Stage 1 Visit 1 - DR
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
37 Terms
Type 1 diabetes
Auto-immune condition in which cells that produce insulin are destroyed
10% of Px with diabetes have this type
Lifelong treatment with insulin is required to prevent death
Tends to develop before 40 years old and usually in childhood
Requires injections of insulin
Type 2 diabetes
Body stops producing enough insulin for its needs or becomes resistant to the insulin produced
90% of diabetes cases
Lifestyle management (diet and exercise) as is strongly correlated to obesity
Requires oral drugs (tablets) or injections
Symptoms of Diabetes
Urinating more often
Thirst
Tired
Light headed/dizzy
Weight loss
Blurred vision - due to changes in the refractive index of the lens
Percentage of people with diabetes that will develop some DR?
50% of type 1 and 25% of type 2 have some DR
If a Px has diabetes for 20 years almost all type 1 and 66% of type 2 will have DR
What is the leading cause of preventable sight loss?
Diabetes - 5% of all sight loss is related to DED
What does insulin do?
Regulates Blood glucose levels by stimulating glucose uptake from the blood which is stored as glycogen within the liver
What is HbA1c?
Chemical formed when glucose combines with haemoglobin
Blood HbA1c levels are an indirect measure of?
Useful measure Blood glucose levels over a prolonged period - gets rid of any spikes that may alter results
Non Diabetic levels - <36mmol/l
In Diabetes - 48mmol/l is safe
What is the main modifiable risk factor for type 2 diabetes?
Obesity - increases risk of type 2 by 13x for women, 6x for men
Non-modifiable risk factors for DR
Duration of Diabetes - if diagnosed 20 years ago likely to have DR
Ethnicity - Asians and Afro Caribbeans are 2x more likely to develop type 2
Social Deprivation
Gender - 56% men, 44% women
Age
Modifiable Risk Factors of DR
Glycaemia - control of diabetes = less likely to develop DR
Blood Pressure
Lipid levels - manage cholesterol levels = reduce risk of DR
Signs of Microangiopathy (Background) DR
Pericyte loss
Microaneurysms Formation
Increased vascular permeability
Capillary Occlusion
Pre-Proliferative DR
Chronic Retinal Ischaemia - arteriolar perfusion is gradually reduced over months/years - leads to slow cell infarction
Exudation
CWS - sign of Retinal Ischaemia
Intraretinal Microvascular Abnormalities
Venous beading/looping
Signs of significant severe retinal Ischameia
IRMA and Venous beading/looping are reliable
CWS a sign but less reliable for significant ischaemia
Difference between IRMA and neo
Neo sit on top of the retina, IRMA within the retina
IRMA don’t leak
No Exudation = IRMA
Exudation = Neo
What does Chronic Ischaemia release
VEGF - which stimulates angiogenesis and leads to retinal/iris neovascularisation
Due to this = exudation
Pre-proliferative is indicated by
>1 IRMA
Venous beading
Multiple deep dot or blot haemorrhages
Proliferative DR
Presence of NEO + all the signs in pre-prof
VEGF primary driver of neo
Pre-retinal (between ILM and vitreous) and vitreous haemorrhages - urgent referral
Can potentially lead to Vitreo-retinal traction
Black circle = fibrovascular proliferation - forms around NV
Neovascularisation
2 forms;
NVD
NVE - in any of the 4 quadrants
As NV proliferate, fibrous tissue forms around them - acts as scaffolding for developing NV
OCT shows Neovasc that can extend into the vitreous
Vitreo-Retinal tractional detachment
Fibrovascular material can be attached to both the ILM and vitreous
The tension of the new vessels leads to tearing of the vessels which leads to haemorrhaging and elevation of the retina - T RD
Can be relieved by vitrectomy surgery
Diabetic Maculopathy
Can occur at any stage of DR
Involves any of the following around the macula
Microaneurysms
Exudates
Dot and Blot
Oedema - can see with an OCT
How does DMO occur?
Hyperglycaemia induces microvascular pathology
BRB breakdown
Exudation
Release of VEGF
Further increase in vascular permeability
Which layers are the fluid located in DMO
Fluid build up is concentrated in INL and OPL
Fluid forms cysts which increase retinal thickness
Fluid causes disorganisation or retinal layers
Cataract in Diabetes
Cortical and PSC are more common in diabetics and occur earlier in life
50% of type 2 have cataract
Type 1 require surgery 20 years earlier than non-diabetics
Rx changes in Diabetes
Poor glycaemic control changes osmotic pressure within the lens/cornea which changes the refractive index
Most common myopic shift
Can also be hyperopic shift, no proof of astigmatic
Pre-Proliferative DR screening
Likely to be escalated to surveillance clinic - frequent supervision
If Optom suspects; then should initiate their own referral to HES via GP requesting HES opinion within 6/52
Px is not in screening programme or missed their last appt.
Px had recent screening but DR has progressed
Diabetic Maculopathy referral
Slow progression so routine referral
If Px’s VA’s are reducing then refer 1/12
DMO will be treated with anti-VEGF
Proliferative Retinopathy management/referral
Px will be seen by ophthalmologist every 2-3 months
If found Optom should call local HES and explain findings
Urgent Referral - record details of the call on the px record card
Overall management of the different stages of DR
DM px c no DR - one year recall - make sure px is enrolled on screening programme, if not write to GP to be enrolled
Background DR e.g microaneurysms, haemorrhages
Confirm px is on screening programme
if in doubt ask px to contact their local screening programme / GP
Optom should write a letter to GP to confirm
NO REFERRAL to HES
Pre-Proliferative DR - will likely be in surveillance clinic, ensure you ask px when they last had an appt etc. - if not on screening programme refer to HES via GP
DMac - Refer to HES IF PX COMPLAINS OF BLURRED VISION - if vision remains stable no need for referral
Proliferative DR - Urgent referral
Complications of DR e.g Neovasc Glauc, pre-retinal/vitreous haemorrhage - emergency referral
HES management of Diabetic Eye Disease
primary medical intervention is always to try and manage the systemic side of the disease e.g meds + lifestyle changes to bring the glucose levels under control which will reduce the severity of the disease.
What is Laser Photocoagulation Therapy?
laser targetted at retinal tissue causing a small burn (500 microns)
This laser destroys RPE cells alongside the overlying outer retinal layers
e.g PR destroyed which reduces the metabolic demand of the outer layers
Inner retinal layers are able to receive more oxygen supply from the choroid as the outer layers are no longer taking any oxygen
Oxygen supply improved = reduced ischaemia = reduced VEGF production
What is the most common form of LPT and how does it work?
Pan Retinal Photocoagulation (PRP)
1500 closely spaced burns to mid-peripheral retina
Effective but induces permanent retinal scarring
Preserves central vision
Side effects of PRP
Reduced visual field
Reduced night vision
Reduced dark adaptation due to loss of rods
First line treatment for DMO?
anti-VEGF drugs as intravitreal injections
Ranibizumab and Aflibercept - require a central thickness of 400 microns
Less effective the greater the initial VA reduction and the longer the duration of DMO
Other options include intravitreal corticosteroids - supress inflammation e.g Dexamethasone
Does DR affect DV or NV more
Changes results in DV more
Does DM affect DV or NV first
Changes results in NV first
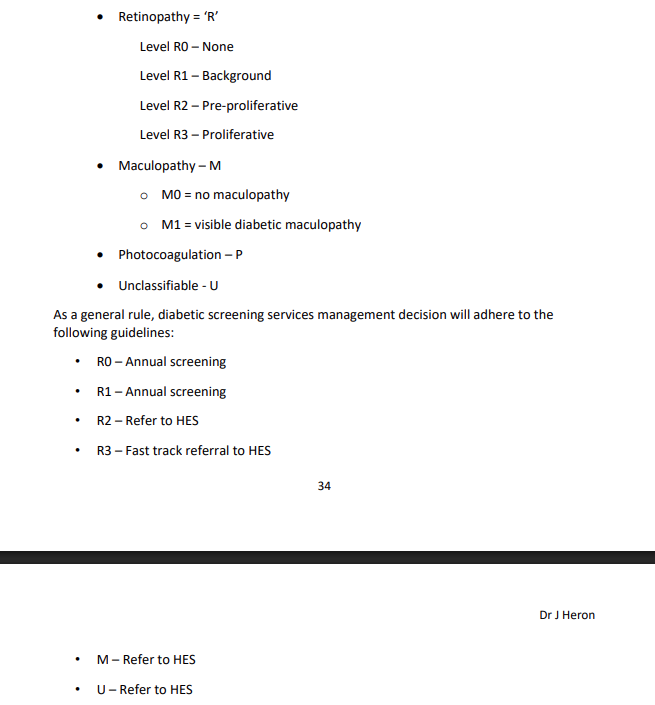
Grading scale