76 Terms
🛑Rights of medication administration: Right drug
Must check the name of the drug ___ times: (list all of the times)
Right drug - must check the name of the drug 3 times - at the medical administration record, while drawing up the medication, and again at bedside before giving it to the patient. Don’t forget to ask the patient if they have any allergies or have had a prior allergic reaction to that medication in the past.
🛑Rights of medication administration: Right dose
If the nurse is unfamiliar with the normal dose of that medication that should be given, what should she do?
Right dose - become familiar with the dosing, or cross reference with a book or the EHR
🛑Rights of medication administration: Right time
Why is knowing whether this is the right time important? What can the nurse do if she believes it is too soon for the medication to be given?
Right time - some drugs need to reach a therapeutic level to be able to work well on the receptor.
NURSE CAN HOLD OFF ON GIVING A MEDICATION - Just because it is scheduled for 2 pm does not mean that it needs to be given at that time - if the toxicity level is too high, then it should not be given as it can harm the patient. Toxicity can be checked with labs for example.
🛑Rights of medication administration: Right route
Importance of knowing the right route. What can be done if the route needs to be changed?
Right route - know that it is the right route for the patient.
For example - if a patient has been ordered a PO medication but they have AMS/fatigue/dysphagia/etc then the route might need to be changed. ((i think call pharmacy to see if there is another route that the drug can be given and then if there is - call provider and ask to change the order))
🛑Rights of medication administration: Right patient
How many identifiers will the nurse use to confirm the patient’s identity (+examples)? How can you double check this information?
Right patient - use 2 identifiers such as name and DOB, double check their ID band. Make sure to check the med order against their ID band by scanning it and making sure that they match.
🛑Rights of medication administration: Right documentation
What information should be documented?
Right documentation - We document the date, time, route, dose, site of administration.
🛑Rights of medication administration: Right reason or indication
Explain importance of knowing right reason for giving the medication.
Right reason or indication - We need to know why the meds are being given.
For example - if a patient has a headache and the provider orders Tylenol, but then they develop a fever - the Tylenol can only be given for the headache and the provider must be notified about the fever as they will need to determine what the underlying cause of it is.
🛑Rights of medication administration: Right response
Things to assess for when trying to determine whether the patient is having the desired response?
Right response - ensure the patient is responding well to the medication - in terms of the therapeutic effects (is the patient’s problem improving with the medication), in terms of the side effects and adverse effects (are they experiencing any and how severe are they?)
🛑Rights of medication administration: Right to refuse
At which point is the patient allowed to refuse treatment? What things should the nurse need to keep in mind when the patient decides to refuse a medication?
Right to refuse - need to inform the patient that they are allowed to refuse the medication at any time- but we need to ensure that they are sound of mind - meaning they are able to make the right decision
🛑ENTERAL drugs
How are these drugs given?
Describe pass effect and bioavailability with respect to enteral drugs.
ENTERAL - mouth and GI
Drugs given orally, sublingual (however, this one goes directly into the bloodstream since there are many blood vessels under the tongue and thus bypasses the ‘first pass effect’ - but because it is considered PO it is considered enteral), buccal, rectal and vaginal (but can also be considered topical).
This will first undergo ‘first pass effect’ - meaning it will go though the liver to be metabolized (AKA break down the drug into its active components) so the drug can have its active effect on the target tissue.
Another way to define it is the processing of that drug by the liver.
Bioavailability is the amount of the drug that is available when it reaches the target tissue/organ after the first pass effect of an ENTERAL drug.
Not all drugs have high bioavailability -for example Bactrim has 100% bioavailability, vancomycin has 0% bioavailability.
This means that Bactim, when taking ENTERAL it will have 100% of the drug reaching the target tissue/organ after it has been metabolized by the liver.
Vancomycin, when taking ENTERAL will have 0% reaching the drug after it has been processed by the liver.
🛑PARENTERAL
How are these drugs given?
Describe pass effect and bioavailability with respect to parenteral drugs.
PARENTERAL - into the bloodstream
Drugs given IV, IM, SUBQ, ID, intraarterial, intrathecal, intraarticular (directly into the joints)
These do not need to go through the liver (AKA no need for first pass effect) as it goes directly into the bloodstream
PARENTERAL drugs will always have 100% bioavailability since they are administered directly into the bloodstream
TOPICAL
How are these drugs given?
TOPICAL - through the skin
Drugs to the skin including transdermal patches (PARENTERAL), ointments (messier but more effective), gels, creams (less effective because they are water based, but often preferred by patients)
🛑DISTRIBUTION (protein bound drugs)
What does it mean when a medication is protein bound?
What is the most abundant protein in plasma?
What is the main function of this protein?
What happens if it is low - especially in regards to what happens when taking protein bound medication?
What happens when the protein bound drug enters the bloodstream?
What happens as the free flowing drug in the bloodstream decreases?
Some medications are protein bound when they get into the bloodstream - meaning they use the proteins in your plasma to travel through the bloodstream and reach the target tissue/organs.
Albumin is the most abundant protein in plasma, it helps hold water within the blood vessels (if low, then water leaks and this leads to edema).
When protein-bound drugs enter the bloodstream, they will mainly bind to albumin (as it is the most abundant) and be carried to the target tissue/organ. The remaining drug will stay in the bloodstream ready to be metabolized.
Eventually as the free flowing drug in the body decreases (bc it has been metabolized) then some of the bound drug (to albumin) will unbind and get released into the bloodstream to continue being metabolized.
If a patient has low albumin levels, they will have extra medication in the bloodstream - meaning more effect which can lead to higher drug toxicity.
🛑 What are the 3 medications that should NOT be crushed?
Extended release - d/t being a higher dose and it dissolves slowly - this is used to reduce amount of time per day that medication is taken.
Coated - meds can be coated for a purpose such as taste masking, protecting med from moisture, or facilitating swallowing. Enteric coated - the coating is designed to resist the acidic environment of the stomach and dissolve in the alkaline environment of the intestines - ensuring the medication is released at a specific location in the GI tract - this coating is used for meds that may cause irritation to the stomach lining or that need to be absorbed by the intestine for optimal effectiveness. Coated or enteric coated medication should not be crushed as they are designed to release the active ingredient in a controlled manner and crushing them will affect their safety and efficacy which can lead to pt having adverse effects or treatment failure.
What is pharmacokinetics?
Pharmacokinetics is the study of what the body does to the drug - the way the drug moves through the body, and the body’s effect to the drug.
🛑What is the major site of drug metabolism in the body?
The liver.
🛑What is the primary organ responsible for excretion of most drugs?
The kidney.
Fun fact (but not for the exam) - some drugs can also be excreted through biliary or bowel excretion (this is not as important for the exam as understanding importance of kidney/renal function)
🛑What is loading dose?
Loading dose - some drugs will need to be given a high dose first to be able to reach a therapeutic effect and then give maintenance (lower dose).
🛑What is pharmacotherapeutics?
Using the drug to treat the patient, and the cellular changes that happen.
(IMPORTANT🛑) - Why this drug - why are you choosing the drug for this patient ?
Is this - acute therapy? Maintenance therapy? Supplemental or replacement therapy? (supplement something the body does not produce on its own), Palliative? Supportive therapy? (like blood products or IV fluids), Prophylactic? (like prophy abx or anti epileptics prior to surg) Empiric therapy? (when suspect the patient to have something but it is not yet proven and you give meds - example is empiric abx after pt presenting with infection signs but we don't have the cultures back)
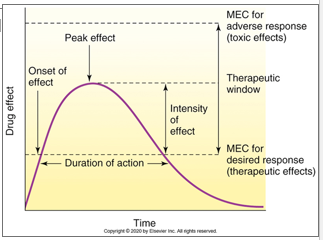
Describe peak and trough of a drug.
Peak level is the highest blood level of a drug.
Trough level is the lowest blood level of a drug.
Describe therapeutic window and range of a drug.
Therapeutic window - it is the dosage range between a minimum effective therapeutic concentration and the minimum toxic concentration.
Therapeutic range - the dosage range or blood plasma concentration usually expected to achieve the desired therapeutic effect.
Toxicity table.
Toxicity occurs if the peak blood level of the drug is too high.
What is half life? How does it affect drug administration?
Half life is the time required for 50% of the drug to be removed from the body.
Knowing half life is important because this determines how often the medication needs to be given.
🛑What is teratogenic effect?
When medications cause congenital disorders in developing embryo or fetus. This usually occurs in early pregnancy (first trimester).
Example - needing to sign iPledge before starting Accutane.
What is carcinogenic effect?
It is when a medication directly causes cancer.
Example - some chemotherapies.
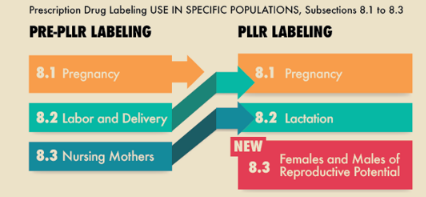
🛑 What are the different drug categories in pregnancy? - per old FDA rules
Which one is safest? Which one is most contraindicated?
Category A - Studies indicate no risk to human fetus. (SAFEST)
Category B - Studies indicate no risk to the animal fetus, information for humans is not available.
Category C - Adverse effects reported in the animal fetus, information for humans is not available.
Category D - Possible fetal risk in humans has been reported; however, in selected cases consideration of the potential benefit versus risk may warrant sue of these drugs in pregnant women.
Category X - Fetal abnormalities have been reported, and positive evidence of fetal risk in humans is available from animal and/or human studies. These drugs are not to be used in pregnant women. (MOST CONTRAINDICATED)
What are the different drug categories in pregnancy? - per new FDA rules
*discusses risk to pregnant woman and breastfeeding mother
What is black box warning and its subcategories? (Scheduled drugs)
List schedule number, abuse potential, medical use, and dependency potential for each.
Black-box warning is seen in meds where there is a reasonable possibility of serious adverse effects or death.
Class-I: HIGH abuse potential - no medical use - severe physical and psychological dependency potential. (HIGHEST WARNING)
Class-II: HIGH abuse potential - accepted medical use - severe physical and psychological dependency potential.
Class-III: LESS THAN C-II abuse potential - accepted medical use - moderate to low physical and psychological dependency potential.
Class-IV: LESS THAN C-III abuse potential - accepted medical use - limited physical and psychological dependency potential.
Class-V: LESS THAN C-IV abuse potential - accepted medical use - limited physical and psychological dependency potential.
🛑Medication errors - how to prevent and reporting of medical errors
Preventing - I don’t feel like typing all that.
Reporting of medical errors - Notify the patient per the institution’s protocol ,assess they are doing well after error is made. Report to prescriber and nursing management and document error per policy and protocols.
What is medication reconciliation and why is it important? When will the nurse reconcile medications for a patient?
what is it?
Medication reconciliation is when the nurse verifies, clarifies, and reconciles the list of medications of a patient - including prescriptions, OTC medications, supplements, etc.
importance -
Having an updated list is important in order to ensure that if the patient is having any symptoms that it may/may not be related to the things they are taking. it is also important for knowing any potential interactions if being prescribed a new medication.
when is it done
Upon admission, before patient is transferred to another unit
🛑Older adult physiologic changes
Cardiovascular system:
Increased/decreased CO = increased/decreased absorption and distribution
Increased/decreased blood flow = Increased/decreased absorption and distribution
**** Their heart might not be working as well so they can have decreased cardiac output and blood flow and thus in absorption and distribution of meds.
Cardiovascular system
Decreased CO = decreased absorption and distribution
decreased blood flow = decreased absorption and distribution
🛑Older adult physiologic changes
GI
Increased/decreased pH = altered absorption
Increased/decreased peristalsis = fast/delayed gastric emptying
GI
Increased pH = altered absorption
Decreased peristalsis = delayed gastric emptying
🛑Older adult physiologic changes
Hepatic
Increased/decreased enzyme production = Increased/decreased metabolism
Increased/decreased blood flow = Increased/decreased metabolism
Hepatic
decreased enzyme production = decreased metabolism
*LESS PRODUCTION OF PROTEINS - DRUG BOUND PROTEINS ARE UNBOUND NOW WHICH LEADS TO INCREASED TOXICITY.
decreased blood flow = decreased metabolism
🛑Older adult physiologic changes
Renal
Increased/decreased blood flow = Increased/decreased excretion
Increased/decreased function = Increased/decreased excretion
Increased/decreased glomerular filtration rate = Increased/decreased excretion
Renal
decreased blood flow = decreased excretion
decreased function = decreased excretion
decreased glomerular filtration rate = decreased excretion
*DECREASED GFR MEANS DRUGS ARE CLEARED LESS EFFECTIVELY.
🛑Cultural Assessment - Cultural Considerations
Health benefits and practices -what is the goal?
Language spoken
Past use of medicine
Herbal treatments, folk remedies, and home remedies
Usual response to illness
Responsiveness to medical treatment
Religious practice and beliefs
Support from the pt’s cultural community
Dietary habits
Health benefits and practices - goal is to build trust with the patient
Barriers to adequate health care for the culturally diverse U.S. patient population
◦Language, pride, and beliefs regarding medical practices
◦Medications may have a different meaning to different cultures.
Language spoken
Consider the use of an interpreter if needed.
The patient needs to understand you
Past uses of medicine
Historically - what have been their past use of medicine?
Herbal treatments, folk remedies, and home remedies
Consider that others might have different ways of treatments and all of those things are important to consider when caring for them.
Ask: Tell me what you take at home? - that includes OTC drugs, supplements, teas, and any of the remedies mentioned above - they can affect the presentation of their symptoms of interfere with current medication.
Usual response to illness
Responsiveness to medical treatment
Religious practice and beliefs
Important for when considering treatment types for the patients and measures of care (like do they accept blood?)
Support from the patients cultural community
Dietary habits (certain foods can interact with meds)
🛑Patient Centered Care: Cultural Implications -
Cultural group - African
Consider:
Common health benefits and alternative healers
Verbal and nonverbal communications; touch/time
Family
Biologic variations
Common health benefits and alternative healers: Practice folk medicine, employ “root doctors” as healers (use herbs, roots, potions, and spells), spiritualists. Use herbs, oils, and roots.
Verbal and nonverbal communications; touch/time: Asking personal questions of someone met for the first time is seen as intrusive and not proper. Direct eye contact seen as rude and are present oriented.
Family: Have close, extended family ties; women play important key role in making health care decisions.
Biologic variations: Keloid formation, sickle cell anemia, lactose intolerance, skin color
🛑Patient Centered Care: Cultural Implications -
Cultural group - Asian
Consider:
Common health benefits and alternative healers
Verbal and nonverbal communications; touch/time
Family
Biologic variations
Common health benefits and alternative healers: Believe in traditional medicine, hot and cold foods, herbs/teas/soups; use of acupuncturist, acupressurist, and herbalist. Tai Chi, QiGong (exercises)
Verbal and nonverbal communications; touch/time: High respect for others, especially individuals in positions of authority. Not usually comfortable with customs of shaking hands with those of opposite sex. Present oriented.
Family: Have close extended family ties; family’s more important than individual needs.
Biologic variations: Many drug interactions, lactose intolerance, skin color, thalassemia (inherited blood disorder where the body doesn’t make enough Hgb)
🛑Patient Centered Care: Cultural Implications -
Cultural group - Hispanic
Consider:
Common health benefits and alternative healers
Verbal and nonverbal communications; touch/time
Family
Biologic variations
Common health benefits and alternative healers: View health as a result of good luck and living right; see illness as a result of doing a bad deed. Heat, cold, and herbs used as remedies. Use curandero, spiritualist.
Verbal and nonverbal communications; touch/time: Expressing negative feelings is seen as impolite. Avoiding eye contact is seen as respectful and attentive; touching acceptable between two persons in conversation.
Family: Have close extended family ties; all family members involved in healthcare decisions. Past cultural experiences in the family with illness and healing practices hold significant value. Strong adherence to cultural practices.
Biologic variations: Lactose intolerance, skin color.
🛑Patient Centered Care: Cultural Implications -
Cultural group - Native American
Consider:
Common health benefits and alternative healers
Verbal and nonverbal communications; touch/time
Family
Biologic variations
Common health benefits and alternative healers: Believe in harmony with nature and ill spirits causing disease; use medicine man (spiritual healer)
Verbal and nonverbal communications; touch/time: Speak in low tone of voice, light touch of a person’s hands is preferred versus a firm handshake as a greeting. Present oriented.
Family: Have close extended family ties; emphasis on family.
Biologic variations: Lactose intolerance; skin color, cleft uvula problems.
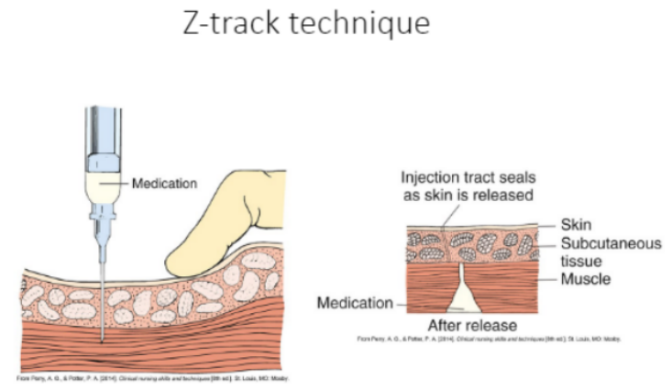
Administering: Intramuscular (IM) medications
Needles used
Amount of medication that can be given.
Angle used.
Special considerations.
Needles used: 18-21 gauge
Amount of medication that can be given: 3 mL is the max
Angle used: 90 degrees
Special considerations:
Technique: Z track technique - prevents med from leaking through the tissue as it can be irritating
PER BOOK - We insert the needle aspirate - if you see blood then do not inject, draw the needle and then go in again. (WHY? because you do not want to give the medication in the bloodstream, you want to give it intramuscularly).
PER CDC - you do not aspirate for self admin, or vaccines.
Administering: Intradermal (ID) medications
Needles used
Amount of medication that can be given.
Angle used.
Special considerations.
Needles used: 25-27 gauge
Amount of medication that can be given: 0.1 mL max
Angle used: 15 degrees
Special considerations: N/A
Administering: Subcutaneous (SUBQ) medications
Needles used
Amount of medication that can be given.
Angle used.
Special considerations.
Needles used: 25-27 gauge
Amount of medication that can be given: 0.5-1 mL max
Angle used: 45 degrees, if patient has a lot of adipose tissue then 90 degrees
Special considerations:
Examples are insulin and heparin. If injecting a blood thinner - DO NOT MASSAGE AREA as it can cause bruising.
Location of medication is a nursing intervention - meaning it is up to the nurse.
Administering: Insulin
For insulin do you use mL or units?
How to mix insulins (which one do you draw first and which one second)
Use units when measuring amount of insulin, not mLs.
When drawing insulin - if using the same syringe - draw clear first then cloudy
Check compatibility before mixing!!
🛑OPIOID ANALGESICS
What are they? where do they bind? what does this binding cause?
Types
Multimodal medications - what is it?
MOA
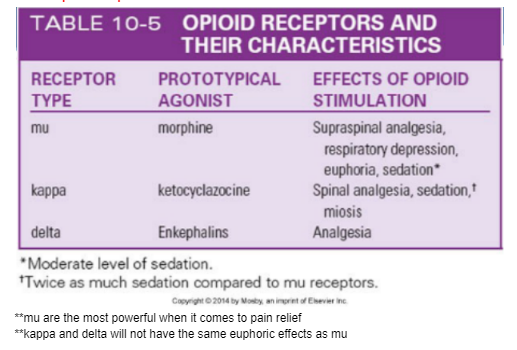
Opioid MOA - how many types of receptors are there? what do they do?
Indications
Side effects
Reversal
Nursing implications - remember what to assess before and after and what to monitor for, and what to do if patient’s condition or VS worsens after taking the medication.
What are they?
Opioid drugs - synthetic drugs that bind to opiate receptors to relieve pain - VERY STRONG pain relievers.
Types - Painkillers, opioid analgesics, adjuvant analgesic drugs (meds not primarily designed to control pain but can be used for this purpose).
Multimodal medications - use of more than one pharmacological class of analgesic medication targeting different receptors along the pain pathway with the goal of improving analgesia while reducing individual class-related side effects.
MOA
Opioid drugs - bind to opiate receptors to relieve pain.
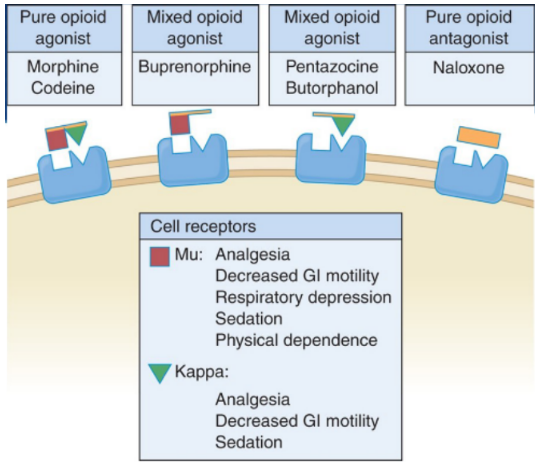
They have 3 receptors (SEE PICTURE)
mu - most powerful when it comes to pain relief
kappa and delta will not have the same euphoric effect as mu
Indications:
Opioids - used for acute p/op pain, CA pain, and severe pain.
Fentanyl patch - only give to pts with chronic pain who have used a lot of drugs (CA pts, etc) - not for opioid naive (acute pain)
Side effects:
OPIOID adverse effects: CNS depression (which leads to respiratory depression, it is the most serious AE), n/v, urinary retention, diaphoresis and flushing, pupil constriction (miosis), constipation (Constipation is a common AE - try to prevent with adequate fluid and fiber intake), itching
Reversal: naloxone (Narcan) and naltrexone (ReVia)
Narcan - blocks opioid receptor completely, if suspect opioid overdose and pt has resp depression - we can give it. Pt will go into withdrawal (anxiety, irritability, chills and hot flashes, lacrimation, rhinorrhea, diaphoresis, n/v, abdominal cramps, diarrhea, confusion) which can be uncomfortable but at least they will be breathing.
Nursing implications: Before giving opioids, make sure you know VS.
Oral forms should be taken with food to minimize gastric upset.
Ensure safety measures, such as keeping side rails up.
Withhold dose and contact physician if decline in patient’s condition or VS, RR <10-12 bmp, may need Narcan.
Instruct patients to follow directions for administration carefully and to keep a record of their pain experience and response to treatments.
Change positions slowly to prevent orthostatic hypotension.
Assess bowel sounds before administration.
🛑 Agonis vs Partial Agonists vs Antagonist
Agonists - where do they bind? What type of response does that binding cause?
Partial agonist - where do they bind? What type of response does that binding cause? When can this be used for a patient?
Antagonist - What do they do?
Agonists
Bind to opioid pain receptor in the brain - cause analgesic response (reduction of pain sensation)
All come down to morphine -
Partial Agonist/Mixed Agonist/Agonist-Antagonist
Bind to pain receptor
Cause weaker neurologic response than full agonist
Can use these when trying to help a patient wean down if they are addicted to opioids
Antagonists
Reverse effects of these drugs in pain receptors (competitive antagonists)
Example - naloxone
🛑Non-pharmacologic pain control
Physical method like hot/cold therapy
Massage, touch
Therapeutic communication
Relaxation
Distraction
Coping skills training
Cognitive behavioral therapy
Transcutaneous electrical nerve stimulation (TENS) - uses low-voltage electrical currents to relieve pain. A TENS unit is a small device that delivers the current at or near your nerves to block or change your perception of pain
Acupuncture
PT/Yoga/PEt therapy/ musci mindful meditation/ imagery
ACETAMINOPHEN (TYLENOL)
MOA
Indications
Side effects
Main organ of concern
Reversal agent
Maximum daily dose
Nursing implication (ie teaching and monitoring)
ACETAMINOPHEN (TYLENOL)
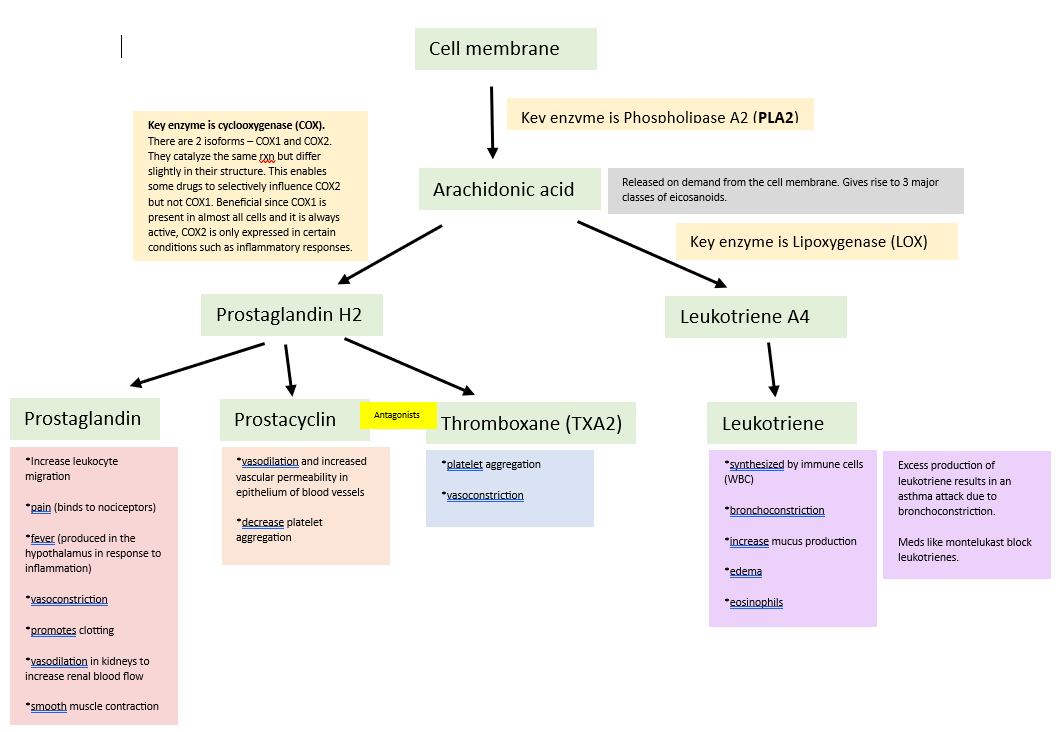
MOA: Stops the production of prostaglandins (the ones that tell your body to feel pain or give you a fever). It mainly does its job in the brain (CNS), meaning it tells your brain to stop making those pain and fever signals.
Acetaminophen has little to no real anti-inflammatory effects (it is considered an anti-inflammatory because it blocks prostaglandin synthesis - but it does not block the inflammatory cascade - the arachidonic acid stuff)
It provides analgesia and has antipyretic effect (reduce fever).
Indications:
Mild to moderate pain
Fever
Alternative to aspirin/NSAID products
Adjunct pain reliever
Side effects: Generally well tolerated.
Possible adverse effects include skin disorders, nausea, vomiting.
Less common - effects of blood disorders, nephrotoxicities, and hepatotoxicity (most serious).
Main organ of concern: Liver
Reversal agent (antidote): Acetylcysteine (Mucomyst)
Maximum daily dose: 3g a day
(if pt has liver disease don’t go over 2g/day)
Nursing implication (ie teaching and monitoring): (*Unclear if this is right*)
Assess the pain level to ensure acetaminophen is appropriate for their needs. Educate patient on purpose, effects, and proper usage. Monitor patient closely for any adverse reactions or side effects - including VS, liver function tests if necessary.
What are NSAIDS?
They are large and chemically diverse group of drugs with the following properties:
Analgesic
Anti-inflammatory
Antipyreptic
Aspirin-platelet inhibition
NSAID Review
Main NSAIDS discussed in class
MOA
Which ones work more on COX2 and what is the benefit and main problem of this
Indications
Main side effects
GI
Kidney
Cardiac
Who can’t take NSAIDs?
Organ of concern
Signs of toxicity
Nursing implication and teaching to the patients
Main NSAIDS discussed in class
MOA: inhibiting leukotriene pathway, prostaglandin pathway, or both. Blocking chemical activity of COX
Which ones work more on COX2 and what is the benefit and main problem of this
One that works more on COX2 is Celebrex
Benefit of blocking COX2: it is only expressed in certain conditions like inflammatory responses (whereas COX1 is only expressed in almost all cells and it is always active)
Problem - then COX1 can become more enhanced
Indications: Mild to moderate headaches, myalgia, neuralgia, arthralgia, alleviation of p/op pain, relief of pain associated with arthritic disorders like RA, juvenile arthritis, ankylosing spondylitis, and osteoarthritis. Treatment of gout and hyperuricemia.
Main side effects:
GI: dyspepsia (discomfort in upper abdomen), heartburn, epigastric distress, nausea. GI bleeding (because of blocking blood flow to the gut - damage to the linng of the GI - can cause GI bleeding GI upset), mucosal lesions.
Renal: reduction in creatinine clearance, acute tubular necrosis with renal failure(Kidney not getting enough blood flow leads to reduction in creatinine clearance - it is a reflection of glomerular filtration rate - if the kidney isn’t clearing it is not working)
CV: noncardiogenic pulmonary edema (the noncardiogenic pulmonary edema - not heart related but more so of the fluid accumulation and it is more than the heart can handle - SUPER IMPROTANT - pts with cardiac history cannot be on a whole class of medications (NSAIDs) )
Organ of concern: GI, Renal, and CV
Signs of toxicity: n/v, HA, drowsiness, blurry vision, dizziness. Seizures rarely documented (from the internet)
Nursing implication and teaching to the patients: Assess for conditions that may be contraindications to therapy like GI lesions, peptic ulcer disease, bleeding disorders. labs like cardiac, renal, LFT, CBC, plt count). Educate patients about the various adverse effects of NSAIDs and inform them to notify their prescriber if the effects become severe or GI pain occurs. Inform that enteric-coated tablets should not be crushed or chewed.
What is malignant hyperthermia? How would a patient with it present?
It is a genetic condition. Associated with administration of general anesthetics - symptoms will include
high temp
muscle rigidity (uncontrolled release of intracellular Ca which causes the muscles to contract)
What is a neuromuscular blocking drug (NMBD)?
What does it do?
Does it provide analgesia or sedation?
Can the patient breathe on their own after receiving this medication?
What is the nursing implication of this?
What does it do? They prevent nerve transmission in skeletal and smooth muscle, resulting in muscle paralysis.
Does it provide analgesia or sedation? No, they are strictly paralytic
Can the patient breathe on their own after receiving this medication? No, it causes muscle paralysis of the diaphragm and intercoastal muscles which are needed to breathe.
What is the nursing implication of this?
Always assess past history of surgeries and response to anesthesia.
Assess past history of allergies, and medications.
Assess use of alcohol, illicit drugs, and opioids.
Succinylcholine
MOA
Side effects -
Indications
Nursing Implications
Black box warning
Succinylcholine - a depolarizing neuromuscular blocking drug
MOA - binds to Ach receptors at neuromuscular joints, depolarizes receptors which cause Na channels to open = membrane polarizes (pt will have fasciculations followed by flaccid paralysis) = prevents repolarization from happening.
Side effects -
Indications - used mainly to facilitate controlled ventilation during surgical procedures - short acting (used with rapid sequence intubation). Also used to reduce muscle contraction in an area that needs surgery. Can also be used to diagnose MG.
Nursing Implications: Assess pass SHx and response to anesthesia, h/o allergies and meds, and use of alcohol, illicit drugs, and opioids. Assess VS, labwork, O2 stat, etc. Watch for sudden elevations in body temperature, which may indicate malignant hyperthermia.
Black box warning: Contraindicated in patients with personal or familial history of malignant hyperthermia and/or skeletal muscle myopathy. There have been rare reports of ventricular dysrhythmias and fatal cardiac arrest secondary to rhabdomyolysis with hyperkalemia, primarily in healthy-appearing pediatric patients who were subsequently found to have undiagnosed skeletal muscle myopathy, most frequently Duchenne’s muscular dystrophy.
General anesthetics, effects
What are they, MOA
What are their effect
What do IV anesthetics do? are they short or long acting?
General anesthetics - inhalation or IV
Block flow of Na+ into neurons, delay nerve impulses and reduce neural activity
Exact mechanism unknown but likely activate GABA receptors in the brain
They produce unconsciousness, lack of responsiveness to painful stimuli.
They can decrease metabolic rate, feeling cold, gut shuts down,
Some patients can be more sensitive to the anesthesia than others
What do IV anesthetics do? are they short or long acting?
All IV anesthetics are - induce consciousness, used in combo with inhalation agents - anesthesia and muscle relaxation - balance anesthesia (multiple modalities)
IV anesthetics can be short acting - procedures that are 15 mins or less
Triptans (for migraines)
MOA
Triptans - second line therapies for migraines (first is NSAIDS)
Examples Maxalt & Imitrex (Abortive treatment)
Stimulate 5-HT-1 cerebral arteries, causing vasoconstriction and reducing headache symptoms. They also reduce the production of inflammatory neuropeptides.
Benzos (Diazepam, lorazepam)
MOA
Indications
Adverse effects
Reversal agent
Nursing implications
Benzos (Diazepam, lorazepam) - most commonly prescribed sedative-hypnotic drug. Classified as either sedatives or hypnotic and antianxiety.
MOA - depress CNS activity in the brain. Facilitate the binding of the inhibitory neurotransmitter GABA at various receptors throughout the CNS = calming effect. (not restful sleep because they interfere with REM sleep)
Indications:
3 S = for sedation (moderate conscious sedation), sleep induction, skeletal muscle relaxation.
Balanced anesthesia
Anxiety relief (if pt has severe anxiety attack which constitutes as an medical emergency - it acts quickly), alcohol withdrawal, agitation relief
Treatment of acute seizures especially status epilepticus,
Adverse effects: Drowsy, dizziness, cognitive impairment, respiratory impairment (with overdose or drug interaction), lethargy, fall hazard for older patients, can have hangover effect the next day - daytime sleepiness.
Reversal agent: Flumazenil
Giving someone this medication can actually cause them to go into withdrawal which can lead to higher anxiety, seizure activity which can be dangerous. So in real life, we don’t use this anymore, we use supportive care.
Nursing implications: Monitor adverse effects, safety (side rails up, keep call light within reach, etc), most benzodiazepines cause REM rebound and a tired feeling the next day; use with caution in the elderly, instruct pts to avoid alcohol and CNS depressants.
🛑 Salicylate toxicity: signs/symptoms
CV ___ HR
Pulm broncho____
CNS: ear, eyes, cognitive, triangle
GI - classic
Metabolic: acidosis/alkalosis, how it affects breathing? __other stuff
Toxicities of salicylate
Cardiovascular - increased HR
Pulmonary - bronchoconstriction
Central nervous - tinnitus, HL, dimness of vision, HA, dizziness, mental confusion, lassitude, drowsiness
GI - n/v/d
Metabolic: metabolic acidosis, sweating, thirst, hyperventilation, hypoglycemia or hyperglycemia
FYI - Salicylates are NSAIDS - example aspirin , inhibit COX1 and COX2. Do not give to children d/t risk of Reye’s syndrome.
Barbiturates (Phenobarbital mainly)
MOA
Indications
Adverse effects
Toxicities
Nursing implications -
**Remember, this medication is an enzyme inducer, what does this mean?
Barbiturates (Phenobarbital mainly) - oldest sedating drug, can be very toxic very quickly.
MOA: They are potentiating GABA inhibition (meaning this promotes a calming effect of the nervous system), they are less selective than benzos which means can have more respiratory depression.
Indications: Sedatives (less likely), Anticonvulsants (if patient has refractory seizures (aka drug resistant epilepsy), status epilepticus, then barb can be used), Anesthesia for surgical procedures(more likely)
Adverse effects: Dependence, drowsiness, hypotension, respiratory depression, low plt count, hypersensitivity reaction like SJS, lack of restful sleep (interferes with REM sleep) which can lead to agitation and inability to deal with normal stress.
- Can cause rebound headaches (like exedrin -)
Toxicities: - at high doses it can have hypnotic effects and lower RR and can even lead to respiratory arrest. Overdose can produce CNS depression (sleep to coma and death)
Nursing implications -
**Remember, this medication is an enzyme inducer, what does this mean? This means that they stimulate the action of enzymes in the liver that are responsible for metabolism or breakdown of many drugs. By stimulating the action of these enzymes, they cause many drugs to be metabolized more quickly, which usually shortens their duration of action.
🛑What are anticonvulsants or antiepileptic drugs? What is the goal of therapy?
AEDs - they help prevent seizures while maintaining QOL. They work by stabilizing the electrical activity in the brain, thereby reducing the likelihood of abnormal excessive firing of neurons that can lead to seizures.
Might need more than one agent to get control
Pts with true epilepsy it is a lifelong dx = meds forever
Hydantoins family:
Phenytoin (Dilantin)
MOA
Indications
Therapeutic effect
Adverse effects
General
What happens if phenytoin is given IM or the IV infiltrates?
If given IM
If given IV
How should this med be mixed and what tubing?
How fast to give?
Signs of Toxicity —
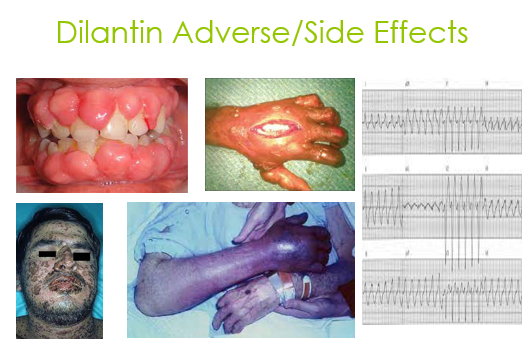
Hydantoins family - prototype drug is Dilantin
Phenytoin (Dilantin)
MOA: Desensitize Na channels. It is a protein bound drug - meaning it is highly bound to protein (albumin). ((If patient has low albumin then this can lead to toxicity)).
Indications: Effective for most seizure types (except absence seizures), has anti-dysrhythmic properties. CAN BE GIVEN PO OR IV
Therapeutic effect (remember): Narrow therapeutic window of 10-20 mcg/mL. Toxicity happens over 20.
Adverse effects:
Has anti-dysrhythmic properties. If given too quickly, it can make the patient hypotensive. Can cause SJS. Can cause oversedation, gingival hyperplasia (interferes with collagen and causes inflammation), can cause excessive hair growth in face?
IM - it can cause irritation in the skin leading to tissue necrosis.
IV: We can only give it with saline (as opposed to D5W - which is 5% dextrose with water) as it can precipitate and crystalize.
It needs to be a slow infusion as it can lower BP if given too quickly.
If it leaks into the nearby tissue, it can kill your hand (tissue necrosis) = purple glove
How should this med be mixed and what tubing?
Should be given with normal saline, mixed slowly and carefully to avoid precipitation.
Type of tubing - use line filter with pore size of 0.22 micrometers - this filter helps trap any potential particles or precipitates that may form during the mixing process, ensuring that only the dissolved medication reaches the patient's bloodstream.
How fast to give?
Depends, but slow infusion.
Signs of toxicity?
Fosphenytoin (Celebryx)
How is Phenytoin (Dilantin) different from Fosphenytoin?
Which one can be given IM?
How is Phenytoin (Dilantin) different from Fosphenytoin?
Fosphenytoin (Celebryx) is a product of phenytoin. (NOT TO BE CONFUSED WITH CELEBREX WHICH IS AN NSAID)
It’s water soluble, meaning it can be given IV with D5W - which is 5% dextrose with water
Can be given IV at a faster rate
Which one can be given IM?
Only fosphenytoin
Valpiroic acid (Depakene)
MOA
Indications
Adverse effects
Therapeutic level
Blood test needed to monitor for AEs
Main organ of concern
Valpiroic acid (Depakene)
MOA: desensitizes Na channels
Indications: Wide range of seizure types like focal, generalized, absence seizures. Also used for bipolar disorder.
Adverse effects: limited CNS depression, visual disturbances, ataxia, vertigo, headache. Additional ones include GI effects, hepatotoxicity, pancreatitis.
Therapeutic level: 50-100 mcg/mL
Blood test needed to monitor for AEs: Monitor LFTs at 2 month intervals
Main organ of concern: Liver- hepatic effects dysfunction possible in first 6 months
Lamotrigine (Lamictal)
MOA
Indications
Adverse effect (main one discussed in class)
Lamotrigine (Lamictal) - FIRST LINE AED
MOA: Blocks voltage gated Na channels in the nerve cells - which are essential for generating an electrical signal.
Indications: Focal and generalized seizures as well as bipolar disorder for mood stabilization.
No need for checking therapeutic levels as toxicity is rate with this med.
Adverse effect (main one discussed in class)- SJS
Medications used for status epilepticus
What is status epilepticus?
What meds are used?
Side effects
Reversal
Status epilepticus - Continuous seizure activity >5 minutes without returning to baseline, can lead to a comma or death. Considered a medical emergency.
What meds are used: Benzodiazepines like diazepam (Valium)
Side effects - drowsiness, dizziness, respiratory depression
Reversal - Flumazenil (Romazicon)
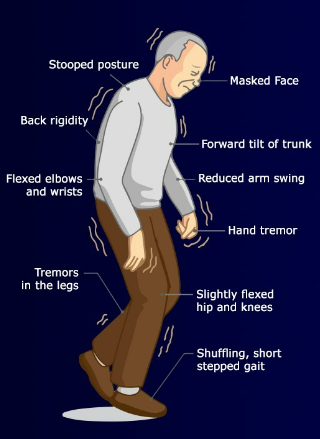
Parkinson’s Disease
What is it?
Signs and symptoms
Goals of pharmacological therapy
PD
What is it? Chronic progressive degenerative disorder that affects the dopamine-producing neurons in the brain leading to low levels of dopamine. Since dopamine and Ach work in conjunction - when dopamine levels are decreased the Ach effects increase which is what causes the symptoms as the dopamine is no longer able to regulate the Ach.
Signs and symptoms: Loss of muscle control, tremors, bradykinesia, rigidity, postural instability, can lead to difficulty swallowing.
Goals of pharmacological therapy: Try to inhibit the breakdown of dopamine.
Carbidopa-Levodopa - prevents breakdown of catecholamines (dopamine) in the CNS, primarily in the brain, which leads to increase in dopamine levels.
Amantadine (Symmetrei) - causes release of dopamine. It was initially found as an antiviral agent for influenza but was seen that it causes a release in dopamine and thus used in the early diagnosis of PD to enhance dopamine on board, usually effective in early course of treatment.
BOTH DRUGS = Usually effective for a short period of time
goal is to improve QOL and extend QOL - pt to be as independent as possible for as long as possible
Benztropine (Cogentin)
MOA
Indications
Side effects
Benztropine (Cogentin)
MOA: Anticholinergic drug used in the treatment of Parkinson’s disease and also of extrapyramidal symptoms from antipsychotic drug (block action of Ach - what does this mean? - helps relieve sx of PD (since low dopamine = higher lvls of Ach))
Indications (remember avoid in elderly): help with tardive dyskinesia and extrapyramidal symptoms - automatic involuntary movements that can occur with lip smacking (these can also occur with pts that are on anti psychotics but also with pts that have PD)
Not a good medication for older patients, usually for younger patients with Parkinson's
Side effects (Think anticholinergic) - tachycardia, confusion, disorientation, toxic psychosis, urinary retention, dry throat, constipation, nausea, and vomiting
Review nursing implications for Parkinson meds
Nursing implication
Perform a thorough assessment, nursing history, and medication history.
Include questions about the patient’s:
CNS
GI and GU tracts
psychologic and emotional status
MAKE SURE U KNOW - goal is to improve QOL and extend QOL - pt to be as independent as possible for as long as possible
Antipsychotics
Adverse effects
Antipsychotics - Treat psychosis delirium schizophrenia (Block dopamine receptors in the brain)
Side effects are:
Neuroleptic malignant syndrome (NMS) - mental status change, rigidity, fever, and dysautonomia (can alter BP, HR, etc)
Myoglobinuria - excess amount of myoglobin in the urine (can indicate damage of the cell membranes of myocytes)
Extrapyramidal symptoms - sx include various motion disorders similar to those seen in PD
Tardive dyskinesia - repetitive, involuntary movements, such as grimacing and eye blinking.
Selective serotonin reuptake inhibitors (SSRI)
Side effects
Main concern when putting a patient on an SSRI
Risk for serotonin syndrome- when can it occur? and how does it present?
Can feel too heightened (from my notes)
Anxiety, dizziness, drowsiness, headache, mild GI disturbance, sexual dysfunction, asthenia (weakness, lack of energy and strength), tremor (from the book).
If pt is on SSRI - concerned for suicide
If pt was very depressed in the past but now they have a boost of energy with SSRIs, they can now have enough energy to plan to kill themselves
Risk for serotonin syndrome (if toxicity)
Increased BP, HR
Delirium
Agitation
Sweating
Myoclonus (brief involuntary twitching or jerking of a muscle)
Hyperreflexia
In any question always prioritize ABCs and safety
Medication to treat extrapyramidal side effects
Anticholinergic and antihistaminergic medications - the one mentioned in class was anticholinergic
Anticholinergic drug like Benztropine (Cogentin)
🛑How to prevent lithium toxicity-nursing teaching interventions
What type of disorders can Lithium be used for?
How does it work? What does it interfere? What lab levels should we keep an eye on?
What is the therapeutic range for lithium?
How can toxicity present?
Lithium is a drug used to treat bipolar disorder - old drug choice for mania.
It works by interfering with the Na ion transport as it uses the same pathway - the exact mechanism is unclear though. But we do need to keep an eye on the Na levels.
It has a very narrow therapeutic range (0.6-1.2 mmol/L - in labwork) - if toxicity occurs it can cause arrhythmias, epilepsy like seizures
🛑 Therapeutic index
Concentration of drug working on the receptors and having good response before reaching toxicity = AKA - concentration of effectiveness between no effect and toxic effect.
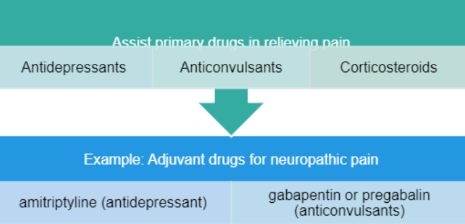
🛑Adjuvant drugs - The way we should be thinking about using pain meds.
Adjuvant drugs can be used to enhance the effects of pain medications, treat concurrent symptoms, and provide analgesia for other types of pain.
Examples (for neuropathic pain)
amitriptyline (antidepressant)
gabapentin or pregabalin (anticonvulsant)
🛑 Neuromuscular blocking drugs - NMBD: Depolarizing vs non-depolarizing (KNOW THE DIFFERENCE)
Depolarizing
MOA - how does it work?
Example drug and what does it do?
Non-Depolarizing
MOA - how does it work?
Drugs that end in -____ ?
Which type is more common?
Which one is short acting? Which one do we use for rapid sequence intubation?
Depolarizing - succinylcholine (for short acting short procedure) is the one we use, use with rapid sequence intubation
Depolarizing succinylcholine - (non competitive) works by binding with Ach receptors at neuromuscular joints - cause Na channels to open membrane depolarizes- then pt will have fascilulations- then flaccid paralysis - prevents repolarization from happening
Non depolarizing - most common, paralyzed for longer periods
They will compete with acetylcholine for cholinergic receptors at neuromuscular junctions, do not depolarize the muscle
Prevent depolarization from happening
Drugs end with -urium
🛑Xanax
Xanax
commonly used anxiolytics - used for Generalized anxiety disorder - short term relief of anxiety symptoms
CNS depression is a common side effect
🛑Ativan
used for seizure activity - first line AED
You can also use diazepam, midazolam to stop seizure activity
🛑 Monoamine oxidase inhibitors (MAOIs) and Tyramine
Use: Treatment of major depressive disorder, atypical depression, Parkinson's disease, and several other disorders
Mechanism of action: Enzyme inhibitor
Ingestion of foods or drinks with tyramine leads to hypertensive crisis, which may lead to cerebral hemorrhage, stroke, coma, or death
Avoid foods that contain tyramine!
Aged, mature cheeses (cheddar, bleu, Swiss)
Smoked, pickled, or aged meats, fish, poultry (herring, sausage, corned beef, salami, pepperoni, paté)
Yeast extracts
Red wines (Chianti, burgundy, sherry, vermouth)
Italian broad beans (fava beans)