II | cardiac output and hemodynamics
1/10
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
11 Terms
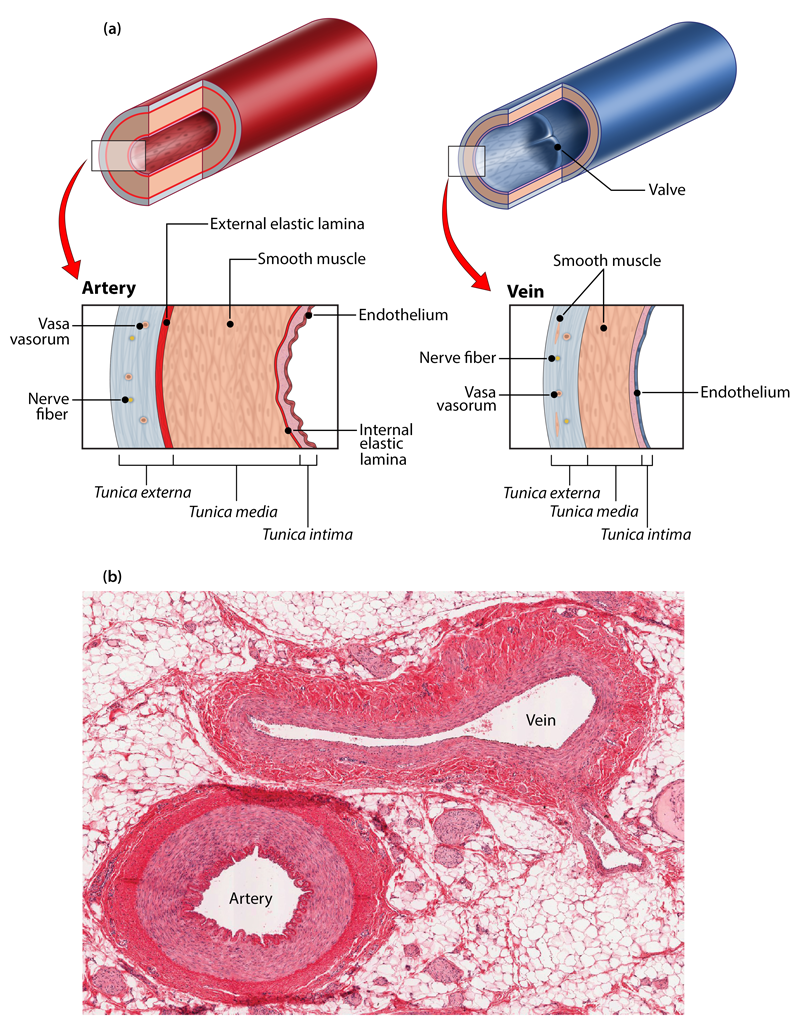
blood vessel structure
endothelium: layer of cells that lines blood vessels and regulates exchanges
smooth muscle: regulates diameter of lumen
elastic fibers: in all 3 layers (tunica externa, media, and intima/interna), recoil moderates pressure changes
arteries vs veins
arteries:
function: carry oxygenates blood
wall: thick, muscular, elastic to withstand high pressure
veins:
function: carry deoxygenated blood
wall: thinner, less muscular, less elastic
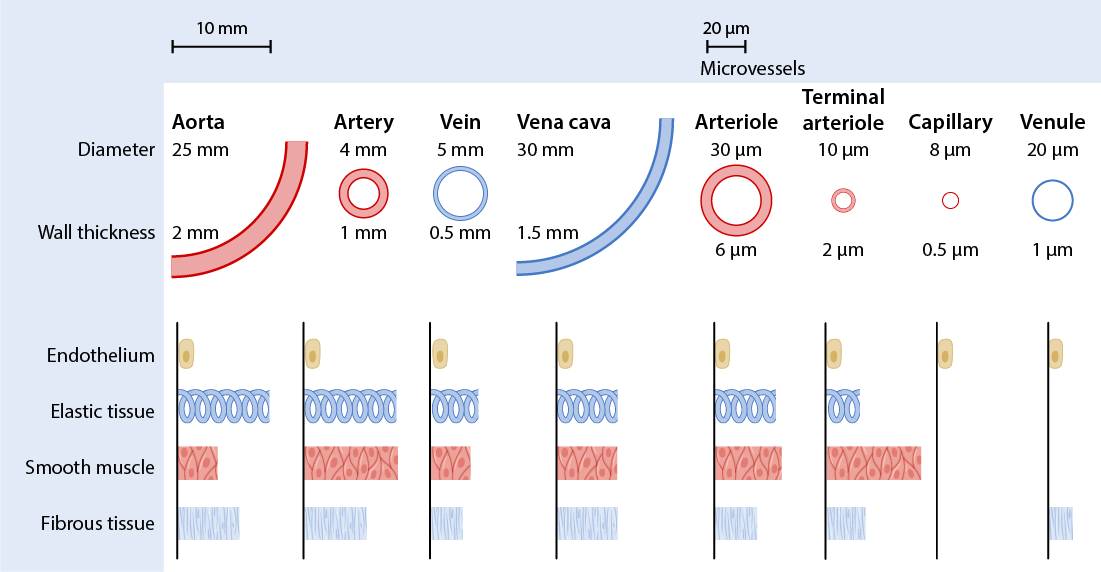
different types of blood vessels
large arteries: carry oxygenated blood away from the heart to various parts of the body
thick, elastic walls
muscular for pressure regulation
ex: aorta, pulmonary arteries
mid-sized arteries: distribute blood to specific regions and organs
muscular walls, less elastic
connect arteries to arterioles
arterioles: regulate blood flow into capillaries
smaller, muscular vessels
control blood flow via smooth muscle contraction
connect arteries to capillaries
capillaries: facilitate exchange of gases and nutrients with tissues
single-cell layer walls for easy diffusion
small diameter, extensive network
connect arterioles to venules
smallest blood vessel
do NOT contain smooth muscle
venules: connect blood from capillaries
smaller than veins
merge to form larger veins
mid-sized veins: collect blood from venules, transport toward heart
thinner walls compared to arteries
large veins: carry deoxygenated blood back to the heart
thinner walls than arteries
ex: superior and inferior vena cava
hemodynamics
hemodynamics: mechanical and physical forces that determine blood flow
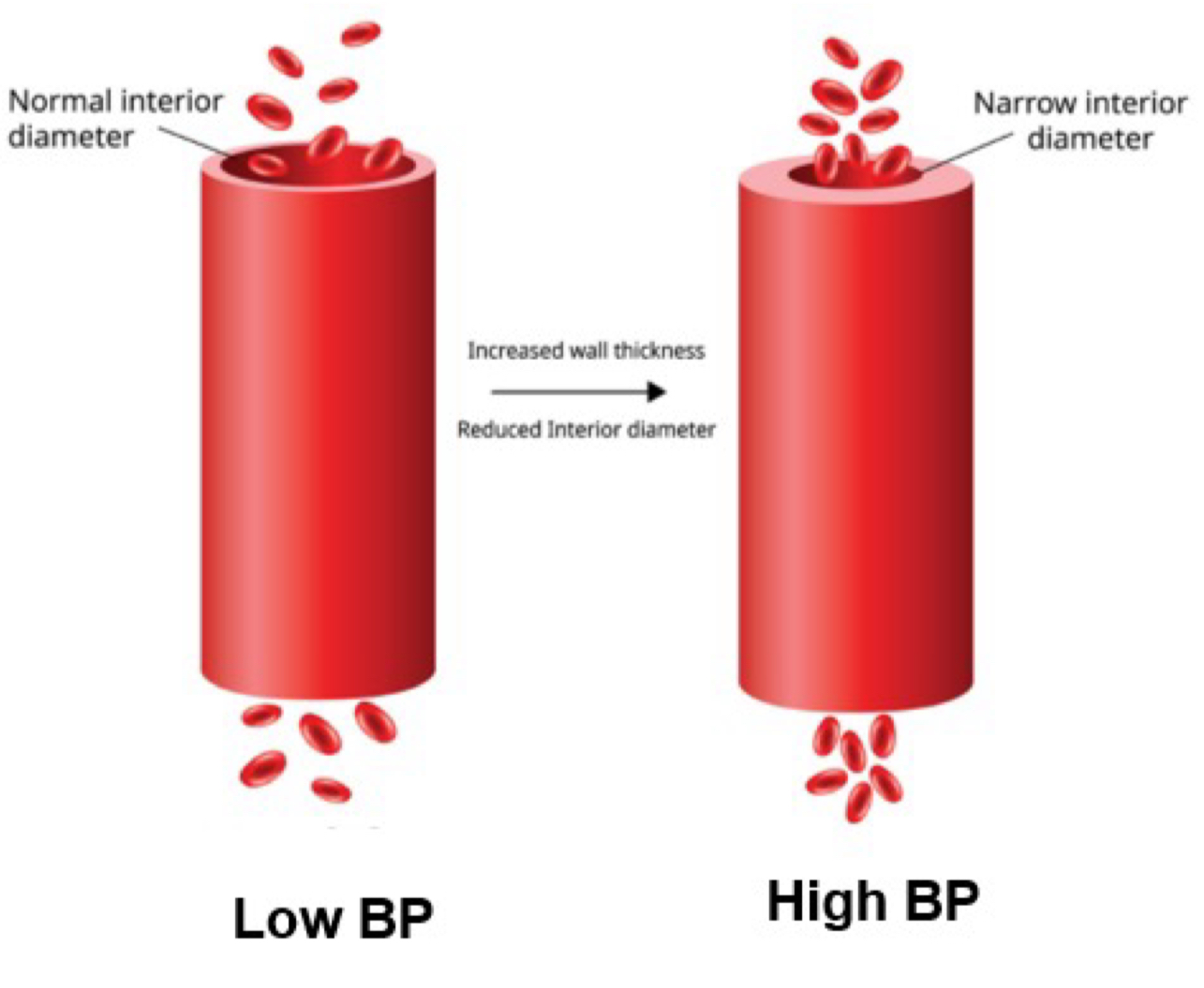
blood pressure
blood pressure (BP): force exerted on a given area of vessel wall by blood (mmHg)
force mainly generated by ventricular contraction
area = diameters of vessel
↑ area (vasodilation) → ↓ resistance → ↓ bp
↓ area (vasoconstriction) → ↑ resistance → ↑ bp
pressure (P) = force / area
pulse pressure - systolic pressure - diastolic pressure
mean arterial pressure (MAP) = diastolic pressure + 1/3 pulse pressure
compliance vs elasticity
compliance: a measure of how easily a structure changes its volume in response to a change in pressure
volume and pressure are inverse
arterial compliance maintains blood flow during systole
accommodates volume changes
elasticity: ability of a blood vessel to expand and recoil (and return back to original state)
arterial elasticity maintains blood flow during diastole
maintains blood flow and pressure
compliance and elasticity are more prominent in aorta and large arteries and are mainly due to vascular elastic fibers
*the aorta and arteries sustain the driving pressure for blood flow during ventricular relaxation to keep blood moving continuously
resistance
resistance: the friction encountered by blood that opposes flow
affected by: radius, viscosity (blood composition), length
resistance opposes flow (as resistance increases flow decreasing)
poiseuille’s law: vascular resistance R = Lη / r 4
L = length of vessel
η = viscosity of blood
r = radius of vessel (vasoconstriction vs vasodilation)
capillary exchange
hydrostatic pressure: physical pressure that fluid exerts on the structures around it (ex: capillary wall)
colloid osmotic pressure: dissolved particles that cannot diffuse across the capillary wall (ex: plasma, proteins) which “pull” water toward them
net filtration pressure = pressures to filtrate - pressures to reabsorb
→ [ capillary hydrostatic pressure (CHP) + interstitial fluid osmotic pressure (IFCOP) ] - [ interstitial fluid hydrostatic pressure (IFHP) + blood colloid osmotic pressure (BCOP) ]
![<p><strong>hydrostatic pressure</strong>: physical pressure that fluid exerts on the structures around it (ex: capillary wall)</p><p><strong>colloid osmotic pressure</strong>: dissolved particles that cannot diffuse across the capillary wall (ex: plasma, proteins) which “pull” water toward them</p><p><em>net filtration pressure = pressures to filtrate - pressures to reabsorb</em></p><p><em>→ [ capillary hydrostatic pressure (CHP) + interstitial fluid osmotic pressure (IFCOP) ] - [ interstitial fluid hydrostatic pressure (IFHP) + blood colloid osmotic pressure (BCOP) ]</em></p>](https://knowt-user-attachments.s3.amazonaws.com/c687cf2d-aa40-4046-896b-51137ff53afb.jpeg)
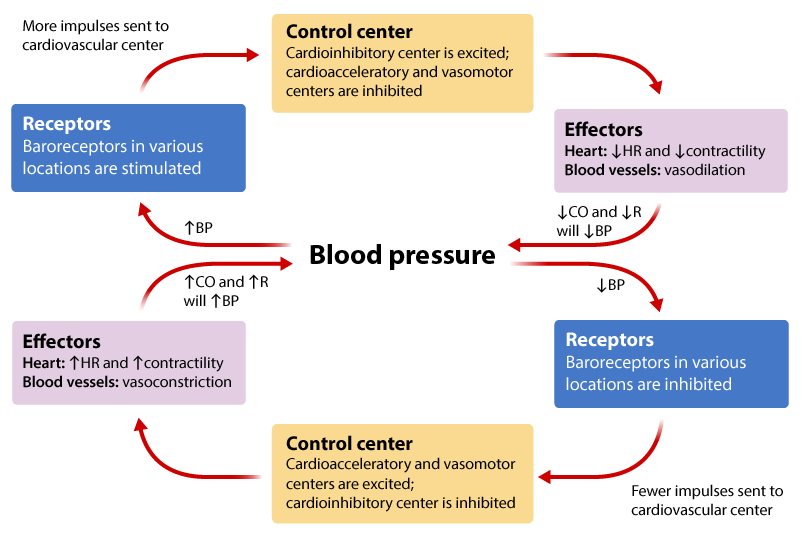
short-term regulation of blood pressure by nervous system
baroreceptors initiate negative feedback mechanisms in response to changes in blood pressure
↑ blood pressure: stimulate various baroreceptors, excite the cardioinhibitory center, inhibit the cardioacceleratory and vasomotor centers, decrease heart rate, and cause vasodilation to ultimately lower blood pressure
↓ blood pressure: baroreceptors are inhibited, exciting the cardioacceleratory and vasomotor centers, inhibiting the cardioinhibitory center, increasing heart rate, and causing vasoconstriction to increase blood pressyre
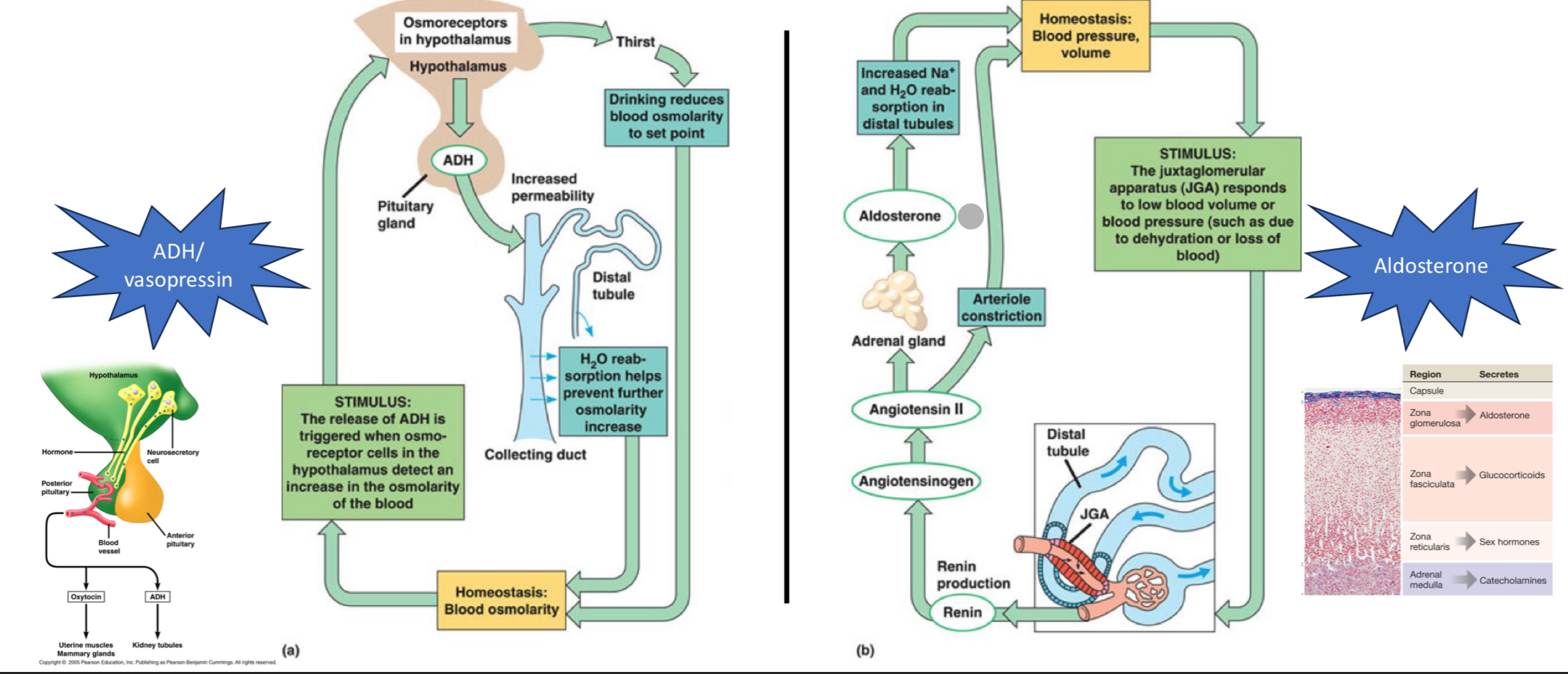
short-term regulation of blood pressure by endocrine system
blood osmolarity: osmoreceptors in hypothalamus detect increase in blood osmolarity → posterior pituitary is stimulated to secrete ADH (aka vasopressin) → ADH binds to receptors in the kidney, stimulates insertion of aquaporins in collecting duct, which increases H2O reabsorption → more water adjusts osmolarity of blood (left image)
juxtaglomerular apparatus (JGA) for low blood volume/pressure: kidney synthesizes, stores, and secretes the enzyme renin → renin converted angiotensinogen to angiotensin II
→ binds to receptors in adrenal gland → stimulates the secretion of aldosterone, which increases Na+ and H2O reabsorption → ↑ blood volume
→ contracts vascular smooth muscle of arterioles → ↑ blood pressure
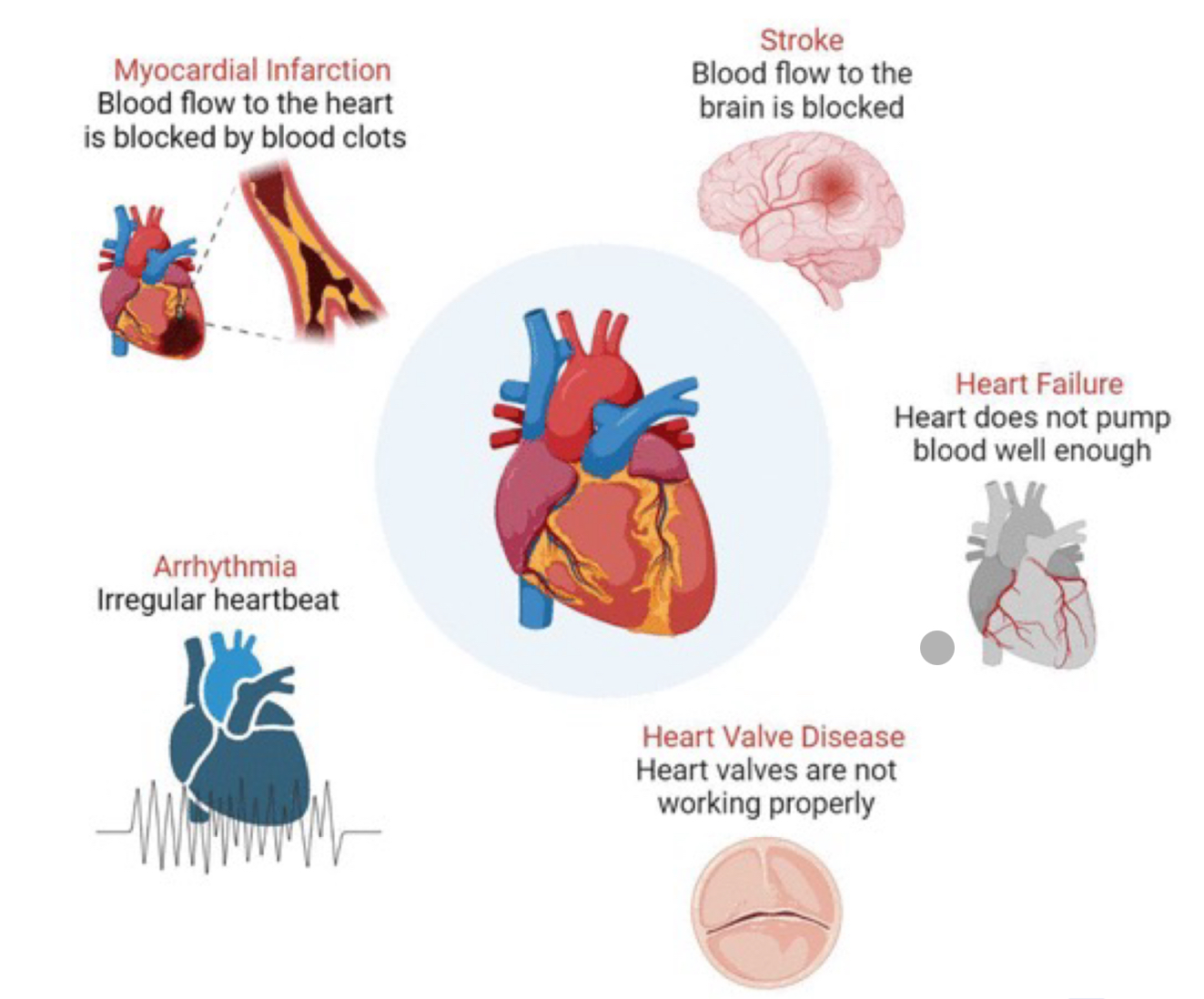
effects of cardiovascular disease and aging on circulation
arterial stiffening (hardening): reduced elasticity of arteries → increased afterload on the heart, contributing to hypertension and impaired blood flow
decreased elasticity of heart tissues: reduced compliance of heart muscle → impaired filling of the heart chambers, potentially leading to heart failure
reduced cardiac output: decline in the heart’s ability to pump blood → decreased blood flow to tissues and organs
valve changes: thickening and stiffening of heart valves → impaired valve function, potentially leading to regurgitation or stenosis
decline in baroreceptor sensitive: reduced responsiveness of baroreceptors in blood vessels → impaired ability to regulate blood pressure in response to changes
increased risk of atrial fibrilation: higher likelihood of irregular heart rhythms → elevated risk of stroke due to blood clot formation