KNES 323 2nd HALF
1/600
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
601 Terms
what is blood pressure?
hydrostatic pressure measure, the force exerted by blood upon the walls of the blood vessels or the chambers of the heart
what are the components of arterial blood pressure in larger vessels?
in aorta and brachial, systolic, diastolic, pulse, and mean arterial pressure
what is systolic pressure?
peak arterial pressure resulting from a ventricular contraction
what is diastolic pressure?
arterial pressure of blood during ventricular relaxation
how are diastolic and systolic pressure reported?
as a ratio of two numbers with systolic pressure over diastolic
what is pulse pressure?
difference between systolic and diastolic pressure, at least 25% of systolic pressure
what would be the pulse pressure of someone with systolic pressure of 120mmHg, and diastolic of 80mmHg?
40mmHg
what is meant by low/narrow pulse pressure?
pulse pressure <25% systolic pressure, may indicate low stroke volume as seen in congestive heart failure, stenosis of the aortic valve, or significant blood loss following trauma, poor circulation
what is meant by hide/wide pulse pressure?
common in healthy people during and following strenuous exercise, pulse pressure may increase temporarily to >100mmHg
what is meant by mean arterial pressure?
average pressure of blood in the arteries
how can we approximate MAP?
since cardiac cycle is about 1/3 in systole and 2/3 in diastole, adding 1/3 of pulse pressure to diastolic pressure, adding 1/3 systolic pressure to 2/3 of diastolic pressure
what are the 5 main variables affecting blood flow and blood pressure?
cardiac output, compliance, volume of blood, viscosity of blood, blood vessel length and diameter
what is cardiac output?
measurement of blood flow from the heart through ventricles
What will increasing CO result in?
increasing CO via HR or SV increases BP (ex: sympathetic stimulation, epi, norepi, thyroid hormones, increased Ca)
What will decreasing CO result in?
decreasing CO via HR or SV will decrease HR (ex: parasympathetic stimulation, altered K+ levels, decreased Ca)
what is compliance?
ability of a vessel to expand to accommodate increased content
what are the characteristics of a more compliant vessel?
able to expand with surges in blood flow without increased resistance or BP (veins are more compliant and can hold more blood)
when is compliance reduced and what is the effect of this?
arteries stiffen (hypertension) compliance is reduced and resistance to blood flow is increased, increases afterload and forces the heart to work harder when pumping blood
what happens to pressure and flow if blood volume decreases by >20%?
pressure and flow decreases (dehydration, vomiting, severe burns, diarrhea or bleeding)
what happens to pressure and flow if blood volume increases?
pressure and flow increase (retention of water and Na)
how does the viscosity of blood relate to flow?
directly proportional to resistance, any condition causing viscosity to increase will increase resistance and decrease flow rates
what are the two main determinants of blood viscosity?
formed elements, plasma proteins
how does vessel length relate to blood flow?
directly proportional to resistance, longer vessels have greater resistance and lower flow, shorter vessels have lower resistance and greater flow
how does blood vessel length change as we age?
increase in length as we grow and relatively unchanged in adults
how does decreased vessel diameter impact flow?
a decreased lumen diameter increases amount of blood contacting vessel walls, increasing friction and resistance and BP
what is Poiseuille’s law? What is the main idea behind it?
resistance is inversely proportional to the radius of the blood vessel raised to the fourth power
what does Poiseuille’s law state?
if an artery or arteriole constricts to half its original radius resistance to flow will increase 16 times, it it dilates twice its initial radius then resistance will decrease to 1/16 of original value
what is blood pressure predominantly determined by?
factors affecting cardiac output, blood volume, and vascular resistance
what factors help maintain pressure gradient between the veins and atria?
atria pressure (during diastole is low often approaching zero when atria are in diastole), physiological pumps (used to increase pressure and velocity of blood in the vein)
what is the function of the skeletal muscle pump?
increase the pressure in the veins through contraction of the surrounding skeletal muscles
what happens as leg muscles contract in the skeletal muscle pump?
exert pressure on nearby veins with their one way valves, causes blood to flow upward opening valves superior to the contracting muscles so blood flows through, valves inferior to contracting muscles close and prevents blood from flowing back towards the feet
what is the function of the respiratory pump?
aids blood flow through veins of thorax and abdomen
what is the role of the respiratory pump during inhalation?
volume of thorax increases and compresses the abdominal cavity, decreases air pressure and enables us to inhale, thoracic vein BP drops falling below pressure in abdominal veins, blood flows into thoracic region and promotes return of blood into the atria from thoracic veins
what is the role of the respiratory pump during exhalation?
air pressure increases in thoracic cavity, thoracic vein BP increases, increase velocity of blood flow to heart, valves in veins prevent blood from flowing backward from thoracic and abdominal veins
Why is mean arterial pressure not in the middle?
The time spent in systole vs diastole is not the same
Which key property does diastolic pressure determine?
After load
What does pulse pressure show you?
How efficient, smaller the number the more trouble the heart is having
If we have a low or narrow pulse pressure what does this indicate?
The system isn’t able to deliver nutrients to working body
What can extremely high blood pressures cause?
Cardiovascular failure, after load increases so heart has to work really hard and vessels are more stiff leading to more wear and tear, fatigue, thinning of walls, rupture
What do extremely low blood pressures lead to?
Brain impairments due to insufficient nutrient supply
how does the pressure in the brain and legs compare to the mean arterial Pressure ?
Higher in legs, lower in brain
How does high viscosity of blood impact the structure of the hearts vessels?
More wear and tear
Is vessel length or diameter more important in determining BP?
Diameter
What does Poiseuille’s law show you?
How changing vessel diameter impacts flow
If we have increased pressure due to constriction in one vessel how does this change blood flow?
Causes redistribution of blood to other vessels
What is mean arterial pressure determined by?
Factors affecting CO (effectiveness of heart as pump), blood volume (determined by fluid intake and loss, passive or regulated by kidney) and vascular resistance (determined by arterials diameter), distribution of blood between arterial and venous BV (determined by diameter of veins?
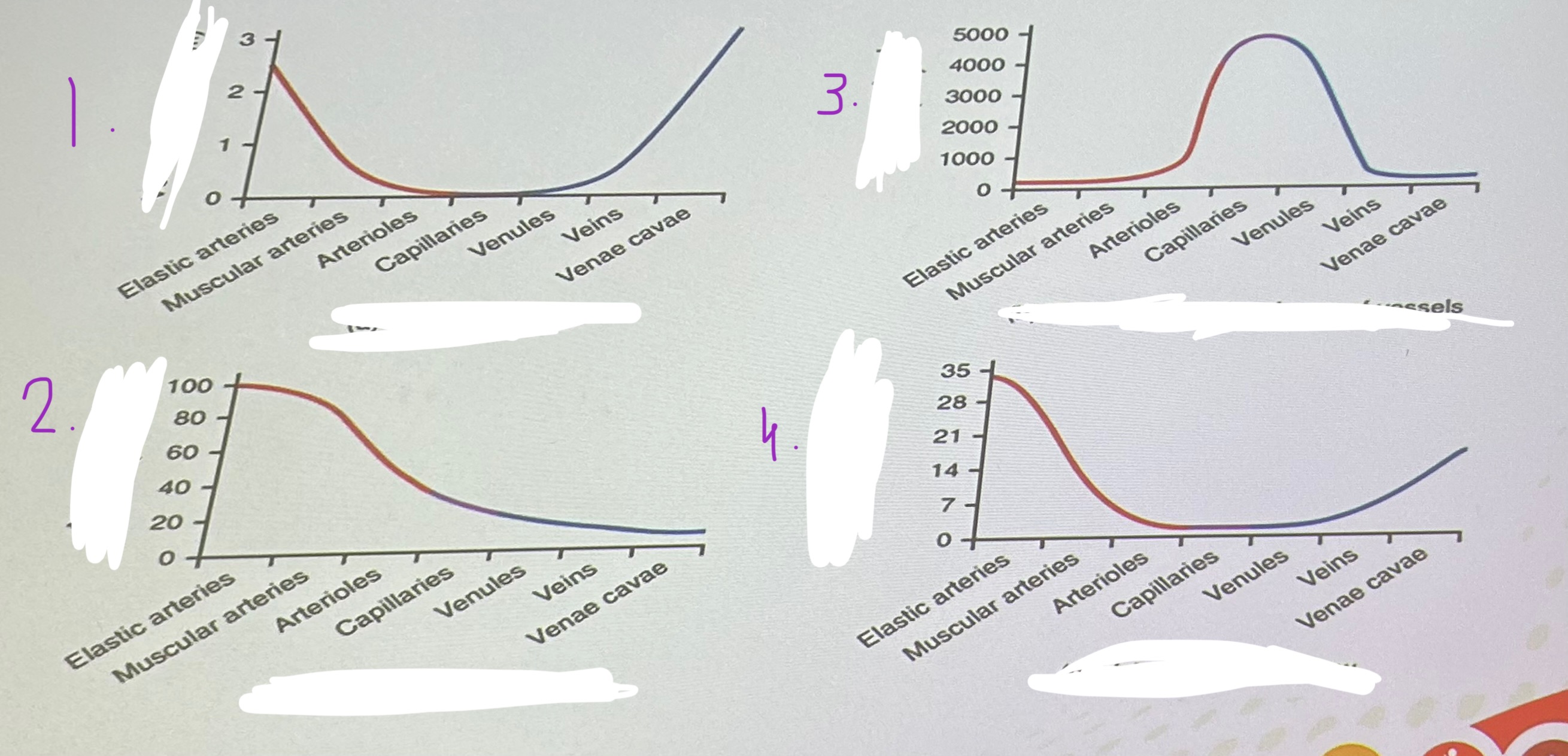
What key factor in relation to BP is shown in diagram one?
Vessel diameter
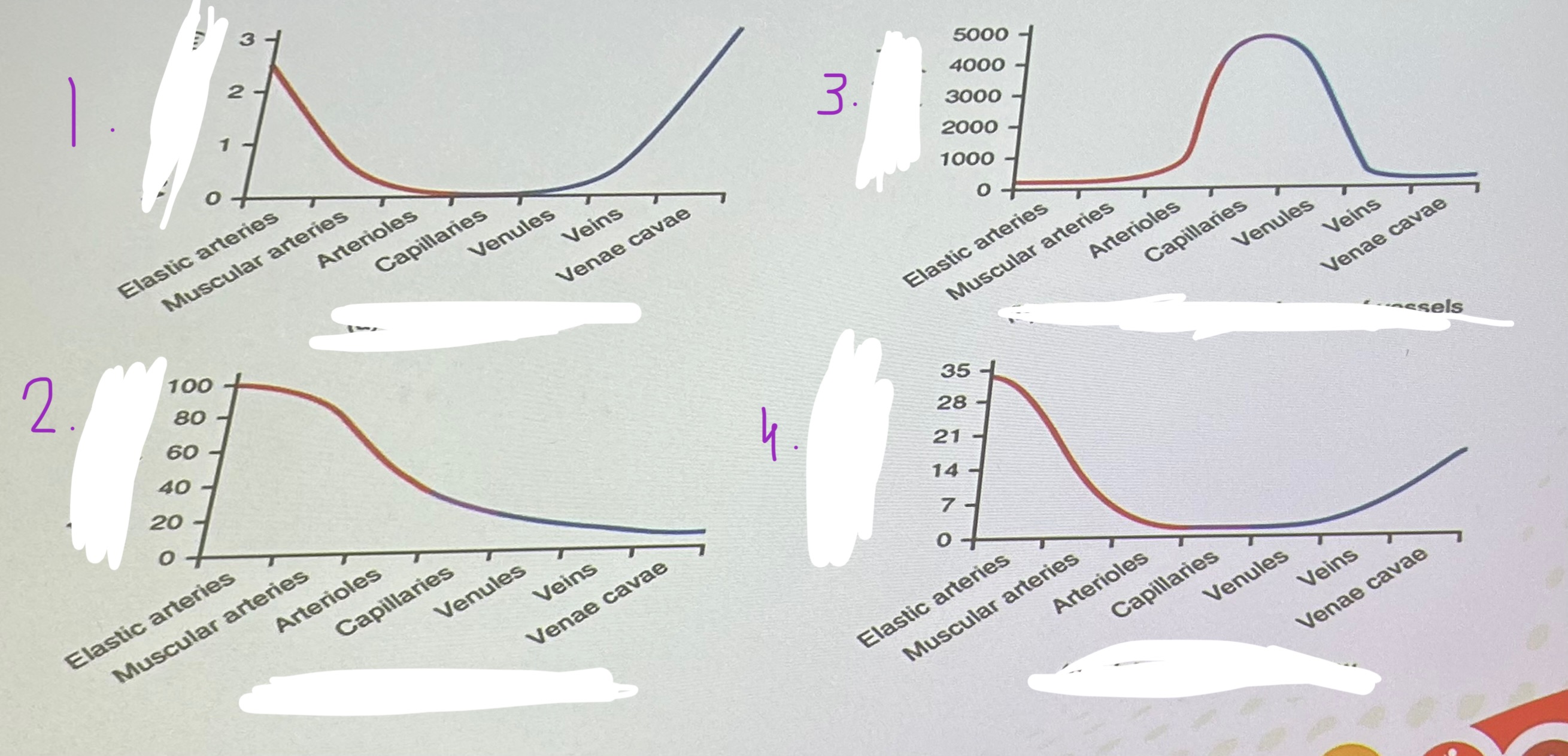
What key factor in relation to BP is shown in diagram TWO?
Average blood pressure
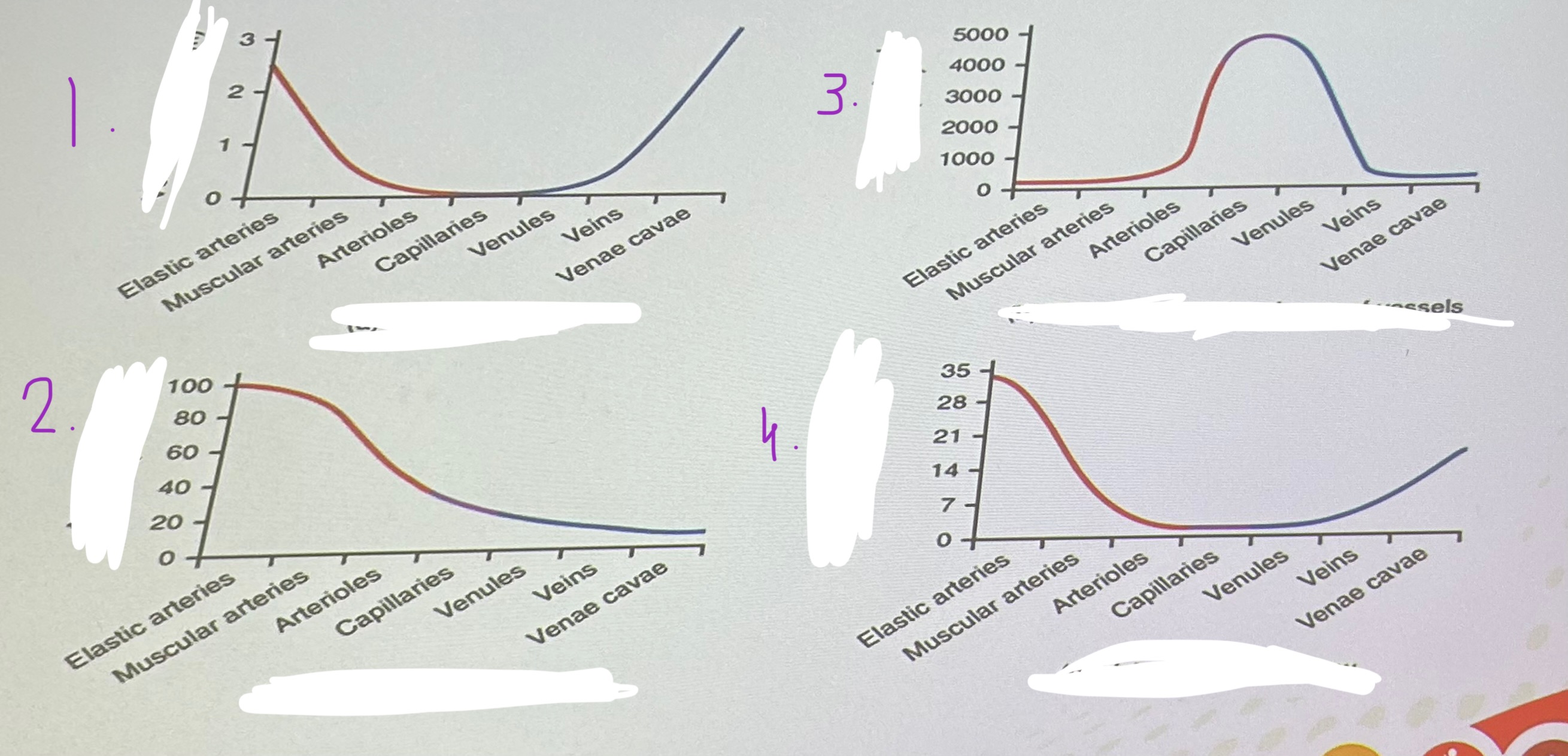
What key factor in relation to BP is shown in diagram THREE?
Cross sectional area
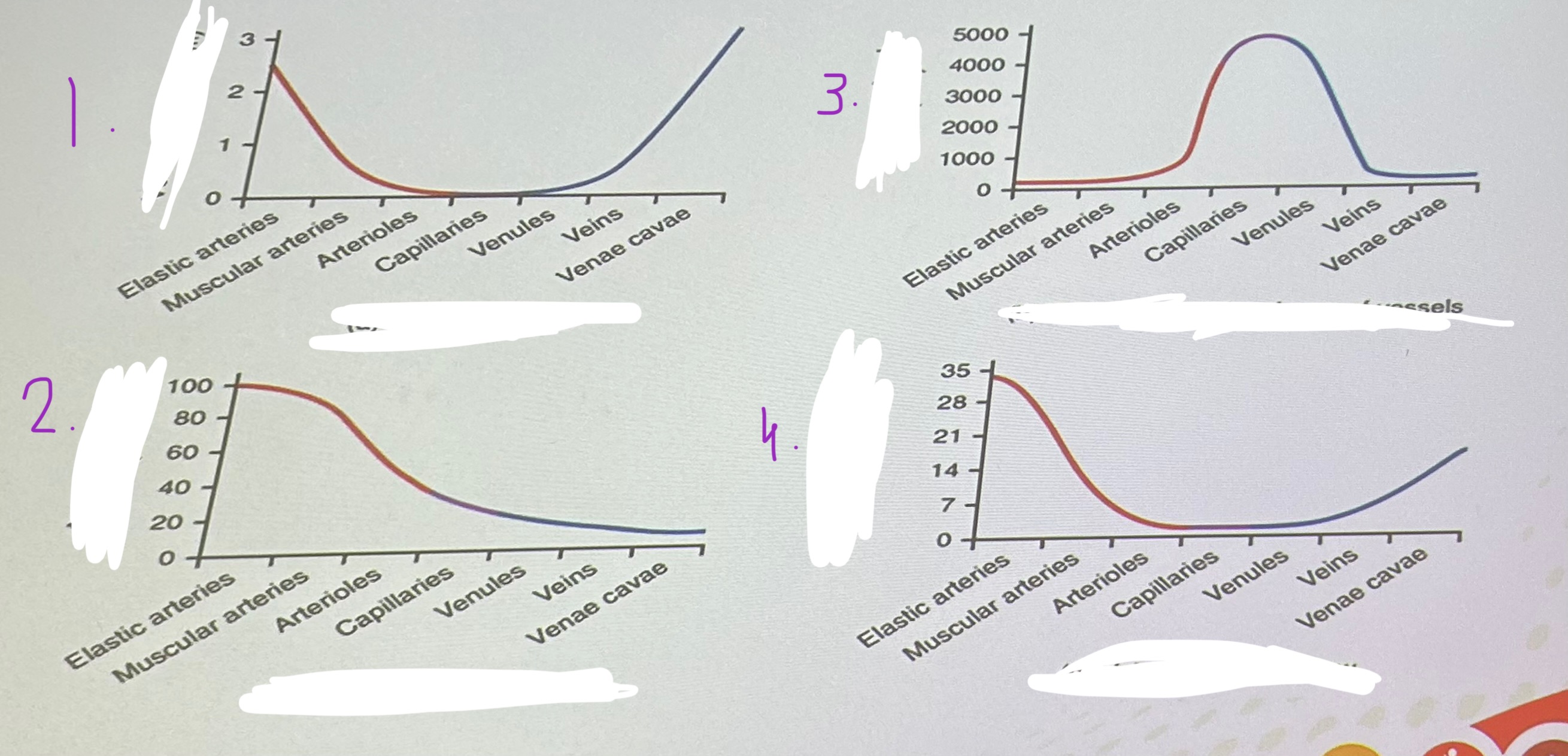
What key factor in relation to BP is shown in diagram four?
velocity of blood
how does cardiac suction impact venous return?
increase causes decrease in pressure in the heart and increase in pressure gradient
how does pressure imparted to blood by cardiac contraction impact venous return?
increase venous pressure and gradient
how does sympathetic vasoconstrictor activity impact venous return?
increase venous pressure and pressure gradient, decrease venous capacity
what is a key factor in ensuring adequate blood to tissues?
blood flow must be continually redirected to the tissues as they become more active
what are baroreceptors?
specialized stretch receptors located within thin areas of blood vessels and send impulses to cardiovascular center in the medulla oblongata to regulate BP
where are vascular baroreceptors typically found?
aorta and carotid sinuses
what is the role of stretch receptors if blood pressure falls?
receptors decrease their firing rates initiating sympathetic reflexes to accelerate HR, increase force of contraction and promote vasoconstriction
what is the role of stretch receptors if blood pressure rises?
receptors increase their firing rates initiating parasympathetic reflexes to decelerate HR, decrease force of contraction, and promote vasodilation
what is the relationship between HR and BP?
resting Bp and HR work like a teeter totter to maintain cardiac output as evenly as possible
what do chemoreceptors monitor?
levels of O2, CO2, and H+ (pH) to contribute to vascular homeostais
where are chemoreceptors found?
close to baroreceptors in aortic and carotid sinuses and transmit their signals to cardiovascular center and respiratory centers in medulla oblongata
what do chemoreceptors respond to? How do they change with increasing and decreasing CO2 and H+?
increasing CO2 and H+ levels (falling pH) by increasing CO and constricting peripheral vessels increasing return to lungs, decreasing CO2 and H+ levels (rising pH) by decreasing CO and dilating peripheral vessels decreasing return to lungs
what does neurological regulation of BP depend on?
cardiovascular centers in medulla oblongata
how do cardiovascular centers in medulla oblongata decrease cardiac function?
decrease HR and SV via parasympathetic stimulation
how do cardiovascular centers in medulla oblongata augment cardiac function?
regulating HR and SV via sympathetic stimulation
how do cardiovascular centers in medulla oblongata control vessel tone?
control vessel tone or contraction of smooth muscle in tunica media via vasomotor centres
how does the endocrine system play a role in managing the cardiovascular system?
through catecholamines (epi and norepi), and several hormones that interact with kidneys to regulate blood volume
what is the function of catecholamines?
enhance and extend the body’s sympathetic response, increase HR and contractile force, increase blood flow to liver, muscles, and heart, decrease blood flow to organs not essential for flight or fight responses (digestion, urinary)
what is ADH secreted by?
cells in the hypothalamus and released by posterior pituitary
what is the role of ADH in BP control?
signals kidneys to reabsorb more water, decreasing fluid lost in urine, increase overall fluid levels and help restore blood volume/pressure, small role in peripheral vessel constriction
what is the major effect of renin-angiotensin aldosterone mechanism on the cardiovascular system?
specialized cells in the kidneys secrete renin in response to decreased blood flow, renin activates angiotensinogen into angiotensin I, which is converted to angiotensin II in the lungs
where is angiotensinogen produced?
liver
what is the function of angiotensin II?
stimulates thirst in hypothalamus, powerful vasoconstrictor that increases BP, stimulates release of ADH and aldosterone increasing reabsorption of Na (and water) into blood by kidneys
what are the overall effects of the renin-angiotensin-aldosterone mechanism?
limit losses in blood volume, and vasoconstriction to raise BP
what is the thirst response?
as blood becomes more concentrated, blood osmolality increases above ideal value the hypothalamus transmits signals that result in conscious awareness of thirst
what are osmoreceptors?
sensory receptors in thirst center in hypothalamus that monitor the concentration of solutes (osmolality) of the blood
how does a person typically respond to thirst response?
respond by drinking water
When is atrial natriuretic hormone released?
secreted by cells in atria when blood volume is high enough to cause extreme stretching of the cardiac cells
how does ANH release relate to angiotensin II and BP control?
antagonists to angiotensin II, promotes loss of Na and water from kidneys, suppress renin, aldosterone, and ADH production and release
what is the overall effect of ANH?
promote loss of fluid from body so blood volume and BP decrease
what are the characteristics of autoregulation mechanisms?
don’t need specialized nervous stimulation or endocrine control, local, self-regulatory mechanisms that allow each region of tissue to adjust its own blood flow and perfusion
what do autoregulation mechanisms control in relation to BP?
control local blood flow through chemical and physical alterations
what is the role of chemical signals in BP control?
work at level of precapillary sphincters to trigger either constriction or relaxation
what are the effects of chemical signals in BP control?
dilating precapillary sphincter allows blood to flow in as a result of NO released from endothelial cells (decreased O2, increased CO2, histamine release), constricting precapillary sphincter temporarily shuts off blood flow as result of endothelins (vasoconstrictors) released from endothelial cells (increased O2 and decreased CO2, antihistamine release)
what is the role of physical signals in BP control?
work at myogenic level due to reaction to stretching of arteriole smooth muscles due to changes in blood flow , largely protective function against dramatic fluctuations in BP and blood flow to maintain homeostasis
what is the response to increased transmural pressure in BP control?
evokes myogenic response (bayliss effect) causing activation of Na and Ca channels in the smooth muscle layer of the blood vessel
what is a part of the short term control of BP?
baroreceptors, cardiovascular system
what is a part of the long term control of BP?
renal/blood volumes, endocrine function
what is the valsalva maneuver?
forced expiration against closed glottis, mimics many normal activities such as straining during defecation, blowing p a balloon, or playing the saxophone
what does performing a valsalva maneuver result in?
increase in intrathoracic pressure leading to reduction in preload to heart especially by restriction of IVC
what is phase I of the valsalva maneuver?
onset of strain, transient rise in BP because of emptying of some blood from the large veins and pulmonary circulation
what is phase II of the valsalva maneuver?
follows positive intrathoracic pressure leading to reduced venous return to heart, preload, SV, and BP falls activating baroreceptors, vagal withdrawal followed by increased sympathetic discharge ensues and marked tachycardia, increased CO and vasoconstriction leading to recovery of BP to normal
what is phase III of the valsalva maneuver?
transient phase involving release of strain leading to sudden dip in BP, release of positive pressure leads to expansion of pulmonary vascular bed and reduces left ventricular cross-sectional area resulting in a transient fall in BP
what is phase IV of the valsalva maneuver?
overshoot of BP above baseline, because of resumption of normal venous return to heart stimulated by sympathetic NS during phase II, overshoot leads to stimulation of baroreflex leading to bradycardia and return of BP to baseline
how many phases are their in the valsalva maneuver?
4
why do we have baroreceptors in the internal carotid?
we can monitor stuff going on in the brain, close to aorta
when blood pressure rises how do the stretch receptors cause vasodilation?
promote it by decreasing innervation of PNS, not direct reduction
what do the parasympathetic and sympathetic neurons impact in BP control?
parasympathetic impact heart, sympathetic impact veins, arterioles, ventricles, and heart
what does the input to cardiovascular centers include in BP control?
nerve impulses, from higher brain centers (cerebral cortex, limbic system, hypothalamus), proprioceptors (monitor joint movements), baroreceptors, chemoreceptors
what are the outputs to effectors from the cardiovascular center in the brain?
increased frequency of nerve impulses, decrease rate or increase rate and contractility in heart, vasoconstriction of BV