Lymph Nodes
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
What are the 3 common causes of lymphadenopathy
reactive hyperplasia
Inflammation (lymphadenitis)
Neoplasia
Two key functions of lymph nodes
filtering lymph
Initiating immune responses
Why does lymphadenomegaly occur
Lymph Flows through node → macrophages that line the sinuses remove foreign material → antigen recognition by dendritic cells/macrophages/sensitized B cells → helper T lymphocytes (Th1 = cytotoxic, Th2 = humoral (Ab) response) → B cells in follicles proliferate → germinal center hyperplasia
What is required for determining the underlying cause of lymphadenomegaly?
Diagnostic sampling → FNA, cytology or biopsy
What is a baseline FNA of a normal lymph node?
75-85% small, well differentiated lymphocytes
<10-15% intermediate to large lymphocytes (lymphoblasts)
less than 3% plasma cells
Less than 1% macrophages, neutrophils, eosinophils, mast cells
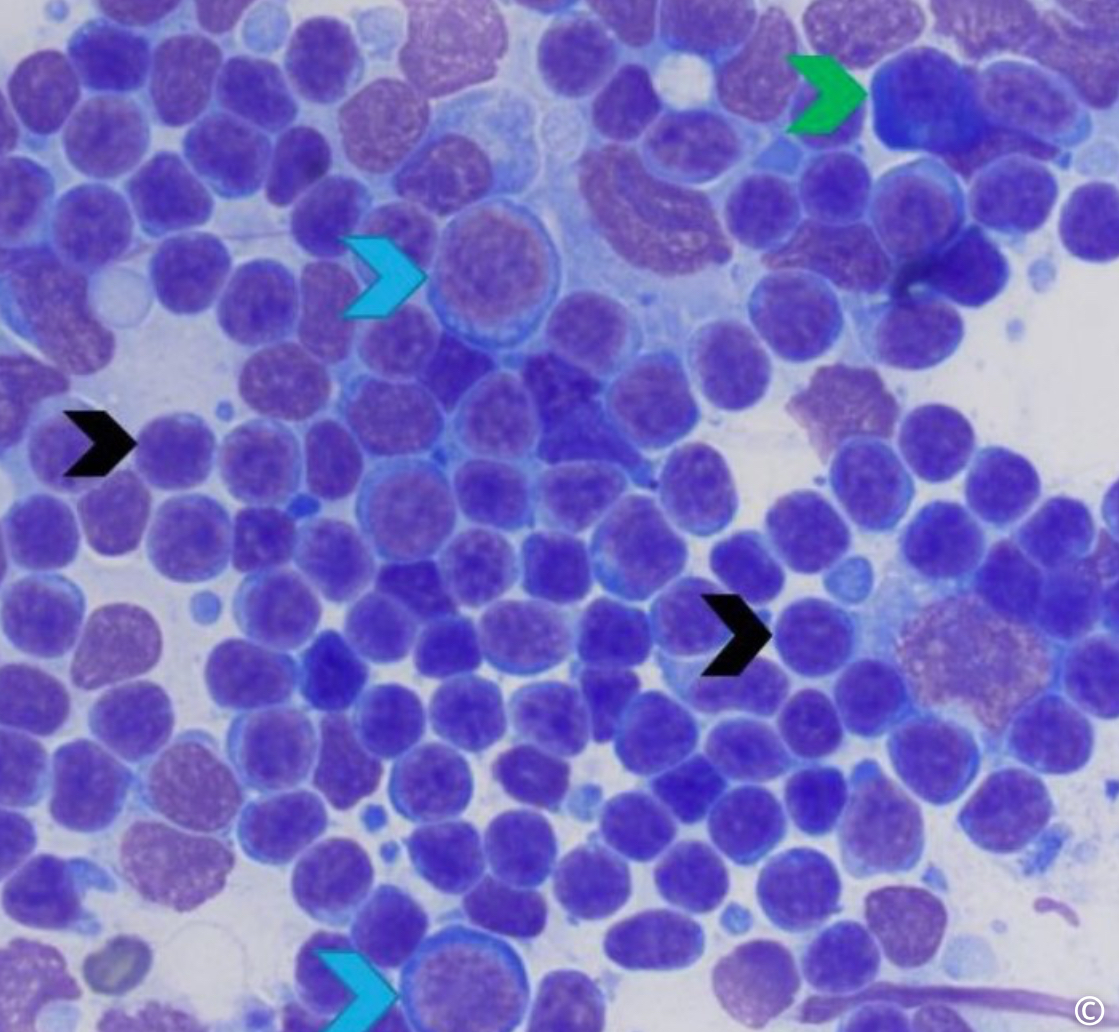
Cell ID (blue, black & green arrow)
blue arrow = plasma cell
Black arrow = small lymphocytes
Green arrow = lymphoblasts
What is reactive lymphadenopathy + example
Benign & common response to lymph nodes to antigenic stimulation in their drainage area. Not considered true inflammation - no significant neutrophilia infiltration, edema, and normal LN architecture is preserved
Can also occur in response to tumor antigens from a neoplasm located outside the node
No systemic illness, nonpainful lymph node, firm but not hard
Example: abscess in the sole of a cow foot results in an enlarged popliteal lymph node.
Mechanism of sole abscess to enlarged popliteal lymph node in reactive lymphadenomegaly
Sole abscess forms → antigens from abscess enter the lymphatic circulation → travel to the draining lymph node in reactive→ lymph node responds by proliferating lymphocytes
What is lymphadenitis
inflammation of a lymph node, often resulting from an infection in the area that the lymph node drains
Typically painful upon palpation, especially during acute stages of the disease
How can the predominant type of inflammatory cells within an inflamed lymph node (neutrophils, eosinophils/mast cells, macrophages) provide clues to its origin?
neutrophils → predominant in suppurative lymphadenitis, often indicates a bacterial infection
Eosinophils/mast cells → parasitic infection
Macrophages → granulomatous lymphadenitis, commonly present in chronic stages of various disease
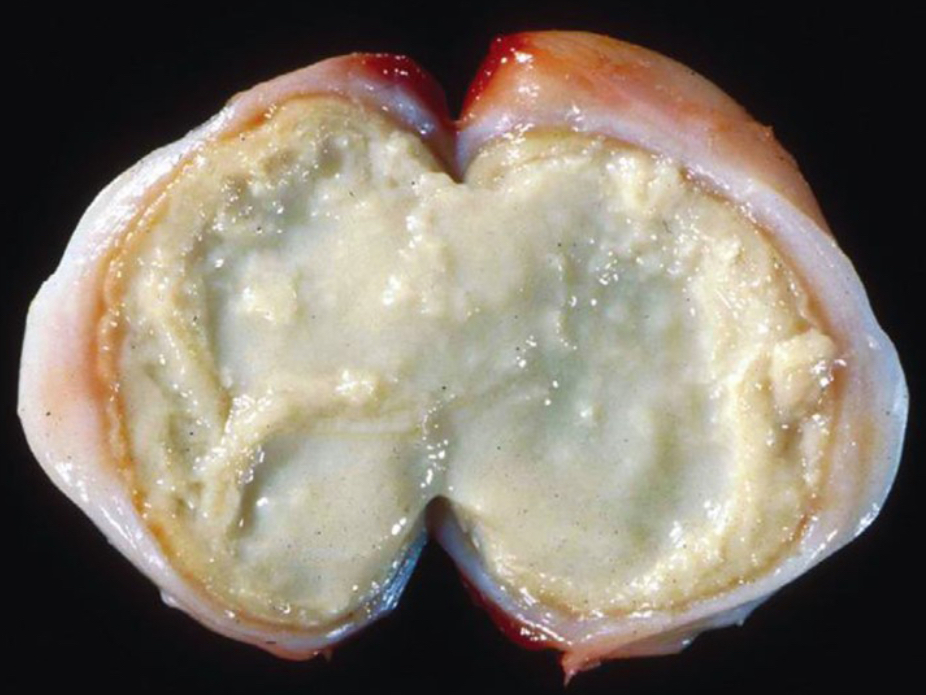
What are two common differential diagnoses of this type of necrosis?
certain bacterial infections
Mycobacterium bovis (bovine tuberculosis)
Corynebacterium pseudotuberculosis (cause of caseous lymphadenitis in sheep & goats)
How is CLA characterized?
Chronic suppurative lymphadenitis caused by Corynebacterium pseudotuberculosis
Primarily affects sheep & goats
Characterized by abscess formation in superficial lymph nodes & internal organs
Results in decreased milk & wool production, reduced growth rates, carcass condemnation
What are the features of Corynebacterium pseudotuberculosis?
Gram positive, Non motile, Facultative intracellular bacterial rod
Persists in soil contaminated with feces or exudates
Resistant to desiccation & sunlight
Pathogenesis of CLA
transmission (tail docking, castration, shearing or infected discharges or inhalation from infected animal→ invasion to local lymph node → suppurative lymphadenitis → lymphogenous & hematogenous dissemination in older animals → organ abscess → bacteria lives intracellularly, eventually killing host cell → releases more bacteria into surrounding tissue → macrophages arrive to site → chronic infection leads to formation of capsule of connective tissue
Clinical findings of CLA
enlargement of one or more superficial lymph node (parotid, submandibular, prescapular)
Lesions may have whitish/creamy pus
Weight loss
Reduced milk production
Discomfort on palpation
Progression to visceral disease → slow, occurs in older animals; affects lungs, liver, kidneys, or mediatstinal lymph nodes

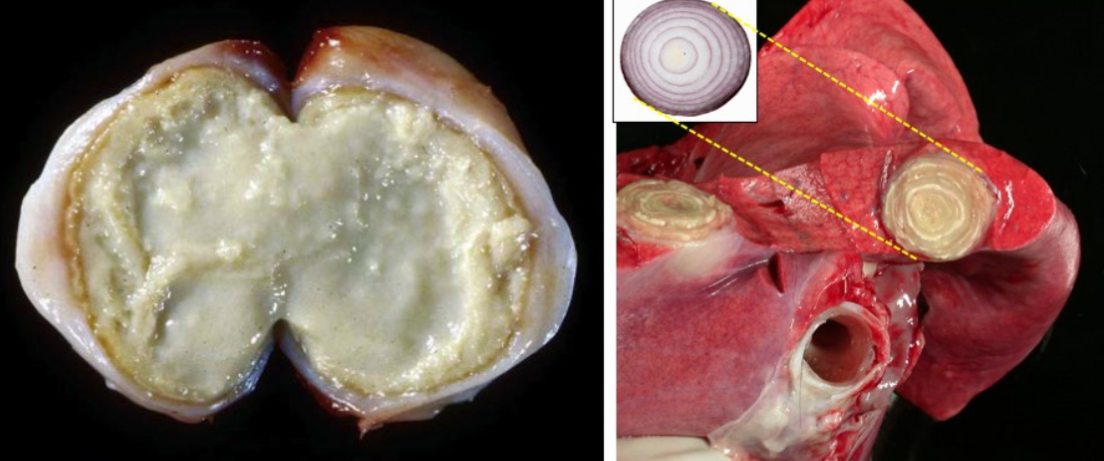
Gross findings of CLA
Enlarged LN with central core of thick creamy necrotic material, greenish-white & gritty
Older lesions = onion skin formed due to concentrically lamellated layers of fibrous connective tissue with alternating zones of caseous friable material
How would you confirm a diagnosis of CLA & what lab test would be used?
Collect pus samples from abscess using sterile techniques → submit lab sample for bacterial culture & identification (gold standard for confirming C. Pseudotuberculosis)
FNA from deeper or non ruptured lymph nodes
Blood samples for CBC or serological testing (need to determine if it is worth cost)
Cytology (cannot specifically ID Corynebacterium pseudotuberculosis)
What is effective prevention of CLA?
Good Biosecurity practices (isolating affected animals, limiting introduction of new animals without testing)
Regular herd screening through serology
Careful monitoring of wounds for signs of infection
Prompt tx of abscesses with drainage or surgical intervention can help reduce spread
Vaccination in areas where CLA is endemic
Pathogenesis of bovine tuberculosis
inhalation of infected aerosol droplets → respiratory tract infection → spread to regional lymph nodes (bronchial or mediastinal LN) → mycobacteria are phagocytosed by macrophages → some macrophages may clear the infection but others may allow bacteria to proliferate → granuloma formation
What constitutes the primary complex of bovine tuberculosis?
granulomas in the lungs & their draining lymph nodes
Bacteria can also spread through the blood stream & lymphatics and can lead to generalized disease
Gross lesions of bovine tuberculosis
appearance of affected LN varies based off of species, degree of immunity, type of mycobacteria involved - many animals show no clinical signs
Cattle
Multiple pale, caseous granulomas that may become calcified, indicating chronic granulomatous lymphadenitis
Deer & Possums
LN lesions are more suppurative
Clinical signs of bovine tuberculosis
enlarged lymph nodes in throat latch region
Chronic cough, occasional nasal discharge
Weight loss
Mild respiratory effort
What is lymphoma
Malignant lymphoid neoplasia arising in solid tissues (lymph nodes, spleen, gut associated lymphoid tissue)
Usually occurs without circulating neoplastic cells
Usually sporadic, but some are associated with viral infections
Classification of lymphoma - anatomic classification
Multi centric → multiple LN (dogs)
Alimentary → GI tract & mesenteric LN (cats)
Mediastinal → thymus or mediastinal LN
Cutaneous → skin
Extranodal → CNS, eye, kidney
Classification of lymphoma - cell type + prognosis
B cell → better prognosis
T cell → aggressive
Classification of lymphoma → how aggressive is it → cell size, mitosis index, nuclear figures
High grade → rapid growth, more responsive to chemo
Low grade → slower progression, harder to detect early
Classification of lymphoma - clinical staging
Stage l → single LN or single organ affected
Stage ll → multiple LN in a regional area
Stage lll → generalized lymphadenopathy
Stage IV → involvement of liver and/or spleen, with or without LN involvement
Stage V → involvement of bone marrow, blood, or other extra nodal sites (CNS, eye, lungs)
Diagnostic approach in lymphoma cases
FNA + cytology → first line diagnostic test to assess cells in the affective tissue, only okay for presumptive dx
Biopsy → confirms dx & allows grading & structural assessment
Immunohistochemistry → ID T-cells vs B cell origin in tissue samples, useful for prognosis & tx plan
Flow cytometry from FNA or blood
CBC & blood smear examination → assesses for leukemic phase or cytopenias
Thoracic/abdominal imaging → assess internal organ involvement & staging
Bone marrow aspiration → cases with cytopenias or suspicion of leukemic spread
PARR → confirms clinal lymphoid population
What is the most common presentation of lymphoma in dogs?
Multicentric (multiple LN affected), with generalized lymphadenopathy
May involve liver, spleen, & bone marrow
Dogs are usually clinically well despite large LN
Common lab findings of lymphoma in dogs
Non-regenerative anemia & thrombocytopenia with chronic disease or bone marrow involvement
Leukocytosis, lymphocytosis, or neoplastic lymphocytes in peripheral blood (usually seen in Stage V)
Paraneoplastic hypercalcemia → 10-20% of cases, most often associated with T-cell lymphoma
Always consider paraneoplastic hypercalcemia → elevated blood Ca levels caused by a tumor - hypercalcemia can lead to secondary complications (PU/PD + renal dysfunction)
Types of lymphoma in cattle
bovine leukemia virus (Enzootic bovine leukosis)
adult cattle 4-5 years
BLV infects B cells in cattle
Most infected animals are asymptomatic carriers
Multicentric lymphadenopathy
Common lymphoma sites → heart (R atrium), abomasum, uterus, LN, spinal canal
Sporadic lymphoma
juvenile form
Birth-7 months
Multicentric, involving LN, bone marrow, liver, kidneys
May cause dystocia
Often presents with leukemia
Thymic form
6-24 months
Massive thymic enlargement, causes ventral neck swelling (cranial thoracic mass)
Leukemia uncommon
Cutaneous form (rare)
1-3 years
Presence of skin nodules that may ulcerate or regress
Internal organ infiltration occurs later
Leukemia rare
How does lymphoma present in horses?
visceral organs involved → LN, spleen, GIT, liver, kidneys
Leukemia rare
Types of lymphoma in cats
LYMPHOMA IS MOST COMMON MALIGNANT NEOPLASM IN CATS! Can affect virtually any organ system, ALWAYS CONSIDER IN DDX FOR CHONIC ILLNESS IN OLDER CATS w/ VAGUE SIGNS/LYMPHADENOPATHY!
Sporadic (FeLV-negative) lymphoma
Middle aged to older cats (>10 years)
Chronic inflammation, genetic mutation, & environmental exposures may contribute
Common organs affected → GIT, mesenteric LN, liver, spleen, kidneys
Retrovirus-associated lymphoma
Feline leukemia virus (FeLV) associated lymphoma
Younger cats (<4 years)
Thymus is more commonly affected, Multicentric form common
Gamma retrovirus that can cause direct cell transformation by insertional mutagenesis
1/3 of cats may develop lymphoma or leukemia
Feline immunodeficiency virus (FIV) associated lymphoma
Characterized by increased susceptibility to opportunistic infections, neurological disease, tumors
Acquired immunodeficiency syndrome
Clinical signs of FeLV
dyspnea, coughing
Muffled heart sounds
Pleural effusion
Rads - cranial mediastinal mass may displace lungs & heart
Cats can have a thymic lymphoma & be FeLV negative
Clinical signs of alimentary or gastrointestinal lymphoma in cats
most common presentation (esp older, FeLV negative cats)
Weight loss
V/D
Anorexia
Thickening of intestinal wall with loss of normal layering
Mesenteric lymphadenopathy
A young dog presents for vaccination. The only abnormal finding is mild submandibular lymph node enlargement. Cytology shows a mixed population of lymphocytes, some plasma cells, and macrophages. What is the most likely diagnosis?
Lymphoma
Lymph node metastasis
Reactive lymph node hyperplasia
Suppurative lymphadenitis
Reactive LN hyperplasia
A ewe has firm swellings around the head and neck. Post-mortem shows laminated abscesses in lymph nodes.
What is the most likely cause?
Corynebacterium pseudotuberculosis
Mycobacterium bovis
Mannheimia haemolytica
Trueperella pyogenes
Corynebacterium pseudotuberculosis → causes caseous lymphadenitis with characteristic onion ring abscesses
A cow shows weight loss and chronic cough. Retropharyngeal lymph nodes are enlarged and gritty on sectioning.
Most likely diagnosis?
Enzootic bovine leukosis
Sporadic bovine lymphoma
Tuberculous lymphadenitis
Suppurative lymphadenitis
Tuberculous lymphadenitis → granulomatous inflammation with caseous necrosis & mineralization is typical of TB
A 6-year-old dog has generalised lymphadenomegaly. Cytology shows large, monomorphic lymphocytes with frequent mitoses. What is the most likely diagnosis?
Lymphoma → presence of large, monomorphic & presence of mitotic figures + generalized lymphadenopathy is consistent with lymphoma
A cat presents with vomiting and an abdominal mass. Imaging shows thickened intestines and enlarged mesenteric lymph nodes. What is you most likely diagnosis? Include the correct terminology according to the anatomic location.
Alimentary lymphoma → most common form of lymphoma in older cats, affects GI tract & mesenteric nodes
A 2-year-old beef steer presents with progressive weight loss, dullness, and firm enlargement of the prescapular and mesenteric lymph nodes. The remainder of the herd appears unaffected. BLV serology is negative. Based on the signalment and findings, which form of lymphoma is most likely?
Adult sporadic lymphoma
BLV negative, affects young adult, presents with peripheral lymphadenopathy without herd involvement
Cytology of a cat's lymph node is inconclusive. PARR testing is recommended. What is the main purpose of this test?
ID clonal lymphocyte population
Helps distinguish lymphoma from reactive processes