Larynx
1/10
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
11 Terms
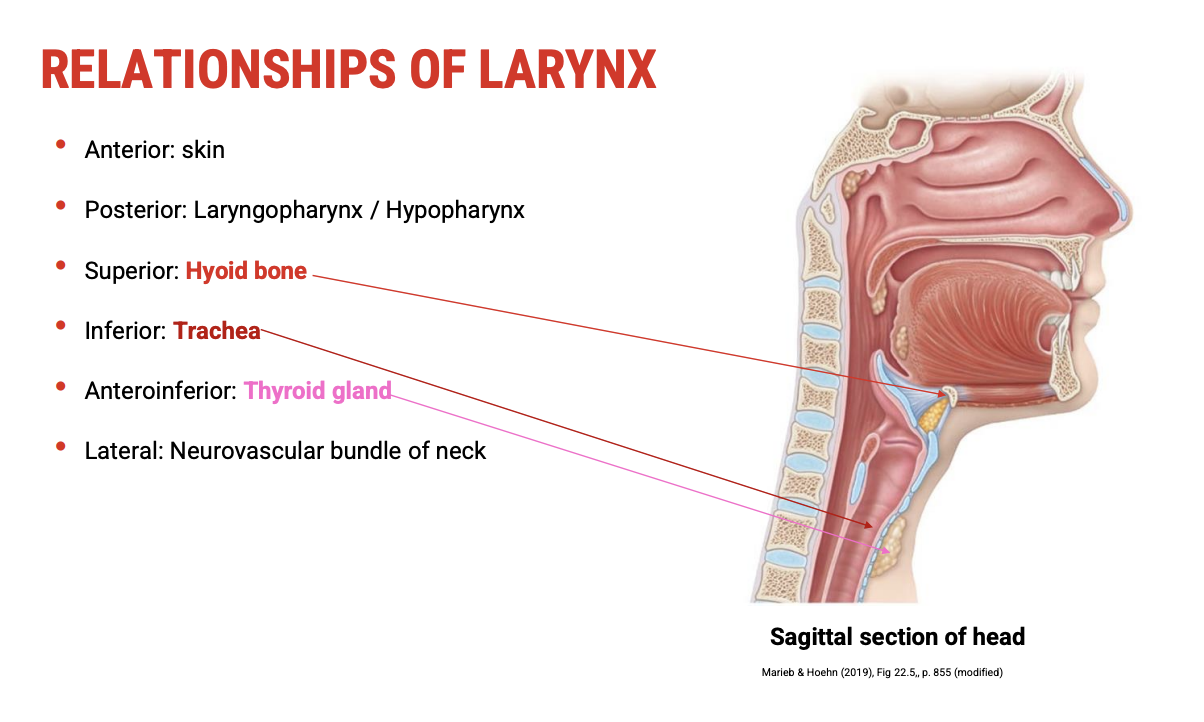
Laryngeal Structure Review
🦴 Key Anatomical Structures Covered
🧠 Relations to Adjacent Structures
Pharynx – posterior to the larynx
Hyoid bone – superior support structure
Trachea – inferior continuation of the airway
Thyroid gland – lies anterior and lateral to the larynx
Major neurovascular bundles of the neck – crucial for innervation and blood supply
🛠 Principal Laryngeal Cartilages
Epiglottis – elastic cartilage for airway protection during swallowing
Thyroid cartilage – largest cartilage, forms the "Adam's apple"
Cricoid cartilage – complete ring, foundation of the larynx
Arytenoid cartilages – paired, pivotal for vocal fold movement
🧵 Vocal Fold Anatomy
True vocal folds – involved in sound production
False vocal folds (vestibular folds) – protective function
Membranous connections:
Quadrangular membrane (above) connects to false folds
Conus elasticus (below) connects to true folds
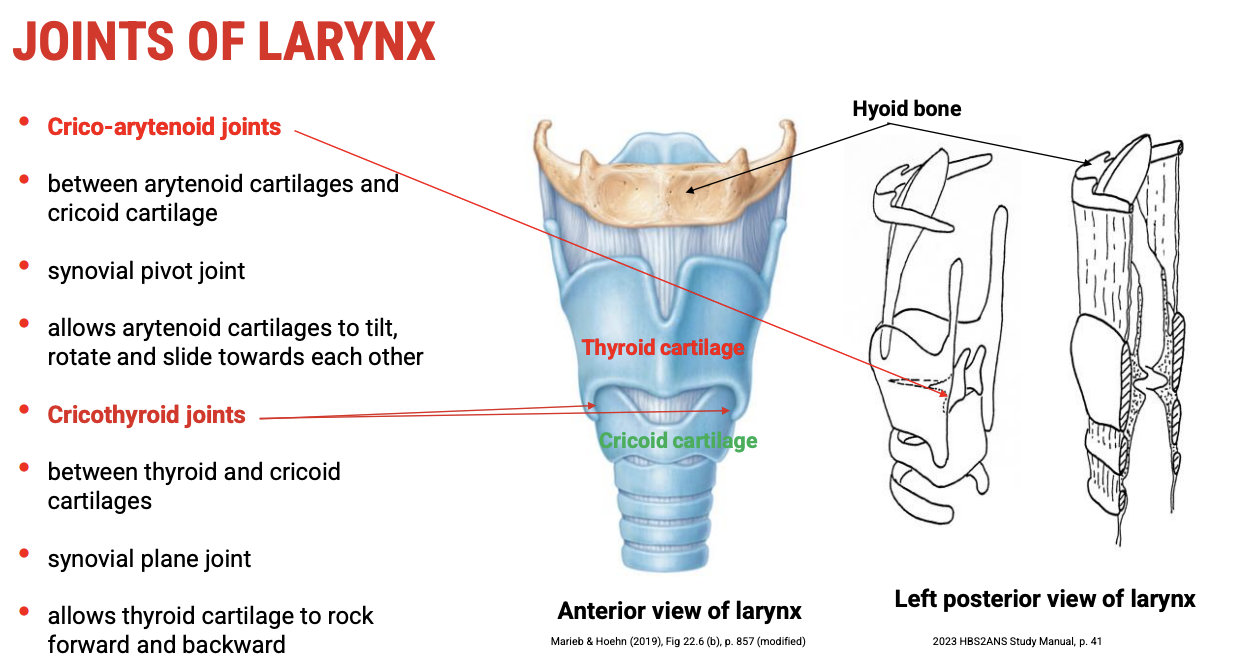
🔄 Laryngeal Joints
Cricothyroid joint
Histology: synovial
Function: tilts thyroid cartilage to adjust pitch
Cricoarytenoid joint
Histology: synovial
Function: adducts and abducts vocal folds (phonation and respiration)
📌 Clinical Relevance to Robert
Understanding the anatomy, histology, and movement of these structures is essential for:
Interpreting Robert’s voice difficulties
Assessing possible structural or neuromuscular dysfunctions
Planning targeted therapy or intervention strategies
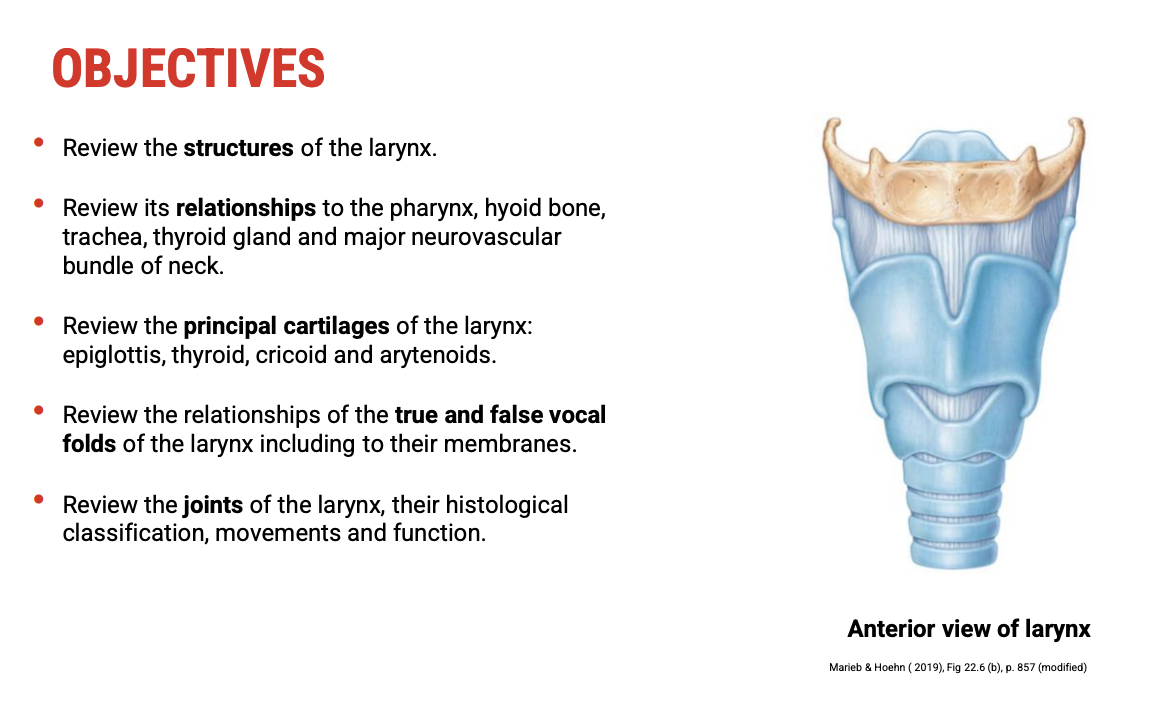
Structure and Function of the Larynx
🧱 Structural Overview
The larynx is a musculo-cartilaginous structure.
It is located between the laryngeal inlet (superiorly) and the trachea (inferiorly).
Composed of cartilage, muscle, ligaments, and membranes, it maintains airway patency and enables movement required for voice and airway protection.
🌬 Primary Function: Airway Management
Air Passageway: Allows air to travel from the pharynx to the trachea and lungs.
Airway Closure:
The glottis (space between the vocal folds) functions as a sphincter.
Can close tightly to:
Prevent aspiration (protect the lower airway)
Clear the upper airway (via coughing)
Assist in abdominal straining (e.g. lifting, defecation, childbirth)
🎤 Special Function: Phonation
Exhaled air from the lungs causes the true vocal folds to vibrate.
This vibration generates sound, which is shaped by the supralaryngeal structures (e.g. oral and nasal cavities) to produce speech.
Voice quality depends on the health, position, and coordination of the vocal folds.
📌 Clinical Link to Robert
Understanding these functions is crucial when evaluating voice disorders in children like Robert.
Issues may relate to:
Incomplete closure (leading to breathy or weak voice)
Tension abnormalities (impacting pitch or loudness)
Neuromuscular control affecting fold vibration and closure
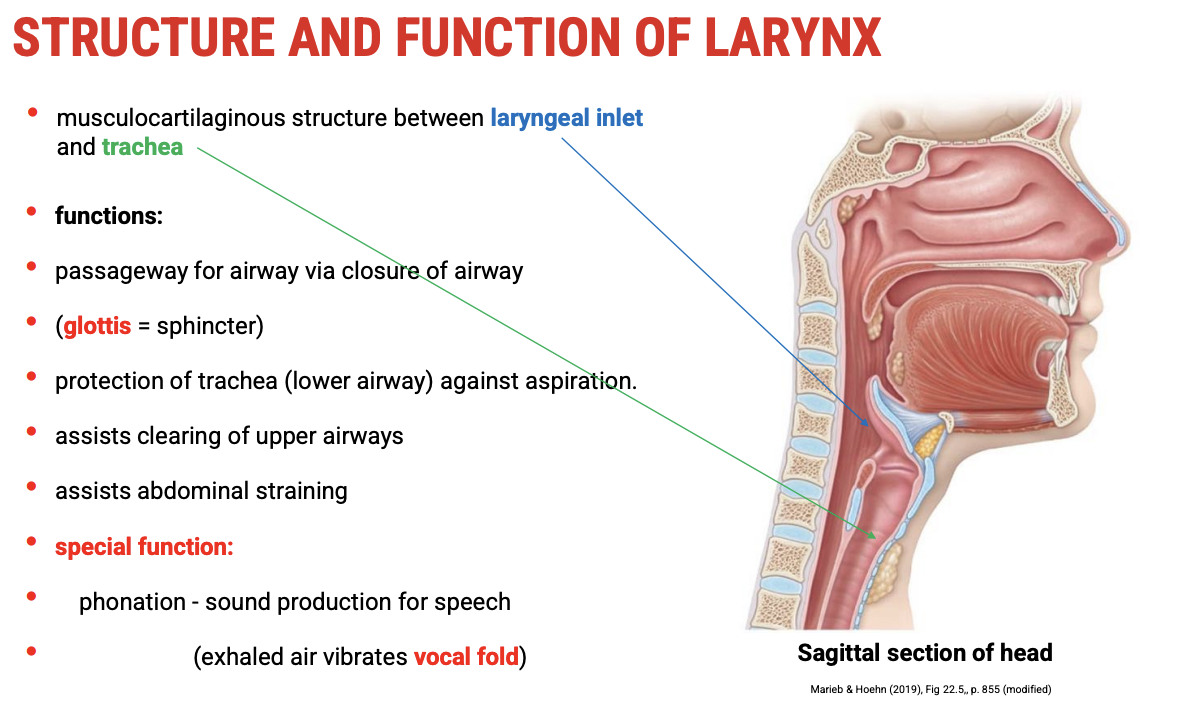
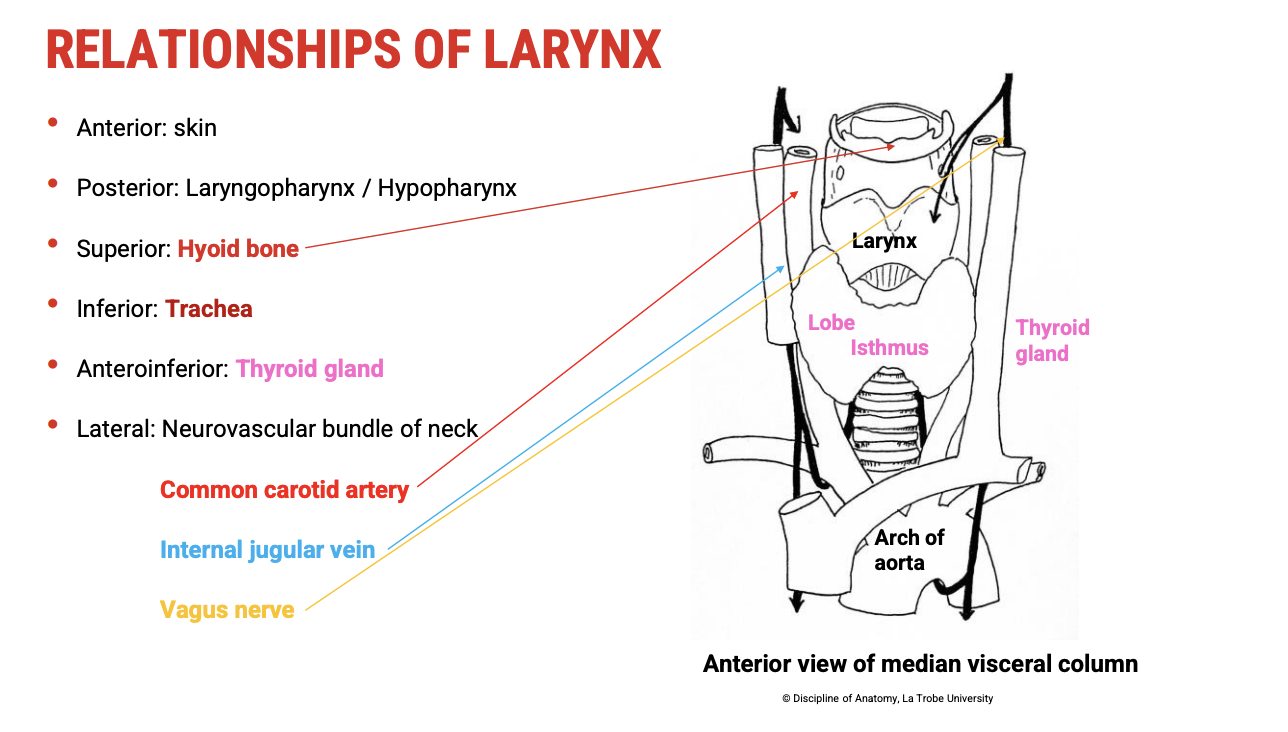
Anatomical Relationships of the Larynx
📌 Position Overview
The larynx is centrally located in the anterior neck and is surrounded by several key anatomical structures:
🔄 Spatial Relationships
Anterior (in front):
Skin
Subcutaneous tissue
Strap muscles of the neck (e.g. infrahyoid muscles)
Posterior (behind):
Laryngopharynx (also called the hypopharynx)
Critical for swallowing; lies directly behind the larynx
Superior (above):
Hyoid bone
Suspends the larynx
Forms part of the upper boundary of the airway
Will be discussed in detail in a later section
Inferior (below):
Trachea
Continuation of the airway
Thyroid gland
Lies anterior and lateral to the upper trachea and larynx
Important in relation to surgical procedures and voice changes
Lateral (to each side):
Major neurovascular bundles of the neck, including:
Common carotid artery
Internal jugular vein
Vagus nerve (CN X) — crucial for laryngeal innervation
📍 Relevance to Robert
These relationships are important when considering causes of voice issues, such as:
Compression, inflammation, or pathology involving adjacent structures (e.g. thyroid gland)
Nerve involvement, especially recurrent laryngeal or superior laryngeal nerve damage
Neurovascular Bundles in Context of the Larynx
🩻 Anatomical Diagram Reference
When viewing a median visceral column cross-section of the neck, we see paired neurovascular bundles on either side of the larynx and trachea.
🔀 Key Components of the Neurovascular Bundles
Common Carotid Artery
Major artery supplying head and neck
Located medial in the bundle
Bifurcates into internal and external carotid arteries around the level of the thyroid cartilage
Internal Jugular Vein
Major venous drainage from the brain and superficial face
Positioned lateral to the common carotid artery
Vagus Nerve (Cranial Nerve X)
Sits between and slightly posterior to the artery and vein
Crucial for parasympathetic control and laryngeal innervation
🔌 Laryngeal Innervation by the Vagus Nerve
Superior Laryngeal Nerve (branch of CN X)
External branch: motor to cricothyroid muscle (pitch control)
Internal branch: sensory to supraglottic larynx
Recurrent Laryngeal Nerve
Loops around major arteries (aortic arch on left, subclavian on right)
Ascends in the tracheoesophageal groove
Motor to all intrinsic laryngeal muscles (except cricothyroid)
Sensory to infraglottic larynx
🧒 Relevance to Robert’s Voice Disorder
Any compression, inflammation, or injury to these neurovascular structures can affect laryngeal nerve function, leading to:
Weak voice or dysphonia
Impaired pitch modulation
Aspiration risk if sensory nerves are affected
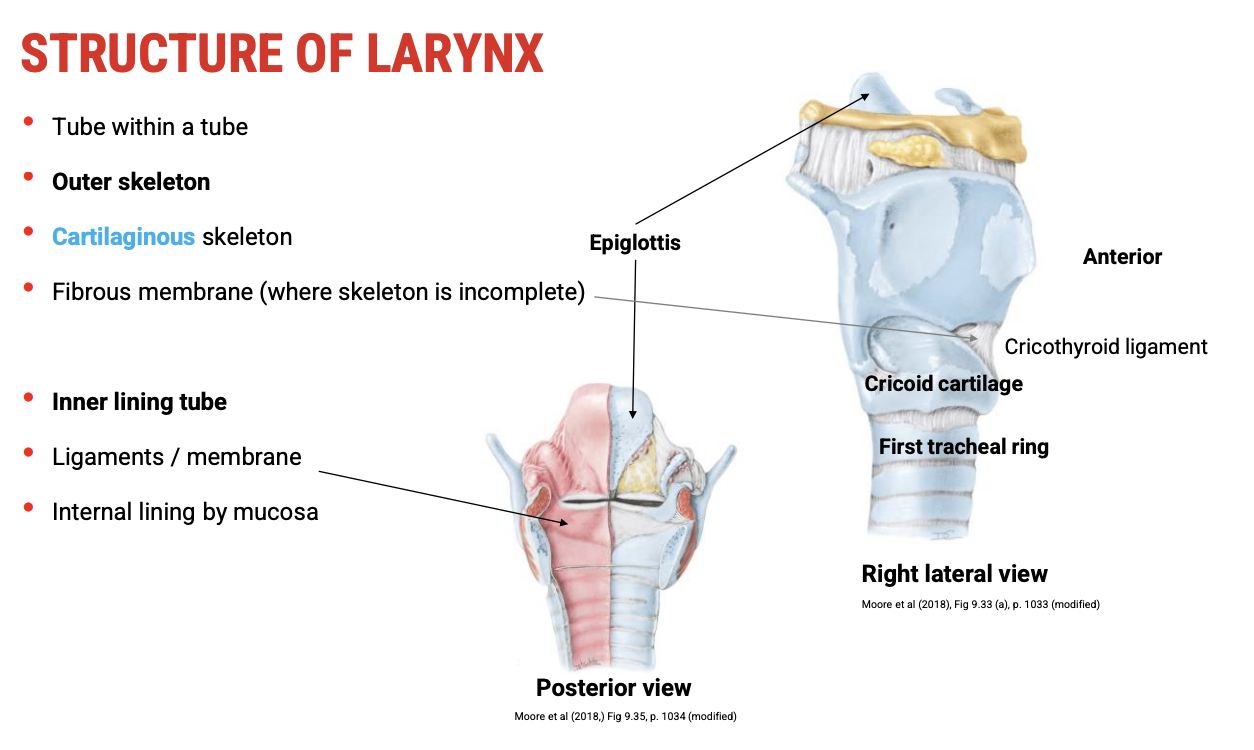
Structure of the Larynx: "Tube Within a Tube" Concept
🧊 Outer Tube: The Laryngeal Skeleton
Function: Provides shape, support, and protection
Composed of:
Cartilages (e.g. thyroid, cricoid, arytenoid, epiglottis)
Fibrous membranes connecting the cartilages
This outer tube forms an incomplete skeleton, open posteriorly in some regions (e.g. thyroid cartilage).
🧵 Inner Tube: The Functional Core
Lies within the cartilaginous framework and comprises key structures involved in voice and airway protection:
🦴 Ligaments and Intrinsic MembranesProvide structural integrity and movement pathways
Anchor the vocal folds and shape the glottis
🧫 Lining and EpitheliumLined with mucosa, which is:
Stratified squamous epithelium over areas of high mechanical stress (e.g. vocal folds, epiglottis)
Ciliated pseudostratified epithelium in lower-resistance regions (e.g. subglottis)
Mucosa is vital for hydration, protection, and vocal fold vibration
🎯 Functional Significance
This dual-tube structure:
Maintains structural flexibility and movement capacity
Supports fine control of airflow and vocal fold tension
Allows for phonation, breath control, and airway protection
👶 Clinical Relevance to Robert
Disruption in any layer (e.g. cartilage, membranes, mucosa) may affect:
Voice quality
Airway patency
Sensitivity of the larynx, impacting protective reflexes and phonation
Cartilages of the Larynx and Their Connections
🔢 Three Unpaired Cartilages
These form the midline framework of the larynx and serve as anchors for ligaments, membranes, and muscles.
1. Epiglottis
Type: Elastic cartilage
Function: Folds down during swallowing to protect the airway
Shape: Leaf-like, attached to the inner surface of the thyroid cartilage
Clinical note: Elastic cartilage resists calcification with age, maintaining flexibility
2. Thyroid Cartilage
Type: Hyaline cartilage
Structure:
Laryngeal prominence (Adam’s apple) — anterior bulge
Superior horns — connect to the hyoid bone
Inferior horns — articulate with cricoid cartilage
Function: Largest laryngeal cartilage; houses the vocal folds on its internal surface
Muscle and ligament connections:
Thyrohyoid membrane (to hyoid)
Cricothyroid membrane (to cricoid)
3. Cricoid Cartilage
Type: Hyaline cartilage
Shape: Signet ring — broad posteriorly, narrow anteriorly
Position: Lies below the thyroid cartilage and above the trachea
Key connection:
Cricothyroid membrane (joins anterior part of cricoid to thyroid cartilage)
Articulates with:
Thyroid cartilage (at cricothyroid joint)
Arytenoid cartilages (posterior surface)
🧠 Why Names Matter
Many ligaments, membranes, and muscles are named after the cartilages they connect or act upon:
Cricothyroid membrane
Thyroepiglottic ligament
Cricothyroid muscle
👶 Relevance to Robert’s Case
Structural or developmental issues in these cartilages or their associated joints and membranes could:
Affect vocal fold positioning or tension
Impair voice production or airway protection

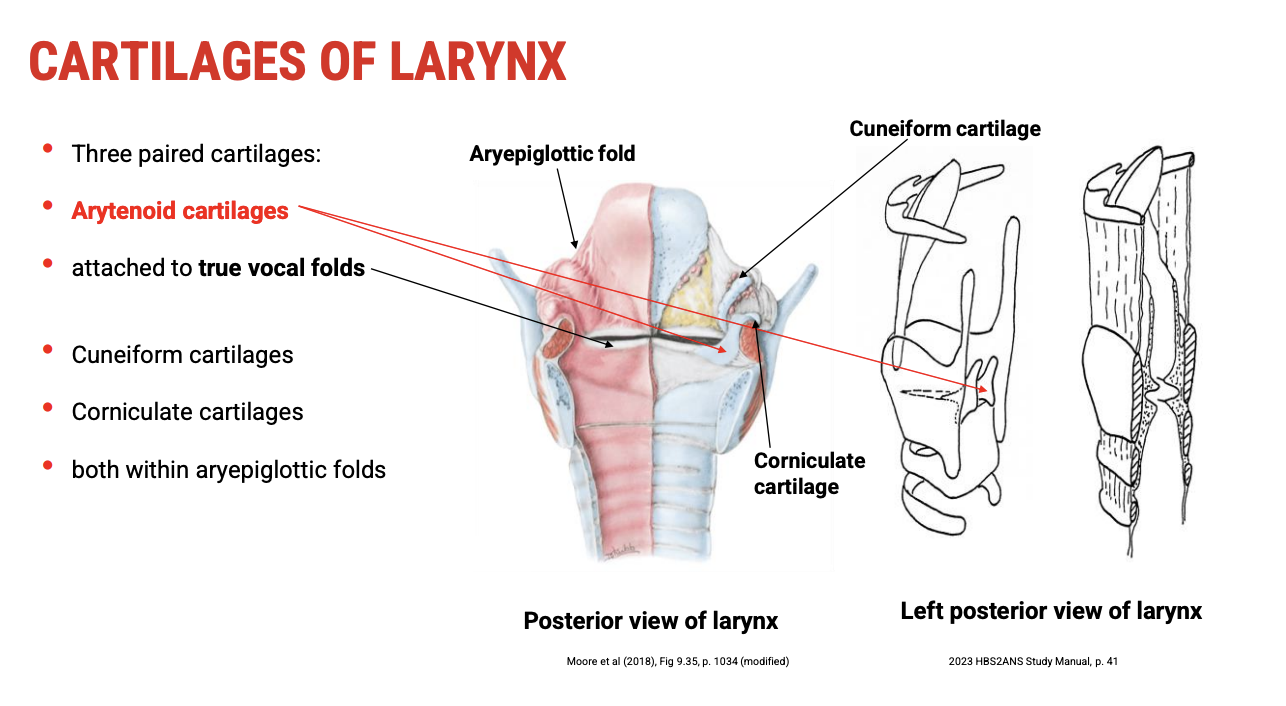
Paired Cartilages of the Larynx
🔢 Three Paired Cartilages
These six smaller cartilages (in three bilateral pairs) are crucial for vocal fold movement, support, and structure within the laryngeal inlet.
1. Arytenoid Cartilages 🔄
Type: Hyaline cartilage
Shape: Pyramidal (three-sided)
Position: Sit on top of the posterior cricoid cartilage
Function:
Anchor the posterior ends of the true vocal folds
Enable movement of the vocal folds through rotation and gliding
Muscle attachments:
Posterior cricoarytenoid (abducts vocal folds)
Lateral cricoarytenoid (adducts vocal folds)
Arytenoid muscles (assist in adduction)
2. Corniculate Cartilages 🌽
Type: Elastic cartilage
Position: Sit atop the arytenoids
Function:
Provide structural support to the aryepiglottic folds
Covered by mucosa — not directly visible
Lined by: Stratified squamous epithelium within the aryepiglottic fold
3. Cuneiform Cartilages 🌀
Type: Elastic cartilage
Position: Embedded within the aryepiglottic folds, anterior to corniculate cartilages
Function:
Provide support and stiffness to the aryepiglottic fold
Help maintain the opening of the laryngeal inlet
Lined by: Mucosa with stratified squamous epithelium
🧒 Clinical Relevance to Robert
Arytenoid dysfunction may lead to:
Poor vocal fold closure
Breathy, weak, or hoarse voice
Corniculate and cuneiform abnormalities are rare but may cause:
Laryngeal inlet collapse
Inspiratory stridor or airway resistance during breathing
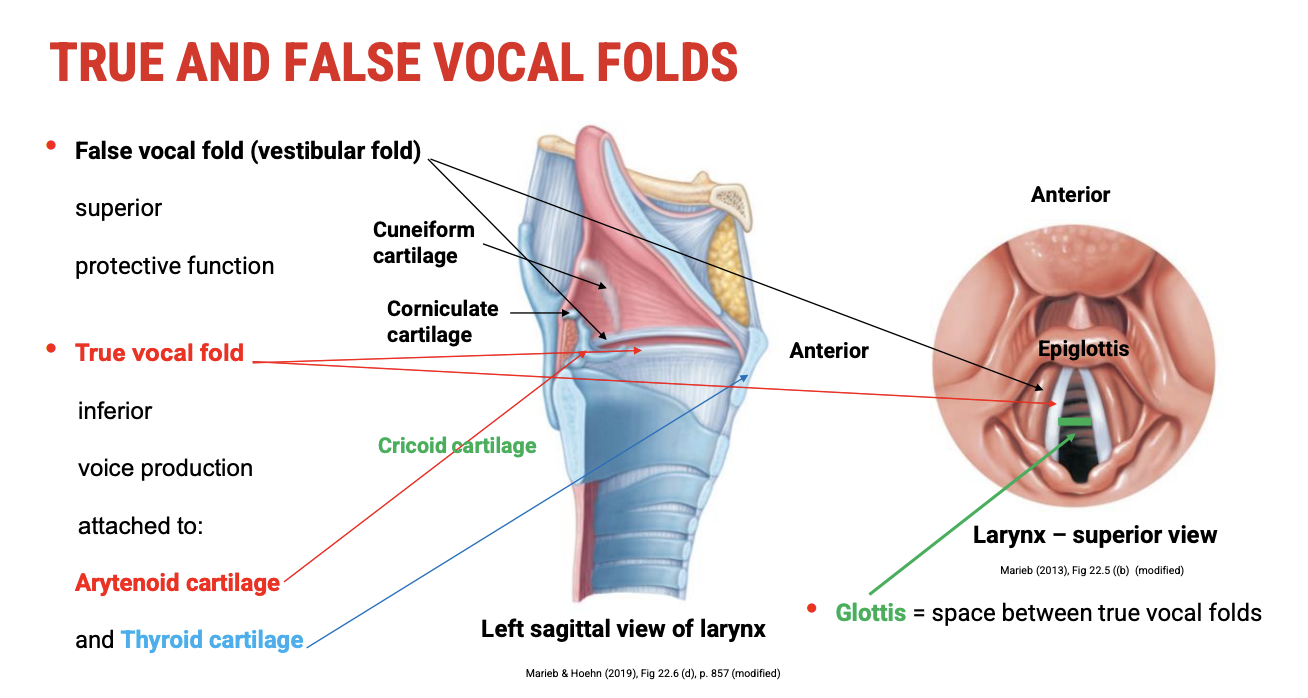
True vs False Vocal Folds
🧩 Overview of the Folds
The vocal folds (cords) are key components of the larynx. They are divided into false (vestibular) and true folds, each with distinct locations, structures, and functions.
🔹 False Vocal Folds (Vestibular Folds)
Location: Superior to the true vocal folds
Function:
Protective — help close the airway during swallowing
Not involved in normal phonation (sound production)
Structure:
Composed of mucosa and vestibular ligament
Contain few muscle fibres
Why “Vestibular”?
“Vestibule” refers to an entrance — these folds form the roof of the laryngeal vestibule, guarding the airway entrance
Clinical note: Can contribute to ventricular phonation (a voice disorder where false folds are used to compensate)
🔸 True Vocal Folds
Location: Inferior to the false vocal folds
Function:
Voice production (phonation)
Contribute to airway protection and control
Attachments:
Posteriorly to the arytenoid cartilages
Anteriorly to the inner surface of the thyroid cartilage (at the midline)
Structure:
Formed by the vocal ligament and vocalis muscle (part of thyroarytenoid)
Covered by stratified squamous epithelium (due to mechanical stress)
Highly dynamic: Tension, length, and position change with voice and breathing
🔳 Glottis
Definition: The space between the true vocal folds
Function:
Opens (abducts) during breathing
Closes (adducts) during phonation or protective reflexes (e.g. coughing)
Importance: Acts as a sphincter to protect lower airways and control vocal tone
👶 Relevance to Robert
Voice issues in children often involve the true vocal folds — e.g. nodules, poor closure, or misuse
Observation of glottic behaviour can reveal key pathologies (e.g. incomplete closure, asymmetry, or tension abnormalities)
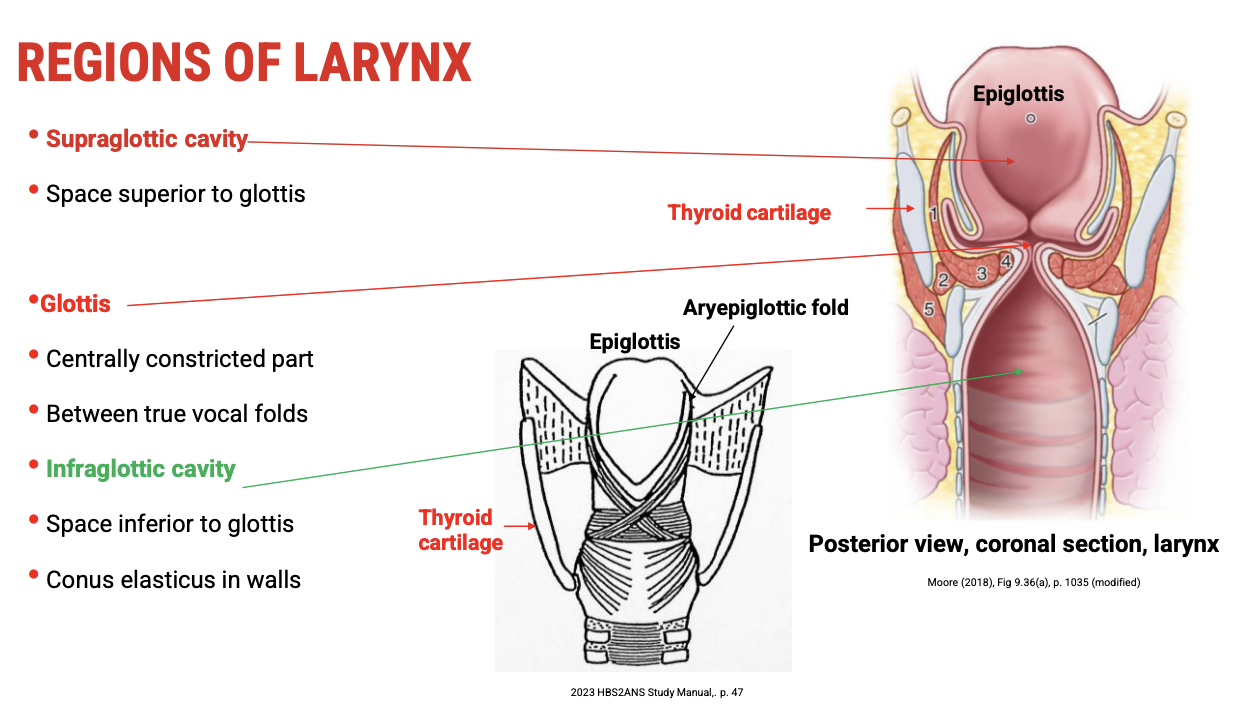
Three Regions of the Larynx
Understanding the division of the larynx is essential for identifying the location of lesions, voice pathologies, and functional roles of each region — especially in the context of paediatric voice disorders like Robert's.
1⃣ Supraglottic Cavity (Vestibule)
Location: Above the glottis (superior to the true vocal folds)
Boundaries:
Superior: Laryngeal inlet
Inferior: Vestibular (false vocal) folds
Contents:
Epiglottis
False vocal folds (vestibular folds)
Aryepiglottic folds
Function:
Assists in airway protection
Redirects food away from glottis during swallowing
Epithelium: Mostly respiratory epithelium (except areas under mechanical stress)
2⃣ Glottis
Location: Middle part of the larynx
Includes:
True vocal folds
Rima glottidis — space between the folds
Function:
Voice production
Sphincteric protection during swallowing and coughing
Highly dynamic: Width and tension adjust during phonation, respiration, and effort closure
3⃣ Infraglottic Cavity
Location: Below the glottis, extending to the lower border of the cricoid cartilage
Boundaries:
Superior: Lower edge of true vocal folds
Inferior: Continues into the trachea
Contents:
Lined by conus elasticus (a key fibroelastic structure)
Function:
Supports the vibratory mechanism of the vocal folds from below
Forms part of the cricovocal membrane, contributing to the vocal ligament
Conducts air to and from the trachea
⚙ Conus Elasticus (Lateral Cricothyroid Ligament)
Structure:
Shaped like an inverted cone
Extends from the cricoid cartilage upward to the vocal ligaments
Function:
Helps form the true vocal folds
Provides tensile strength and recoil properties for vibration
Integral to phonation mechanics
👶 Clinical Link to Robert
Pathology in the supraglottic or infraglottic areas (e.g. inflammation, mass lesions, malformations) can:
Impede airflow
Alter voice quality
Influence resonance or pitch
Intrinsic Ligaments of the Larynx & Their Functional Significance
The intrinsic ligaments of the larynx form a critical part of the inner lining of the “tube within a tube” structure. These ligaments give rise to the true and false vocal folds, and their elasticity and tension are key to voice production and airway protection.
🔹 1. Quadrangular Membrane
Location: Lines the supraglottic cavity
Extent: From the lateral edges of the epiglottis to the arytenoid cartilages
Lower border:
Thickens to form the vestibular ligament
This ligament is covered by mucosa to become the false vocal fold (vestibular fold)
Function:
Helps seal the supraglottic airway during swallowing
Structural support for the upper larynx
Not involved in phonation
🔸 2. Conus Elasticus (Cricovocal Membrane)
Location: Lines the infraglottic cavity (below the glottis)
Structure: A cone-shaped fibroelastic sheet extending from:
Superiorly: Vocal ligaments (true vocal folds)
Inferiorly: Upper border of the cricoid cartilage
Upper border:
Thickened to form the vocal ligament
This ligament is covered by stratified squamous epithelium and forms the true vocal fold
Contains: Elastic tissue — enabling stretch and recoil
📢 Functional Importance of Elasticity
Conus elasticus = key player in phonation:
Its elastic properties allow the vocal folds to:
Stretch to modulate pitch
Tense to generate subglottic pressure
Vibrate efficiently for sound production
Greater elasticity = better pressure regulation:
Especially for increasing loudness (higher subglottic pressure)
👶 Relevance to Robert
The development or pathology of the conus elasticus or quadrangular membrane can:
Affect voice quality (e.g. breathiness, weakness)
Limit loudness or vocal projection
Impact vocal fold tension (e.g. in paediatric voice misuse or congenital abnormalities)

Joints of the Larynx
1⃣ Cricoarytenoid Joints
Location: Between the cricoid cartilage and the arytenoid cartilages
Type: Synovial pivot joints
Movements allowed:
Rotation
Sliding (gliding)
Tilting
Functional significance:
Control the position and tension of the vocal ligaments (true vocal folds)
Enable abduction (opening) and adduction (closing) of the vocal folds during breathing and phonation
Clinical note: Dysfunction can cause vocal fold paralysis or immobility, affecting voice and airway protection
2⃣ Cricothyroid Joints
Location: Between the thyroid cartilage and the cricoid cartilage
Type: Synovial plane joints
Movements allowed:
Rocking (tilting) forward and backward of the thyroid cartilage
Functional significance:
Adjusts tension and length of the vocal ligaments
Primarily responsible for pitch modulation (higher pitch by increasing tension)
Clinical note: Impairment can result in monotone voice or difficulty adjusting pitch
🙏 Conclusion
These joints are essential for the fine motor control of voice production and airway protection.
Their synovial nature allows for smooth, flexible movements required for dynamic vocal fold positioning.