PATH EXAM ONE
1/75
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
76 Terms
common disease of the oral mucosa characterized by the repeated development of one to many discrete, painful ulcers
heal within 7 to 14 days**
3 to 5 mm, round to oval ulcers
with a peripheral rim of erythema and a yellowish adherent exudate centrally.
•the nonkeratinized mobile mucosa of the lips, oral mucosa and tongue margins.
episodes may occur 3–6 times per year. ***
active ulcer: epithelial necrosis w/ fibrinous exudate infiltrated by neutrophils centrally and lymphocytes at the periphery.
Beneath is a layer of granulation tissue with dilated capillaries.
Deeper still is a repair reaction, with fibroblasts forming collagen matrix.
• The etiology is unknown.
—> unknown antige Elevated concentration of pro-inflammatory cytokines
Recurrent aphthous stomatitis (RAS).
AKA canker

rare immune-mediated
small-vessel systemic vasculitis that presents
TRAID: (i) oral ulcers, (ii) genital ulcers, and (iii) uveitis.
• Middle Eastern \ Asain »
-20 and 30 years.
• Painful oral ulcers, indistinguishable from common aphthous ulcers,
-episodes 10* times a year, last 1-4 weeks
unpredictable exacerbations and remissions.
Erythrocyte sedimentation rate, C-reactive protein and peripheral leukocyte counts are elevated.
Histologically:
lesions exhibit leukocytoclastic vasculitis with fibrinoid necrosis,
early perivascular neutrophilic and later lymphocytic infiltrate.
• unknown etiology.
HLA-B51 incr, risk
—————————————————————
notes:
• Genital ulcers:
are similar to oral ulcers in appearance and course.
(men scrotum // women major labori)
• Uveitis (80% of patients)
usually appears 2-3 years after oral/genital ulcers,
recurrent, bilateral, non-granulomatous
mainly: posterior pole.
Posterior uveitis presents with blurred vision and floaters.
Anterior uveitis (pain, redness, and photophobia) is rare. •
Polyarthritis
Behçet syndrome (BS).
all ages, 20-30 years*
female »
associated w/ BRAF mutations**
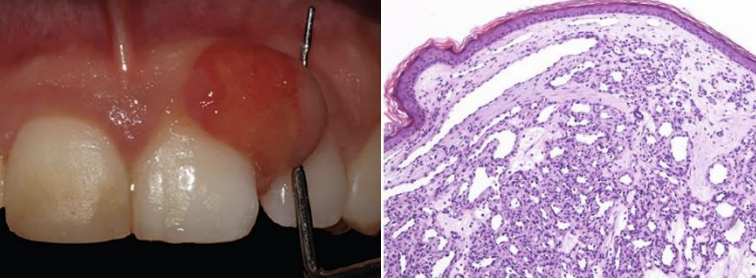
benign vascular tumor of the skin or mucous membranes characterized by rapid growth and friable surface.
prefers: gingiva > > > *
elevated exophytic lesion w/ a red to purple surface**.
pedunculated or sessile soft tissue mass*
grows rapidly over weeks to months —> stabilizes.
bleeds profusely after minor trauma.
Microscopically,
covered at top with thin oral epithelium with variable ulceration.
The tissue underneath the oral epithelium shows
large number of proliferating capillaries,
plump fibroblasts,
and a dense chronic inflammatory cell infiltrate.
resembles granulation tissue.
Oral pyogenic granuloma (PG)
most correct term for PG is capillary lobular hemangioma.
20’s most common, female»
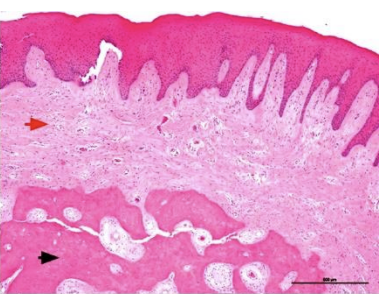
reactive soft tissue growth
mostly loc’d: Anterior maxilla! (interdental papilla).
pedunculated or broad based,
smooth surfaced and shows a pink to red color.**
Microscopically,
stratified squamous epithelium covering an exceedingly cellular mass of connective tissue* w/ plump fibroblasts in between the collagen bundles associated with irregular masses of woven or lamellar bone and cementum-like materials.
etiology unknown: considered to be reactive lesion due to repeated trauma**
Peripheral ossifying fibroma (POF)
age groups, peak: middle-aged females»
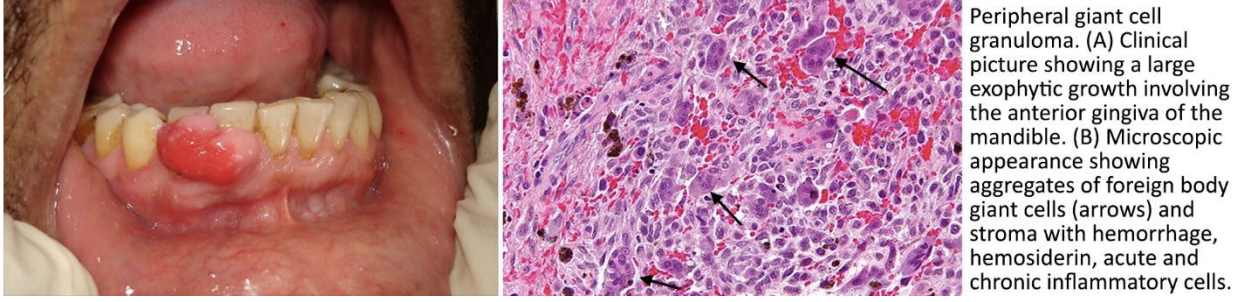
relatively common soft* tissue growth of the oral cavity,
LOC’d: exclusively on interdental gingiva/alveolar crest.*
firm, dark red nodule
sometimes:ulcerated surface,
edentulous alveolar margin, or at the edge of gingiva surrounding the teeth.
vary in size, but rarely exceed 2 cm in diameter.
most of the time is painless
In some cases, the underlying bone suffers erosion.
Histologically,
originates from the periosteum // periodontal membrane
consists of a mass of multinucleated giant cells that stain positively with osteoclast markers
in an active vascular stoma with plump spindle-shaped cells, acute and chronic inflammatory cells, and hemorrhage.
• etiology unknown.
benign neoplasm as KRAS gene mutations (50%)
maybe reactive proliferation of connective tissue as a response to local chronic irritation (implants).
Treatment comprises surgical resection. (low recurrance)
Peripheral giant cell granuloma (PGCG).
aka: giant cell epulis,
(note: similar to Pyogenic Granuloma (PG))
(HSV) are enveloped and have a linear dsdna genome.
(HSV):
HSV-1 vs HSV-2.??
which one causes cold sores
which one causes genital sores
HSV1:
causes herpetic gingivostomatitis
(cold sores at the orolabial region) and herpetic keratitis.
transmitted through contact with oral secretions during asymptomatic shedding (sharing utensils or food).
HSV-2:
genital herpes.
Kids»
Primary HSV-1 infection:
onset: prodrome of fever followed by the appearance of clusters of small, tense vesicles on an erythematous base.
Clusters vary —> may coalesce.
The entire oral mucosa can be affected: the lips, the gingiva, the palate, or the tongue and is associated with submandibular or cervical lymphadenopathy.
Vesicles typically persist for a few days, then rupture and dry, forming a thin, yellowish crust.
Lesions usually heal completely. •
After primary infection, recedes via the sensory nerve into the trigeminal ganglion,(goes latent)****
—> relapsing infections are limited to the lip mucos (herpes labialis).
• Microscopically,
keratinocytes degenerate, lose intercellular connections (acantholysis), and separate
(^forms)—> unilocular blisters.
Several keratinocytes may fuse to produce multinucleated giant cells.
Cowdry type A intranuclear inclusions* form
single, eosinophilic, droplet-like masses surrounded by a clear halo.
The dermis shows edema, inflammatory cellular infiltrate with lymphocytes, neutrophils and eosinophils.
dx: Tzanck test
is prepared by craping the base of a freshly deroofed lesion and smearing the tissue onto a microscope slide;
ID: multinucleated giant cells and intranuclear inclusion bodies.(+ test)
acute herpetic gingivostomatitis
what dx test is this & what is used for ?
is prepared by craping the base of a freshly deroofed lesion and smearing the tissue onto a microscope slide;
ID:
multinucleated giant cells*
intranuclear inclusion bodies.*
= (+ test)
Tzanck test
HSV-1
clinical types
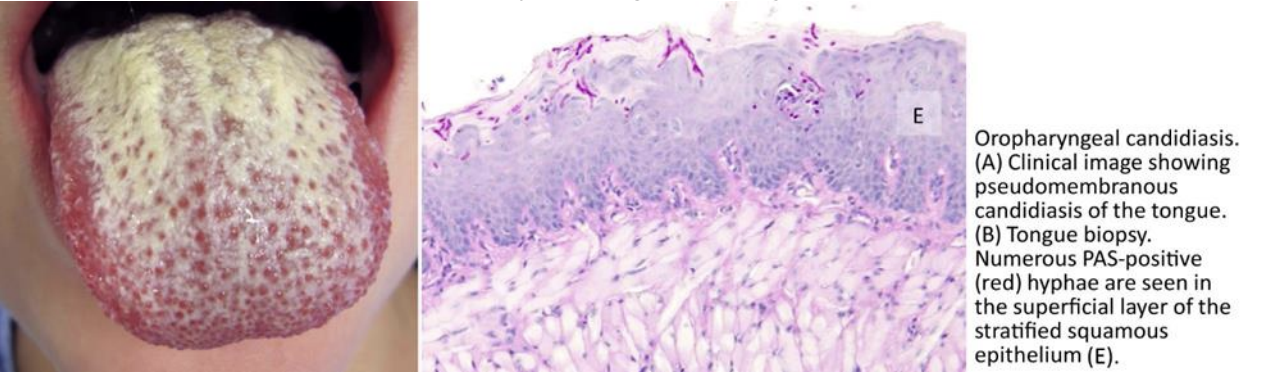
1. ◦ Acute pseudomembranous candidiasis.
most common form — thrush.
an acute infection — coating of the tongue and other oral mucous membranes
by loosely attached: white pseudomembranous plaques —> an underlying erythematous inflammatory base.
(easily scraped off^)
2. ◦ Acute atrophic candidiasis
(erythematous candidiasis)
manifests as painful localized, flat, erythematous areas without plaques*
3. ◦ Chronic hyperplastic candidiasis
(candida leukoplakia)
white patch on the dorsum of the tongue and the commissures of the oral mucosa.
Lesions are non-scrapable*.
distinguishable only by biopsy from other leukoplakias*
4. ◦ Angular cheilitis
occurs as red, fissured lesions in the corners of the mouth.
Fungal elements (pseudohyphae and budding yeasts)
PAS (vivid pink color)
silver methenamine (black color).
+ Gram stain and potassium hydroxide!!
Microscopically,
all forms: + of fungal hyphae & neutrophils
within the squamous epithelium associated with prominent inflammatory infiltrate along the lamina propria.
-opportunistic infection by Candida species.
-considered normal flora in the gi
However, under immunocompromising conditions in forms such as diabetes, smoking, dentures, AIDS, steroid use, malnutrition, vitamin deficiencies, and recent antibiotic use rapid conversion to symptomatic infection may occur.
The immune system is not fully functional at birth and infants are at risk for OPC. •
Oropharyngeal candidiasis (OPC)
-thrush
( most common fungal infection in humans )
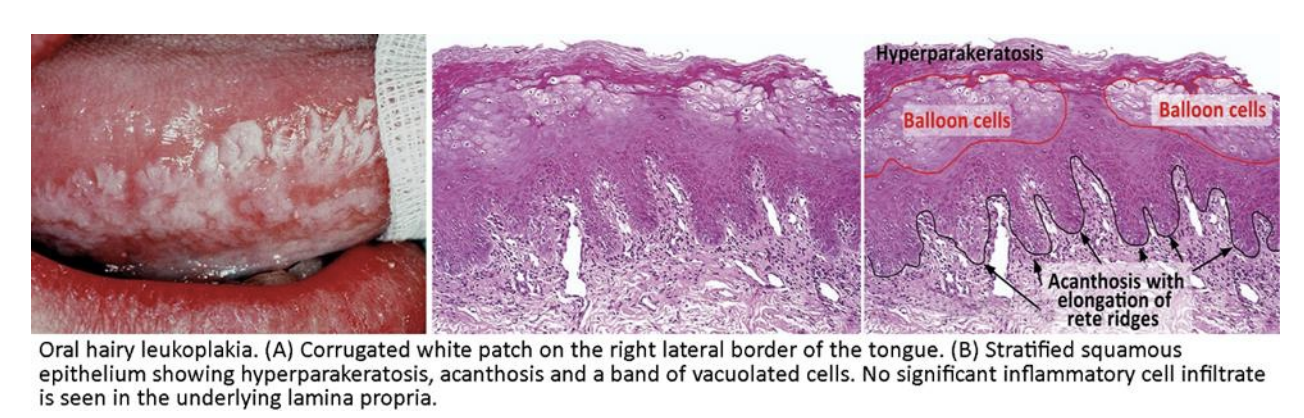
benign mucosal lesion by Epstein-Barr virus (EBV).
affects severely immunocompromised subjects
HIV-infected individuals, solid organ transplant recipients).
Clinically,
unilateral or bilateral,
white, corrugated, painless patches on the lateral margins of the tongue
cannot be rubbed off.
rarely described in other surfaces of the oral mucosa.
Microscopically,
the white patches demonstrate marked acanthosis of the stratified squamous epithelium
(i.e., increased thickness of the stratum basale and stratum spinosum manifested as elongation of the rete ridges), surface hyperparakeratosis
band of balloon cells (clear cells or ballooning degeneration) in the upper stratum spinosum.
There is minimal or no inflammatory infiltrate in the underlying lamina propria.***
Electron microscopy: EBV viral particles in the nuclei of balloon cells.
Hyperkeratosis —> "hairy" gross appearance of the lesion.
• no tx, resolves spont. & recurrence is high
Oral hairy leukoplakia (OHL)
Invasive oral cancer is preceded by ___________
(often presents as white patches or red patches)
preinvasive oral lesions

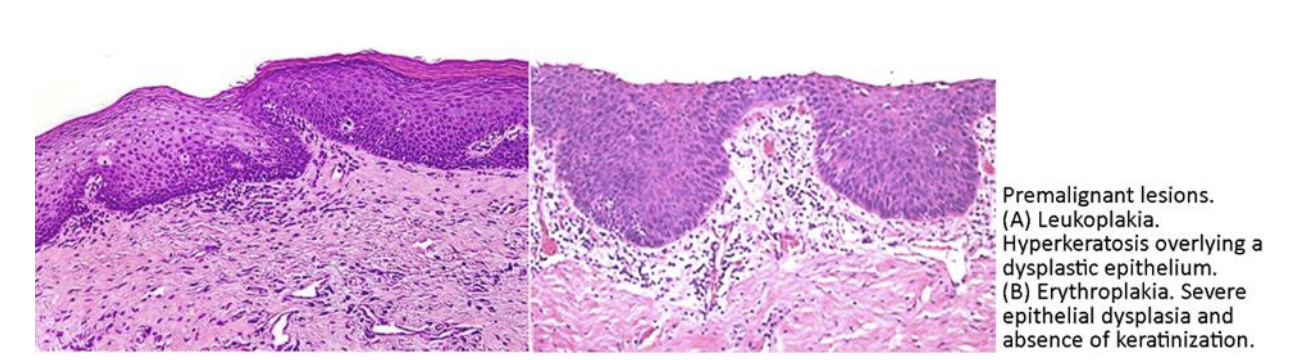
(leukoplakia v. eythroplakia)
preinvasive oral lesions biggest risk factors
(2)
Smoking and alcohol
50yrs-60yrs
male
About 90% of HCN are squamous cell carcinomas.
very common in developing countries, not so much USA
===
Invasive presents clinically as an
(i) exophytic (fungating) mass,
or
(ii) ulcer with indurated borders.
painless initially, —> develop pain or burning sensation when the tumor is advanced.
metastases in the ipsilateral cervical lymph nodes at presentation is common!
lung,» mediastinal lymph nodes »liver »bone.
Oral cancer
what are the 5 top risk factors for oral cancer
(A) Tobacco smoking and alcohol.
(B) Tobacco chewing.
(C) Areca nut. Betel leaf chewing
(D) Human papillomavirus (HPV) infection. oropharynx*
(E) Ultraviolet radiation. - lower lip*
what is the seperation of the oral cavity and the throat?
oral cavity —- oropharyngeal tumors.
oral cavity proper
is comprised of the lips, gingiva, retromolar trigone, hard palate, buccal mucosa, mobile tongue, and floor of the mouth,
tobacco and alcohol
oropharynx
is comprised of the palatine tonsils, soft palate, tongue base (posterior to the circumvallate papillae), and posterior pharyngeal wall.
HPV infection.
most common sites of oral cancer:
(3)
lateral margin of the tongue
floor of the mouth,
lower lip
occur in the palatine tonsils // lingual tonsils areas;
—> tonsillar crypts!!
younger age at onset,
weak or no association with alcohol and tobacco use.
mostly presents as:
cystic or solid neck mass,
or enlarged tonsil
or enlarged cervical lymph node.
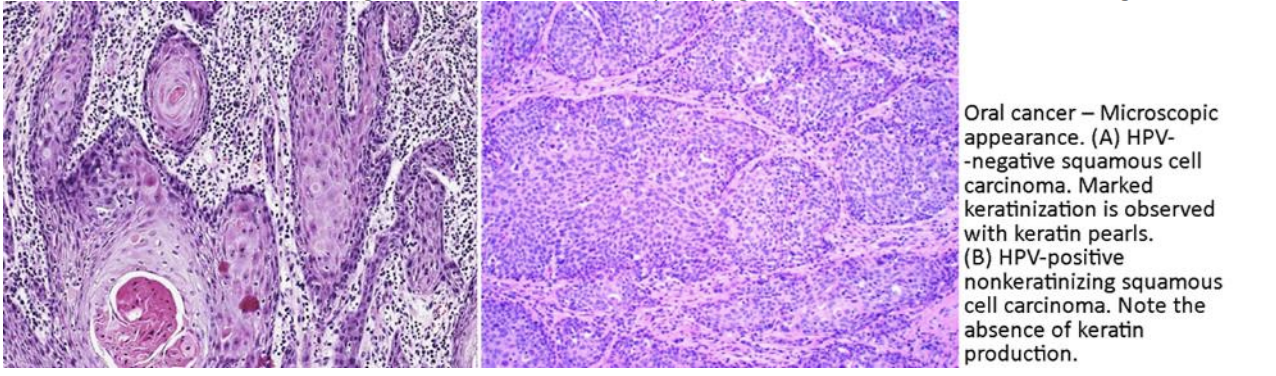
HPV-related oropharyngeal cancers are NON-keratinizing squamous cell carcinomas.
non-K tumors: consist of nests and cords of tumor cells invading the lamina propria.
Central areas of necrosis are often present in the tumor nests.
Tumor cells are smaller than cells of keratinizing tumors: t
monomorphic, with indistinct cell border, hyperchromatic nuclei, and high nuclear-to-cytoplasmic ratio.
Intercellular bridges are less conspicuous and keratin production is markedly reduced or absent.
oropharyngeal cancers
Cancer of the _______________
#1 squamous cell carcinomas (SCC).
in-freq: Verrucous carcinoma // malignant salivary gland-type tumors
rare: Kaposi sarcoma, malignant melanoma and non-Hodgkin lymphoma
arising from mesenchymal and lymphoid tissues.
————————————————————————-
note:
HPV-NEGATIVE KERATINIZING SQUAMOUS CELL CARCINOMA.
The majority of HPV-negative SCCs of the oral cavity are typically ‘keratinizing,
HPV-related oropharyngeal SCCs have a ‘nonkeratinizing’

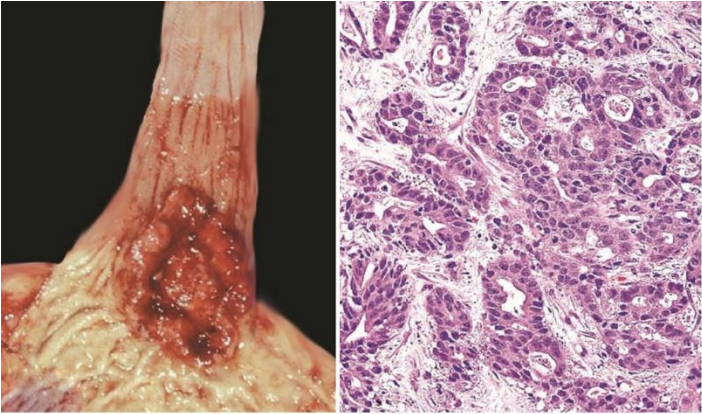
left: HPV-neg .. right: HPV-pos
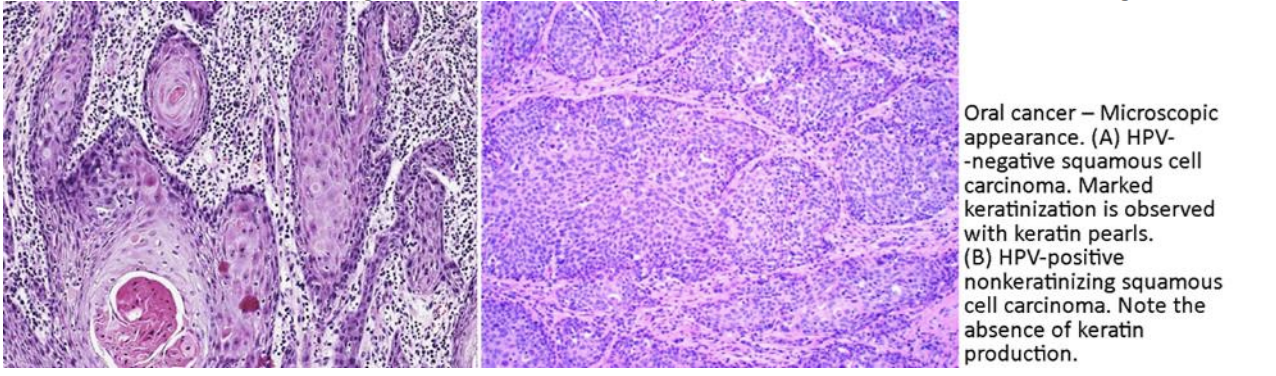
Cancer of the oral cavity proper.
left is HPV-neg and so its {kertized // non-keratinzed}??
Keratinizing SCCs are more differentiated than nonkeratinizing ones.
Keratinizing SCCs form epithelial cords or nests invading the lamina propria. Tumor cells are pleomorphic but resemble normal keratinocytes from spinous layer.
They are large, polygonal, with abundant eosinophilic (pink) cytoplasm 9 and central nucleus.
Immature/basal cells are located at the periphery of the cords, becoming more mature to the center of the cords, where tumor cells transform into keratinized, flat, anuclear squames and form round nodules with concentric, laminated layers, called "keratin pearls”.
presence of intercellular bridges**
The surrounding stroma is reduced and contains inflammatory infiltrates (lymphocytes).
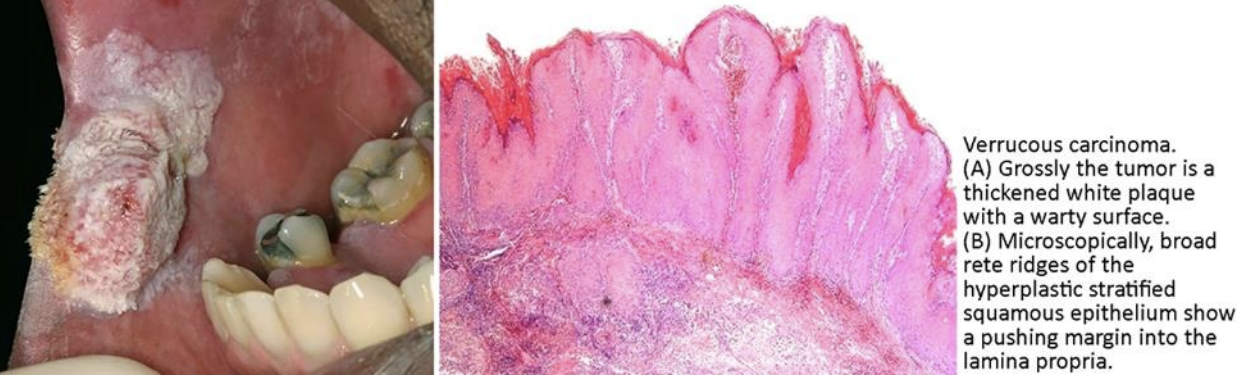
low-grade variant of oral squamous cell carcinoma.
incr. risk w/ smoking and smokeless tobacco use.
does NOT metastasize*
Grossly:
thickened white plaque with a warty or papillary surface
Histologically:
carc.stratified squamous epithelium is very well differentiated,
+hyperplasia but no dysplasia or atypia.
+ keratinization and a pushing border of bulbous rete ridges extending into the dermis.
Verrucous carcinoma
The salivary glands: major and minor salivary gland categories.
major salivary glands:
parotid, the submandibular, and the sublingual glands.
The minor glands: are dispersed(oral/pharnx/larynx)
tumors relatively rare
loc’d in the palate (50%), upper lip (15%), and cheek mucosa (15%).
mostly malignant.
most common: (in order)
mucoepidermoid carcinoma
adenoid cystic carcinoma
adenocarcinoma
Minor salivary gland tumors (MSGT).
p16 and p53, are frequently inactivated in ______
CDKN2A GENE controls p16
loss of the p16 protein leads to cyclin D overexpression,
inactivation of the Rb protein and loss of G1 arrest control.
—
TP53 GENE controls p53
Activated p53 induces a temporary cell cycle arrest at G1 checkpoint and promotes DNA repair to maintain genome integrity and cell viability.
If the DNA damage is beyond repair, p53 induces cell apoptosis of injured cells
HPV-negative oral SCCs. (oral cancer)
HPV early coding region (E) which contains six (E1 to E6) open reading frames.
expression of HPV's E6 and E7 proteins that bind to and inactivate p53 and Rb tumor suppressor proteins —>malignant transformation
p16 hyperreactivity.
overexpressed in cells with inactivated Rb protein.
The p16 overexpression is considered a surrogate marker for HPV-related SCCs***
HPV-associated oropharyngeal cancers.
subjective feeling of oral dryness perceived by the patient.
due to hyposalivation, a manifestation of salivary gland hypofunction (SGH).
associated with burning feeling in the mouth, halitosis, impaired chewing, swallowing, and speech, changed sense of taste, dental caries, and predisposition to oral fungal infections.
symptom of various medical conditions.
ex. Sjögren syndrome.
commonly caused by prescription medications.**
e.g. antihypertensives, antidepressants, and chemotherapy , radaition to head/neck
Aging
is associated with loss of acinar cells, impaired glandular 2 function and lower levels of salivary flow.
Xerostomia
refers to the formation of calculi within a salivary gland or salivary gland duct.
most common disorder of the salivary glands
loc’d: n the submandibular gland (84%)» partoid
dx: CT
peaks: 30 to 60 years of age.
can lead to ductal obstruction, salivary stasis, and secondary bacterial infection (acute bacterial sialadenitis).
Recurrent episodes —> may result in chronic bacterial sialadenitis.
Sialolithiasis
(salivary gland stones)
extra:
are benign pseudocysts that lack an epithelial lining filled with mucus.
These lesions occur as the result of trauma or obstruction to the salivary gland excretory duct and spillage of mucin into the surrounding soft tissues.
minor* salivary gland origin.
mostly on the lower lip*
fluctuant painless swellings of the lower lip and have a blue translucent hue.
common lesions; 20 years&younger!!
. Mucoceles
are mucoceles that occur in the floor of the mouth.
They usually involve the major* salivary glands
(sublingual gland specifically).
There are two types: oral and cervical (or plunging)
oral: typically presents as a painless, bluish, unilateral cyst in the floor of the mouth*.
The plunging: presents as a soft painless, swelling in the neck*
much less frequent compared to mucoceles.
Ranulas
chronic autoimmune disease
DRY EYE, DRY MOUTH, KCS
is the second most common autoimmune disorder in adults, after SLE
characterized by immunologically mediated destruction of salivary and lacrimal glands.
lymphocytic infiltrates are periductal surrounding the salivary and lacrimal excretory ducts and later infiltrate diffusely the glandular parenchyma, and germinal centers form*. —> destorys acinar secretes & replaced with lymphoid
Epithelial-myoepithelial islands in salivary glands*
—> xerostomia (dry mouth)
—> keratoconjunctivitis sicca (dry eyes).
Primary » secondary
^w/o disease vs. w/ disease
female » && ~(40-50yrs)
Laboratory findings:
leukopenia, elevated erythrocyte sedimentation rate, and polyclonal hypergammaglobulinemia. •
antibodies to the Ro/SSA and/or La/SSB autoantigens.
ANA , RF
Complications. Chronic B-cell stimulation results in MALT lymphoma
Sjögren syndrome (SS)
more symptoms associated:
.Spectrum of salivary gland tumors:
Parotid > > > submandibular, minor salivary > sublingual
^more likely benign ……………………….^ more likey cancer
-most common tumor of the parotid gland:
pleomorphic adenoma (60% of all cases).
-About 80% of parotid neoplasms are benign
As the size of the gland decreases, the incidence of malignancy of a tumor in the gland increases.
Among all patients, the most common tumor type:
#1 pleomorphic adenoma
#2 Warthin tumor (benign)
most common malignant tumor:
mucoepidermoid carcinoma
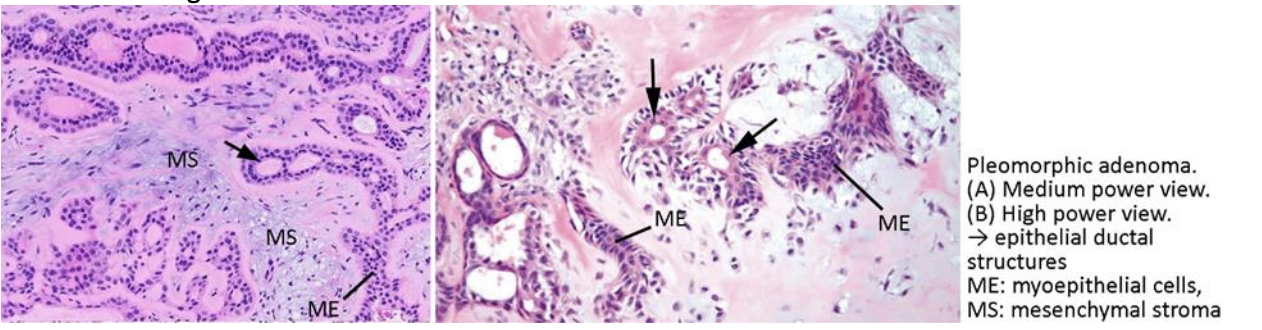
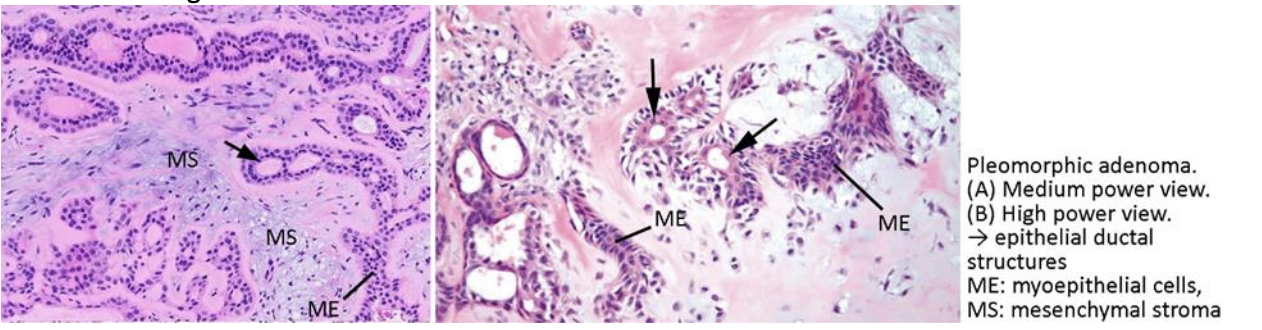
mixture of both epithelial and mesenchymal components.
most common salivary gland tumor.
About 60% occur in the parotid gland > >
30-60’s ,, female >
well-circumscribed ovoid masses that are surrounded by an incomplete capsule.**
histo: a biphasic tumor comprised of ductal epithelial and myoepithelial cells (mixed)****
painless, slowly growing mass.
tx: surgical excision
The most common presentation:
sudden rapid enlargement of a long-standing mass associated with facial nerve palsy, fixation to the surrounding soft tissues, and enlarged lymph nodes.
genes:
PLAG1 (pleomorphic adenoma gene 1) gene*
HMGA2 (high mobility group AT‐ hook 2) gene.*
^increases cell growth
Pleomorphic adenoma (PA),
also known as ‘benign mixed tumor’

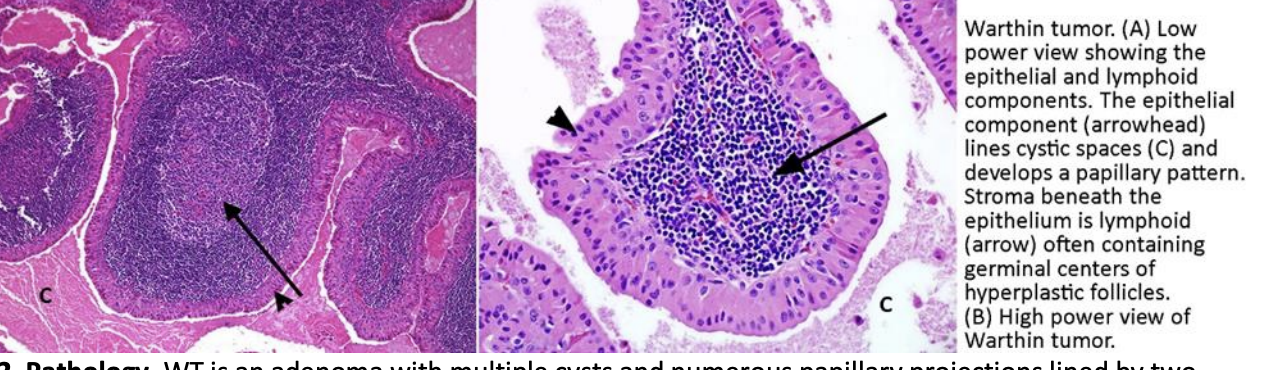
second most common benign tumor of the salivary glands, - ONLY in the parotid gland***
slow growing, painless parotid mass.
60-70’s, male > , +smoker
histo:
adenoma with multiple cysts and numerous papillary projections lined by two layers of columnar and basaloid oncocytic epithelium.
The connective tissue stroma shows dense lymphoid tissue, often with reactive germinal centers**
Oncocytes* are characterized by acidophilic granular cytoplasm due to presence of an excessive number of mitochondria. (+aging)
Warthin tumor (WT),
aka: adenolymphoma,
or papillary cystadenoma lymphomatosum,
to remember: “old man P. Wartin”
malignant epithelial tumor of the salivary glands,
characterized by acini with mucus-producing glandular cells
and by the presence of metaplastic epidermoid (elements that resemble squamous cell carcinoma.)
most common cancer of the salivary glands
20-60yrs // male>
small, mucin-containing cysts.
slowly enlarging painless and firm mass of several years’ duration; clinically mimicking a pleomorphic adenoma
composed of three types of cells:
namely mucus-secreting glandular cells,
epidermoid cells,
intermediate cells.
CRTC1-MAML2 activates the transcription of Notch target genes
Low-grade tumors:
mucus-filled cysts and the epidermoid component is infrequent.
Cytological atypia is minimal and mitoses very infrequent.
benign clinical course, rarely metastasize.
invade locally,, rarely recur
Intermediate grade tumors:
few mucus-filled cysts combined with solid nests of epidermoid cells.
Cellular pleomorphism is mild to moderate, and mitoses are few.
High-grade tumors:
solid nests of epidermoid cells and cystic structures are infrequent.
(+)Cellular pleomorphism and (+)mitoses
Prognosis: dismal.
high-grade neoplasms and, to a lesser extent, intermediate-grade tumors are invasive and difficult to excise and so recur in 30% of cases and metastasize to distant sites in 30% of cases.
The overall 5-year-survival rate is 68%-75%.
Mucoepidermoid carcinoma
rare tumor
the second most common malignant salivary gland tumor
minor sal. glands » …. » partoid glands
50-60’s … men=women
Three growth patterns have been described:
cribriform, tubular, and solid.
genes:
t(6;9)(q22-23;p23-24) chromosomal translocation
This translocation generates a fusion transcript involving the genes MYB and NFIB
*****MYB immunostaining
small and indolent tumor.
It grows with a slower rate in comparison with other carcinomas and is asymptomatic.
In most cases the tumor goes unnoticed until it has invaded local nerves
recurrence rate is high. prognosis bad (long term)
Adenoid cystic carcinoma (ACC)
Adenoid cystic carcinoma (ACC)
which pattern: cribriform, tubular, OR solid??
classic growth pattern→, the most common
proliferation of myoepithelial-type tumor cells form nests in which the cells surround spaces or pseudolumens producing a classic sieve or Swiss cheese
pseudolumens are filled with ground substance (glycosaminoglycans) as well as basement membrane-like material (laminin) produced by the neoplastic myoepithelial cells.
Rarely, true glandular lumina composed of cuboidal cells showing ductal differentiation and filled with scant secretory product can also be found scattered throughout the tumor.
Cribriform pattern
Adenoid cystic carcinoma (ACC)
which pattern: cribriform, tubular, OR solid??
shows well-formed ducts with recognizable inner epithelial and outer myoepithelial layers.
The stroma is commonly dense and hyalinized.
Tubular pattern
Adenoid cystic carcinoma (ACC)
which pattern: cribriform, tubular, OR solid??
contains solid aggregates of small, cuboidal basaloid cells with myoepithelial cell differentiation
but lacking obvious lumens or pseudolumens.
solid pattern
low-to-intermediate grade malignant neoplasm of salivary glands
characterized by serous acinar cell differentiation, which is characterized by cytoplasmic zymogen secretory granules.
40-60’s .. female> .. partoid»
Microscopically,
tumor cells are large and polygonal with abundant basophilic granular cytoplasm (due to zymogen-like granules)
The cytoplasmic zymogen-like granules are PAS positive.
The tumor cells display a variety of growth patterns but solid and microcystic patterns are the most common and are often seen together.
ecur in 30% and metastasize in 15% of cases w. good 5year survival outcomes
Acinic cell carcinoma (AciCC)
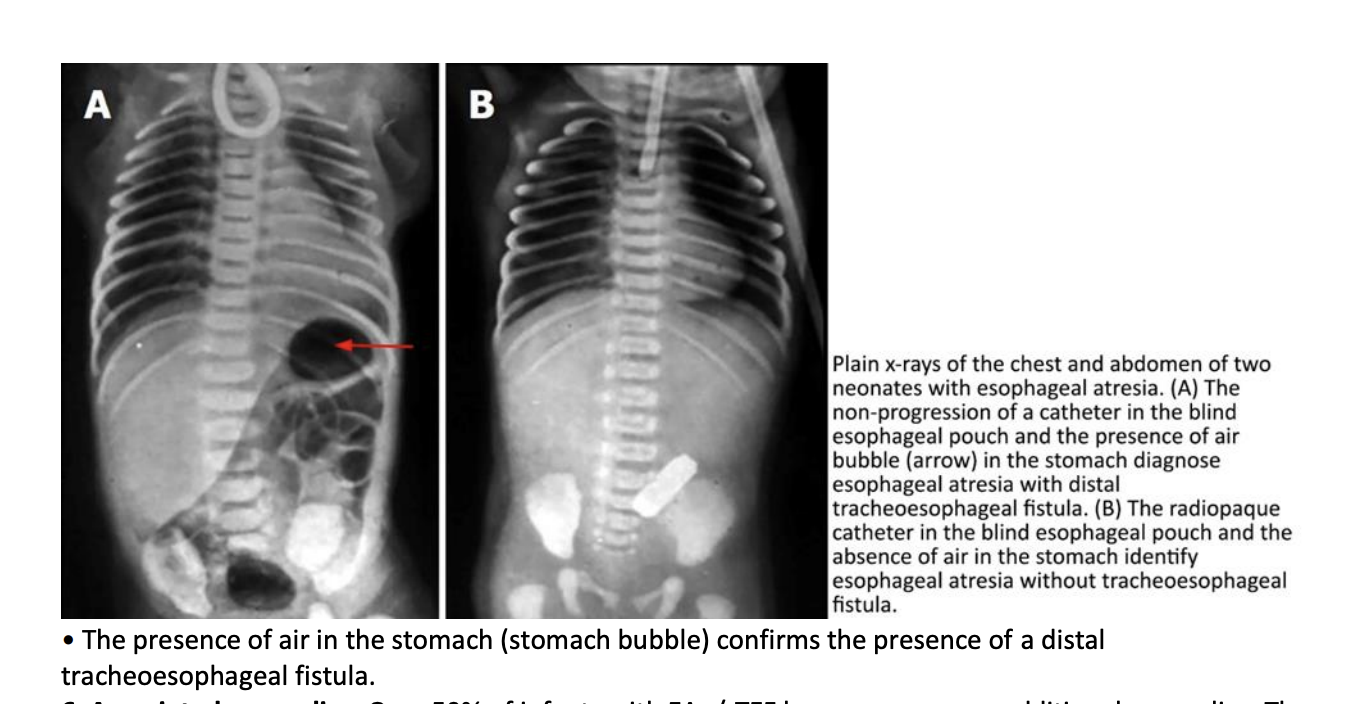
condition in which the proximal and distal portions of the esophagus end blindly and do not communicate.
The upper segment of the esophagus extends to the level of the second to fourth thoracic vertebra.
In contrast, the distal esophageal portion extends 1-2 cm above the diaphragm.
with or without TEF is a common anomaly
1. esophageal atresia with distal tracheoesophageal fistula*»
2. isolated esophageal atresia w/o te fistula
3. H-type tracheoesophageal fistula with no atresia
(other super rare)
prenatal: earliest clinical sign: of an infant is polyhydramnios**
(excess ammino fluid bc baby cant drink it)
Postnatal:, pure EA become symptomatic within the first few hours of life.
cannot swallow and appropriately handle secretions. excess salivation (drooling),
requiring repeated suctioning: copious, fine, white, frothy bubbles of mucus secretions
fluid will always return because of an inability to swallow.
feeding —> infant coughs, chokes and turns blue, due to aspiration of food into the lungs
dx: prenatal ultrasonogram +polyhydramnios
- attempting to pass a catheter through the nose or mouth into the stomach.
In patients with atresia, the catheter typically stops at 10 to 12 cm. (normal: 17cm)
Esophageal atresia (EA)
is an abnormal communication between the trachea and esophagus.
When associated with EA, the fistula commonly enters the trachea posteriorly just above the carina.
Patients with EA and distal TEF are at risk for additional complications:
gastric secretions may also reflux retrograde through the fistula into the tracheobronchial tree, —> pneumonia.**
Patients with H-type TEF without EA present with coughing and choking associated with feeding as the milk is aspirated through the fistula into the trachea and lungs.
Pneumonia and atelectasis develop quickly in these neonates**
dx: fetal stomach bubble
tracheoesophageal fistula (TEF)
50% of infants with EA+/-TEF have one or more additional anomalies.
//// what main syndrome is it associated with?? /////////
The VACTERL syndrome occurs in 25% of patients with EA+/-TEF.
VACTERL:
Vertebral defects, -
Anorectal malformations,
Cardiovascular defects,
TracheoEsophageal defects,
Renal anomalies,
Limb deformities
cardiovascular anomalies (ventricular septal defect),
anorectal anomalies (imperforate anus),
kidney//urinary issues:
urinary anomalies (renal agenesis or dysplasia, horseshoe kidney, polycystic kidney),
skeletal anomalies (hemivertebrae, scoliosis). •
is a condition affecting male» infants, caused by hypertrophy of the pylorus
characterized by:
hypertrophied inner, circular layer of the muscularis propria w/ thickened and edematous mucosa.
(inner = thicker)
The outer, longitudinal layer of muscularis propria is often thinner than norma
(longer = thinner)
clinically normal at birth.
S&S @ 3 and 5 weeks of age.
immediate onset of postprandial vomiting that is nonbilious and forceful (projectile)
Persistent vomiting results in electrolyte disturbances
dehydration, depletion of hydrogen, chloride, and potassium ions, and metabolic alkalosis
DX: US: visualizes the hypertrophic pyloric muscle: thickness of ≥3.0 mm
etiology: multi-factoral, incr. risk w/ Erythromycin or azithromycin exposure & maternal smoking
Infantile hypertrophic pyloric stenosis
most common congenital anomaly of the pancreas
results from failure of fusion of the dorsal and ventral buds leaving the pancreas with two separate ducts.
The major portion of the pancreas is drained by the duct of Santorini through the minor duodenal papilla.
The ventral pancreas drains by the duct of Wirsung into the major papilla.
often: asymptomatic.
can be: associated with recurrent episodes of pancreatitis. - the duct of Santorini and the minor papilla are too small.
Pancreas divisum
background info if needed:
The dorsal bud develops into the anterior head, neck, body and tail segments of the pancreas.
The ventral bud develops into posterior head and uncinate process.
The main pancreatic duct (of Wirsung) draining into the major duodenal papilla forms from the duct of the ventral pancreatic bud in the pancreatic head and the distal part of the duct of the dorsal bud in the body and tail.
The accessory pancreatic duct (of Santorini) draining into the minor duodenal papilla forms from the duct of the dorsal pancreatic bud.
rare
ring of pancreatic tissue partially or completely encircling the second part of the duodenum.
due to incomplete rotation of the ventral pancreatic bud.
asymptomatic, but…. can cause:
Severe duodenal obstruction
results in neonatal presentation with feeding intolerance, vomiting, and abdominal distension.
Moderate obstruction
causes recurrent vomiting in adults usually bt 20-50yrs
Plain abdominal x-ray or ultrasonography findings are similar to those for duodenal atresia: a double bubble, caused by a distended stomach and duodenal bulb.
Annular pancreas
______ , the lumen of a segment of the gastrointestinal tract is completely occluded.
Stenosis is a narrowing of the gut lumen that leads to partial obstruction.
intestinal atresia,
most commonly detected form of gastrointestinal atresia.
occurs at the second part of the duodenum distal to the ampulla of Vater.
DX: US prental: \
(i) polyhydramnios
(ii) two fluid-filled structures consistent with a “double bubble”
(the stomach and the dilated proximal duodenum, but no fluid beyond this point).
There is absence of distal intestinal gas, suggesting complete obstruction.
Once delivered,
an infant typically has a scaphoid abdomen.
Bilious* vomiting occurs following the first oral feeding.
One or two initial meconium stools may be passed, but no further bowel movements occur after that.
associated w/ Down syndrome.
Duodenal atresia
form of gastrointestinal atresia?.
clinically characterized by abdominal distension and bilious vomiting within the first two days after birth.
may pass meconium.
Jejunal and ileal atresia
presents with:
marked abdominal distension,
failure to pass meconium!! (none at all)
and bilious vomiting.
- Because the obstruction is distal, S&S later than with more proximal lesions,
although usually within the first three days after birth
Colonic atresia
fails to pass meconium
abdominal distention.
features absence of a normal anal opening.
3 types:
i) the high type is characterized by no anal opening; the rectum terminatesabove the levator ani muscle complex;
(ii) in the low type, rectum ends distal to levator ani muscle via a perineal fistula; meconium may emerge from fistula;
(iii) in the intermediate type, rectum ends at the level of the levator ani muscle; this type is associated with a partial anal canal or perineal fistula.
Anal atresia (also called imperforate anus)
congenital anomaly referring to either the lack of or incomplete rotation of the fetal intestine.
Intestinal malrotation
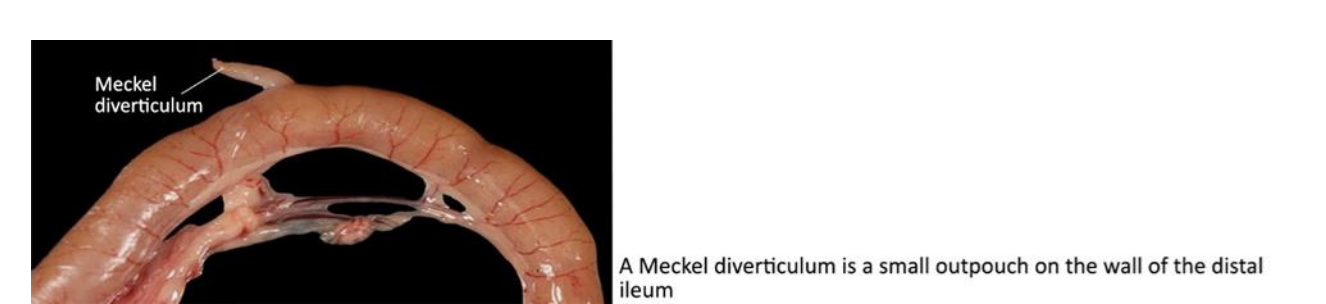
is a congenital blind outpouching of the distal ileum.
due to Incomplete regression of the vitelline duct
true diverticulum composed of all layers of the gastrointestinal tract and lined by typical ileal mucosa.
Ectopic gastric and rarely pancreatic mucosa is present
usually asymptomatic
symptoms in only 4% of patients—can present at all ages, mostly seen in children.
The most common causes:
gastrointestinal (GI) hemorrhage, followed by intestinal obstruction,
and inflammation.
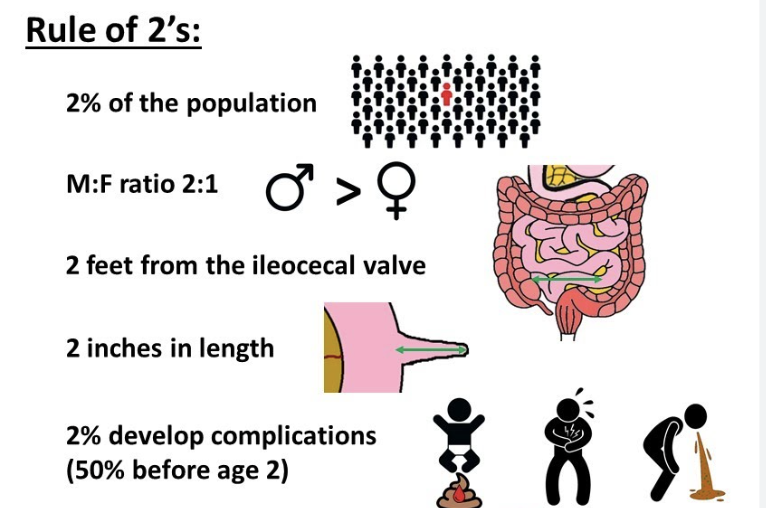
Meckel diverticulum
notes on the S&S:
Hemorrhage
is associated with peptic ulceration by ectopic gastric mucosa within the diverticulum.
Children: +hematochezia
, i.e., dark red or maroon stools,
Adults: + melena
(black/tarry stools), which may be attributable to slower colonic transit time in adults. •
-
Intestinal obstruction
is caused by intussusception
(MD invagination within the ileal lumen),
volvulus of small intestine around a vitelline duct fibrotic band extending from MD to umbilicus, or volvulus around an adhesive band from a previous abdominal surgical intervention.
S&S: bilious vomiting, abdominal distension, periumbilical pain, and constipation.
Both volvulus and intussusception compromise mesenteric vascular flow leading to bowel ischemia and necrosis !!
-
• Inflammation.
Meckel diverticulitis precipitates by obstruction of the diverticulum by a fecolith, or foreign body.
Diverticulitis is accompanied by fever, vomiting, and abdominal pain
and is often indistinguishable from acute appendicitis !!!!!
except that the location of the MD can be quite variable, and the pain and tenderness tend to be located at the periumbilical region rather than at the right lower quadrant.
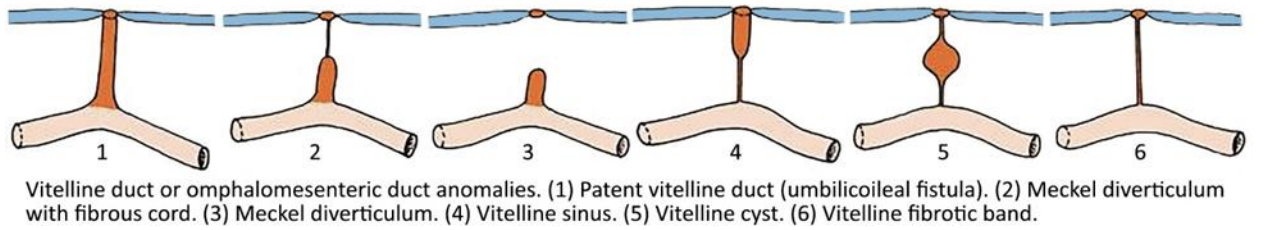
(A) Patent vitelline duct (umbilicoileal fistula).
Patients come to clinical attention in the newborn period because of fecal drainage from the umbilicus.
(B) Vitelline sinus.
umbilical end fails to close and forms a sinus tract that may vary in length. The ileum remains connected by a fibrous band.
Clinically, mucus discharge from the umbilicus is noted during infancy.
(C) Vitelline cyst.
A cyst develops when the midportion of the duct remains patent while each end obliterates.
Mucus accumulates within the cyst because it is lined by intestinal mucosa.
(D) Vitelline duct fibrotic band.
Vitelline duct is not completely obliterated, disintegrated, and absorbed.
A fibrous cord connects the umbilicus to the ileum.
Congenital fibrous bands are clinically significant because they may lead to intestinal obstruction or volvulus.
(E) Meckel diverticulum.
This is the most common (98% of cases) of the vitelline duct anomalies.
The diverticulum results from fibrous obliteration of the umbilical end of the omphalomesenteric duct and complete patency of the ileal end of the duct
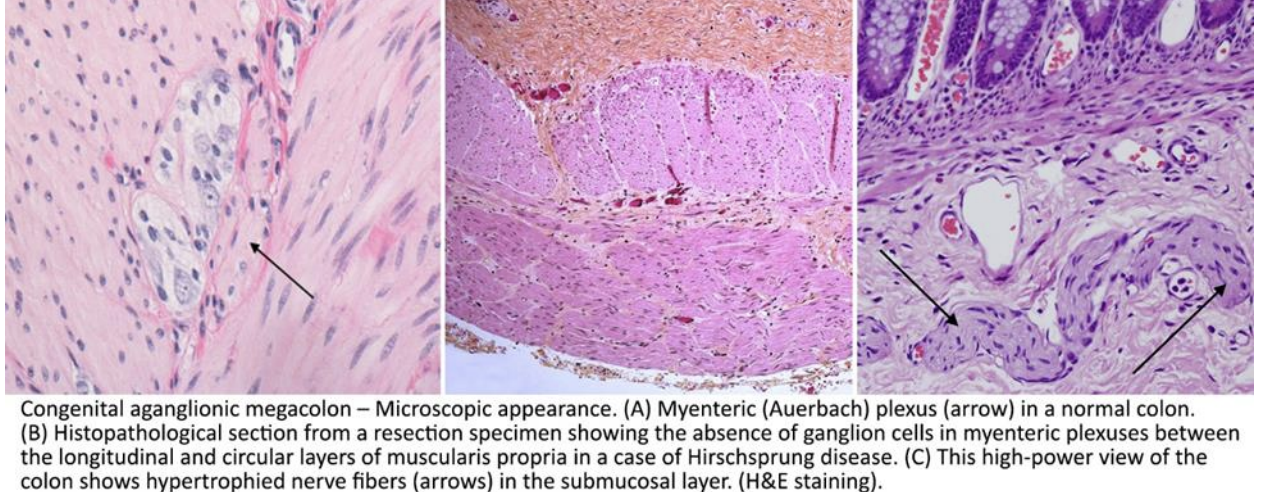
developmental disorder caused by the failure of neural crest cells
(precursors of enteric ganglion cells) to migrate in weeks 4-12 of gestation (gi development)
dx in first year of life » childhood, (rare:teens)
genes associated:
RET protooncogene
endothelin B receptor (EDNRB) gene
loc’d: Aganglionosis of the distal bowel begins with the anus,(always***)
75% of individuals aganglionosis involves most or all of the rectum and part of the sigmoid colon (‘classic’, or ‘short-segment disease’).
15-20%, aganglionosis extends proximal to the sigmoid colon (‘long-segment disease’)
5% of individuals, aganglionosis affects the entire large intestine (‘total colonic aganglionosis’).
Total intestinal aganglionosis = most severe form,,,extremely rare.
path:
aganglionic region may have a grossly normal or contracted appearance.
the normally innervated proximal colon undergoes progressive dilation and may become massively distended (megacolon) as a result of the distal obstruction.
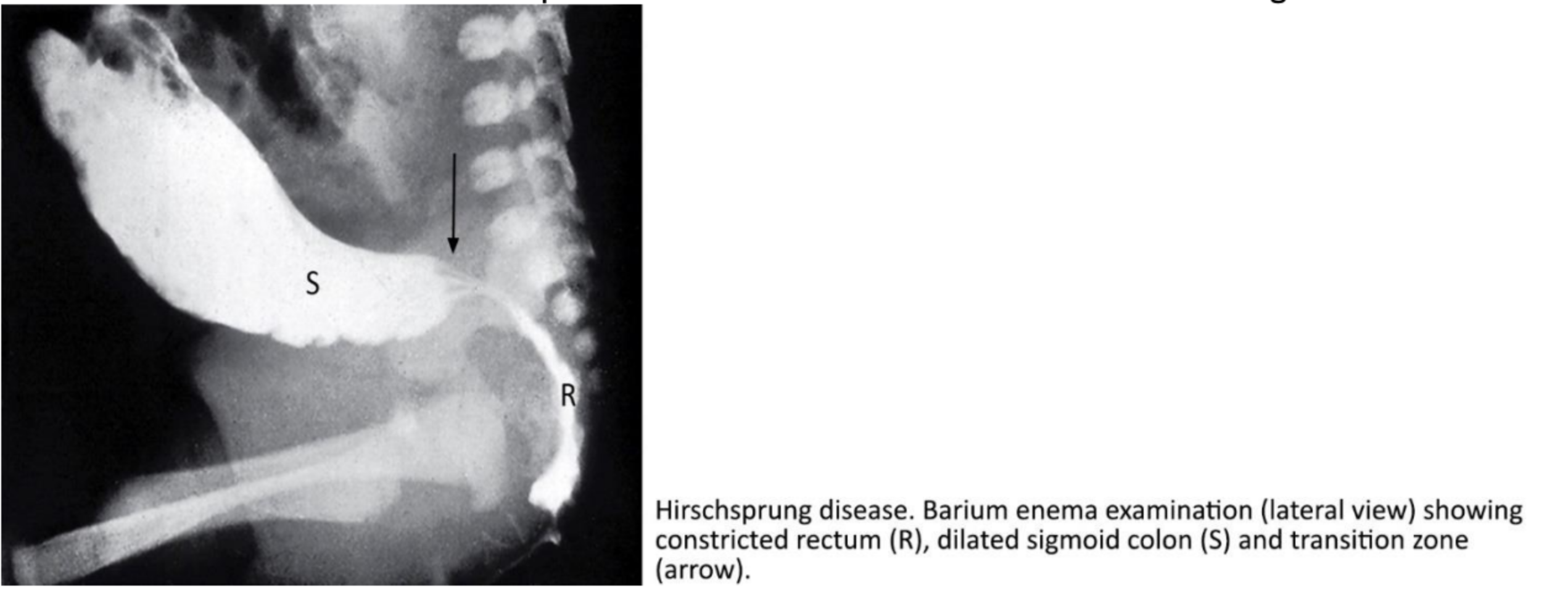
DX: GOLD STANDARD: is a rectal biopsy,
suction » open biopsy
will show complete lack of ganglion cells in all neural plexuses with associated hypertrophy of nerve fibers.
**can also dx with barium enema
contrast is administered via a catheter placed just inside the anus.
will reveal a cone-shaped transition zone* (dilated—>narrow)
complication: (most severe / lethal)
Hirschsprung-associated enterocolitis (HAEC)**
Pts present with explosive, foul-smelling diarrhea, fever, vomiting, colicky abdominal pain and distension, and even lethargy and shock.
due to overgrowth of bacteria in areas of stasis.
Hirschsprung disease —-
also referred to as congenital aganglionic megacolon
is a developmental discontinuity of the diaphragm that allows abdominal viscera to herniate into the chest
-
2 types:
Bochdalek hernia (90% of cases),
loc’d posteriorly & mostly: left side***
contain small bowel, spleen, stomach, colon, and occasionally the left lobe of the liver.
** if Right-sided Bochdalek hernias contain the right lobe of the liver.
more associated w/ resp distress & death
Morgagni hernia (10% of cases).
posterior to the sternum.
contains omentum and part of the transverse colon, and less commonly, liver and stomach.
sometimes not found until adulthood (asymp)
DX: detected prenatally US
Early chest x-ray after delivery confirms dx
when bowel gas visible above the diaphragm is accompanied by a mediastinal shift.*
. Congenital diaphragmatic hernia
large congenital defect in the midline of the abdominal wall, , covered by a transparent membrane.
Prenatal diagnosis: US in late first trimester to mid-second trimester.
In some cases, an elevated maternal alpha fetoprotein level may be detected.
Omphalocele
is a small, full-thickness defect of the abdominal wall, usually located to the right of the normal umbilical cord.
usually associated with evisceration of the intestines and rarely of the liver
the intestines are not covered by a membrane. •
Prenatal diagnosis: US in late first trimester to mid-second trimester.
In some cases, an elevated maternal alpha fetoprotein level may be detected.
Gastroschisis
is defined as a circumferential, smooth, thin (axial length of 0.3-0.5 cm) protrusion of normal esophageal tissue located at the gastroesophageal junction.
consists of mucosa and submucosa and is covered with squamous mucosa proximally and columnar epithelium distally.
distally.
IF - Dysphagia is felt — its at the lower chest level,
first-line tx: single dilation with a large bougie dilator.
iesophageal ring,
also called Schatzki ring,
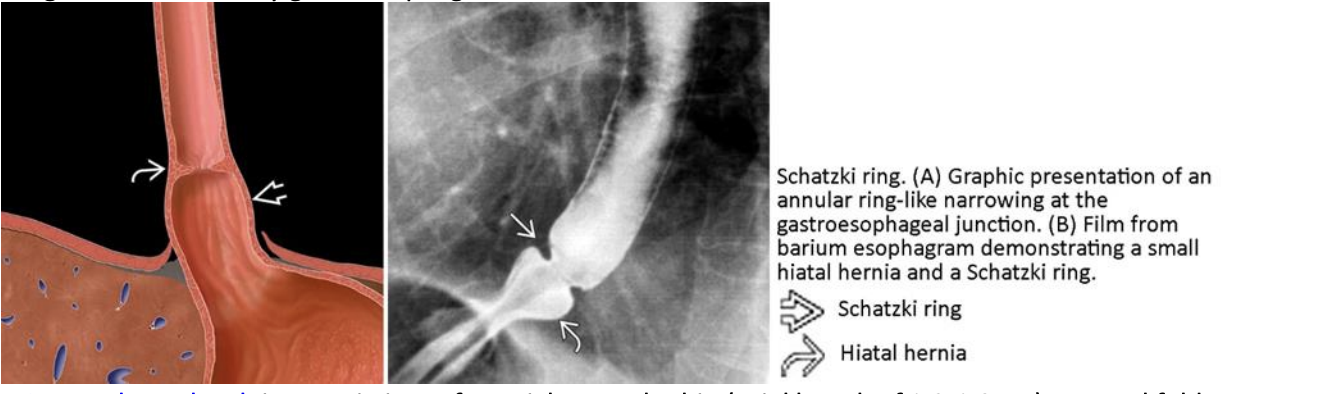
note: Plummer-Vinson syndrome (PVS).
PVS is a rare condition characterized by a triad of iron-deficiency anemia, postcricoid esophageal web, and dysphagia.
is a semi-circumferential, smooth, thin (axial length of 0.2-0.3 cm) mucosal fold that protrudes into the lumen and is covered with squamous epithelium.
consist of mucosa and submucosa and occur in the postcricoid region of the upper esophagus. •
Most w. no symptoms.
But once the internal ring diameter is <1.3 cm rings and webs cause solid food dysphagia,
dysphagia is felt in the throat
first line tx: single dilation with a large bougie dilator.
esophageal web
note: Plummer-Vinson syndrome (PVS).
PVS is a rare condition characterized by a triad of iron-deficiency anemia, postcricoid esophageal web, and dysphagia.
is an outpouching of mucosa through the muscular layer of the esophagus.
==
symptoms: dysphagia, regurgitation of undigested food, halitosis, and aspiration.
esophageal diverticulum
types:
Zenker diverticulum (ZD) is the most common type.
false!** diverticulum that protrudes posteriorly through a triangular region known as Killian triangle,
which is bordered above by fibers of the inferior pharyngeal constrictor muscle and below by the cricopharyngeus muscle.
pulsion* diverticulum caused by increased hypopharyngeal pressure that results from impaired opening of the upper esophageal sphincter
Midesophageal diverticula
true!!* diverticula caused by traction from mediastinal chronic and sclerozing inflammatory lesions that draw the wall of the esophagus outward.
•Epiphrenic diverticula
are pulsion type diverticula that are usually located in the distal 10 cm of esophagus.
They develop secondary to an underlying esophageal motility disorder (achalasia).
Histologically, they are false diverticula as they lack a muscle layer: mucosa and submucosa herniate through a defect in the muscular wall.
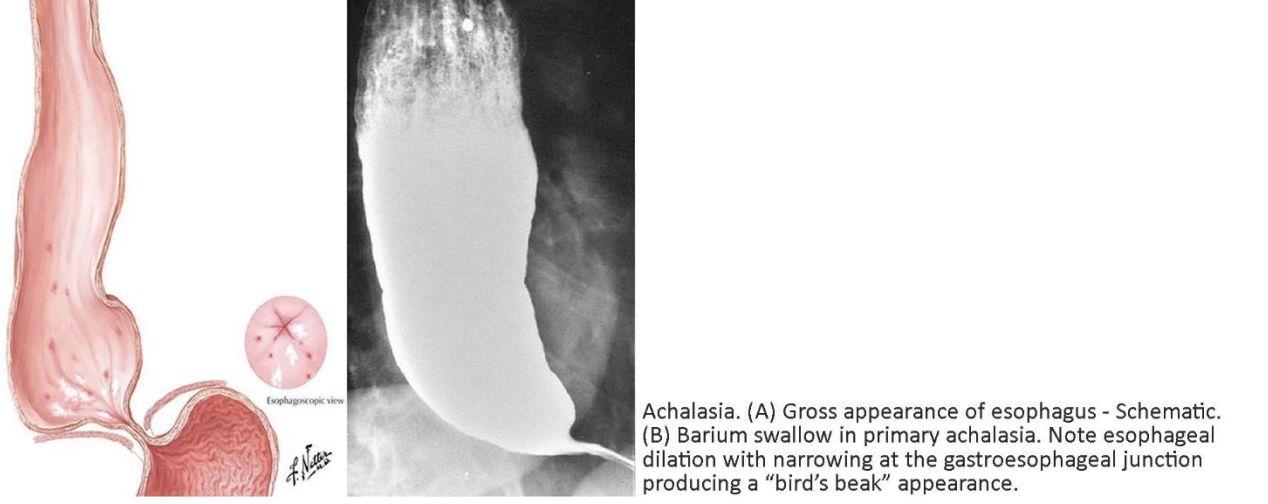
is characterized by the triad of
(i) incomplete lower esophageal sphincter relaxation,
(ii) increased lower esophageal sphincter tone,
and (iii) loss of esophageal peristalsis.
uncommon motor disorder - primary and secondary.
(25yr-60yrs) - expirence symp’s for years before dx
S&S:
(i) dysphagia for solids and liquids,
(ii) regurgitation of undigested food when the patient assumes the recumbent position at bedtime,
(iii) angina-like retrosternal pain, and (iv) heartburn.
GOLD STANDARD DX: Esophageal manometry*****
primary form: are (i) absent peristalsis in the body of the esophagus, and (ii) failure of the LES to relax, resulting in distal esophageal obstruction and proximal esophageal dilation.
can due barium swallow study*** (bird-beak)
The primary form
(autoimmune) is caused by degeneration of neurons in the esophageal myenteric plexuses and in the lower esophageal sphincter (LES)
The excitatory neurons release acetylcholine while the inhibitory neurons release nitric oxide (NO) and vasoactive intestinal polypeptide (VIP) resulting in esophageal and LES contractions and relaxations, respectively****
• Histopathologic studies have demonstrated absence or reduction in ganglion cells by cytotoxic T-cells.
sig. reduction in NO-synthase containing neurons has been demonstrated using immunohistochemical staining.***
Secondary form:
(i) carcinoma of the cardia (75%)
(ii) Chagas disease caused by the protozoan parasite Trypanosoma cruzi
Achalasia
is defined as a displacement of the stomach protruding through an enlarged esophageal hiatus of the diaphragm into the mediastinum.
2 types: sliding and paraesophageal hernias.
most often asymptomatic.
When symptomatic, patients will commonly present with symptoms of gastroesophageal reflux disease (GERD).
The restraining structure is the phrenoesophageal membrane, formed by the fused endothoracic and endoabdominal fascia.
notes:
sliding hernia - most common type»
is characterized by the displacement of the gastroesophageal (GE) junction above the diaphragm. The stomach remains in its usual longitudinal alignment and the fundus remains below the GE junction.
-
• A paraesophageal hernia
is a true hernia with a hernia sac and is characterized by an upward dislocation of the gastric fundus through a defect in the phrenoesophageal membrane.
hiatus hernia
is defined as mucosal damage produced by the abnormal reflux of gastric contents into the esophagus or beyond, into the larynx, oral cavity, or lung.
-
Risk factors. Hiatus hernia, obesity, alcohol, tobacco and caffeine use raise the risk of GERD.
-
Pathogenesis: The dominant pathophysiologic mechanisms causing reflux is LES dysfunction.
transient LES relaxation » grossly hypotensive LES (<10 mmHg).
- mucosa is inflamed and hyperemia, (*redness)
Microscopic changes of reflux esophagitis include:
• Scattered eosinophils within the nonkeratinized stratified squamous epithelium of the esophagus;
• Increased lymphocytes within the epithelium and lamina propria; • Hyperplasia of the squamous epithelium with marked thickening of the epithelial basal cell layer;
• Spongiosis: edema between epithelial cells (keratinocytes);
—
S&S:
heartburn and acid regurgitation.
Heartburn (pyrosis) is felt as a retrosternal sensation of burning or discomfort that usually occurs after eating or when lying down or bending over.
Regurgitation is the return of partially digested food from the stomach to the mouth.
Atypical symptoms include epigastric or chest pain (mimicking angina pectoris), dyspepsia, nausea, bloating, and belching.
Extraesophageal symptoms include chronic cough, asthma, laryngitis, and dental erosions.
GERD
name the 3 complications of GERD
Esophageal ulceration
is secondary to necrosis of esophageal epithelium causing ulcers near the gastroesophageal junction.
Esophageal stricture
is a persistent narrowing of the esophagus caused by persistence of ulcers causing an inflammatory and sclerosing damage of the esophageal wall deep to the lamina propria.
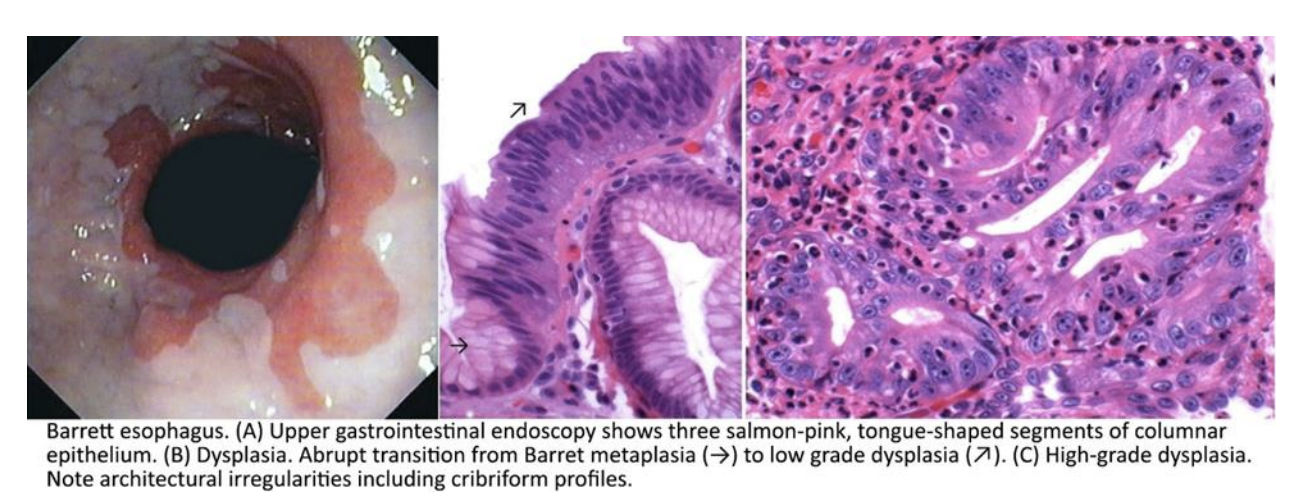
Barret esophagus
is defined as the presence on biopsy of intestinal metaplasia, that is, goblet cells containing acid mucin
is a condition resulting from an acquired metaplastic epithelial change in the esophagus in response to gastroesophageal reflux.
~55yrs , male»
can, but most do not progress to esophageal adenocarcinoma
Pathogenesis.
Prolonged exposure of the esophagus to the acid refluxate causes esophagitis, complicated by epithelial necrosis and erosion of the esophageal mucosa.
This chronic damage is believed to promote the replacement of the stratified squamous epithelium with metaplastic columnar cells.
This is an adaptive response, which, if not for the increased risk of cancer, would have been beneficial.
RF’s: chronic GERD, factors that increase risk for BE include older age, male gender, history of smoking, and obesity.
Pathology.
tongues of salmon-pink,
velvety mucosa extending upward from the gastroesophageal junction.
metaplastic mucosa alternates with residual smooth, pale squamous mucosa of the normal esophagus and interfaces with light-brown columnar (gastric) mucosa distally.
Three types of columnar metaplasia have been discerned: fundic, cardia, and specialized intestinal metaplasia (presence of goblet cells).
Note that only specialized intestinal metaplasia is recognized as a precursor of adenocarcinoma.
There is not universal agreement as to whether metaplasia of the gastric cardia or fundic type mucosa are sufficient for the diagnosis of Barrett esophagus.
Dysplasia develops in this metaplastic epithelium in a minority of patients
Progression to cancer.
risk marker for adenocarcinoma of the esophagus. // The annual incidence of esophageal adenocarcinoma among BE patients is about 1%
Clinical presentation.
The intestinal columnar metaplasia causes no symptoms.
seen initially for symptoms of associated GERD,
Barrett esophagus
—
note: defined only as the presence of intestinal metaplasia (presence of goblet cells).
is associated with immunosuppression.
. (A) Candida esophagitis.
The candida —adheres to the esophageal mucosa forming whiteyellow plaques.
The plaques can be seen on upper endoscopy and do not wash from the mucosa with water irrigation.
DX: H&E stain of biopsies show pseudohyphae
Dysphagia and severe pain on swallowing are the usual symptoms.
(B) Herpes esophagitis.
Clinical manifestations include odynophagia (painful swallowing) and dysphagia.
Frequently one can see herpetiform lesions in the mouth and lips.
Endoscopic examination shows either
(i) small, punched-out lesions with raised margins usually coated with yellowish exudate,
or (ii) multiple ulcers, with a map-like, confluent appearance.
Microscopic examination shows large, red intranuclear (Cowdry A)** inclusion bodies and/or intraepithelial vesicles containing acantholytic cells and multinucleated giant cells.
(C) Cytomegalovirus (CMV) esophagitis.
Typical endoscopic findings are several, well-circumscribed shallow ulcerations found in the distal esophagus.
infected cells are cytomegalic cells, typically two to fourfold larger than normal, containing basophilic intranuclear (Cowdry B)** inclusion bodies surrounded by a clear halo, giving the appearance of an owl's eye.
Clinical manifestations include odynophagia, fever, nausea, and substernal pain.
Infective esophagitis.
are dilated veins immediately beneath the mucosa that are prone to rupture and hemorrhage.
They arise in the lower third of the esophagus in patients with decompensated cirrhosis and portal hypertension.
The response to portal hypertension is the development of a collateral circulation diverting the obstructed portal blood flow to the caval veins
portocaval collaterals form by the opening and dilatation of preexisting vascular channels connecting the portal venous system and the superior and inferior vena cava.
The most important portosystemic anastomoses are the gastroesophageal collaterals.
Varices appear as tortuous dilated veins lying primarily within the lamina propria and submucosa of the distal esophagus and proximal stomach.—> rupture, leading to life-threatening massive upper gastrointestinal hemorrhage.
Esophageal varices
refers to bleeding from tears in the mucosa at the junction of the stomach and esophagus,
40s or 50s.
The classic clinical presentation: consists of an episode of hematemesis following a bout of retching or vomiting secondary to acute alcohol intoxication.
Patients present with a single longitudinal tear involving mucosa and submucosa but not the muscular layer.
The tear is about 2-3 cm in length and a few millimeters in width.
Mallory–Weiss syndrome
AKA: gastro-esophageal laceration syndrome,
Benign tumors of the esophagus are uncommon:
Leiomyomas: tumors of smooth muscle origin, most common*
-
Squamous papillomas: sessile lesions with a central core of connective tissue & a hyperplastic papilliform squamous mucosa.
two most common esophagus cancers
1. esophageal adenocarcinoma
2. squamous cell carcinoma
the middle and upper thirds of the esophagus
gene: lof: TP53 & NOTCH1 // gof: SOX2
over age 45; male »
most common present:
dysphagia and odynophagia.
Compression of the recurrent laryngeal nerve causes hoarseness, and tracheoesophageal fistula is manifested clinically by a chronic cough.
When patients present with symptoms most tumors are unresectable —> poor outcomes/prognosis
squamous cell carcinoma
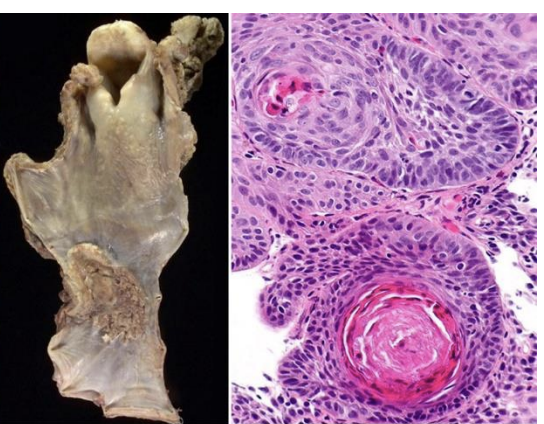
nest w/ keratn pearls^^
old white men w/ Barrett esophagus (BE) and long-standing GERD
distal third of the esophagus
micro: tumors are intestinal-type mucin-producing adenocarcinomas.
presents: pain or difficulty in swallowing, progressive weight loss, hematemesis, chest pain, or vomiting.
By the time symptoms appear, the tumor has usually spread to submucosal lymphatic vessels. (poor prognosis)
gene:
progression of BE to EAC occurs over an extended period through the stepwise acquisition of genetic and epigenetic changes
—>Mutations in p53 are identified in 71% of the EAC cases studied and mutations in CDKN2A gene are encountered in 12% of cases.
(The CDKN1A gene codes for p16)
Esophageal adenocarcinoma
barrett metaplasia
Acute gastritis is an inflammatory condition of gastric mucosa,(usually due to infection)
Acute gastritis
is a multistep, progressive and life-long inflammation of gastric mucosa.
The most common cause of chronic gastritis is Helicobacter pylori infection.
Etiology. H. pylori is a spiral shaped, microaerophilic, gram-negative flagellate bacterium
Chronic gastritis