Micturition
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
16 Terms
What is Micturition?
Micturition is the act of passing urine or peeing and occurs in 2 phases:
→ Filling/Storage Phase
→ Voiding Emptying Phase
The phases of micturition are controlled by the sympathetic (storage), parasympathetic (peeing), and somatic nervous system
What are the two structures comprising the bladder wall?
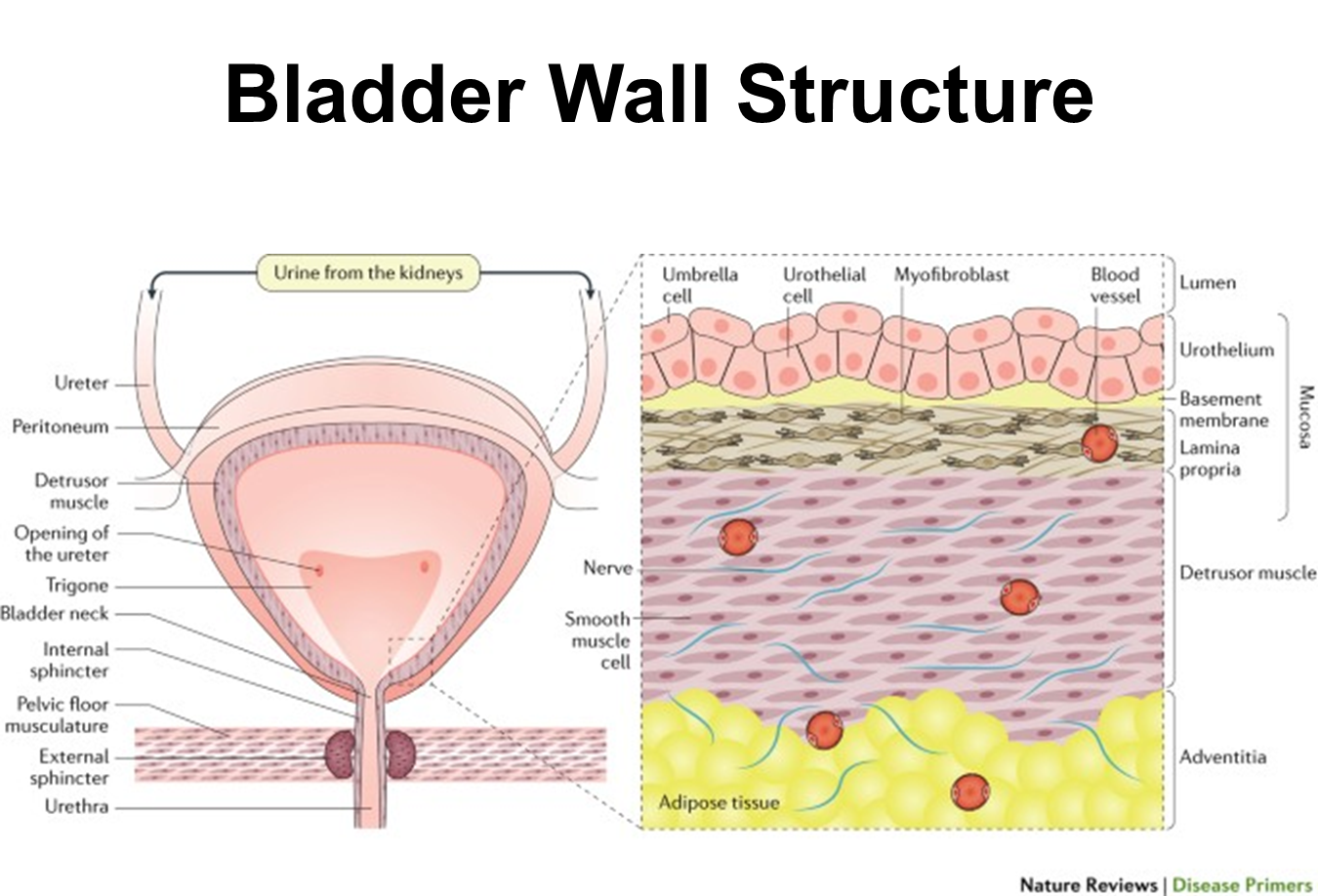
The bladder is composed of a mucosal layer and the detrusor muscle
1) Mucosal Layer composed of the urothelium, basement membrane and lamina propria
→ Urothelium is a stratified epithelial layer of transitional epithelium and umbrella cells that have varied thickness
2) Detrusor Muscle is randomly oriented smooth muscle with no insertion or origin site
→ this allows for the bladder to just squeeze and maintain continuous tension at different muscle lengths
What is the extracellular matrix that surrounds the bladder
The ECM creates a scaffolding for the detrusor muscle. It is comprised of type 1 and 3 collagen as well as a variety of proteins and elastic fiber
1) If the bladder strains due to some kind of obstruction, it will shift the ECM leading to stiffening of the matrix and making the bladder stiff
→ leads to a loss of compliance due to increase in collagen type III deposition
What nerves are responsible for sympathetic innervation to the bladder?
Sympathetic innervation to the bladder is provided by the peripheral nerves exiting the thoracolumbar spinal cord around T10-L2
1) Preganglionic nerves from T10-L2 and are located at varied locations
2) Motor signals that innervate the bladder will travel via the hypogastric nerve
→ this modulates contraction of the bladder neck smooth muscle and relaxation of the bladder
→ inhibits parasympathetics, preventing peeing
What receptors stimulate the SNS at the bladder?
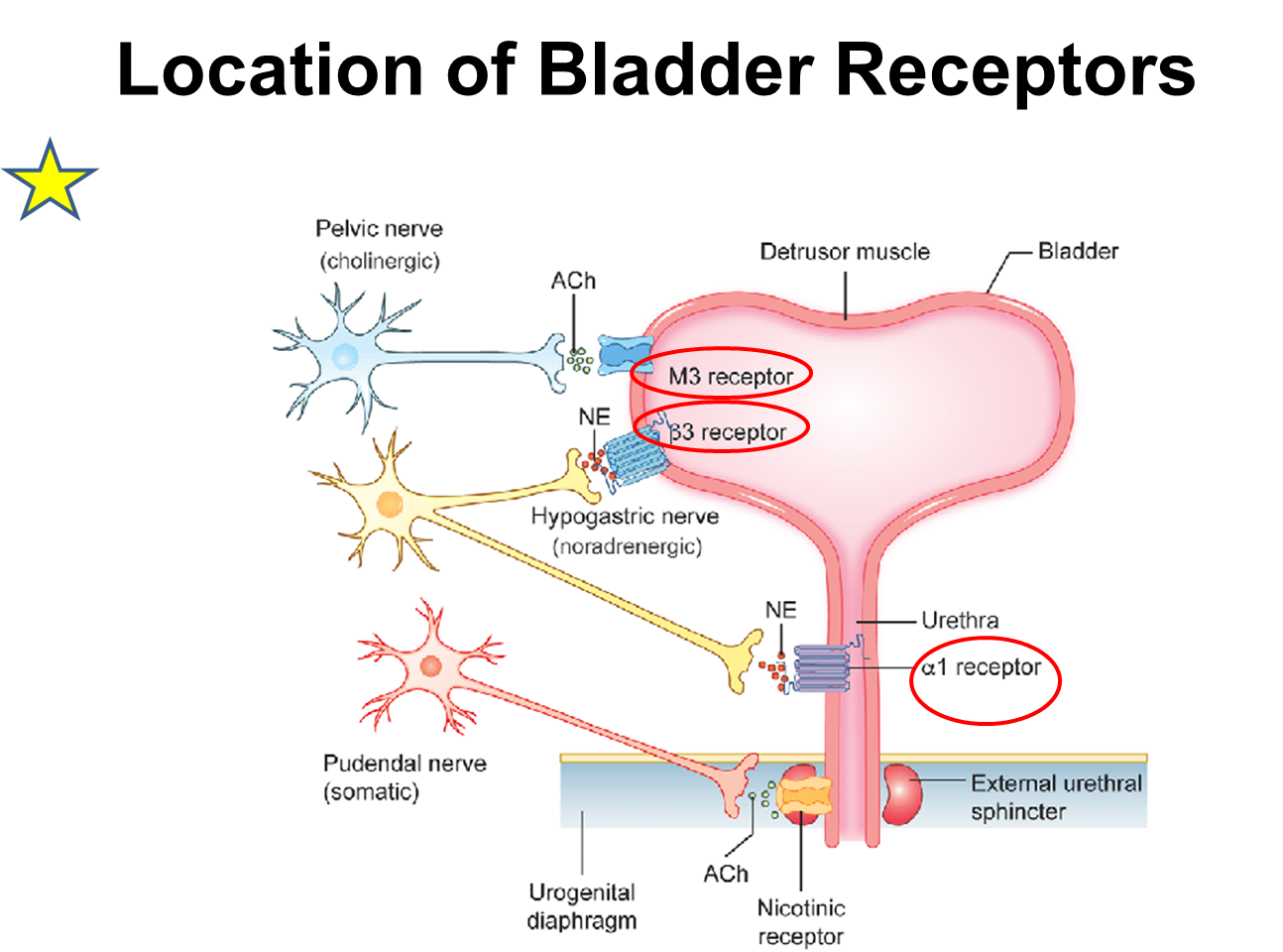
Stimulation of the SNS via the hypogastric nerve at the bladder occurs via both beta and alpha receptors
1) Alpha 1 Subtypes (a,b,d) are located at the prostatic urethra in men and proximal urethra in women
→ stimulation of these receptors causing contraction of the bladder outlet leading to storage
→ Blockade of these receptors will lead to emptying of the bladder
2) Beta Adrenergic Receptors on the detrusor muscle, typically type II and III
→ stimulation will cause relaxation of the detrusor muscle
What is the parasympathetic innervation of the bladder?
Parasympathetic Innervation of the bladder is done via the peripheral nerves that exit from the craniosacral spinal cord
1) Preganglionic nerves will exit at S2-4 at the spinal cord
→ these nerves will travel long distances to ganglia near the target organ
2) Signals are then carried via the pelvic nerve
→ this will be responsible for modulating bladder contractions and promoting peeing
What receptors stimulate the PNS at the Bladder?
Muscarinic Receptors at the bladder in the supratrigonal region are stimulated by the pelvic nerve leading to peeing
1) Muscarinic 2 Receptors are the highest concentration in the bladder
2) Muscarinic 3 Receptors are responsible for detrusor contraction
What is the Somatic Innervation to the Bladder?
Somatic Innervation to the bladder is supplied by the pudendal nerve
1) The preganglionic nerves will exit the spinal cord at the S2-S4 with the nerve bodies being located at Onuf’s nucleus
2) Signals are then carried via the pudendal nerve and modulate striated muscle urethral sphincter contraction via nicotinic receptors
→ Promotes external sphincter contraction which promotes storage
How does the Storage and Voiding Reflex occur?
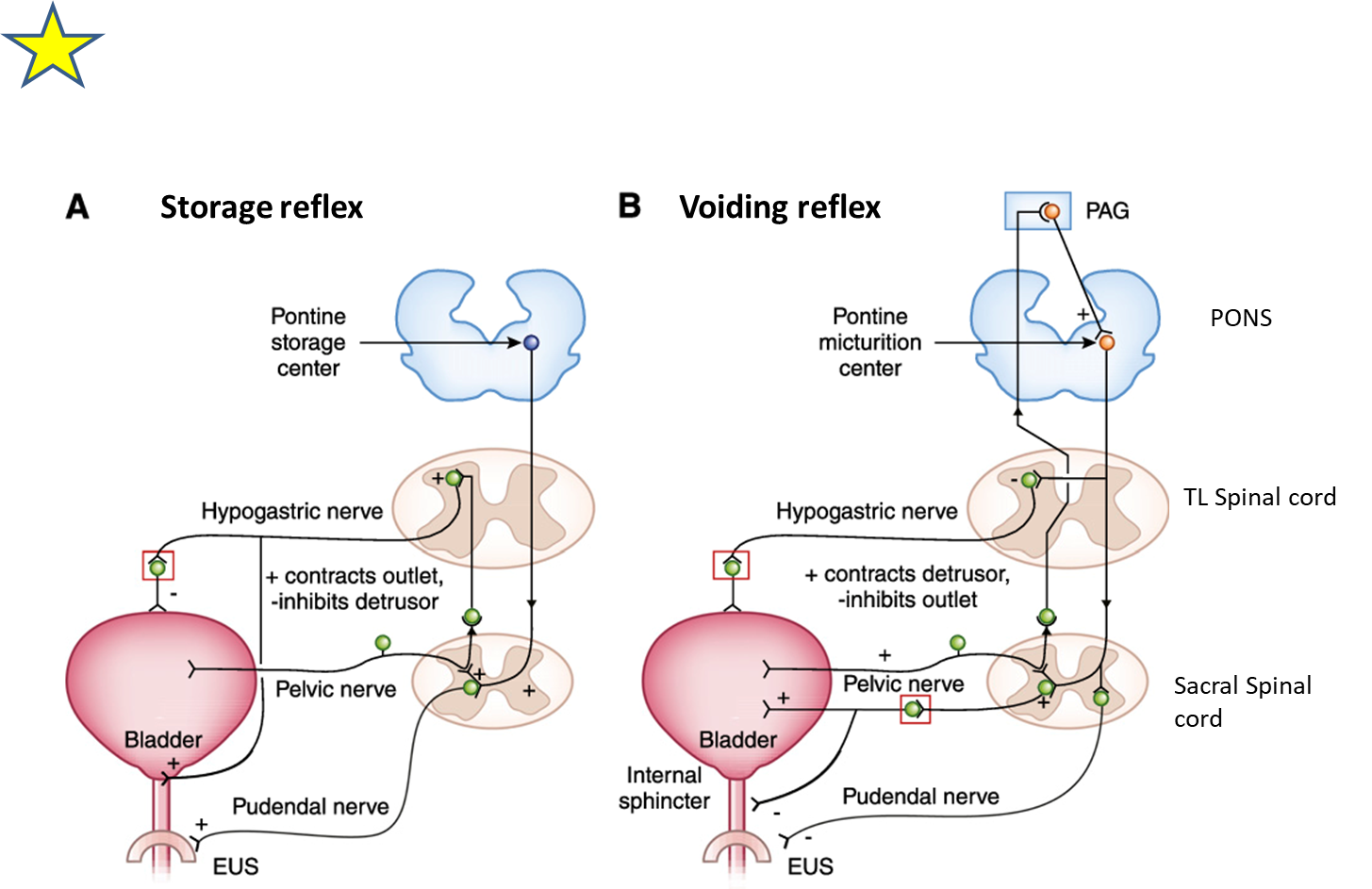
The storage and voiding reflexes are controlled by afferent fibers contained in the pelvic nerves. Stretch receptors on urothelium and detrusor muscle will coordinate signals through the afferent fibers in order to control these reflexes
→ reflexes are coordinated based on the degree of stretch
1) Storage Reflex
→ patient gets a sensation where there is a small amount of stretch which will send signals to the pontine storage center
→ that we are filling the bladder but are not in a position to urinate
→ this will send signals down the spinal cord through the hypogastric cord promoting storage via SNS activation
2) Voiding Reflex
→ patients gets a large amount of stretch, sending afferent signals that bypass the spine and travel to the periaqueductal gray in the brain and pontine micturition center in the brainstem
→ leads to activation of the parasympathetic nervous system via the pelvic nerve leading to urination
What are the two issues that cause incontinence
Incontinence or bladder storage issues can be caused by overactive bladder and stress incontinence
1) Overactive bladder
→ condition characterized by sudden involuntary contractions of the detrusor muscle, causing incontinence
→ patients will urinate frequently and cannot delay urination
2) Stress Incontinence
→ condition characterized by incontinence followed by increase in stress or increase in intraabdominal pressure (coughing, sneezing, laughing)
→ caused by a incompetent external sphincter
What are the two issues that cause retention
Retention can be classified as either detrusor or outlet related
Detrusor Related
→ Detrusor underactivity leading to diminished or absent contractions
Outlet Related (Bladder Outlet Obstruction)
→ failure to pee if there is any obstruction to the urethra
Patients with these issues can have urinary hesitancy, incomplete bladder emptying, and increased urinary frequency
What is Neurogenic Bladder?

Neurogenic Bladder is any bladder dysfunction as a result of some neurological condition, and can manifest as either incontinence or retention. The location of the neurological lesion can indicate the kind of bladder issues they have
1) Brain Lesion
→ detrusor overactivity or a spastic bladder
2) Spinal Cord Lesion
→ varied presentation depending on where in the spinal cord the lesion occurs
3) Peripheral Lesion
→ varied presentation depending on the location of the lesion in the periphery
What are the three non-invasive measures for bladder function?
1) Frequency Volume Chart or a Bladder Diary
→ diary detailing how often they drink fluids and how often they pee
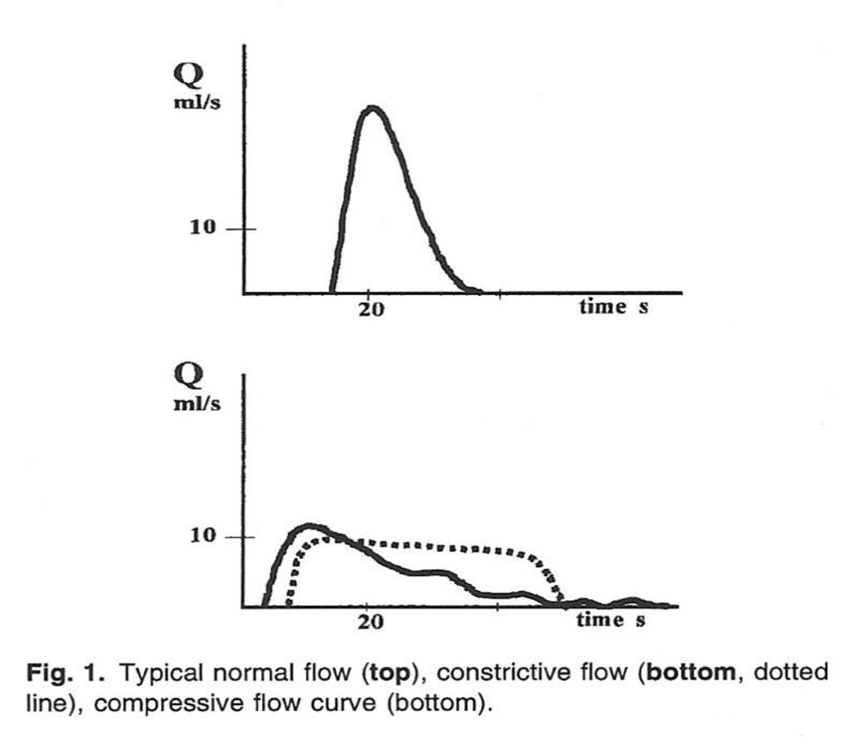
2) Uroflowmetry
→ measures the speed of peeing over time (ml/sec)
→ in a normal person it should produce a bell shaped curve
→ compressive flow is shifted to the left and is flatter
→ constrictive flow is bread loaf shaped
3) Post Void Residual Volume
→ scans the amount of urine remaining in the bladder
What is Urodynamics? What is considered normal?
Urodynamics is an invasive bladder study that assess bladder function
→ tells us sensory function and motor function to the detrusor muscle and sphincters
1) Normal Urodynamics
→ First Sensation - patient becomes aware of bladder filling (150cc)
→ First Desire - urge to urinate but can hold it (200-400cc)
→ Strong Desire - persistent desire to pee (400-600cc)
2) Compliance should be greater than 20cc/cmH2O while anything less than ten cc/cmH2O is considered stiff
What is Benign Prostatic Hyperplasia? How is it treated?
BPH Is a noncancerous enlargement of the prostate that can lead to compression and obstruction of the urethra
When treating BPH you want to decrease voiding pressure by relaxing or opening the outlet/bladder neck
1) Alpha 1 Blockers
→ blockage of alpha receptors on the bladder neck leads to relaxation
2) Outlet Procedures
What puts the kidneys at risk when the bladder is not functioning properly?
both of these can lead to vesicoureteral reflux which is a condition where urine flows backwards from the bladder into ureters up towards the kidney
High Pressure Storage
→ low compliance
→ high pressure detrusor muscle overactivity throughout filling
High Pressure Voiding or bladder outlet obstruction
→ Detrusor external sphincter dyssynergia
→ Detrusor internal sphincter dyssynergia
→ Benign Prostatic Hyperplasia
→ Urethral stricture