Micro weeks 1 and 2
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
106 Terms
A samples can contain?
a single organism
mixed flora
mixture of more than 1 pathogen
contaminants
Where are some examples of mixed cultures?
skin swabs
throat cultures
urine with contaminants
What species forms lancet shaped diplococci?
streptococcus pneumoniae
What species forms palisades/stacks?
Diptheroids
What is the only clinically significant gram negative cocci?
Veillonella
Sheep’s blood agar is?
Supportive and differential (hemolysis patterns)
Chocolate agar is?
Enriched agar, used in the growth of fastidious organisms like Haemophilus and neisseria
MacConkey agar is?
Differential: lactose fermentation
Selective: inhibits growth of GPs
What is sulfamethoazole/trimethoprim agar?
differential: isolation of Group A beta hemolytic strep
selective: inhibits normal flora of upper repiratory tract
What units are used to report colony counts?
CFU/ml
What are the two types of gram stains?
direct (from the culture specimen)
indirect (from single isolate on culture plate)
Why are gram negatives thought to no retain the crystal violet?
Their cell walls have a higher lipid content than gram positives, alcohol removed the lipid from them, increasing their cell permeability and allowing the crystal violet to escape.
What is s. aureus’s size compared to other catalase positive Cocci?
Usually smaller and in grape-like clusters, can be found singly or in pairs
What are staphylococci usually found in?
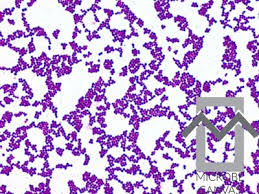
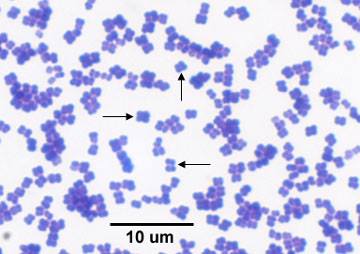
Clusters
What are micrococci usually found in?
pairs and tetrads and ultimately irregular clusters
What do staphylococci and some micrococci do to nitrate?
Reduce it to nitrites
How do staphylococci use glucose?
fermentatively
Which staphylococci are coagulase negative?
S. epidermidis and S. saprophyticus
Which staphylococci is coagulase postive?
S. aureus
What do staphylococci colonies look like?
Staphylococcus colonies are circular, opaque, smooth, raised to slightly convex (1-3 mm in 24 hr) with a butyrous (butter like) consistency; emulsify easily
Which Staph is DNAse positive and which is negative?
S. aureus is positive and S. epidermidis is negative
Which Staph is beta hemolytic?
S. aureus on BA are usually Beta-hemolytic and yellowish (pale yellow to golden pigment produced) but can be non-hemolytic and white
Which staph typically ferments mannitol?
S. aureus ferments mannitol - on Mannitol salt agar colonies are yellow with yellow zones (colonies that do not ferment mannitol are red). Sometimes S. saprophyticus is mannitol + also.
What is micrococci’s reaction to coagulase?
Negative
What is the colony morphology of Micrococcus?
Micrococcus spp. have variably colored colonies that are white, tan, yellow, orange or pink. The most commonly isolated micrococci produce lemon-yellow colonies
Can micrococcus ferment glucose?
Not usually
How is micrococcus usually differentiated from staph?
By its pattern of susceptibility and resistance to Bacitracin, and Furazolidone. Micrococcus = R to furazolidone and S to bacitracin.
What are some other organisms that are occasionally catalase positive gram positive cocci?
rothia
aerococcus
enterococcus
What is Micrococci’s microdase reaction?
Positive
How can you tell Rothia from micrococcus?
Rothia is modified oxidase neg, (Microdase), bacitracin R and furazolidone S.
Where is S. aureus carried?
In the anterior nares of 20-40% of the population
What kinds of diseases can S. aureus cause?
invasive infections: folliculitis, abscesses, wound infections, osteomyelitis, pneumonia and endocarditis
toxigenic: enterotoxin, scalded skin syndrome, toxic shook syndrome
Which Staph is associated with UTIs?
S. saprophyticus
Which CNS can cause infections?
S. epidermitis (patients with indwelling devices like catheters)
S. saprophyticus (UTIs)
S. haemolyticus (second most commonly isolated staph)
S. lugdunesis and S. schleiferi (less frequently isolated and cause infections similar to S. epidermitis)
Are micrococcus usually associated with pathogenesis?
No but have been implicated in rare cases of endocarditis
Which organisms are catalase positive?
staphylococci
micrococci
most corynebacteria
Which organisms are catalase negative?
streptococci
enterococci (may give false positive due to pseudo-catalase)
lactobacilli
actinomyces
What agar can cause a false positive on the catalase test?
Blood agar
What is the principle of the coagulase test?
coagulase positive organism + rabbit plasma (fibrinogen source) = agglutination (formation of fibrin strands)
Since some S. Aureus do no contain clumping factor or clumping factor is masked by a capsule, what testing must be performed?
Tube coagulase test
What is the tube coagulase test?
Tests for free coagulase or coagulase-reacting factor (CRF), a substance found in the rabbit plasma with which the free coagulase forms a complex.
Organism + 0.5 ml rabbit plasma 4hrs/35oC→ fibrin clot (contains "CRF + fibrinogen)
The test should be read at 30-minute intervals during the first 4 hours because some organisms produce strong fibrinolysins that dissolve the clot soon after it is formed
If the reaction is negative, hold tube overnight and read after 18-24 hours/25oC because some SA strains produce only enough coagulase to give a delayed positive result.
What do commercial coagulate tests test for?
clumping factor
protein A (cell wall antigen)
What does DNAse agar contain?
DNA-toluidine blue complexes giving the agar a blue color. Because nucleotide-toluidine blue complexes are pink, the agar turns pink in the areas where DNA is hydrolyzed. A second manufacturer makes an agar where the area around S. aureus clears.
DNA-toluidine blue -- DNAse --- > Nucleotides-toluidine blue (blue) (pink)
Which is novobiocin used and which organism is it the presumptive id for?
Used on urine samples and it the ID for S. saprophyticus, it is resistant while other CNS and SA are not
What are some common gram positive organisms cocci in pairs and chains?
streptococcus
What are some common gram positive organism cocci in clusters?
S. aureus
CNS
What are some common gram positive rods?
Bacillus
Diphtheroids
Corynebacterium diphtheria
Lactobacillus
What are some common gram negative rods?
Escherichia coli
Klebsiella pneumoniae
Pseudomonas aeruginosa
Stenotrophomonas maltophilla
Acinetobacter baumanii
What are come common gram negative coccobacilli?
haemophilus influenzae
Acinetobacter baumanii and Fransicella tularensis (pleomorphic)
What are some common gram negative diplococci?
Neisseria
Neisseria spp. is usually non-pathogenic but what species can be pathogens?
Neisseria meningitidis
Neisseria gonorrhoeae
What is an example of a gram negative cocci?
Veillonella, only clinically significant GNC
Media selection is determined by?
Body site
If isolate grows aerobically of anaerobically
fasitidiousness
What is enrichment factors are in chocolate agar?
Hemin (X factor)
Isovitalex (V factor or NAD)
Vit B12
Fe2+& Mg2+, Cysteine
What fastidious organisms is chocolate agar used for?
pathogenic Neisseria
Haemophilus spp.
What is S-MAC?
MacConkey agar except with sorbitol instead of Lactose
What is Sulfamethoxazole/trimethoprim (SXT) agar?
Selective and Differential
Used by some labs in the isolation of Group A beta-hemolytic strep
Inhibits the normal flora of the upper respiratory tract
SXT is an antimicrobial against normal throat flora (alpha Strep)
What is : Hemophilus Isolation Medium (HIM)?
Enrichment and Differential
Supports growth of Haemophilus
Contains X (Hemin) and V (NAD) factors
Contains horse blood: demonstrates hemolysis of hemolytic Haemophilus
Haemophilus hemolyticus Haemophilus parahemolyticus
H-QUAD Plate
4 quadrans: X,V, XV and horse blood
What is Columbia Colistin-Naldixic Acid (CNA)?
Selective Media
a. Selects for gram positive organisms in mixed cultures
b. Especially good if culture overgrown with swarming Proteus
On BA swarming morphology of some strains of Proteus mirabilis overgrows other organisms making them difficult to isolate.
Colistin and Naldixic Acid inhibit gram negatives
What is Phenyl Ethyl Alcohol (PEA)?
Contains Sheep BA and phenylethyl alcohol
Selective Agar
a. The PEA inhibits gram negative rods including swarming Proteus
b. Used similarly to CNA
c. Used in anaerobic bacteriology
What is Campy CVA Agar?
Selective Media used to isolate Campylobacter spp.
a. Brucella agar base (defibrinated sheep blood + yeast extract, casein)
b. Antibiotics inhibit GI flora
Cefoperazone (gnr)
• Vancomycin (gp)
• Amphotericin B (anti-fungal
c. Incubated under increased temps – 42OC
d. Incubate in micro-aerophilic environment • 85% nitrogen, 5% oxygen, and 10% carbon dioxide
e. Campylobacter is an enteric pathogen
What is Hektoen agar?
Differential Selective Media
a. Used in the isolation of and differentiation of Salmonella spp. & Shigella spp.
Additives
a. Bile salts: inhibit GNR
b. Lactose, sucrose, salicin (not used by S/S)
• Normal enteric gnrs use these sugars and turn media yellow • S/S do not
c. Na thiosulfate: H2S production (black color)
What is XLD Agar?
Xylose-Lysine-Desoxycholate Agar
Selective Differential
a. Used in the isolation of Salmonella spp. and Shigella spp.-
Additives:
a. Bile salts: inhibit GNR
Sugars: Normal enterics use lactose, sucrose & xylose and turn media yellow
• not used by S/S
Na thiosulfate: H2S production (black color change)
What is Thayer Martin Agar?
Enrichment, selective media a.
Used to isolate Neisseria gonorrhoeae
Base Similar to Chocolate but with antibiotics
a. Vancomycin: inhibits GPC
b. Colistin: inhibits GNR
c. Trimethoprim: Stops proteus from swarming
Nystatin: inhibits fungus
What is Martin Lewis Agar?
Similar to TM
Anisomycin: an antifungal, is substituted for nystatin
Concentration of vancomycin is increased
What is V-Agar?
Vaginalis Agar
Enrichment media
Aids in isolation of Gardnerella vaginalis
Composition
Human Blood – beta hemolysis
Peptones & Yeast Extract
What is BCYE agar?
Buffered Charcoal-Yeast Extract Agar
Enrichment media used to isolate Legionella spp.
Key Components
What is Thio Broth?
Thioglycollate broth
Set up on wound and fluid cultures
Supports aerobic and anaerobic growth
Used to preserve organisms until cultures are finalized
What is GN and Selenite Broth?
GN and Selenite Broth
Support the growth of Salmonella spp. and Shigella spp.
Stool cultures suspected of containing the organism are subbed to this media
The media enriches the growth of the organism
Good for samples containing small #s of pathogens
Differentiating micrococci and CNS:
How is glucose used to differentiate the two and what are the results?
A fermentation tube containing glucose, nutrients and bromcresol purple (an indicator) is inoculated (stabbed) to the bottom of the tube. Overlay the tube with sterile mineral oil and incubate overnight. Continue to read negative tubes for 5 days.
• Positive Fermentation: tube turns yellow = organism has fermented the glucose which decreases the pH of the media to an acid pH changing the color of the bromocresol purple in the media to yellow.
• Negative Fermentation: no color change (purple or negative)
• Micrococci use glucose oxidatively
RESULTS: Staphylococci = +
Micrococci = neg
Differentiating micrococci and CNS:
How is furazolidone used and what are the results?
Use 100 ug furazolidone disk, Make a standard 0.5 McFarland standard of the organism in sterile water and swab onto a BAP. Place the furazolidone disk on top of the inoculated plate and incubate overnight. Look for zone of inhibition and measure diameter in mm •
RESULTS Micrococcus = R = (zone = 6-9 mm) Staphylococcus = S = (zone = >15mm)
Differentiating micrococci and CNS:
What is the modified oxidase test and what are the results?
A dropper or disk is impregnated with tetramethyl-p-phenylenediamine dihydrochloride (oxidase reagent) in dimethyl sulfoxide (DMSO). The DMSO renders the cells permeable to the reagent. A blue/purple color within 30 seconds is positive; no color development is negative.
RESULTS Micrococcus = + Staphylococcus = neg
Differentiating micrococci and CNS:
What is susceptibility to bacitracin and what are the results?
0.4u bacitracin disk placed on either Mueller Hinton agar (a nutrient agar used for antimicrobial susceptibility) or BAP after being inoculated with a 0.5 McFarland Standard suspension of the organism. Zones of inhibition are read after overnight incubation in non-CO2
RESULTS Micrococcus ( ≥ 10mm) = S Staphylococcus (no zone) = R
Which organism is sometimes refered to as sticky staph?
Rothia mucilaginosa (formerly Stomatococcus mucilaginosa)
What is the colony morphology of Rothia?
Whitish gray colonies, Large gpc in pairs, tetrads, and clusters on gram stain, have a capsule making them mucoid and difficult to emulsify
What are results of the catalase test, VP, gelatin and coagulase tests for Rothia?
Catalase: weak/negative
VP: +
Gelatin hydrolysis: +
Coagulase: -
Streptococci are usually found in?
Pairs or chains, especially in broth of blood culture
How are streptococci typed?
By their cell wall carbohydrates(Lancefield grouping): A, B, C, D, F and G
Some do not have a Lancefield grouping as they do not have carbohydrates on their cell walls
Which streps are not in the Lancefield group?
S. pneumoniae
Virdidans
Does streptococci reduce nitrate?
Do not reduce nitrate to nitrites
What is the colony morphology of S. pneumoniae?
Alpha hemolytic, small, shiny, flattened and transparent colonies sometimes with concave (crater, checker piece, inner tube, tiny dime colonies) centers; can be mucoid, resembling oil droplets when the capsule this organism possesses is prominent.
What is the colony morphology of GAS (S. pyogenes)?
beta hemolytic, usually a tiny transparent colony with a large zone of beta hemolysis
What is the colony morphology of Group B Streptococci (S. agalactiae)?
Beta hemolytic, usually larger than group A and slightly more opaque. The zone of hemolysis is usually smaller in relation to the colony size compared to group A. Occasionally Gp B is nonhemolytic
What is the colony morphology of Group D strep?
non-hemolytic; colonies are glossier and whiter than Group A or B and look similar to Staph except the colonies are smaller
What is the colony morphology of Group C, F, or G Streptococci?
Can produce beta hemolytic colonies similar to Group A
What is the colony morphology of Viridans Streptococci?
Alpha hemolytic, smaller than S. pneumoniae; can be gamma hemolytic also.
What is the colony morphology of Enterococcus spp?
non-hemolytic; colonies are similar to the Group D. Streptococci.
What are the virulence factors of Streptococci?
hemolysin: Streptolysin O and S, responsible for beta hemolysis
m protein: protects from phagocytosis
streptococcal pyrogenic exotoxin: responsible for rash of scarlet fever and TS-like syndrome
capsule
DNAse and hyaluronidase
What does S. pyogenes cause?
Pharyngitis
scarlet fever
streptococcal pyoderma
Streptococcal toxic shock syndrome
Necrotizing fasciitis and myositis
What does S. agalactiae (GBS) cause?
Disease in neonatal and perinatal infants.
Early-onset: 12 hr to 5 days of life, babies present with bacteremia, pneumonia and meningitis. Given through live birth.
Late-onset: 7 days to 3 months, bacteremia with accompanying meningitis. Given nosocomially
What are group C, F and G beta hemolytic strep associated with?
infections in immunocompromised people
What is group D strep associated with?
Streptococcus bovis is associated with bacteremia and endocarditis in patients with colon and liver disease. It has also been associated with brain abscesses.
Enterococci are associated with?
E. faecalis and faecium.
Both species cause community-acquired and nosocomial infections including urinary tract infections (UTIs), bacteremia, endocarditis, wound infections, neonatal sepsis and abdominal and pelvic infections.
What does S. pneumoniae cause?
pneumonia
bacterial meningitis
What can Viridans Strep cause?
subacute bacterial endocarditis
Infection often acquired during dental procedures
mostly normal flora of the skin, urogenital, gastrointestinal and upper respiratory tract
What are nutritionally variant streptococci (NVS)?
strep that require thiol, cysteine or active form vitamin B12 to grow
Suspect when GPC are observed on a gram stain but fail to grow on blood agar or when pinpoint colonies grow next to S. aureus
What are some other strep-like organsims?
Abiotrophia, Granulicatella, Aerococcus, Gemella, Lactococcus, Leuconostoc, Pediococcus
What is PYR?
L-pyrrolidonyl-beta-naphthylamide hydrolysis test. GAS, nutritionally deficient strep and CNS are positive
What is the CAMP test and what is it used to identify?
Certain Staphylococcus aureus strains produce "beta-lysin" (a toxin). GBS produce "CAMP factor." Enhanced hemolysis is observed when CAMP factor and beta-lysin act synergistically on BA. The test involves streaking S. aureus down the middle of a BAP (blood agar plate). The test organism is then streaked perpendicular to the staphylococcal streak.
Used to ID GBS
What is Hippurate Hydrolysis and what is it used to identify?
GBS hydrolyze sodium hippurate to form glycine + benzoic acid
Used to ID GBS