Module 2 - Learning Hub - CT Data Acquisition & X-Ray Production - Flashcards
1/57
Earn XP
Description and Tags
flashcards cover data acquisition, scan methods, planning, CT hardware concepts (MDCT, isotropy), advanced techniques (dual-energy, dynamic, dual-source), and fundamentals of X-ray production and image formation.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
58 Terms
What is data acquisition in CT?
How the scanner is programmed to acquire data during an exam, relating to image reconstruction.
What are the three main scan methods in CT?
Localizer (scout/topogram), Sequential (axial/step-and-shoot), and Helical (spiral).
What additional acquisition methods exist?
Dual source CT, Dual energy CT, and Dynamic CT.
Do modern CT scanners use single-slice or multislice technology?
All modern scanners use multislice/multidetector CT (MDCT).
What does scan planning involve?
Reviewing exam request/protocol and setting patient orientation, positioning, centering, and zeroing.
What patient orientations are possible?
Supine or prone, head first or feet first.
What is centering in CT?
Aligning patient’s midcoronal and midsagittal planes to gantry isocenter.
Why is accurate centering important?
Prevents uneven attenuation, ensures proper dose modulation, and avoids repeat scans.
What is landmarking (zeroing)?
Setting the scan’s reference or starting location on the gantry.
Give examples of common exam landmarks.
Head = EAM/vertex/base of skull; Chest = sternal notch or C7; Abdomen = xiphisternum; Pelvis = iliac crest; C-spine = EAM or TEA; Extremities = joint space or ends of range.
Why should foreign bodies be removed before localizer scans?
To avoid repeating the localizer after repositioning the patient.
What are localizer scans also called?
Scouts, topograms, or scanograms.
What type of image is a localizer?
A low-dose radiograph.
What are localizers used for?
To plan scan range, determine DFOV, and calculate tube current.
How many localizers are usually taken?
At least two (AP and lateral).
How does sequential scanning work?
The table is stationary while the tube rotates once, then turns off; the table moves to the next position – “step and shoot.”
What was the original reason for using sequential scanning?
Pre-slip ring scanners required rewinding heavy cables between rotations.
What are the advantages of sequential scanning?
Slightly better spatial resolution due to less interpolation and narrow collimation.
What are the disadvantages of sequential scanning?
Long scan times, motion artifacts, slice misregistration, data gaps, and limited post-processing.
What are modern uses of sequential scanning?
Specialized exams like inner ear imaging and interventional CT procedures.
How does helical scanning work?
Continuous tube rotation while the table feeds through the gantry.
What is pitch in CT?
Table movement per rotation ÷ beam width (detector collimation).
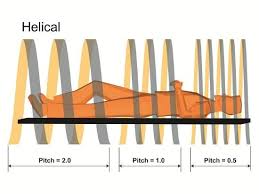
What does pitch < 1 indicate?
Oversampling (anatomy scanned more than once).
What does pitch > 1 indicate?
Data gaps, lower quality.
What is a typical pitch range in MDCT?
0.75–1.5 (rarely exceeds 1.7).
What are the advantages of helical scanning?
Fast acquisition, less motion artifact, flexible reconstructions (MPR, 3D, reslicing).
What principle is often used in CT acquisition vs reconstruction?
“Scan thin, reconstruct thick.”
What is the main advantage of MDCT detectors?
Multiple slices per gantry rotation.
What are fixed detector arrays?
Detectors of equal size that can be electronically combined for thicker slices.
What are adaptive detector arrays?
Arrays with detector rows of varying sizes for flexible acquisition setups.
What tradeoff exists when configuring detector arrays?
Full array for speed and coverage vs fewer rows for better image quality.
What are isotropic voxels?
Voxels with equal dimensions in x, y, and z planes.
Why is isotropic data important?
Allows high-quality reconstructions in any plane, reduces volume averaging, and improves 3D imaging.
What is Dual Source CT?
A system with two tube-detector arrays, allowing faster scans, high-power imaging, and dual-energy applications.
What is Dual Energy CT?
Uses two different kV levels (e.g., 80 & 120 kV) to differentiate tissue composition by attenuation fingerprints.
Give an example of a dual energy CT application.
Differentiating uric acid vs calcium oxalate kidney stones.
What is Dynamic CT?
Continuous scanning of the same region (table stationary) to assess function, e.g., perfusion studies.
What is a common clinical use of Dynamic CT?
Brain perfusion scans in stroke evaluation.
How are X-rays produced in a CT tube?
Electrons from a heated filament strike the rotating anode, converting kinetic energy mostly into heat and partly into X-ray photons.
What is a space charge?
Cloud of electrons hovering near the heated filament before acceleration.
What controls the quantity of electrons in CT?
Tube current, measured in milliamperes (mA).
What controls the energy/intensity of the X-ray beam?
Tube voltage (kVp).
What proportion of electron energy becomes X-rays vs heat?
99% heat, <1% X-rays.
Why does the anode rotate?
To spread heat over a larger area and prevent damage.
What are heat capacity and dissipation in CT tubes?
Heat capacity = ability to withstand heat; Heat dissipation = ability to release it.
How do detectors convert X-rays into signals?
- Scintillator: X-rays → light → electrical current (via photodiode). - Xenon gas (older): X-rays ionize gas → ions collected by detector plates.
What are the main advantages of CT over conventional radiography?
Cross-sectional imaging (no superimposition), high contrast resolution, multiplanar/3D reconstructions, and quantitative data via Hounsfield units.
What does the Z-axis represent in CT?
The head-to-foot axis of the patient, defining slice thickness.
What is a pixel?
The smallest 2D image element, representing tissue in x and y directions.
What is a voxel?
A 3D volume element (pixel size × slice thickness).
What is a matrix?
The grid of rows and columns forming the image; each cell is a pixel.
What is beam attenuation?
Reduction of x-ray beam intensity as it passes through matter.
What factors determine a structure’s ability to attenuate the beam?
Tissue density, atomic number, thickness, and photon energy (kVp).
What unit quantifies a structure’s ability to attenuate x-rays?
Hounsfield Unit (HU).
Why does slice thickness vary across protocols?
Thin slices improve resolution and 3D reconstructions; thick slices reduce noise, dose, and are used when high detail isn’t needed.
How are x-ray photons produced in CT?
Heated filament releases electrons → accelerated by high voltage → strike rotating anode → >99% energy = heat, <1% = x-ray photons from the focal spot.
What are the main CT scan modes and their pros/cons?
Axial (sequential): Step-and-shoot, high z-resolution, less interpolation, slower overall.
Helical (spiral): Continuous table movement, fast, motion-robust, slight interpolation needed
How does changing pitch affect scan time and patient dose?
↑ Higher Pitch = ↓Decreased Scan time,
↓ Lower Pitch = Increased ↑ Scan time,