TSE and ANS cases
1/31
Earn XP
Description and Tags
- give examples of TSEs - discuss role of prions in TSE development - describe pathology of TSE and current diagnostic procedures - clinical signs of diseases - transmission risk of TSE in context of public health - explain economic impact of TSEs in UK - relate clinical abnormalities in patients with dysfunction of the ANS to normal autonomic structure and function
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
32 Terms
give examples of TSEs in sheep and goats
scrapie and atypical scrapie
give examples of TSEs in mink
mink spongiform encephalopathy
give examples of TSEs in deer and elk
chronic wasting disease
give examples of TSEs in cattle
BSE
give example of TSE in cats
FSE (feline spongiform encephalopathy)
what is an example of a TSE disease affecting camels
camel prion disease
what are TSEs/prion diseases
neurological disorders
they have very long incubation periods
neuronal loss
invariably fatal
caused by misfolded prion protein PrPSc (prion protein scabie - because scabie was the first prion disease found)
why does the histology of TSEs have the spongy appearance?
prions cause neurone damage
gives a spongy appearance
what is a prion
a completely novel infectious agent
they’re a misfolded protein that goes from primarily alpha structures to having more beta structures. It’s practically indestructible.
what is the role of prions in TSE disease development
it’s an autocatalytic protein, generates more of itself.
It has different shapes depending on the disease
Accumulates over time, especially in the brain which leads to the symptoms over time
can be inherited which leads to faster misfolding and accumulation
what are the properties of prions
relatively insoluble
self catalytic conversion
exceptionally high stability for a protein
resistant to proteases
resistant to heat treatment
resistant to UV
what are the concerns with prion properties
can’t easily decontaminate premises or in clinical setting
can survive in environmental reservoirs for many years
how are genetics linked to TSEs?
some animals are more genetically susceptible to PrPSc
Some are exposed to the prion leading to spontaneous conversion - inherited
what is the pathology of TSEs
prion is absorbed in the gut
passes through Peyer’s patches (especially M cells)
passes through gut associated lymphoid tissue
passes through ENS
goes to SLOs (spleen, lymph nodes, tonsils, appendix) or straight to CNS
ends up in the brain
what is the pathology of TSEs dependant on?
species
shape of prion strain
What are the 2 places we test for prions in the brain and why
just a brain stem sample post mortem
a sample of the cerebrum and cortex as well as brain stem
why?
classical scrapie accumulates in the brainstem (obex)
atypical/Nor98 scrapie accumulates in the cerebrum and cerebellum
How do we test for what kind of strain of prion disease an animal has?
why do we do prion strain testing?
we need to compare strains to existing ones to identify what kind of prion it is
need to know if it’s zoonotic or not
how do we find out if a prion strain is zoonotic and therefore poses a threat?
place the prion in with a mouse with a transgenic gene for the human prion.
See if a disease develops
if it does = zoonotic
what are clinical signs of TSE diseases?
weight loss, subtle behavioural changes
licking lips, grinding teeth, scratching
pruritus (scrapie)
posture, gait
ataxia, tremors
none, animal found dead
What are the 5 ways we can diagnose TSE diseases?
transfer brain extract to permissive experimental animal (susceptible mouse strain)
ethical issues
long incubation periods and cost
specific identification of PrPSc, disease specific protein
confirmatory tests e.g. histology, immunohistochemistry
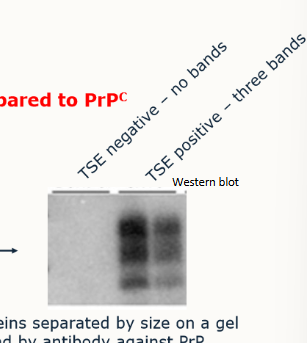
Western blots
ELISAs
how do western blot tests and ELISAs work?
rely on protease resistance of PrPSc compared to PrPC
sample is taken from obex and homognenised in buffer solution
sample is digested with protease
separated by size on a gel (proteins present), bound by an antibody against PrP
How are all TSE confirmatory tests conducted
post mortem
what 2 groups do prions fall into in regards to transmission
very difficult to transmit b/w susceptible hosts:
all human TSEs including vCJD
BSE (& FSE) → zoonotic
MSE
readily transmitted
scrapie in sheep/goats → non-zoonotic
CWD in cervids → unlikely to be zoonotic
how are the 2 groups of TSE transmitted?
Group 1: through medical procedure or ingestion of contaminated food/feed
Group 2: direct contact and environmental reservoirs
compare vCJD to CJD
variant:
affects much younger age group
different initial symptoms (psychiatric/behavioural vs dementia)
causes death > 1 year after illness onset (vs 4-5 months)
How was the BSE epidemic controlled?
culling, cohort culling (animals born 2 years either side of the cow detected with BSE were culled)
feed ban for ruminant material
older cattle banned from human food chain
ban of specified-risk material from food chain
export ban
surveillance (veterinary profession)
plan to eradicate TSEs from sheep
outline the economic impact of TSEs in the UK
BSE outbreak cost around £3.7bn
direct costs of BSE:
loss of income for agriculture/government compensation
culling and older cattle can’t be used
export ban
collapse of home market for beef
lower market for milk, lamb
cost of surveillance
cost of research
plan to eradicate all TSEs in sheep
what is the national scrapie plan (NSP)?
suspect cases of scrapie: report to Animal health division office, farm visit by veterinary officer, compulsory slaughter and tests, movement restrictions until lab results available.
Compulsory scrapie flocks scheme (CSFS) - any flock with suspected and positive scrapie test, will be registered automatically registered in CSFS, state veterinary service VO visit to identify all sheep and goats on holding (including embryos)
what are we trying to do to help improve genetic resistance to scrapie?
genotyping
sheep with required resistant genotypes (ARR/ARR = desirable, AHQ/VRZ or AHR/VRQ or VRQ/VRQ = undesirable)
selected for breeding or culled/slaughtered for food chain as appropriate - 3 year testing
what is atypical scrapie?
first identified in Norway in 1998
all clinical cases presented with ataxia w/o pruritus or wool loss
positive fro rapid screening ELISAs
low molecular weight fragment on Western blot
immunopathology in more rostral areas of brain including cerebellum
immunostaining at obex distinct from classical scrapie
in older animals
spontaneous
what other new strains have been discovered?
atypical BSE
CWD - only affects free-ranging wildlife - chronic wasting disesase