Research Methods I: Class 2
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
18 Terms
Define translational research
the direct application of scientific discoveries into clinical practice; describes as taking knowledge from “bench to bedside”
using articles to inform your practice, direct application
Discuss the advantages and limitations of comparative effectiveness research in providing evidence for practice
advantages: helps inform decisions about Tx choices; compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor or improve delivery of care
limitations: usually include studies done on patients who are seen in every day practice → small sample size
Discuss the relevance of considering patient-reported outcome measures and patient-oriented evidence that matters
patient reported outcome measure: any report of the status of a patient’s health condition that comes directly from the patient; relevant because they have a strong correlation to objective measures of movement and function and help inform decision making
patient reported evidence that matters: outcomes that measure things that a patient would care about, such as Sx, QOL, function, cost of care, LOS, etc.; relevant because it is informative in making clinical choices for clinical management
Discuss the purpose of implementation studies
focus on ways to change behavior; not intended to demonstrate the health benefits of clinical intervention → wants to demonstrate the quality of the use of that intervention and which behaviors are needed to achieve relevant outcomes
seeks to understand the behavior of healthcare professionals and other stakeholders as a key variable in the sustainable uptake, adoption, and implementation of evidence-based interventions
Differentiate evidence-based practice from practice-based intervention studies
Evidence-based practice | Practice-based interventions | |
-a process, beginning with clinical questions, appraisal of evidence, application of the evidence (considering the clients wishes and needs), and finishing with an evaluation of the clinical outcomes | -the systematic collection of patient-reported measures associated with a particular treatment goal or desired outcome. -purpose is to objectively understand the relationship between your actions as an OTR and the unique response of your clients on an individual basis | |
Discuss the factors that have influenced the need for EBP in OT
overuse of procedures without justification | underuse of established procedures | misuse of available procedures |
occurs when Tx tests are given without medical justification | occurs when clinicians fail to provide necessary care or tests, employ preventative strategies, or follow practice guidelines | inappropriate use of interventions or tests |
contributes to high costs | could lead to lack of referral services | often results in medical errors that can cause harm |
Describe sources of knowledge and how they relate to the use of evidence in practice
Tradition: “that’s the way it has always been done”
Authority: “that’s what the experts say”
Experience: “it’s worked for me before”
over time, they are likely to result in a lack of progress, limited understanding of current knowledge, or resistance to change even in the face of evidence
seeking evidence can substantiate or refute experience, authority, and tradition, and thereby strengthen foundations to consider new, more valid methods
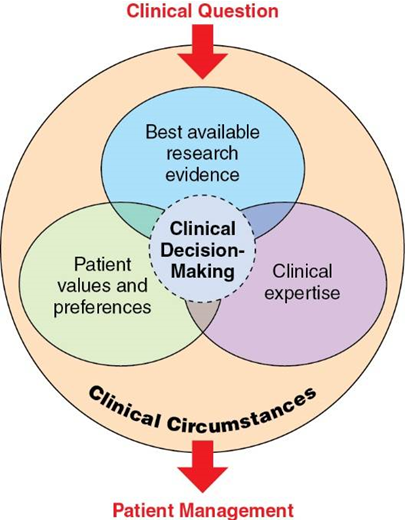
Define EBP and how the model contributes to practice decision-making
EBP: an approach to decision making that incorporates scientific information with other sources of knowledge; the integration of best research evidence with clinical expertise and the patient’s values and circumstances
evidence does not make a decision! the clinician and patient will do that together with all of the relevant and available evidence to to inform them for optimal shared decision-making
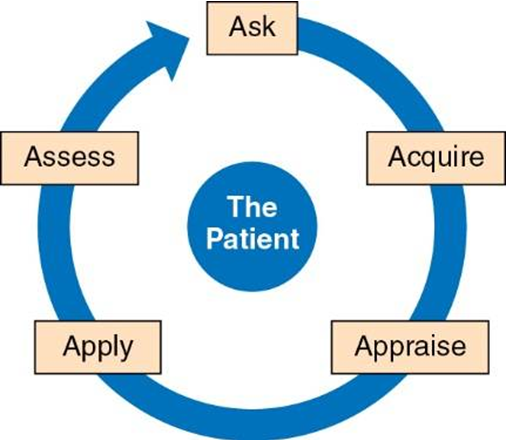
Describe the five steps in the EBP process
Ask a Clinical Question
Acquire Relevant Literature
Appraise the Literature
Apply the Evidence
Assess the Effectiveness of the Evidence
Step 1 of EBP: Ask a Clinical Question
background questions: who, what, when, where, why, how
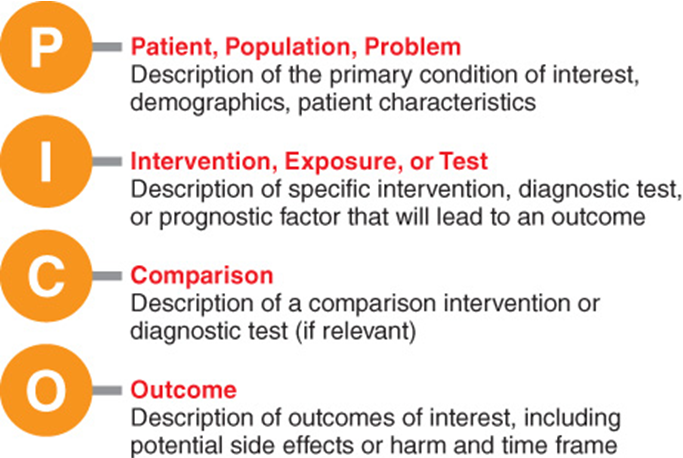
foreground questions: PICO
sources of clinical/practice questions: diagnosis and measurement, prognosis, intervention, client experiences
Step 2 of EBP: Acquire Relevant Literature
types of studies used depend on the clinical question
finding specific evidence
synthesized evidence
systematic reviews
meta-analyses
clinical practice guidelines
scoping review
Step 3 of EBP: Appraise the Literature
means “so what, does the study help me?”
3 primary questions:
is the study valid?
are the results meaningful?
are the results relevant to my patient?
Step 4 of EBP: Apply the Evidence
putting evidence, clinical expertise, patient values, and clinical circumstances all together to inform a clinical decision
Step 5 of EBP: Assess the Effectiveness of the Evidence
did the client improve?
is additional evidence needed
do additional questions need to be answered?
Develop clinical questions using the PICO format for studies of interventions, diagnosis, and prognosis
PICO example:
P: type 2 diabetes, frozen shoulder, age, gender
I: physical therapy, occupational therapy
C: corticosteroids (other option being questioned)
O: reduced shoulder disability, decreased pain, increased ROM
Describe the general questions used to critically appraise a study
is the study valid? | are the results meaningful? | are the results relevant to my patient? |
determining the quality of the design and analysis and the extent to which you can be confident in the study’s findings | results must be interpreted in terms of their impact on patient responses and outcomes | are the findings applicable to your patient and clinical decisions |
ex: was the sample selected appropriately? was bias sufficiently controlled? what were the outcome measures? does data support conclusions? | ex: is the sample sufficiently representative of the target population so that results can be generalized? is the effect large enough to be clinically meaningful? | ex: were the subjects in the study similar to my patient? can I apply the results to my patient’s problem? |
Describe the levels of evidence used to distinguish the strength of studies for quantitative and qualitative studies
Level I: Systematic reviews of RCTs; not actually research study, just a literature review
Level II: RCTs
Level III: Nonrandomized controlled trial studies
Level IV: 1 group trial with pretest and posttest (no control or comparison group)
Level V: Case reports; expert opinion paper about what they value in practice
Define the importance of implementation studies and knowledge translation to the EBP process
implementation studies focus on ways to change behavior; figuring out what works well in an intervention and what we need to change to make interventions better
knowledge translation is the process of accelerating the application of knowledge to improve HC outcomes and change behavior in all those providing care; creating and applicating new knowledge
these are important in EBP because through KT, we are able to build on our clinical expertise and implementation studies help change research into becoming better