NSAIDs
1/53
Earn XP
Description and Tags
My immunology background strikes again
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
Antipyretic, analgesic, anti-inflammatory
What are NSAIDs used for?
Nonselective reversible inhibitors of COX 1 and 2 (ASA is irreversible)
What is the MOA for NSAIDs
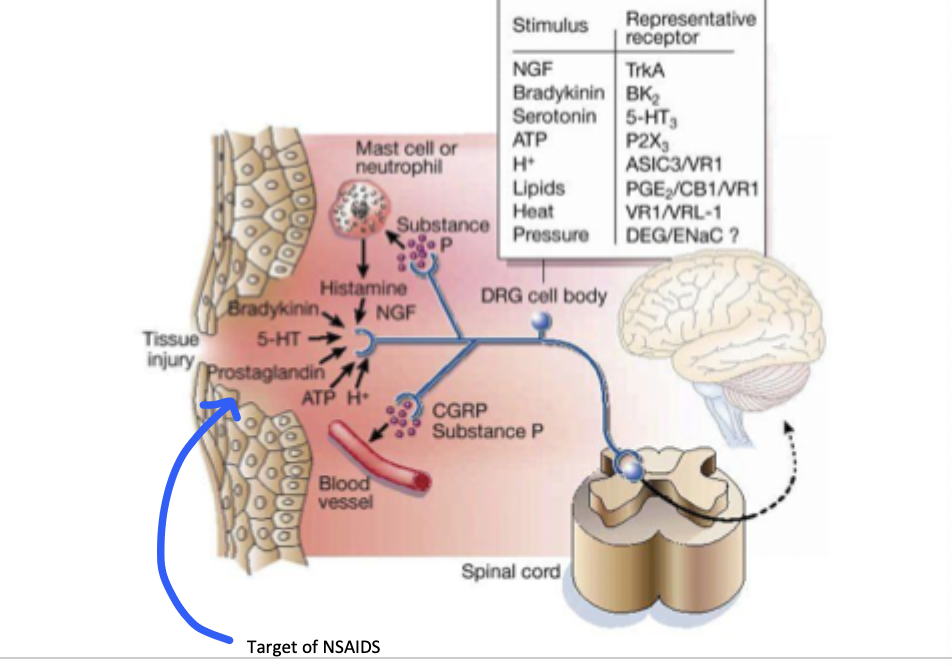
stimulus → Phospholipase A2 → free phospholipids → arachidonic acid → lipoxygenase (leukotrienes) or COX pathway (prostaglandins, TXA2)
Describe Eicosanoid synthesis
histamine
The release of leukotriene precursors (HpETE) is usually accompanied by the release of
Constitutive particularly in the stomach, inducible (2-4x), major product is TXA2 (platelet aggregation), inhibition by ASA reduces cardiac evens
Tell me about the COX-1 enzyme
Inducible (10-20x) by inflammatory response, found in the kidneys, lungs, macrophages (inflammatory cells), inhibited by NSAIDs and steroids
Tell me about the COX-2 enzyme
Increases lipocortin, decreasing PLA2 (both paths are blocked)
MOA for glucocorticoids
If we block the COX pathway, all the arachidonic acid is moved through the lipoxygenase pathway
What is the SHUNT hypothesis?
inhibit COX at low doses (200 mg), anti-inflammatory effect requires larger doses (600-800 mg)
Describe the dosage regimen for NSAIDs
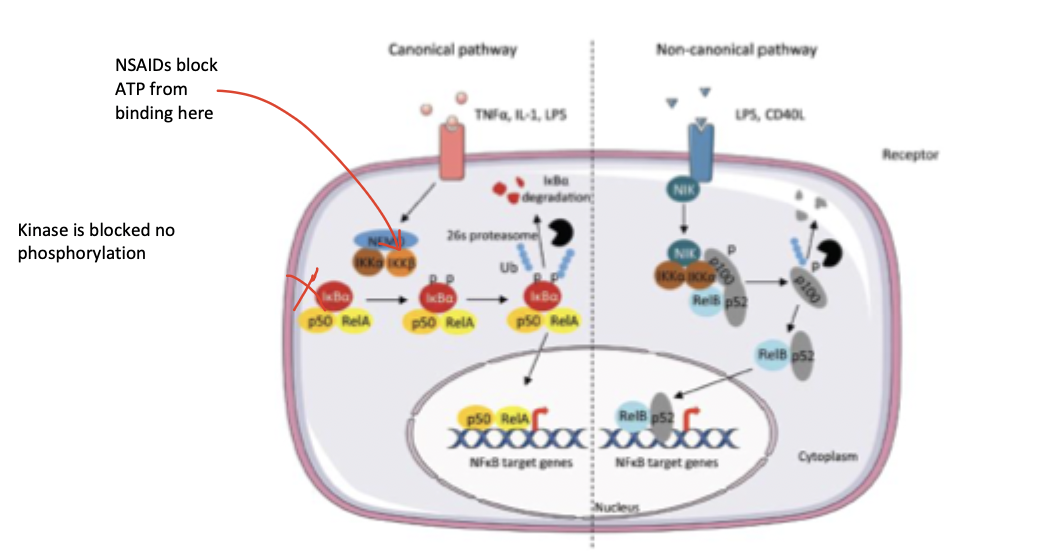
blockage of the ATP binding site of IKK to prevent phosphorylation of IKB and activation of NFKB
Describe the anti-inflammatory MOA for NSAIDs (NOT TYLENOL)
Blocks the release of PGE2 (no increase of thermoregulatory set point)
Describe the Antipyresis MOA for NSAIDs
Only acts in the brain (no peripheral, no anti-inflammatory)
Why is acetaminophen the drug of choice for fever?
Decreases available PGs able to hit nocioreceptors (work peripherally)
Describe the analgesia MOA for NSAIDs
Decreases PGs (which normally potentiate contractions)
Describe the anti-parturition MOA for indomethacin → NO NSAIDS in PREGNANCY
Anti-inflammatory at 150-300 mg, ZERO ORDER KINETICS (enzymes become saturated at therapeutic range, large doses increase half-life), If you see tinnitus you took to much, DDI with NSAIDs (decreases anti-platelet effects)
Tell me about the acetylated salicylates (ASA)
little effect on platelets and thus risk for bleeding
Tell me about the non-acetylated salicylates
Choline salicylate, diflunisal, mag salicylate, salsalte, sodium salicylate, sodium thiosalicylate
Examples of non-acetylated salicylates
little anti-pyretic effect, not metabolized to salicylate
What is special about diflunisal
Diclofenac, etodolac, ibuprofen, indomethacin, meloxicam, nabumetone, naproxen, naproxen sodium , oxaprozin, piroxicam, keteorlac
Examples of NSAIDs
relatively COX-2 selective, less GI tox, some inhibition of the lipoxygenase, may increase MI risk
What is special about diclofenac?
COX-2 selective, less GI tox
What is special about etodolac?
some inhibition of the lipoxygenase, High incidence of CNS side effects in geriatric patients
What’s special about Indomethacin?
acutely moderate-severe pain ONLY, high risk of PUD
What is special about ketorolac?
Less risk of PUD, used for arthritis, dysmenorrhea, post-surgical pain, NO effect on platelets, Increase risk of MI or stroke
Tell me about the COX-2 inhibitors (Coxibs)
T1/2 of 10 hrs,
Quirks of Celecoxib
good bioavailability, low 1st pass, small Vd (highly bound), secreted via kidneys, concentration in synovial fluid is about 60%
NSAID pharmokinetics
ASA, diclofenac, etodolac, ibuprofen, indomethacin, ketorolac, salicylate
Short acting NSAIDs (under 6 hours) - underlined have slow release preparations available
diflunisal, naproxen, salsalte, sulindac, celecoxib
Intermediate acting NSAIDs (7-14 hours)
Nabumetone, oxaprozin, prioxicam, salicylate
Long acting NSAIDs (15+ hrs)
Peeps who have already had a stroke or MI, Coronary bypass, angina, High MI risk, DM + another risk factors
Who is a baby ASA recommended for?
ASA hypersensitivity, increased BP, nephrotoxicity, GI ulceration and bleeding; CNS reactions (rebound HA, dizziness)
ADRs of NSAIDs
Not true anaphylaxis but symptoms arise from increased LT synthesis (the SHUNT), associated with nasal poyps
What is special about ASA allergies?
rhinoconjunctivitis, angioedema, urticaria
Symptoms of ASA allergies - occurs within 3 hr
full expression of NE-led vasoconstriction (may interfere with anti-hypertensives)
MOA for HTN with NSAIDs
PGs help produce diuresis by increasing GFR so without that its not looking good especially for geriatric patients (can produce hyperkalemia, interstitial nephritis, and AKIs)
MOA for nephrotoxicity with NSAIDs
prior hx of PUD, prior NSAID intolerance, chronic EtOH usage, corticosteroid usage, chronic smoking, 60+
Who is at risk for GI ulcerations and bleeding with NSAIDs
Misoprostol + dicofenac (if not tolerated → celecoxib or NSAID + H2 or NSAID + PPI)
Treatment plan of NSAID associated GI ulceration
You use all your glutathione, so you get more NAPQI in the system (which is toxic)
Why can you kill yourself by taking a ton of tylenol? (NOTE: alcohol abuse increases risk)
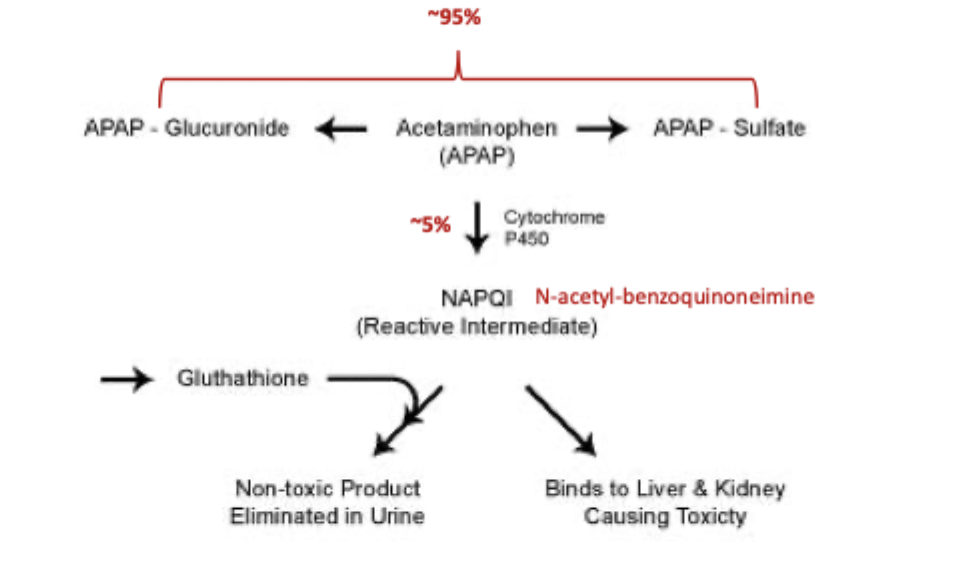
gastric lavage + IV N.acetylcysteine
Treatment plan for tylenol OD
Allergies, autoimmune diseases, miminize transplant rejection
Indications for immunosuppressants
corticosteroids, calcineurin inhibitors, mTOR inhibitors, IMDH inhibitors, biologic, MABS
Classes of immunosuppressants
We need a signal transduction from CD3, followed by a signal transduction from Cd28, stimulation by IL-2. The TCR complex (includes CD3) (t-cell) binds to the MHC/peptide complex (APC) -> antigen recognition. B7 (APC) binds to CD28 (T-cell) -> signal transduction. IL-2 induces cell proliferation and eventual differentiation into an effector cell.
How are T cells activated
Suppresses IL-2 production in T cells (no activation)
MOA for calcineurin inhibitors
cyclosporine, tacrolimus
Examples of calcineurin inhibitors
Prevents GVHD, T1/2 of 24 hours, 3A4 metabolism, swelling of gums
Tell me about cyclosporine
reduces risk of organ rejection, T1/2 is 11 hours, 3A4 and 3A5 metabolism
Tell me about Tacrolimus (Pro-graft)
suppresses intracellular signalling pathway important for cell growth and proliferation of T lymphocytes
MOA for mTOR inhibitors
Sirolimus, everolimus, temisirolimus
Examples of mTOR inhibitors
Prevents transplant rejection, coats coronary stents, 2-3 day T1/2, 3A4 metabolism
Tell me about sirolimus
Prevents transplant rejection, 30 hr T1/2, 3A4 and 3A5 metabolism, chemo agent for HER-2 neg breast cancer
Tell me about everolimus
Blocks DNA synthesis → no clonal expansion
MOA for IMDH inhibitors
Azathioprine, mycophenolate, lefunomide
Examples of IMDH inhibitors
Used for RA, Crohn’s, and transplants; T1/2 is 1.5 hr and 18 hrs,
Tell me about Azathioprine, mycophenolate ($$$)
Used for RA, T/12 is 2 weeks, hepatic metabolism, chemo agent for HER-2 neg breast cancer
Tell me about Lefunomide