topic 3 - exchange & transport systems
1/115
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
116 Terms
What is digestion?
Breaking down large, insoluble molecules into small, soluble molecules which can be absorbed into the bloodstream
Which molecules don't need to go through digestion to be absorbed?
Already small molecules e.g. monosaccharides and minerals
What is the structure of the digestive system?
mouth, salivary glands ,esophagus, stomach, duodenum,jejuneum, illeum, large intestine, rectum, anus, liver, gallbladder
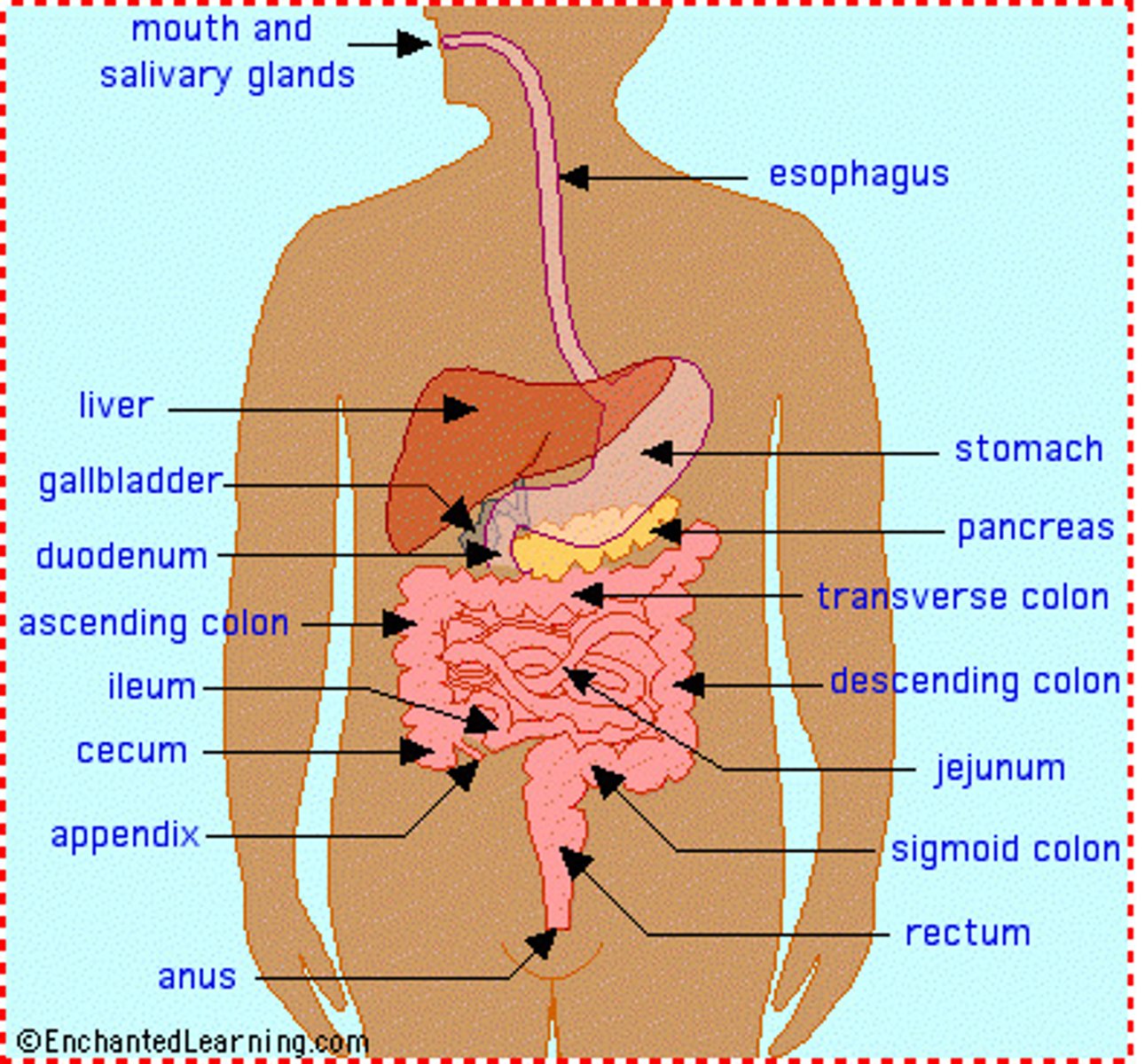
What is the structure of the small intestine?
duodenum - top part where enzymes from the pancreas & bile from the bile duct secrete into
jejunum - middle part where absorption begins of digestive material
ileum - last part where digested matter is absorbed
How is the polymer starch digested?
Amylase : first breaks down starch into maltoses by hydrolysing the alternate glycosidic bonds
Then membrane-bound disaccharidases : they hydrolyse the bonds in maltose to relase alpha glucose
Amylase is found in the salivary glands & pancreas where as the membrane-bound disaccharidases are found in the membrane of the epithelial cells in the illeum
What are the names of the different disacchardiases for the different disaccharides?
Sucrose - Sucrase
Maltose - Maltase
Lactose - Lactase
How are monosaccharides absorbed?
glucose and galactose are absorbed via co-transport with sodium ions; fructose passes via facilitated diffusion - all this happens across the epithelial membranes in the ileum and into the blood
What is the first step of lipid digestion?
The lipids are emulsified by bile salts to increase surface area.
Then lipase enzymes hydrolyse the ester bonds in triglycerides to form a monoglyceride and fatty acids.
This occurs in the small intestine but lipases are made in the pancreas.
What is the second step of lipid digestion?
Once the lipids are broken down into monoglycerides and fatty acids these molecules stick to bile salts.
This forms mielles which are tiny structures that constantly break up and reform releasing the monoglyerides etc.
This means they can be absorbed across the epithelial cell membrane through simple diffusion.
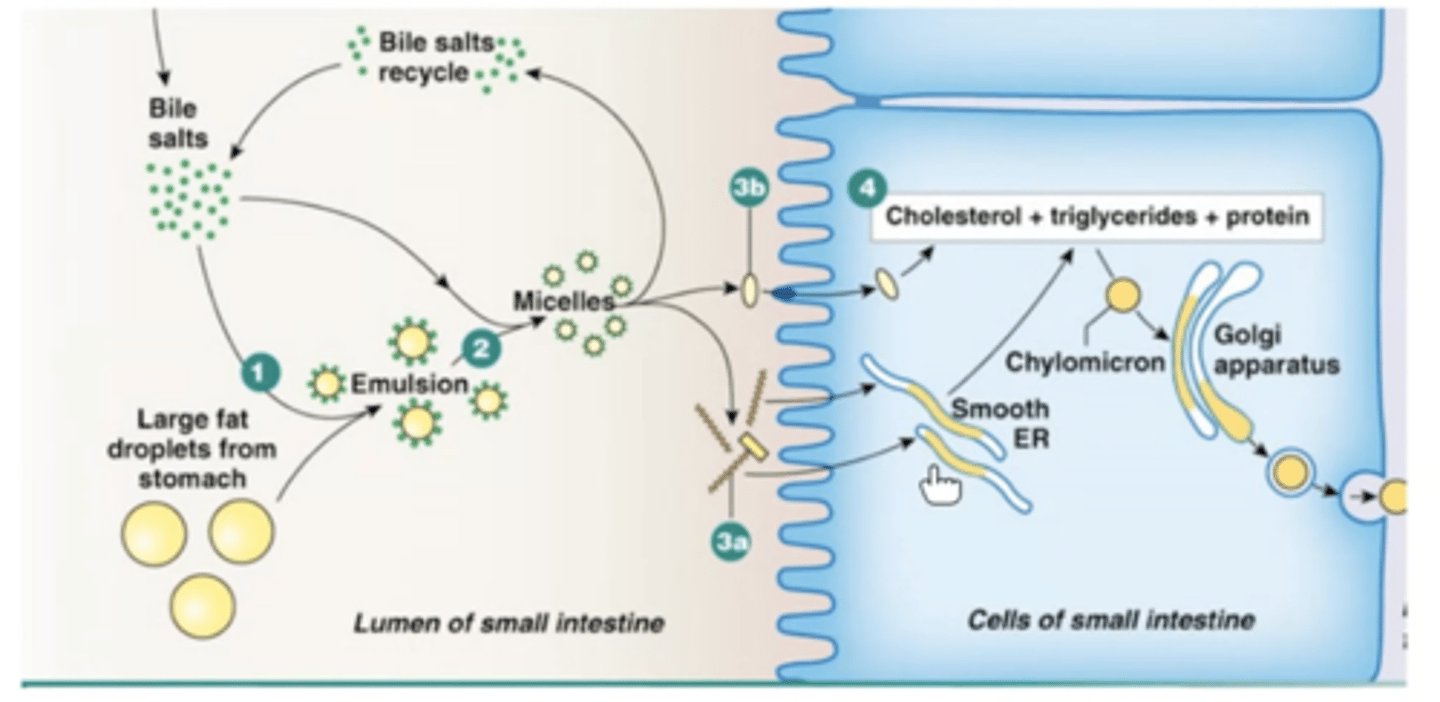
What doesn't happen in lipid digestion?
The mielles aren't absorbed! Only the molecules they release are absorbed.
What is the first step of protein digestion?
The proteins are broken down by 2 different peptidases.
- Endopeptidases hydrolyse the peptide bonds in a protein forming poly-peptide fragments
- Exopeptidases then hydrolyse the peptide bonds at the end of protein molecules removing one amino acid at a time
---> Dipeptidases are a type of exopeptidase that works on dipeptides specifically and breaks them into 2 amino acids
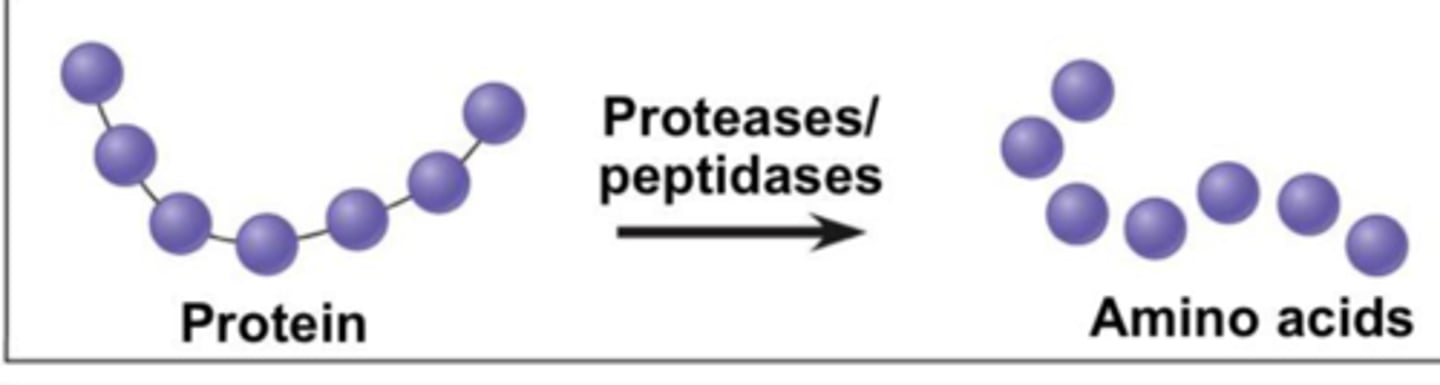
Where can the different types of peptidases be found in the digestive system?
Some are produced/found in the stomach - pepsin
Some are made in the pancreas and then secreted into the small intestine - tryprin & ohymotyprin
Dipeptidases are found on the cell surface of epithelial cells in the small intestine.
What is the second step of protein digestion?
The newly formed amino acids are absorbed in a similar way to glucose & galactose - co-transport with a sodium ion
How do single celled organisms carry out gas exchange?
They’re able to have substances diffuse in and out directly across the cell membrane as that’s the only “barrier”.
This allows for a fast diffusion rate because of the short diffusion distance
Why can multicellular organisms not use the same method of gas exchange as single celled organisms?
Diffusion across the outer membrane would be too slow:
Some cells are deep in the body - large distance between them & outside environment
Low surface area to volume ratio meaning there is too small of an outer membrane for all the cells in the body
This means multicellular organisms have to use specialized exchange organs & an efficient system to transfer substances to all cells.
What are the factors required for a fast rate of diffusion?
Large surface area - more substances at one time
Short diffusion pathway
Steep concentration gradient
What is the structure of the gas exchange system for insects?
Spiracles - small holes on either side of an insects body/exoskeleton through which gases leave or enter the body
Tracheae - large impenetrable system of tubes connected to a spiracle
Tracheoles - very small tubes which grow into & between body cells - where exchange actually happens
How can insects “ventilate”?
Insects can ventilate to a small extent through abdomen compressions which squeeze air out of the tracheoles etc
How do insects maintain a high rate of gas exchange when most active?
The tracheoles have fluid in their ends so when an insect is very active & lactic acid builds up in their cells the water/fluid is drawn into their cells. This is because the lactic acid build up decreases water potential.
This means there’s less water in the tracheoles so more air is in contact in the tracheoles with the tissues so more oxygen is diffused in & more CO2 can be diffused out.
How do insects reduce water loss?
The spiracles have muscular valves around them which can close to reduce water loss and hairs around the spiracles can trap moist air also reducing water loss.
How does an insects gas exchange system meet the factors for a high rate of diffusion?
Large surface area - many microscopic tracheoles which go all the way into all the cells
Short diffusion pathway - short distance from air in tracheoles to cells & from the spiracles to tracheoles - however limits size of insect
Steep concentration gradient - maintained through cells doing respiration & through ventilation of tracheae by abdominal compressions
What is the gas exchange surface for fish?
The gills which are made up of the gill arch, gill filaments & lamellae.
Why is it not advantageous for fish to have water as their respiratory medium?
Air is roughly 21% oxygen but water is only 1% oxygen so fish have to pass large quantities of water over their gills.
How do fish ventilate?
The fish can open its mouth increasing volume & so decreasing pressure so water moves in.
The fish then closes its mouth and squeezes water over the gills so diffusion occurs & out of the fish.
This movement keeps the concentration gradient high.
How does the structure of the gills make for an efficient gas exchange system?
Many gill filaments which increases surface area
Lamellae at right angles to filaments further increases surface area
Gills have a rich blood supply over the lamellae so look pink
What is the counter current system of the gills?
Blood & water flow over lamella in opposite directions.
The water flows across the lamellae from highly oxygenated blood to less oxygenated blood & them to deoxygenated blood
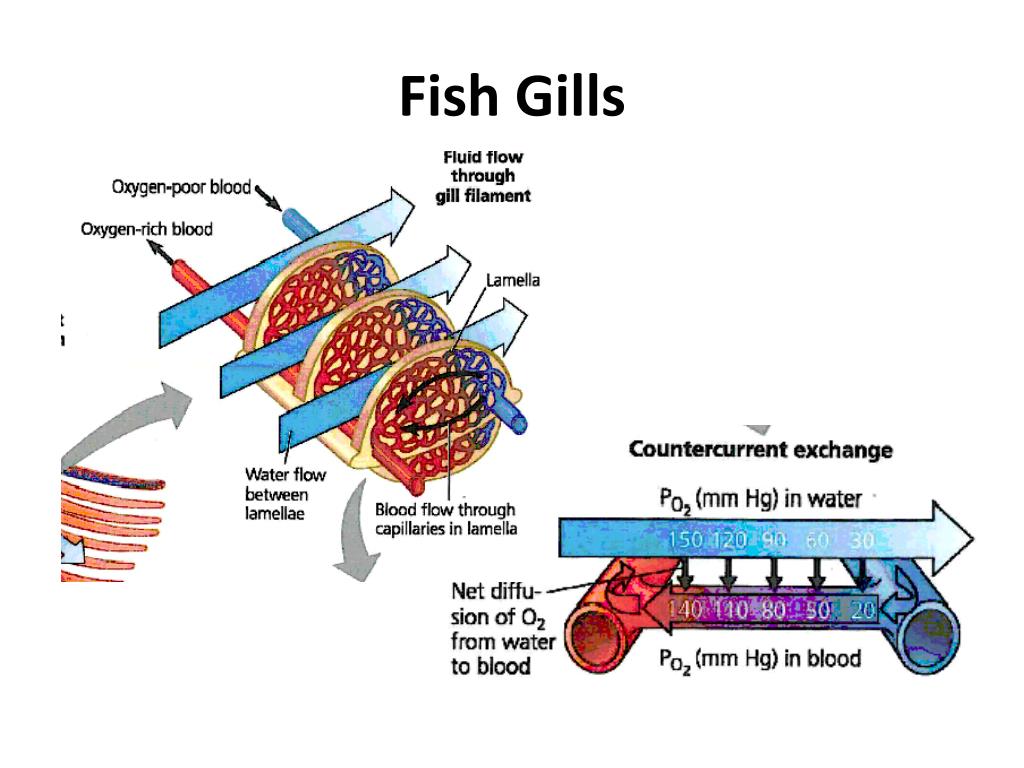
Why is the counter current system of the gills important?
Blood high in O2 meets water - max O2 conc - so O2 diffuses into the blood
Blood with little/no O2 meets water with most of the water removed O2 so O2 still diffuses into the blood
This doesn’t maximise the conc gradient but it does maintain it across the length of the gill plate so almost all of the O2 from the water diffuses into the blood via the lamellae.
What would happen if there wasn’t a counter current system?
The blood & water would eventually reach equilibrium while flowing across the gill plate etc so only 50% of the O2 in the water diffuses into the blood.
What is the structure of the human gas exchange system?
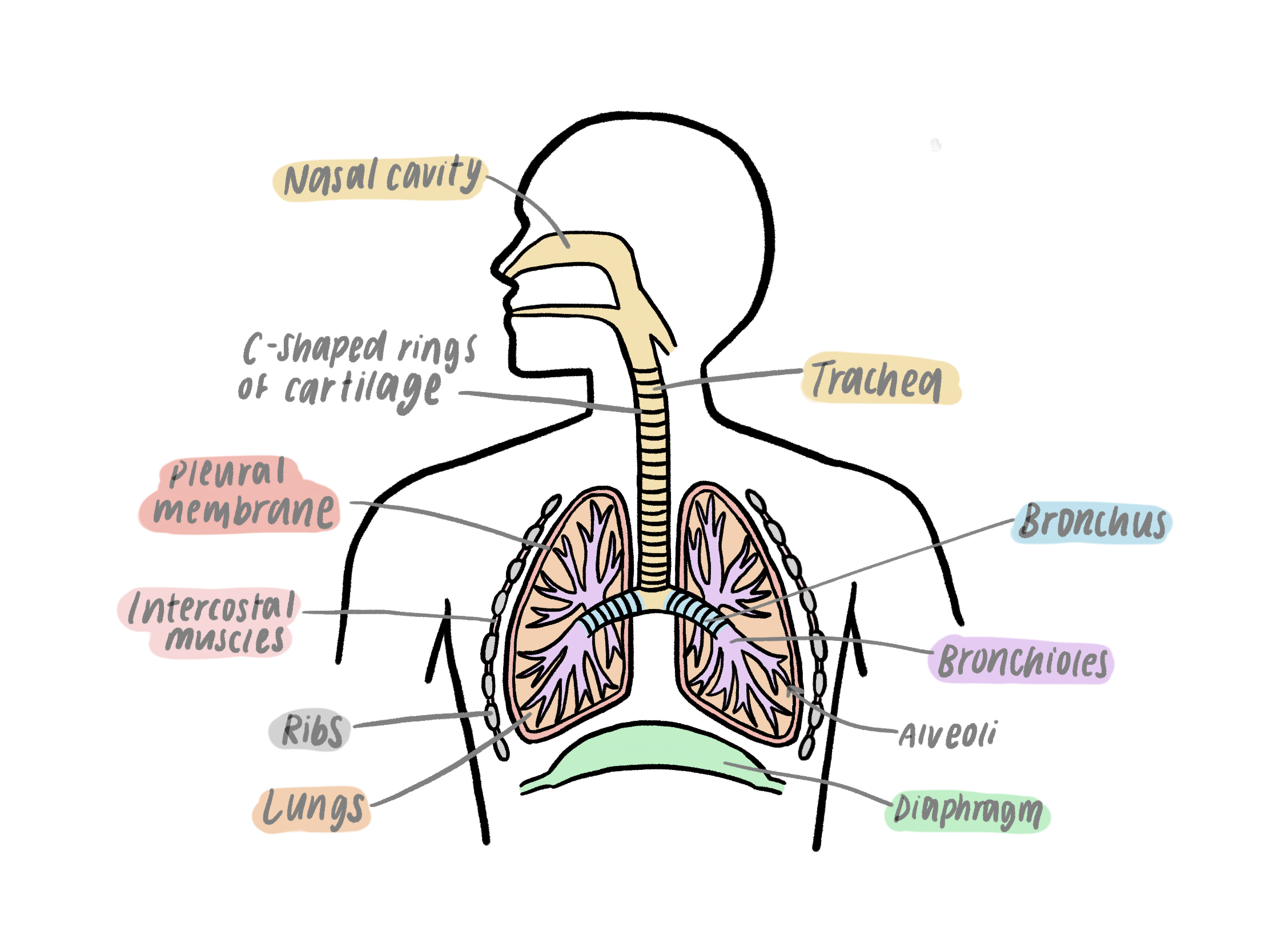
What are the lungs?
Pair of lobed structures made up of a series of branched tubules that end in tiny sacs called alveoli.
What are the bronchioles?
A series of subdivisions of the bronchi whoes walls are made with muscle and lined with epithelium cells. The muscle allows contraction and thus air flow into the alveoli.
What are the bronchi?
Bronchi = 2 bronchus where each one goes into each lung with a similar structure to the trachea. They also produce mucus to trap dust & dirt, cilia to move this towards the throat.
What is the trachea?
A flexible airway supported by rings of cartilage that prevent collapsing when breathing in. The walls are made up of muscle and lined with ciliated epithelial calls & goblet cells.
What are the alveoli?
Minute air sacs lined with epithelium with collagen & elastic fibres. These allow them to streach & recoil as ventilation occurs. Their membrane is the gas exchange surface.
How do alveoli achieve a very large surface area?
There are millions of microscopic air sacs - singular is an alveolus.
An alveolus also has a bumpy/ uneven shape which also increases the surface area compared to a perfectly spherical alveolus.
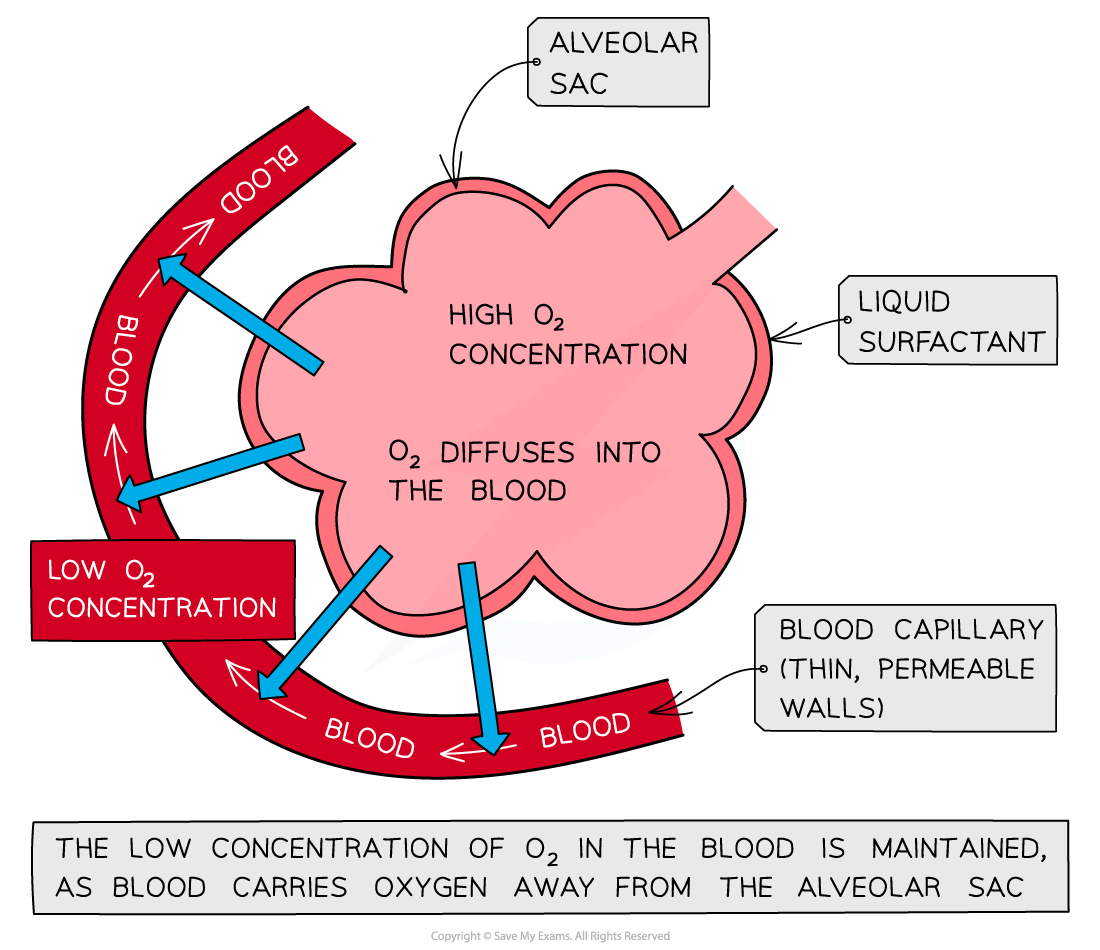
How is a steep concentration gradient maintained in the alveoli?
They have a very rich blood supply from the many capillaries surrounding the alveoli.
This means there is always a flow of blood transporting O2 away so deoxygenated blood is next to the alveoli.
The constant ventilation of the lungs also maintains a steep concentration gradient.
How do the alveoli ensure a short diffusion pathway?
Alveoli are made out of squamous epithelial cells.
Squamous epithelial cells are the most flattened/thinnest type of epithelial cell
This means the gases have a shorter distance to travel over so faster rate of diffusion.
What are expiration & inspiration (simple definitions)?
Expiration = breathing out
Inspiration = breathing in
How does ventilation occur in humans?
Inspiration - when atmospheric pressure is greater than the pressure in the lungs.
Expiration - when atmospheric pressure is less than the pressure in the lungs
What happens in inspiration?
External intercostal muscles contract
Internal intercostals relax
The ribs pull up and out
The diaphragm contracts causing it to flatten
Overall this causes the space in the thorax/chest cavity to increase so a reduction of the pressure in the lungs due to the increased space.
Air is forced into the lungs & avleoli expand and directly after this occurs the alveoli recoil in order to bounce back to their original shape forcing air & CO2 out.
What happens in expiration?
External intercostal muscles relax
The diaphragm relaxes returning to a dome shape
Unlike in inspiration
When and how is expiration an active process?
When someone is exercising, expiration becomes an active process as the internal intercostal muscles contract forming the ribs down. This reduces the volume of the thorax and increases pulmonary pressure.
This is done to increase breathing rate.
What are forced expiratory volume(FEV) and forced vital capacity?
Forced Expiratory Volume - maximum volume of air that can be breathed out - FEV1 is this but measured in one second
Forced Vital Capcity - maximum volume of air that you can force out of the lungs after a large breath in
What are the effects of tuberculosis?
Tuberculosis is a infectious disease caused by a bacteria.
When infected the immune system cells build a wall around the bacteria - tubercules where the tissue inside dies.
The damage to the alveoli reduces their surface area and so tidal volume.
This can also cause scarring - fibrosis - which further decreases tidal volume and increases the diffusion distance.Overall the rate of diffusion.
What are the symptoms of tuberculosis?
Someone with tuberculosis would experience a reduction of tidal volume so less air can be inhaled with each breath - ventilation rate increases
Persistent cough
Coughing up blood
Chest pains
Shortness of breath
Fatigue
What is fibrosis?
The formation of scar tissues due to infection - TB, exposure to asbestos etc
What are the effects of fibrosis?
Scar tissue makes the alveoli thicker so increases the diffusion pathway - reducing the rate of diffusion.
Scar tissue is also less elastic so tidal volume & FVC decreases due to inflexibility of alveoli.
What are the symptoms of fibrosis?
Faster ventilation rate
Shortness of breath
Dry cough
Chest pain
Fatigue & weakness
What is asthma/ an asthma attack?
Airways becoming inflamed & irritated often because of allergic reactions to pollen, dust etc.
During an asthma attack the smooth muscles lining the bronchioles contract making them narrow creating a difficulty to breathe which is furthered by a large amount of mucus being produced.
What are the effects of asthma/ an asthma attack?
Reduced air flow means the air in the lungs becomes stale so the conc gradient isn’t as steep and FEV1 is severely reduced.
Symptoms - wheezing, tighter chest & shortness of breath - this can be relieved with an inhaler which relaxes the smooth muscles in the bronchioles & airways
What is emphysema caused by?
Disease caused by long term exposure to air pollution & smoking.
Occurs when foreign particles get trapped in the alveoli causing inflammation attracting phagocytes which produce an enzyme that breaks down the elastin in the alveoli.
What are the effects of emphysema?
Breakdown of elastin by phagocytes means the lungs have less elastic recoil so don’t expel air as well - lowered con gradient.
In the long term it can lead to the destruction of the alveoli walls reducing the alveolis S.A by removing their bumpy shape - reduces rate of diffusion
What are the symptoms of emphysema?
Shortness of breath
Wheezing
Higher ventilation rate
The symptoms can be treated with oxygen if they are very severe.
What are the risk factors for lung diseases?
Smoking
Air pollution
Genetic makeup
Infections
Occupations
What is mass transport?
The bulk movement of gases or liquids in one direction, usually via a system of vessels and tubes.
Used by larger organisms which cannot simply diffuse substances to all cells in the body as there are many layers of cells etc - too large of a diffusion distance for the rate of diffusion to be fast enough.
What is the main mass transport system in mammals?
The circulatory system : the one-way flow of blood within the blood vessels carries essential nutrients and gases to all the cells of the body
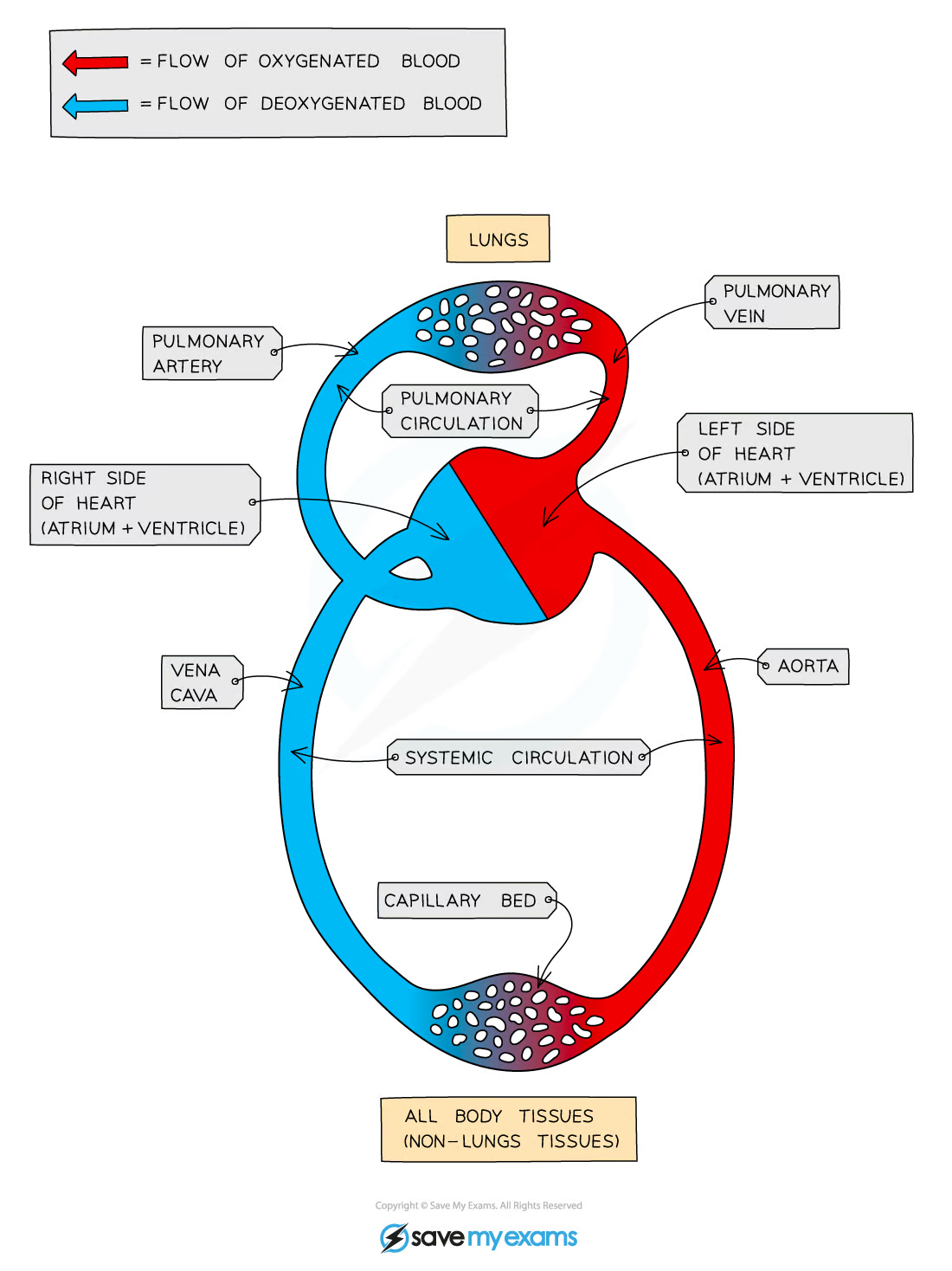
What does it mean for the human circulatory system to be a closed double circulatory system?
Closed - the blood is always contained in blood vessels as it’s pumped around the body.
Some animals e.g. molluscs have open systems where blood is pumped directly into body cavities
Double - in one complete circuit of the body the blood goes through the heart twice - first from the heart to the lungs then back through heart and into the body
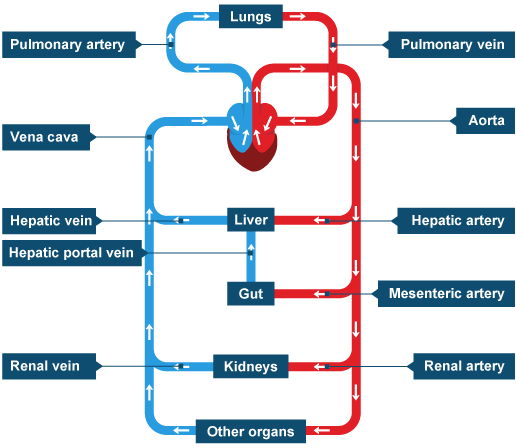
What are the pulmonary circulatory system & the systematic circulatory system?
Pulmonary circulatory system - the right side of the heart pumps blood deoxygenated blood to the lungs for gas exchange
Systematic circulatory system - blood then returns to the left side of the heart, so that oxygenated blood can be pumped efficiently (at high pressure) around the body
What are main body blood vessels to know?
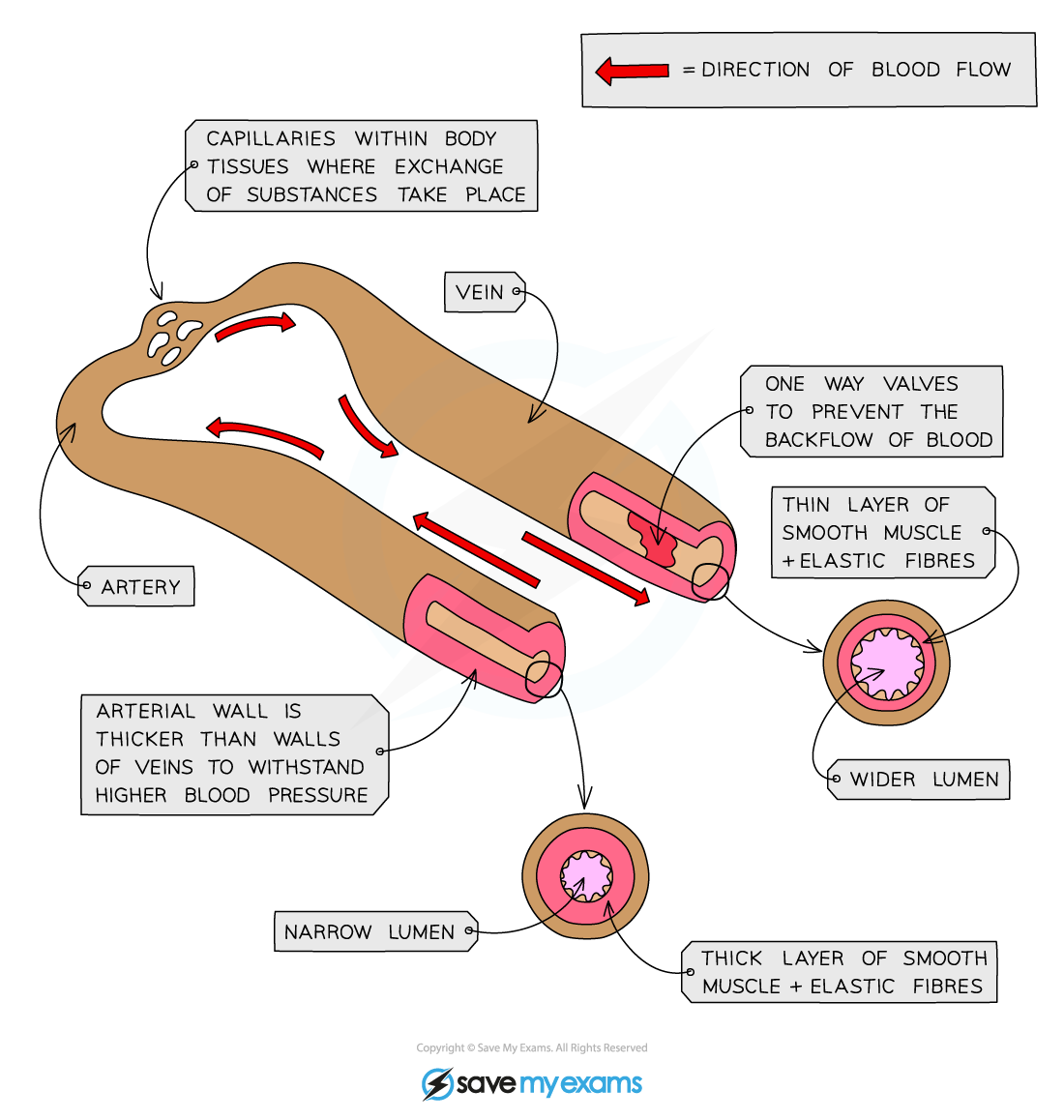
What is the structure of all larger blood vessels?
They have a 3 layer structure:
Inner layer = the endothelium - made up of a layer of flat squamous cells
this makes it smooth to prevent friction & prevent clotting so allows for smooth efficient blood flow
Middle layer - smooth muscle and elastin
elastin allows for recoil and stretch
Outer layer - connective tissue - made up of collagen
able to resist the pressure changes from within & outside the blood vessel
+ Lumen - the narrower the lumen the more pressure the blood is under
How are the structures of larger blood vessels - veins & arteries different to one another?
Arteries :
thicker smooth muscle & elastin layer lowers the pressure of the blood so capillaries don’t burst when given blood
and the stretch allows for recoil after a surge of blood to maintain blood pressure
arteries have smaller lumens in order to push blood everywhere around the body
Veins :
larger lumen in order to minimise the friction so blood goes back to the heart - thinner smooth muscle & elastin layer
contain valves in order to prevent the backflow of blood
What is haemoglobin?
Large protein found in red blood cells that is made up of 4 polypeptide chains joined to 4 haem rings which contain iron ions - making haemoglobin red and allow for 4 binding sites for oxygen.
What is the role of haemoglobin?
To carry oxygen around the body - it contains 4 binding sites for oxygen to allow for this.
What is the structure of haemoglobin?
Protein :
primary - order of amino acids in polypeptide chains
secondary - alpha helices
tertiary - individual 3D shapes the polypeptides fold into
quaternary - various subunits combined together - iron ions and the 4 polypeptide chains - the folding of the polypeptide chains makes a basket for the haem rings to sit in
What is meant by the loading/ association of oxygen to haemoglobin?
Loading/association = the non-permanent binding of oxygen to haemoglobin in RBCs to form oxyhaemoglobin
This occurs in the lungs/alveoli.
What is meant by the unloading/disassociation of oxygen to haemoglobin?
Unloading/disassociation = when the non-permanent bond between oxygen & haem in oxyhaemoglobin is broken so that the oxygen can be used by respiring cells.
This occurs by respiring cells and forms haemoglobin & oxygen - the haemoglobin can then be transported & associate with oxygen etc.
What causes dissociation & association of oxygen & haemoglobin?
The affinity of the haemoglobin - how easily it binds to oxygen - is influenced by the partial pressure of oxygen.
pO2 is a measure of oxygen concentration.
The greater it is the more association/loading occurs as the haemoglobin has a higher affinity & vice versa.
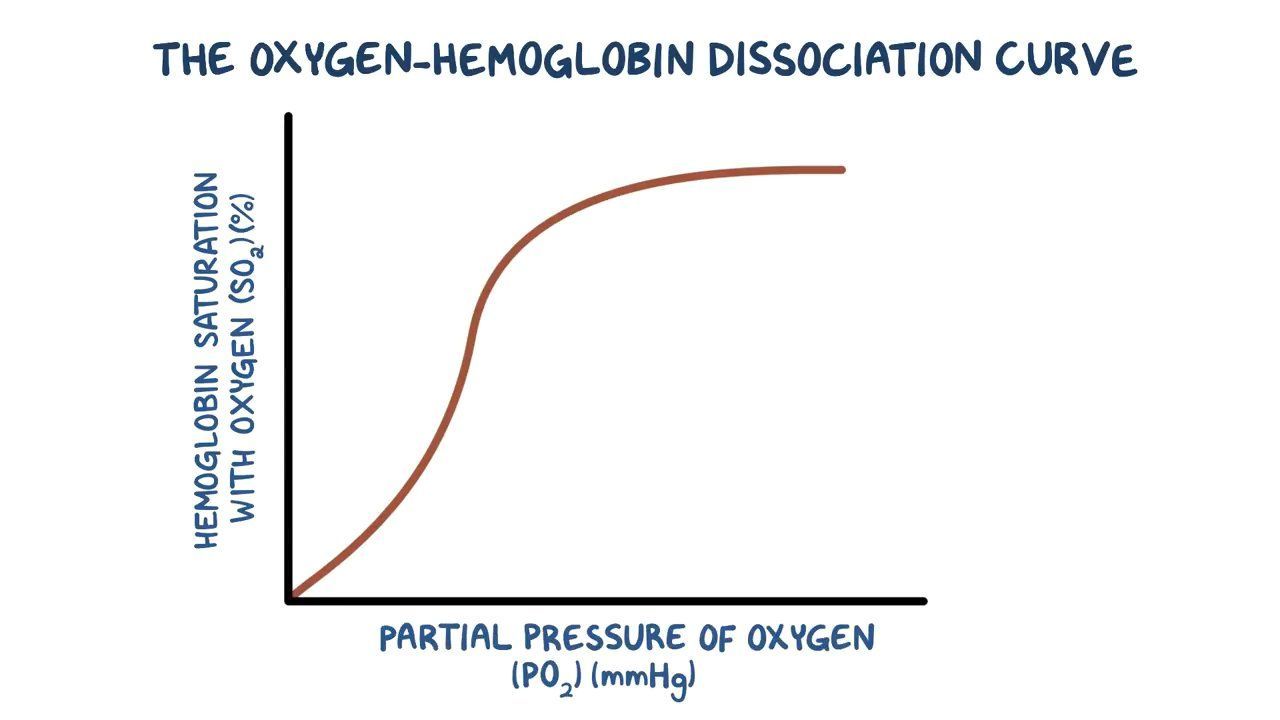
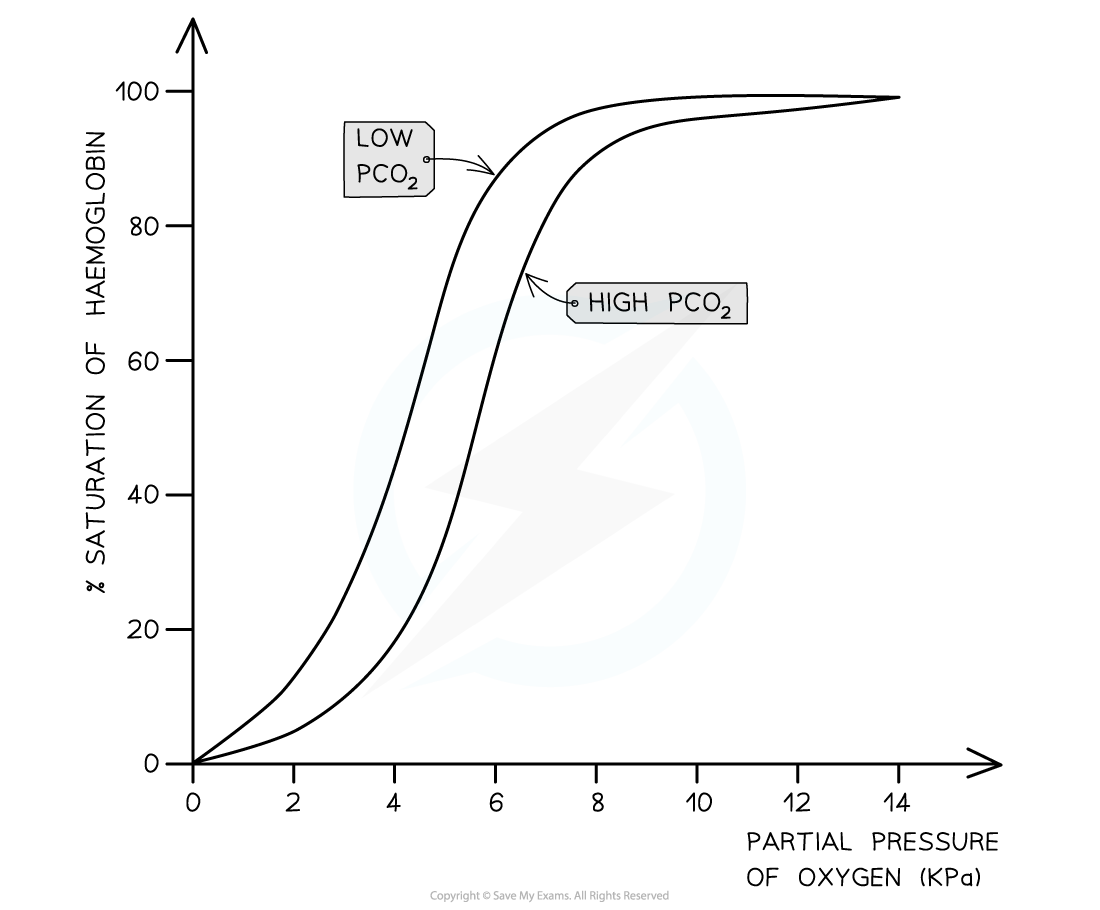
What is an oxygen dissociation curve?
X- axis = partial pressure of oxygen
Y axis = percentage saturation of a sample of haemglobin
100% means that all of the haemoglobin have bonded to oxygen but this depends also if all 4 binding sites are bonded to oxygen
What is the percentage saturation of haemoglobin?
(oxygenated haemoglobin/ max saturation) x 100
What does the S-shape of a dissociation curve show about the association/loading of haemoglobin?
It shows that it’s initally hard for oxygen to bind to haemoglobin but once the first oxygen molecule has bonded to a binding site it’s easier for the next 2 but become harder again for the 4th/last binding site & oxygen molecule.
we can see this through the changes in rate and percentage saturation
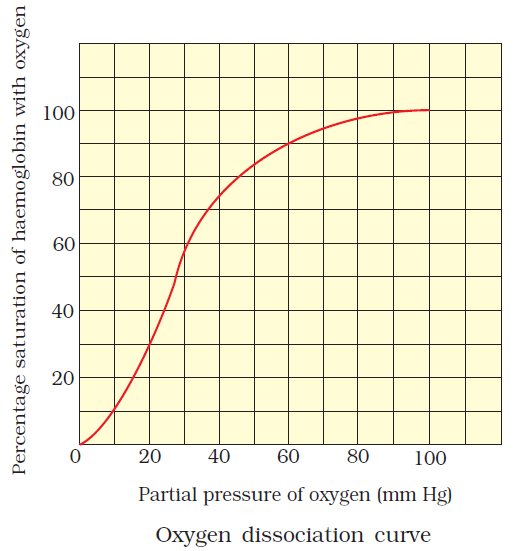
What can an oxygen dissociation curve show when read in terms of haemoglobin in the lungs vs in respiring tissues?
At the lungs there is high partial pressure of oxygen - most of the haemoglobin is saturated as oxyhaemoglobin
At the respiring tissues there is low partial pressure - lots of oxygen has been given up to the cells.
This hows that in the lungs the blood gets loaded with oxygen then by respiring cells the blood is unloaded so the oxygen can be used.
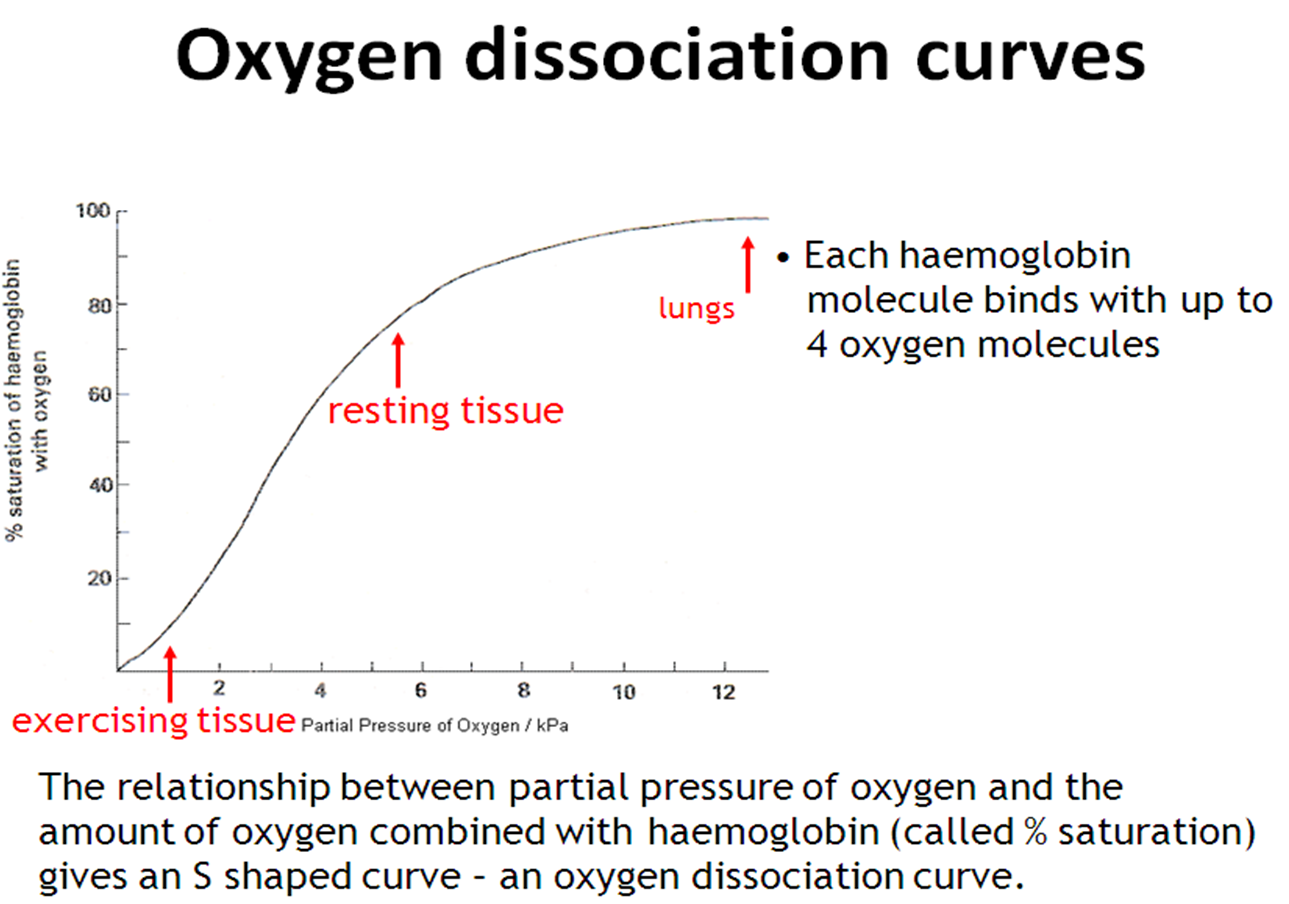
What can an oxygen dissociation curve show when read in terms of movement of blood from the heart to body?
The top of the graph shows that as the partial pressure gets lower across that section in the pulmonary veins & aorta, most of the haemoglobin is still in the form of oxyhaemoglobin.
This means oxyhaemoglobin carries oxygen molecules in the bloodstream from the lungs with very little unloading/dissociation until it reaches the respiring tissues far away from the lungs.
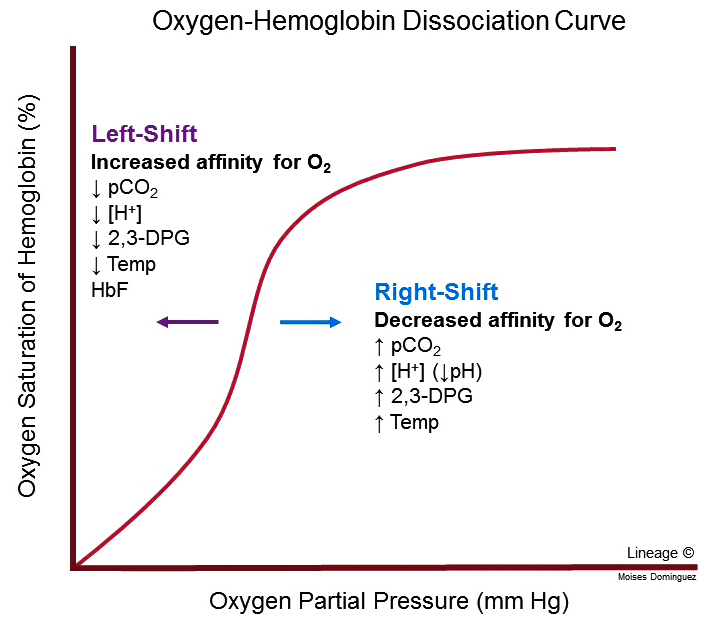
What is the Bohr Effect?
When there is more CO2 present, the oxygen dissociation curve remains s-shaped but shifts to the right - Bohr Shift. This means for a given partial pressure of oxygen, more oxygen will be dissociated compared to the “original" curve.
This can also be explained in terms of saturation e.g. normal curve = higher % saturation
The Bohr Effect states that haemoglobin will have less affinity for oxygen/ will bind less tightly as the concentration of CO2 increases.
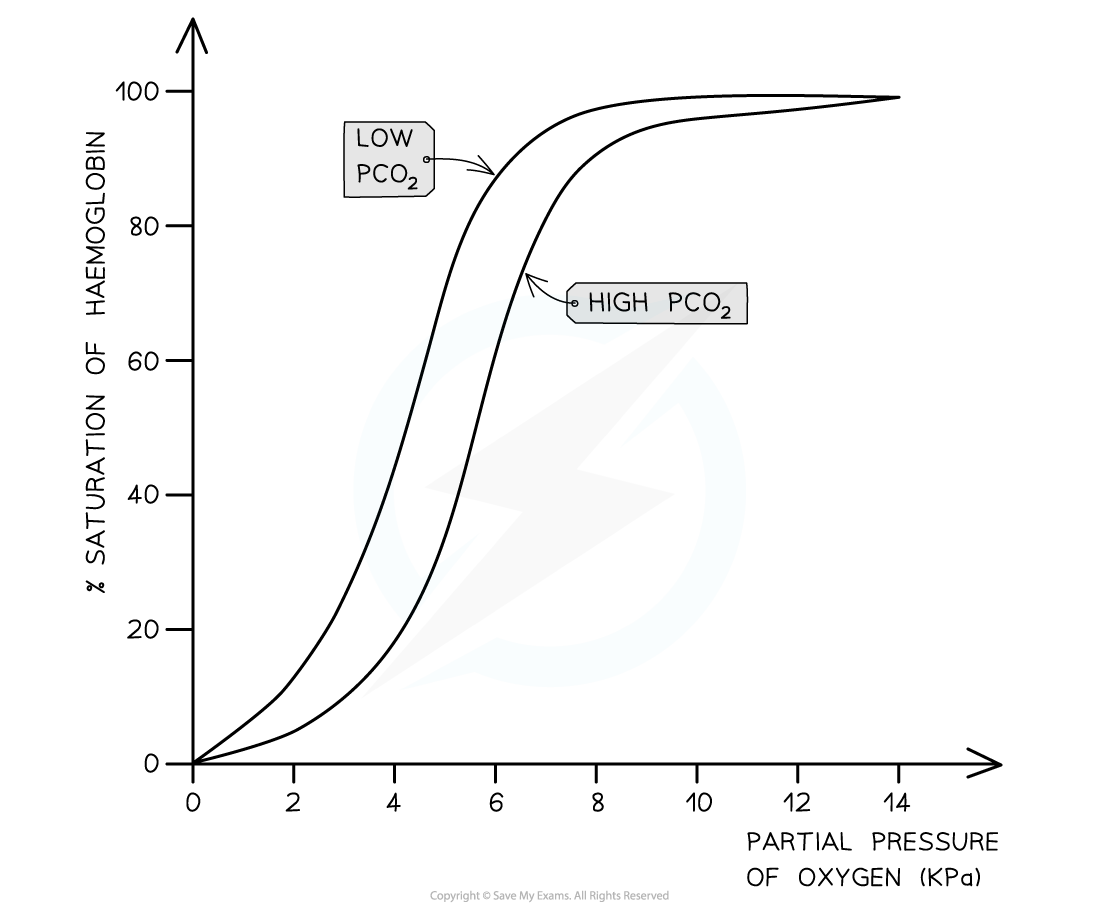
Why is the Bohr shift beneficial?
It means that respiring cells releasing lots of CO2 that need more oxygen obtain it by promoting the dissociation of oxyhaemoglobin.
What does myogenic mean?
Something that can be controlled both unconsciously and can change depending conditions.
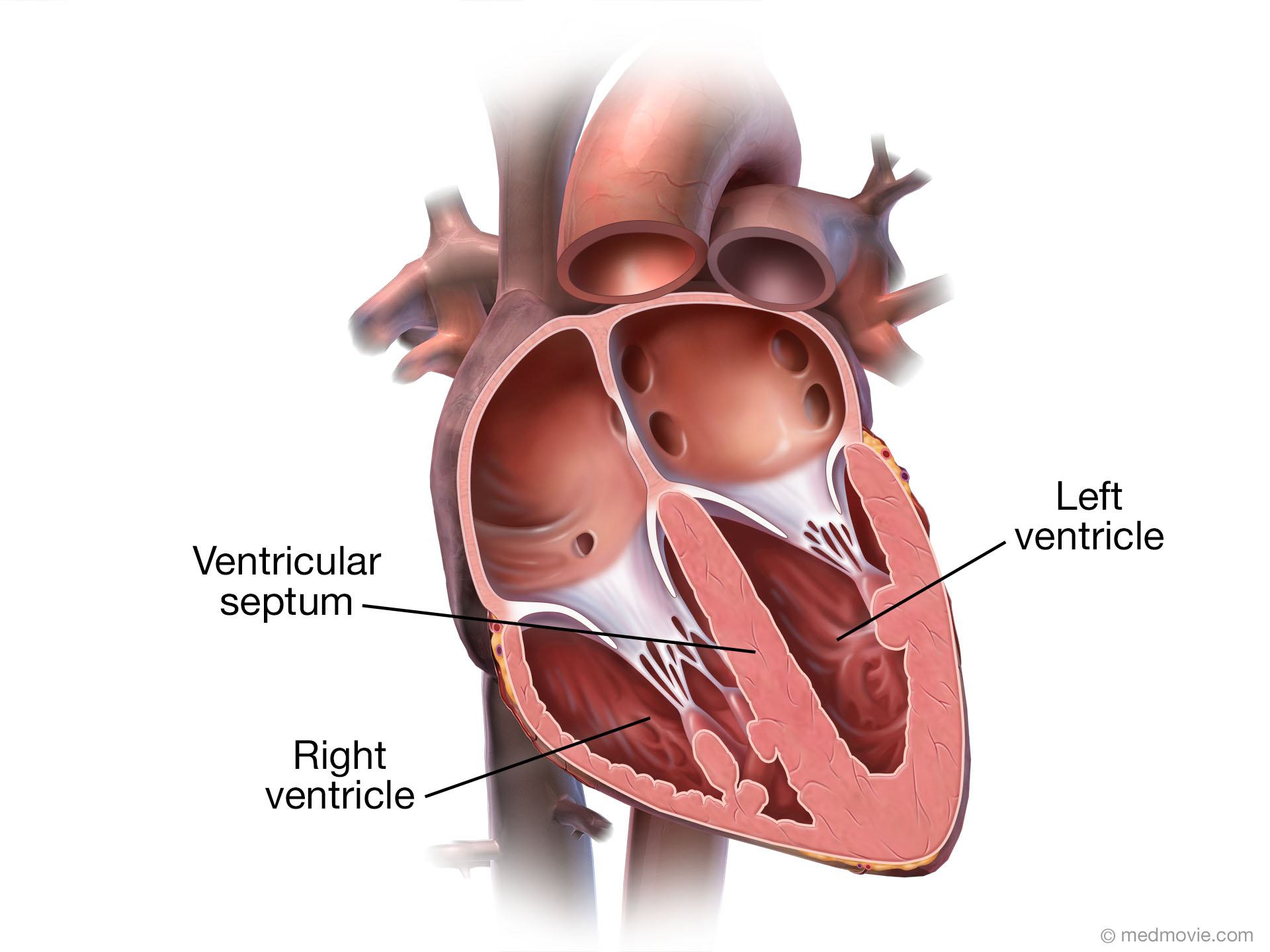
What is the structure of the heart?
Atria - left & right
Left ventricle
Right ventricle
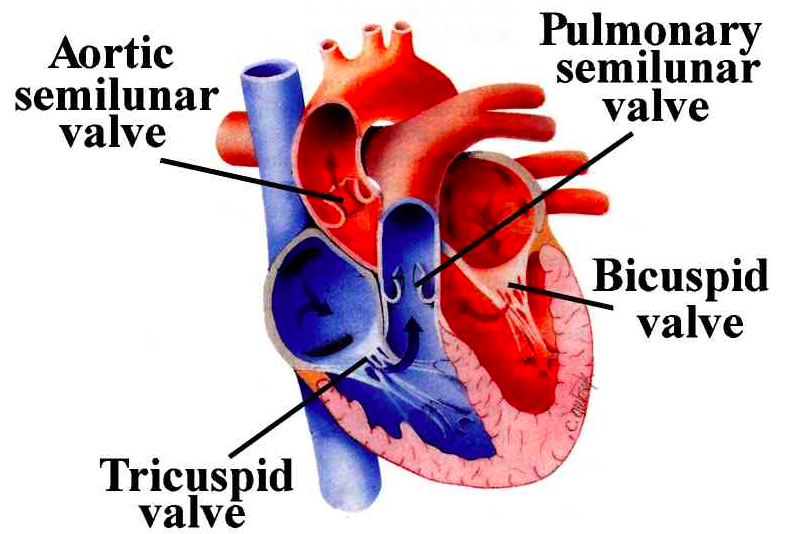
Atrioventricular valves
Semi Lunar valves
Aorta
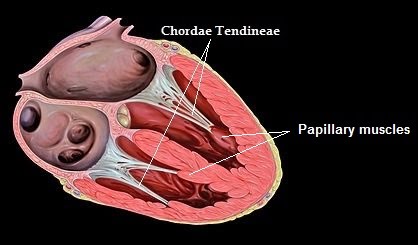
Tendinous Chords
+ reminder that heart diagrams have left & right as if you’re the person with the heart not the surgeon looking down
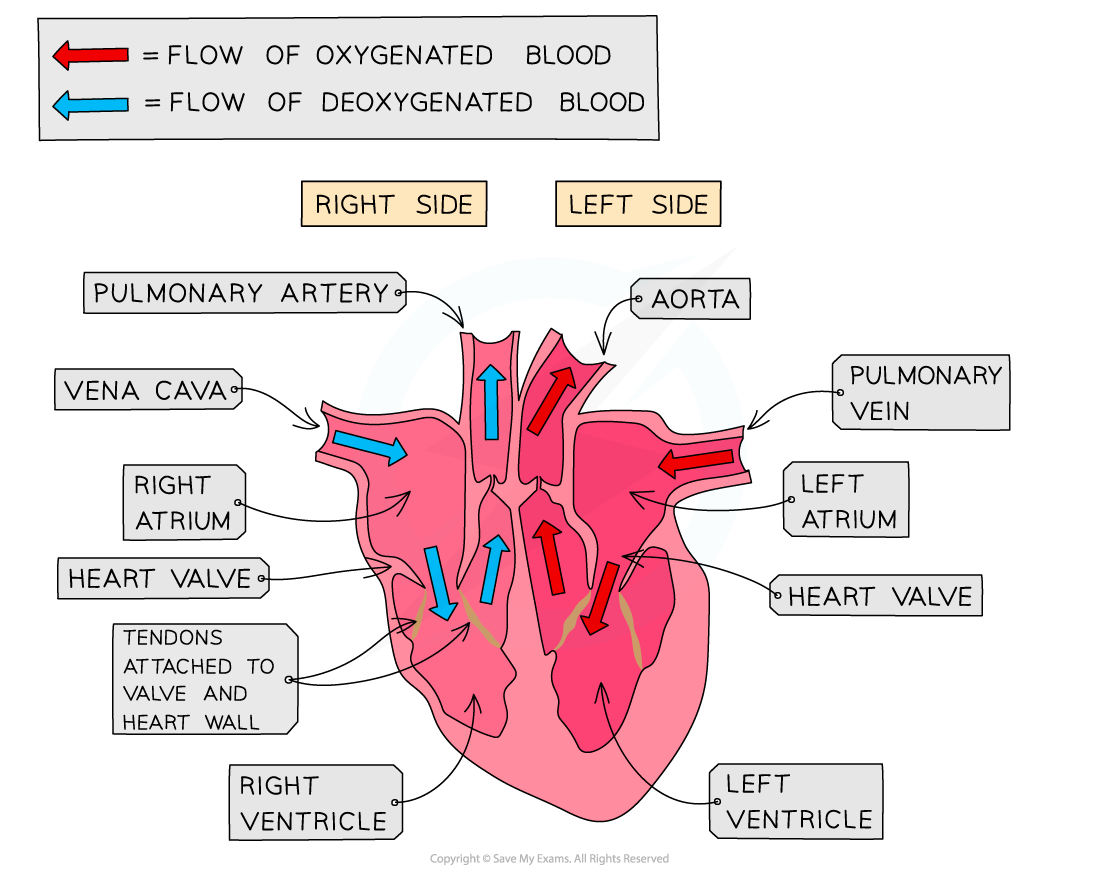
What are the atria and their function?
Small ,elastic, muscular chambers
Receive blood/ first chambers entered by the blood
Tiny chambers compared to the ventricles but are able to hold the same volume of blood due to their stretchiness
Right atrium receives blood from body
Left atrium receives blood from the lungs
What are the ventricles and their functions?
Both are larger muscular chambers
Pump blood out of the heart
Left ventricle has thicker more muscular walls allowing for more powerful contractions so blood is pumped all around the body
Right side pumps blood only to the lungs so doesn’t need to be as muscular etc
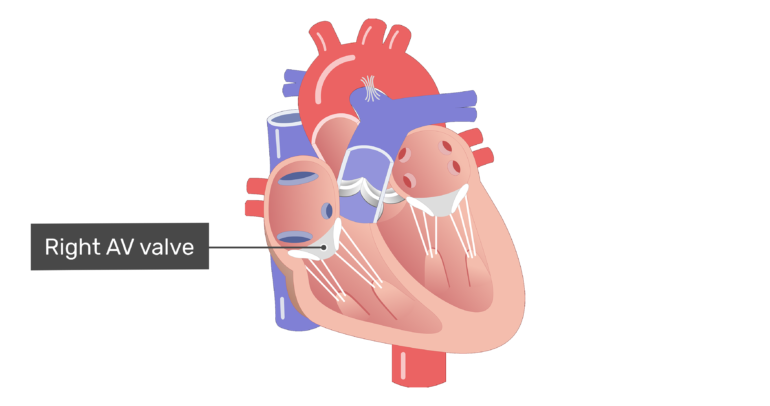
What are the atrioventricular valves and their function?
Found between atria and ventricles & link the two
Allow the one way flow of blood from atria to ventricle but not the other way around
If the valves are functioning normally there should be no back flow into the atria
What are the semilunar valves and their function?
Have a half moon shape
Found between the ventricles and the pulmonary artery on left and aorta on the right and links them together
Stop blood flowing back into the heart after the ventricles contract
What are the tendinous chords and their function?
Very strong collagen fibres
Hold the valves in place
Control the movement of the valves as the valves themselves are fragile
Why are there different types of haemoglobin?
Different types of haemoglobin comes around from the molecule’s DNA having a mutation so there’s a slightly different primary structure etc etc.
This can change the affinity of the haemoglobin so it’s more adapted to the oxygen availability of a species habitat.
What are the different types of haemoglobin to remember?
Haemoglobin in conditions in active muscle
Foetal haemoglobin
Lugworm haemoglobin
Llama haemoglobin
Shrew haemoglobin
Myoglobin - not actually haemoglobin but still need to know
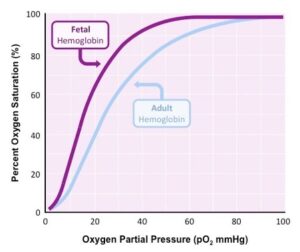
How is foetal haemoglobin different to normal haemoglobin and why is this difference necessary?
Foetal haemoglobin has a higher affinity to oxygen - this is seen as a shift to the left compared to normal haemoglobin.
This means that at the same partial pressure the F.haemoglobin loads while the maternal haemoglobin unloads. This allows the f.haemoglobin to take oxygen from the m.haemoglobin.
A higher affinity is also required because foetuses get oxygen from the placenta not the lungs - there will never be 100% saturation like in the lungs. The higher affinity means the f.haemoglobin is able to get all the oxygen from the m.haemoglobin that it requires.
How is a lugworm’s haemoglobin different to human haemoglobin and why is this difference necessary?
Lugworms have a greater affinity to oxygen compared to human haemoglobin - this is seen as a shift to the left.
This allows them to load oxygen at lower partial pressures than humans in order to load as much oxygen as possible which is necessary because lugworms live in sandy condition = less oxygen available.
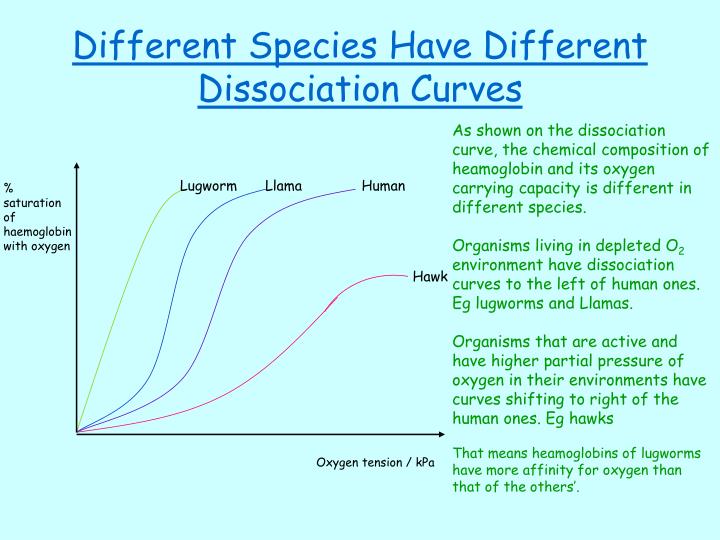
How is a llama’s haemoglobin different to human haemoglobin and why is this difference necessary?
Llama haemoglobin has a higher affinity to oxygen than human haemoglobin - this is seen as a shift to the left.
This means the haemoglobin is able to become saturated at lower partial pressures of oxygen which is necessary as llamas live at high altitudes = less oxygen available.
How is a shrew’s haemoglobin different to human haemoglobin and why is this difference necessary?
Shrew haemoglobin has a lower affinity to oxygen than human haemoglobin - this is seen as a shift to the right.
This means that oxygen is more readily unloaded to respiring cells which is necessary as shrew’s have a higher metabolic rate and a higher surface area than humans.
They still get saturated at high partial pressures like humans but have a lower affinity.
What is myoglobin?
Myoglobin is not a type of haemoglobin but it is a similar protein.
It acts as an oxygen store so it picks up oxygen readily but will only give it up/unload at very low partial pressures.
Myoglobin is found in most muscle tissue but is particularly common in marine mammals.
What is the “key” for disassociation curves?
Right shift - lower affinity to oxygen & unloading is more important
found in shrews - higher metabolic rate, animals with higher oxygen availability - hawks and in the Bohr Effect
Left shift - greater affinity of oxygen & loading is more important
found in animals etc with lower oxygen availability- foetal, llamas & lugworms
How and why is the myoglobin dissociation curve so different to a haemoglobin dissociation curve?
It’s so different because myoglobin has a very high oxygen affinity compared to haemoglobin in order to act as an oxygen store.
This means it will associate with oxygen readily but only disassociate at very low partial pressures.
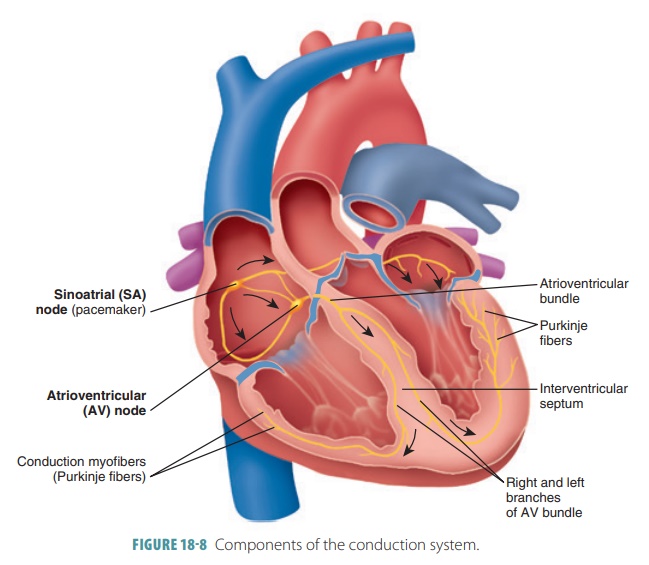
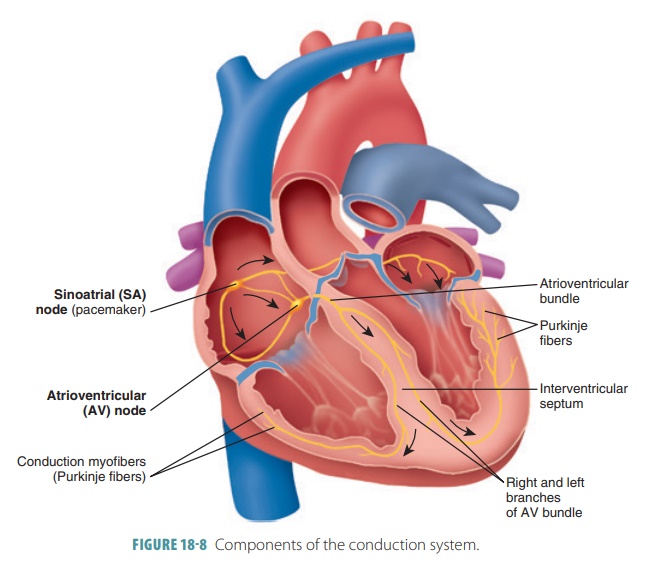
What are the structures involved in the pathway of an impulse during a heartbeat?
Sino-atrial node - the pacemaker - found in the right atrium
Atrioventricular node - sits centrally between the atria and ventricles
The Bundle of His - found along the papillary muscle
Purkinje Fibres - found in the lower muscles surrounding the ventricles
What impulses happen during a heartbeat?
The sino-atrial node sends an impulse
The atria contract/empty
The impulse from the sino-atrial node is passed to the atrioventricular node
There it’s held onto for a tiny bit and then continues to flow
This allows for the atria to completely empty
The impulse is passed onto the Bundle of His
Here the impulse is slowed by the nerves having more insulation than a normal nerve
The impulse is then passed to the Purkinje fibres
The impulses cause the ventricles to contract so all the blood from the bottom is emptied into the artery etc
What is the cardiac cycle?
The series of events that take place in one heart beat, including muscle contraction and relaxation
What is required for a valve to open?
The pressure behind it is higher than the pressure after it.
The valves in the heart are one way so will not open if the blood pressure is higher after it than before it.
What are the 3 stages of the cardiac cycle?
Atrial systole
systole = contraction
Ventricular systole
Diastole
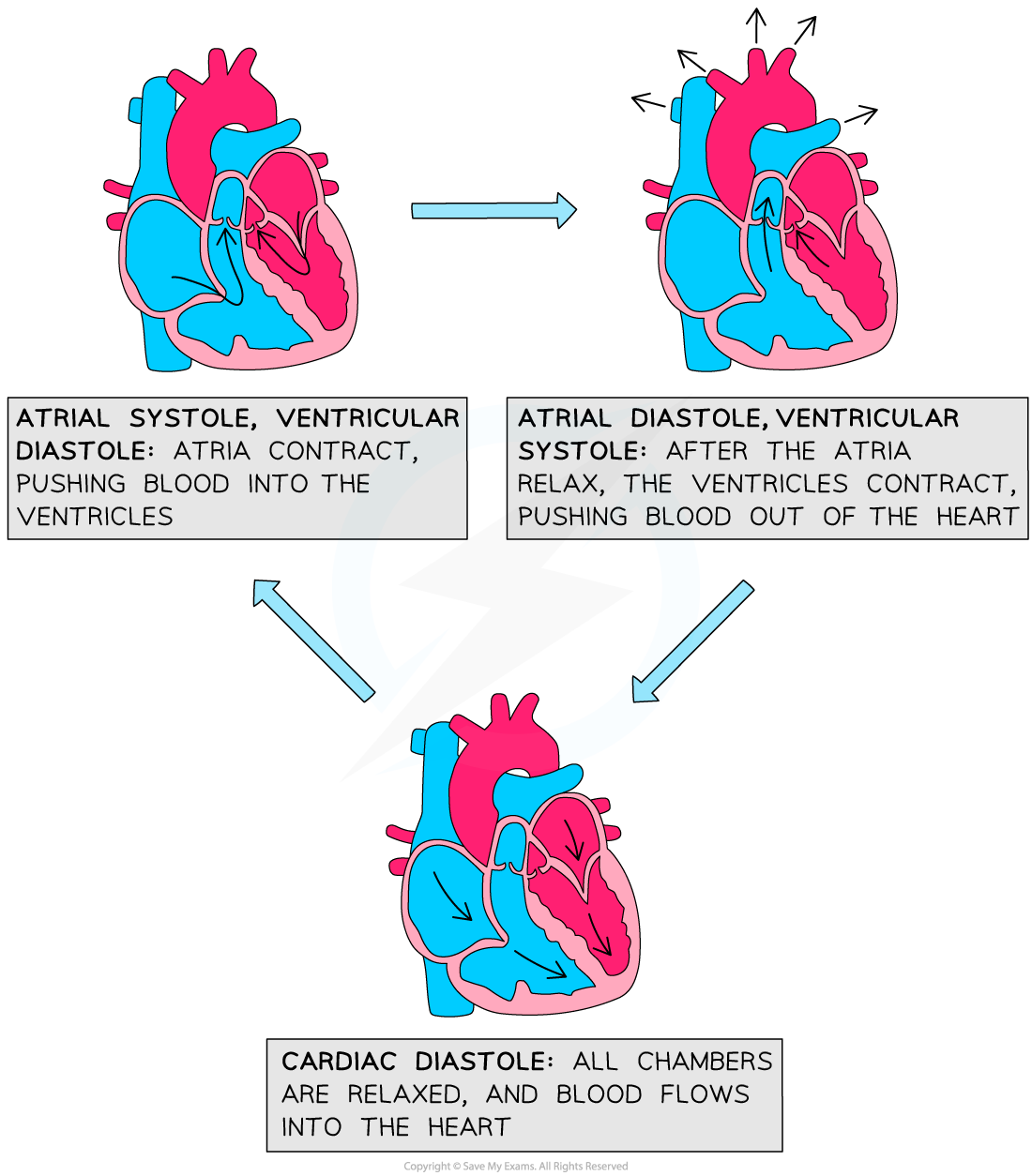
What happens during an atrial systole?
The atria contract while the ventricles remain relaxed
This decreases the volume in the atria so pressure inside increases
The atrioventricular valves open - the pressure in the atria is higher than the pressure in the ventricles
Blood moves into the ventricles
What happens during a ventricular systole?
The ventricles contract while the atria are relaxed
Pressure increases in the ventricles due to them filling with blood
This forces the atrioventricular valves shut - AV valves only go from atria to ventricle
The semi lunar valves open - the pressure in the ventricles is higher than the pressure in the aorta
Blood is forced into the arteries
What happens during a diastole?
Both the atria and ventricles are relaxed for a moment
This allows for the ventricles to empty and the atria to refill
this is so the cardiac cycle can repeat
The higher pressure in the aorta & pulmonary artery causes the semi lunar valves to close
Blood follows into the atria due to higher pressure in the vein
Atrioventricular valves are open to allow some blood to trickle through to the ventricles but there is no significant pressure behind it as the atria are relaxed