SSS 1,2,3,5,6,7,9,11
1/181
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
182 Terms
Myopia
short sightedness
condition in which an image of a distant object becomes focused in front of retina, either bc eyeball axis is too long or because refractive power of object is too strong
corrected by concave (minus) lenses
Hyperopia
far sightedness
refractive error in which image of a distant object becomes focused behidn retina, either bc eyeball axis is too short or bc refractive power is too weak
corrected by convex (plus) lenses
Astigmatism
eye condition that exists when surface of cornea or crystalline lens is irregularly shaped
corrected by toric lenses (football shaped)
Presbyopia
age-related loss of near vision, typicaly starting around 40, caused by eye’s lens becoming less flexible and losing its ability to focus on close objects
age related loss of accomodation
corrected by convex (plus) lenses
Symptoms in an eye exam
abnormal vision
abnormal sensation eg. discomfort
altered appearance
types fo abnormal vision
reduced
central
peripheral
impaired night or colour vision
onset
if sudden —> vascular
or gradual
.
floaters
haemorrhage
inflammation
vitreous degeneration
muscae volitantes
.
flashers
irritative stimulation of retinal or visual pathway
can be unilateral —> retinal deatchment?
bilateral —> migraine/basilar artery insufficiency
.
haloes - rainbow coloured rings around lights due to corneal oedema or increased intraocular pressure
metamorphopsia / micropsia
apparent distortion of straight lines/minification of objects due to retinal oedema or macular degeneration
diplola
binocular
resolves when either eye is covered, due to misalignment of visual axes
monocular
persists when unaffected eye is covered
caused by optical/intraocular problems (not alignment)
typical causes
cataracts, corneal irregularity/scar, refractive error, dry eye, intraocular foreign body
Abnormal sensation types
foreign body sensation
subjective localisation unreliable
causes include: trichiasis, entropion, conjunctivitis, dry eye
local anaesthetic relieves
photophobia
iritis
keratitis
cycloplegic drops relieves
severe deep pain
acute angle closure glaucoma
zoster/shingles
asthenopia (eye strain)
occurs after intensive use of eyes
due to
inadequately corrected refractive error
heterophoria
watery eyes/ discharge
overproduction (due to ocular irritation or FB)
faulty drainage
instability (dry eyes often blepharitis)
Types of altered appearance
What are the 3 mechanisms of Cellulitis
spread from local infection like sinusitis
skin disruption
haematogenous spread (common under age 2)
GAS/staph/s.pneumo
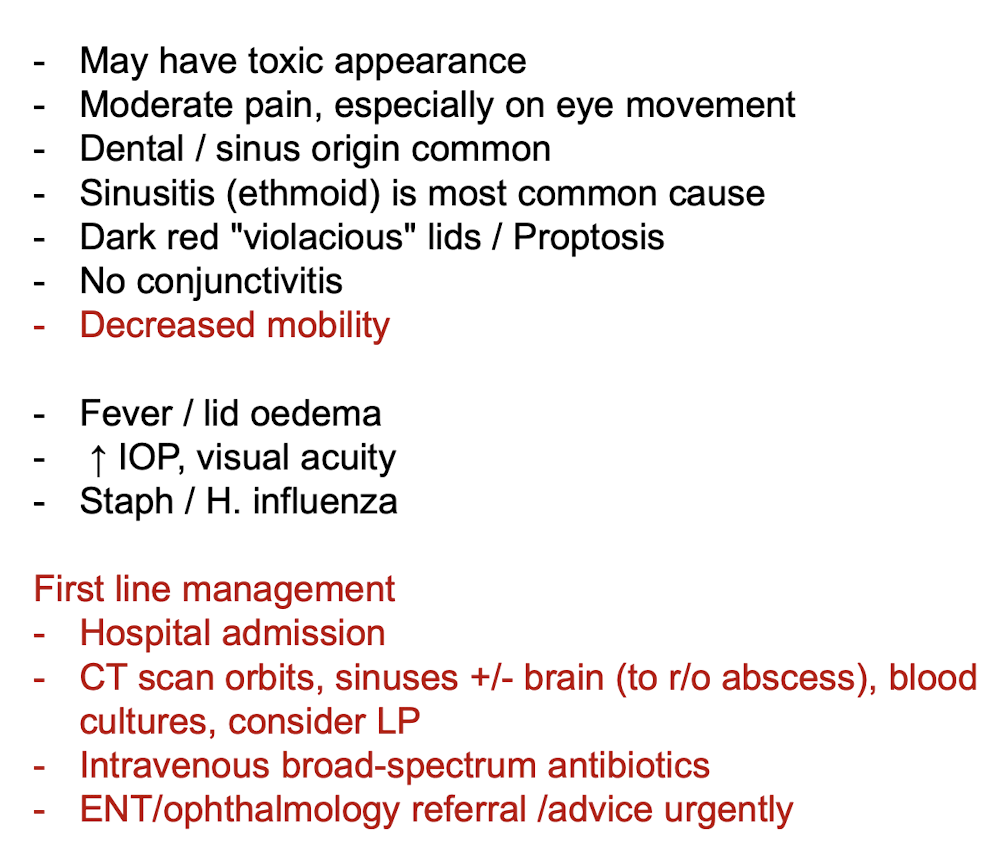
Periorbital vs orbital cellulitis
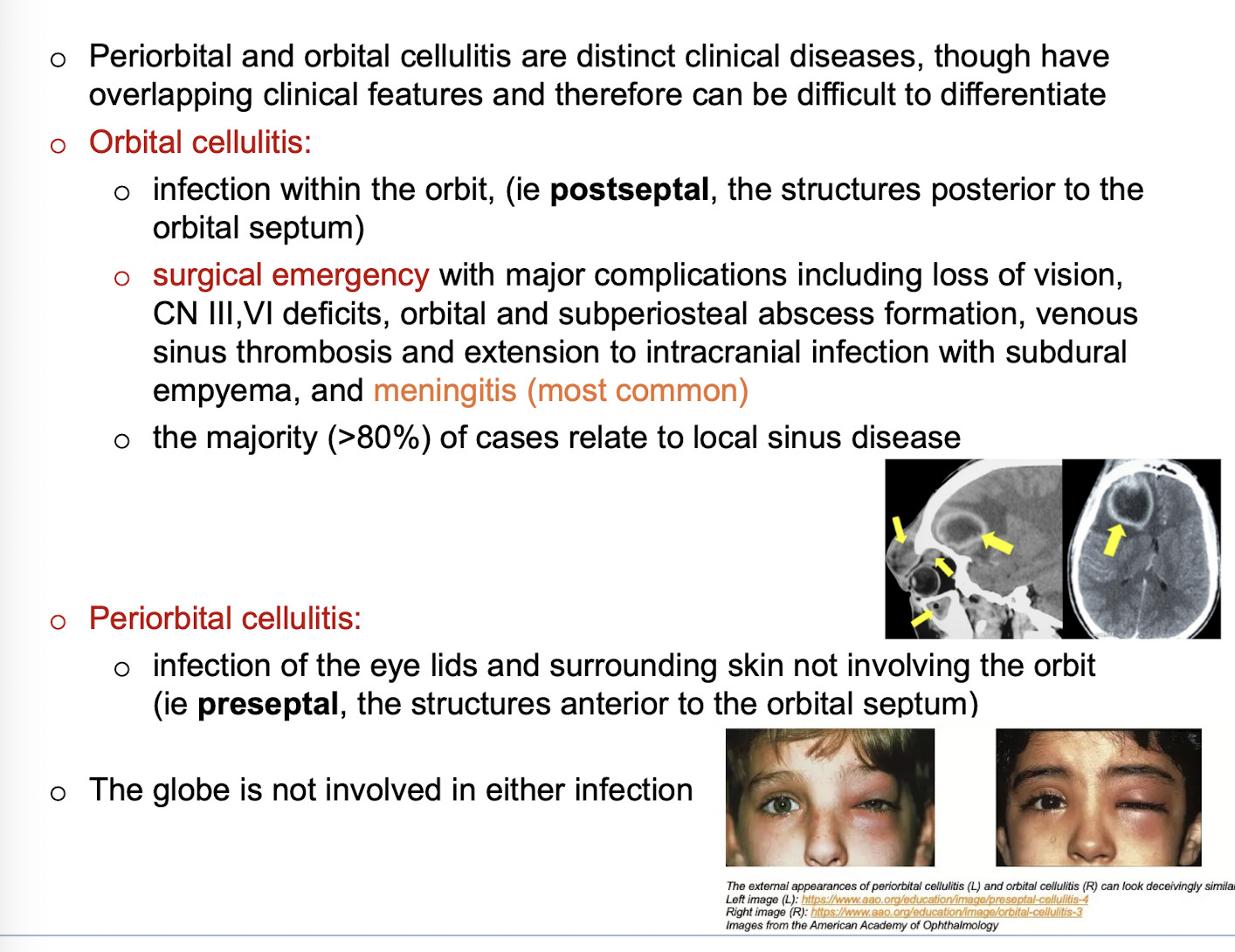
Red flags concerning for orbital cellulitis
painful or restricted eye movements
visual impairment: reduced acuity, relative afferent pupil defect, diplopia
proptosis
severe headache or other features of intracranial involvement
Cellulitis characteristics
Dermatitis vs eczema
terms are used interchangeably but … technically eczema is a type of dermatitis.
Dermatitis refers to any cause of skin inflammation affecting the epidermis
Eczema - oedema within the epidermis (called spongiosis)
Acute vs chronic dermatitis
Acute - red, wet, oozing, even blistering
Chronic - skin thickened, dry, scaly, and fissured (lichenification - secondary lesion)
Subacute - stage between acute and chronic so will show features of both
Seborrhoeic dermatitis
(endogenous)
red itchy patches (which become scaly or crusted)
caused by combination of endogenous factors and overgrowth of malassezia furfur yeast
dermatitis may be aggravated by a combination of endogenous factors - illness, stress, fatigue, change of season, and reduced general health (eg. especially infection with HIV)
Infantile seborrhoeic dermatitis
characteristic cradle cap ‘greasy’
erythematous but non-itchy rash, well defined and covered in greasy scale… (sebaceous glands release a greasy substance that makes old skin cells attach to scalp as they try to dry and fall off)
the rash may spread to affect armpit and groin folds (via flexures)
possibly due to overactive sebaceous glands in skin of newborn babies due to maternal hormones still in baby’s circulation
super-infection with staph and candida albicans is common resulting in weeping and crusting
treatment: for
mild/localised - use gentle emollient or repeated shampooing, remove scales with a soft toothbruhs or comb
extensive/resistent - treat with low-potency topical steroid or antifungal for 1-2 weeks…. topical steroid preferred if significant inflammation
Adult seborrheic dermatitis
usually appears at any age after puberty
exacerbated by emotional and physical stress
clinical features: erythema and fine, greasy scale on cheeks, nose and nasolabial folds
scale and itching of scalp and eyebrows
well defined but non scaly, erythema of axillae, groin, scrotum and perianal skin
management:
scalp:
anti-dandruff shampoos containing selenium sulphide, ketoconazole, miconazole or zinc pyrithione (which all control malassezia)
tar containing shampoos are also helpful and combination of a tar and antifungal shampoo gives better control than either alone
non scalp areas:
topical steroids first and consider adding topical antifungal agent for malassezia
weak tar creams such as LPC 2% cream may assist (you used this! for something else tho)
Atopic dermatitis (+aetiological factors* (5), clin features (5), distribution, treatment 9) + pityriasis alba
(endogenous)
most common form of dermatitis
atopic eczema also associated with asthma, allergic rhinitis (hayfever), food allergies
aetiological factors
family history
immune dysregulation - increased IgE due to Th2 immune dysregulation
abnormal epidermal barrier - deficiency of fillaggrin (an epidermal protein) which causes impaired skin barrier which holds water poorly and is more susceptible to irritants and allergens
susceptibility to infection - epidermis is deficient in peptides known as defensins
environmental irritants - bc of the impaired epidermal barrier eg. soap, sand, woollen, synthetic fabrics and dust
clin features
a patchy erythematous, poorly defined rash
xeroderma - dryness of skin
excoriation (de to scratching and itching)
lichenification (prurigo may develop)
in bacterial infections crusting and weeping
Distribution
infants
cheeks are often first place
may have widely distributed small patches of eczema
napkin area is frequently spared due to mositure retention of nappies
tends to be vesicular and weeping
in babies of non-caucasian descent, a micropapular variant is common (instead of vesicular) and temporary hypo/hyperpigmentation may occur
toddlers and pre-schoolers
as children begin to mvoe around, eczema becomes more localised and lichenified
flexor aspects of joints (wrists, elbows, ankles, and knees +maybe genitals)
some individuals have reverse presentation where it affects the extensors
some develop discoid pattern
adults
become quite localised involving hands, eyelids, nipples, genital area, lips or face
in severe: it may involve entire skin (erythroderma)
TREATMENT
explanation fo chronicity and overall good prognosis (requires long term management not just reactive care, also need to treat flareups)
modification of lifestyle to avoid exacerbating factors
use of moisturisers and bath additives (use of emollients and bath oils)
investigation and treatment of infection (MCS if flare ups, antibiotics), for recurrent or chronic, add a very dilute chlorine bleach to water
discussion, possible investigation and treatment of allergy (allergy testing)
use of topical anti-inflammatory agents (MAINSTAY- TOPICAL CORICOSTEROIDS)
understanding role of anti-histamines (minimal use as not much benefit)
use of wet dressings
understanding psychological issues
other options
Pityriasis alba
low-grade type of atopic dermatitis mainly seen in children
mild scattered areas of facial eczema complicated by depigmentation on face
several round or oval slightly scaly pink patches appear, leaving pale marks when redness faded
regresses spontaneously
more apparent in summer, especially in dark-skinned children
management: weak topical corticosteroid, emollient and soap avoidance
once dermatitis is controlled, sun exposure will return the pigment
Discoid dermatitis (two forms)
(endogenous)
affects middle age and elderly
OFTEN with a previous history of atopic dermatitis
pink, red, brown and well defined, dry cracked surface and can have blistered or crusty surface
TWO FORMS
exudative (wet) nummular dermatitis: oozy papules, blisters and plaques
dry nummular dermatitis: red scaly, very itchy, discrete, round or oval plaques with well defined edge
may be symmetrical
lichenification can occur rapidly due to intense scratching
affects any part of body particularly lower leg
treatment: similar to atopic dermatitis
moderately potent topical steroids are usually requried
lichenified lesions may require very potent topical steroids or intralesional steroids
wet wraps
antibiotics if bacterial infection
Stasis dermatitis (+complications (8) and management)
occurs on lower legs due to chronic venous hypertension
mainly in elderly women
look for venules, phlebactasia and brown haemosiderin deposition around ankles (early signs)
characteristic dryness, scale and brown hyperpigmentation (due to diapedesis of red blood cells from peripheral circulation into dermis, eczema and ulceration can subsequently develop
usually associated varicose veins, woody oedema (due to lipodermatosclerosis)
allergic contact dermatitis may coexist (eg. bandages or leggings for chronic venous hypertension may be an irritant/allergen)
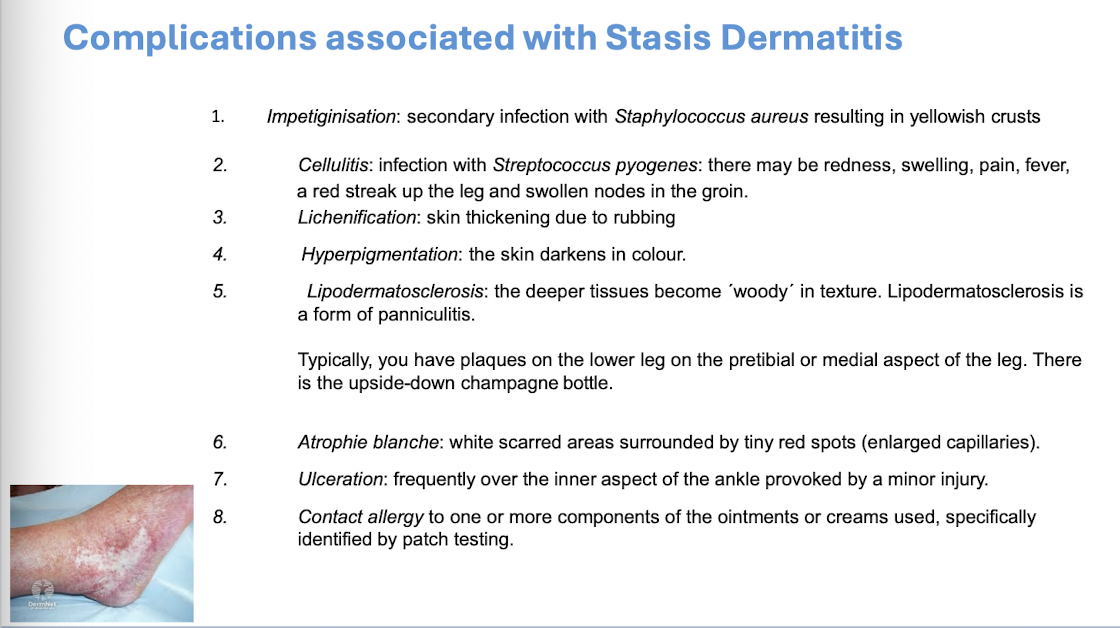
Management
dryness is managed by avoidance of soap, using a soap substitute and application of a greasy moisturiser at least twice a day
inflammation treated by moderate topical corticosteroid
acute attacks are settled by short bursts of potent topical corticosteroids, wet dressings and antibiotics if an infection (like discoid and atopic management)
In order to treat and prevent you need to treat the cause of the stasis dermatitis by attention to the underlying venous insufficiency. This involves compression bandaging or stockings and elevation of the foot of the bed at night
Pompholyx (dyshidrotic) dermatitis
(endogenous)
a vesicular or bullous dermatitis
affects palms, sides of fingers and soles of feet
cause: unknown, may be precipitated by stress, sweating and overheating
acute stage: vesicles deep in skin of palms, fingers, instep or toes, the blisters are often intensely itchy or have a burning feeling, the condition may be mild with only a little peeling or very severe with large blisters and cracks
Management
Management is the similar as for other dermatitis.
Potent topical corticosteroids should be used initially with wet dressings and antibiotics if secondary bacterial infection.
Rest is important and because of the location on the hands this can mean time off work for adults.
After an acute attack, the skin is vulnerable, and patients need to protect their hands from irritating substances including soap for three months.
Very severe attacks of bullous Pompholyx may require a 2-to-3-week course of oral prednisone.
Asteatotic Dermatitis
(miscellaneous)
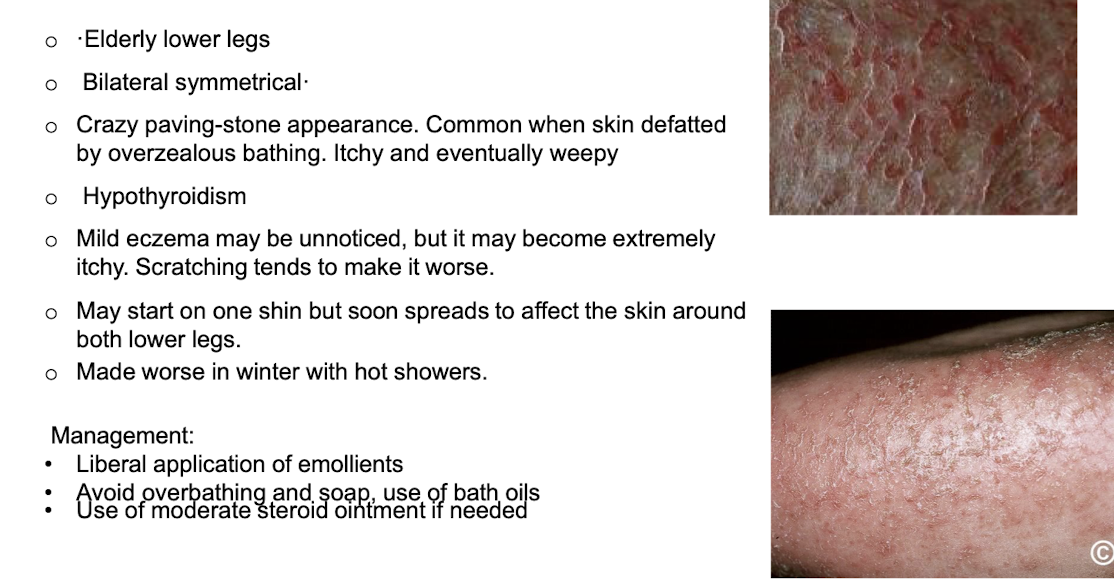
hypothyroidism can contribute to condition
Irritant dermatitis
(exogenous)
Cause
Strong irritant elicit an acute reaction after brief contact
Sometimes a weak irritant over many years
Usually, hands and forearms
E.g. water, detergents, chemicals, oils o Previous Atopic dermatitis increases the risk
Often on backs of hands, between fingers, Napkin area
Dry "chapped". Later thickened and fissured
more likely in Cleaners, catering, hairdressing, engineering, health workers
Investigations - patch testing with irritants is not helpful but with common allergens may be
treatment
avoidance of irritant
protective gloves and clothing
barrier cremes more for prevention
avoid harsh solvents when cleaning hands
emollients
corticosteroids
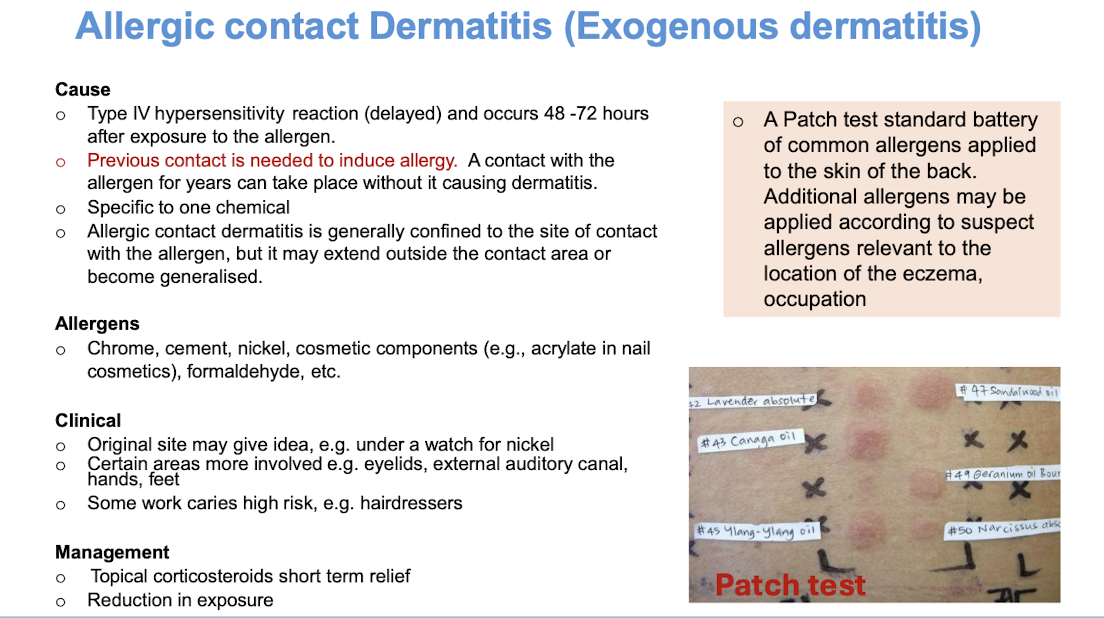
Allergic contact dermatitis
(exogenous)
Functions of the skin
thermoregulation (evaporation of sweat, in hot or cold weather, cutaneous blood vessels dilate or constrict to give off/conserve heat, arrector pili contraction produces heat (goosebumps))
protective function and repair
sensation
immunological response
metabolic (vit d synthesis)
psychological and communication (aesthetic appearance, apocrine gland secretion - odour)
Important notes on epidermis
stratum corneum - anuclear
(stratum lucidum)
stratum granulosum
stratum spinosum
stratum basale - melanocytes, keratocytes (where it develops but migrates up) and merkle cells
+basement membrane zone and then dermis
epidermis is avascular
cells of epidermis
keratinocytes: develops from basal layer and then migrates upwards to the stratum corneum where it is shed
langerhan cells - APCs found in epidermis
melanocytes produce pigment, protect cells of epidermis and dermis from sun damage
Merkles cells - (sensory mechanoreceptors) transducers associated with fine touch via fine unmyelinated nerve fibres — only present in thick skin
epidermis has an undulating surface with cross-crossing ridges and valleys, with invaginations due to follicles and sweat duct ostia (what we see as fingerprints)
Important notes on dermis (major fibres, major cells)
fibrous connective tissue in skin
major fibres
collagen: provide the skin with strength and toughness. Collagen bundles are small in the papillary dermis and form thicker bundles in the reticular dermis (deeper).
Elastin: provides the properties of elasticity and pliability to the skin.
dermis also contains nerves, blood vessels, lymphatics, epidermal adnexal structures, arrector pili muscle and cells.
major cells
fibroblasts
macrophages
mast cells
t and b lymphocytes
What are the physiological changes of the skin in aging
thinning of epidermis
flattening of dermal-epidermal junction
hyperpigmentation
loss of melanocytes
degradation of collagen and elastin
Hypodermis
Adipocytes organised into lobules (between these lobules are septa) septa contain nerves, larger blood vessels, fibrous tissue and fibroblasts — cna form cellulite
function
cold insulation
site of fat and energy storage
epidermal crosstalk
immune surveillance
Epidermal appendages - hair types, hair cycle
on all body except glabrous skin (lips, glans penis, labia minora, palms and soles)
provides protection, sensation and social communication
three types
lanugo - fine long hair of fetus that is shed 1 month prior to birth
vellus - fine short hair found all over body
terminal - thick hair on scalp, beard, axilla and genital area
hirsutism - vellus to terminal
male pattern alopecia - terminal to vellus
hair growth cycle
anagen - long growth phase
catagen - where active hair growth stops and the follicle begins to regress
telogen - ‘resting’ follicle shrinks and atrophies, and new hair follicle begins to grow
exogen - hair shed
Epidermal appendages - nails
specialised plates of hard keratin that develop from epidermis overlying small bones at ends of fingers and toes
stratching
grooming
picking up ifne objects
psycho-sexual communication
weapon
paronychium - skin around nail
lunula - white area of base of nail
Types of glands - epidermal appendages
sebaceous glands
associated with hair follicles
secreted onto skin through pilosebaceous canal-discharge into hair follicle ducts
antibacterial and antifungal action
eccrine sweat glands
all over body
merocrine
opening directly into skin
cholinergic innervation
watery (hypotonic) secretion
sweating/thermoregulation
onset of activity: birth
apocrine sweat glands
axilla, groin, mammary area, umbilicus
apocrine
opens into hair follicle (like sebaceous glands)
adrenergic innervation
viscous secretion
body odor
onset of activity: puberty (androgen dependent)
Macule
flat area of altered colour ≤ 1cm
Patch
flat area of altered colour > 1cm
Papule
elevated, solid, palpable lesion that is ≤ 1cm in diameter.
may be
acuminate (pointed)
dome shaped (ronded)
filiform (thread like)
flat-topped
oval or round
pedunculated
sessile
umbilicated
verrucous
Nodule
elevated, solid, palpable lesion > 1cm
Cyst
papule or nodule that contains fluid or semi-fluid material so is fluctuant
Plaque
circumscribed, palpable lesion > 1cm, most plaques are elevated, with a flat top
Vesicle
raised clear fluid-filled lesion ≤ 0.5cm
Bullae
raised clear fluid-filled lesion > 1cm
Pustule
pus-containing lesion < 0.5cm
Abscess
localised accumulation of pus in dermis or subcutaneous tissue (u can’t rlly see pus that much compared to a pustule)
Wheal
transient-raised lesion due to dermal oedema —> indicates urticaria
Comedone
papule due to blocked sebaceous follicle (occurs in acne) —— open (blackhead) or closed (whitehead)
What is diascopy
test where a clear glass slide is pressed against a skin lesion to assess if it blanches
helps differentiate between telangiectasia and petechiae
Petechiae is caused by blood leaking out from capillaries into surrounding tissue, whereas telangiectasia is the blood is still in the vessel but the capillaries are just dilated which means the blood can be pushed aside in the vessel —> blanching
Auspitz sign
peeling off surface scale to reveal areas of pinpoint bleeding (typical in psoriasis)
Woods light
fluorescence in visible range when applied to certain skin conditions
dermographism
where skin is stroked and a wheal is formed (indicative of tendency to urticaria)
nikolski’s sign
shearing stress of skin causes separation of skin resulting in traumatic bulla
koebner phenomenon
localisation of a non-infective skin disorder to area of trauma eg. psoriasis developing at site of a scar
dariers sign
rubbing of area of mastocytosis causes an intense urticarial reaction
pathergy
penetrating injury to skin causes area of pustulation 72 hours afterwards
bullous diseases types
subcorneal —> impetigo (children)
intraepidermal —> pemphigus vulgaris (middle aged), herpes zoster (older adults)
subepidermal —> bullous pemphigoid (elderly), dermatitis herpetitiformis (adults)
subcorneal - thin roof, not usually intact
intraepidermal - thin roof, rupture easily and leaves oozy denuded surface
subepidermal - thick roof so tending to be tense and intact - may contain blood
Risk factors for bacterial infections
skin barrier disruption (trauma, insect bites)
moist, macerated environments (common in warm, occluded areas such as the axilla and groin)
colonisation with skin flora pathogens
impaired host defenses
What causes impaired host defenses
Metabolic - diabetes mellitus
Vascular insufficiency - Peripheral arterial disease, chronic venous insufficiency (varicose veins)
Immunodeficiency - HIV/AIDS, malignancy, immunosuppressive therapy eg. glucocorticoids
Impetigo
staph
~ most common in young children (but occurs at any age)
~ less commonly caused by strep pyogenes
~ spreads in warm moist environments with close physical contact and poor hygiene
Two presentations
1 Bullous (SUBCORNEAL BULLAE)
~ thin-roofed bullae with clear yellow fluid which rupture quickly leaving exudative and yellow brown crust erosions
~ more likely to have systemic symptoms of malaise, fever, and lymphadenopathy
[staph attacks intracellular adhesion molecules in stratum granulosum, causing bullae formation – explored later]

2 crusted or non-bullous (most common)
~ begins with a single erythematous macule which evolves into a pustule or vesicle
~ pustule or vesicle ruptures releasing serous contents which dries leaving honey-coloured crust
~ has satellite lesions due to autoinoculation
what areas of skin are prone to impetigo? broken by insect bites. superficial injury, excoriated eczema
complications?
Can trigger post-strep glomerulonephritis and rheumatic heart disease
Can grumble on for several weeks and lead to deeper ulcerated and scarring infection called Ecthyma
general measures - TREATMENT
cover affected areas with watertight dressing to prevent spread
hand hygiene
school exclusion (until at least 24 hours after starting appropriate antibiotic treatment)
TOPICAL: for localised non-bullous impetigo, antiseptic recommended for 5-7 days… if ineffective or not appropriate (if around eyes) topical antibiotics can be considered (fusidic acid 1st, mupirocin - reserved for MRSA infection)
SYSTEMIC: fluclox (1st)
alternatives may include trimethoprim and sulfamethoxazole or erythromycin (for MRSA infection or if penicillin allergy)

Ecthyma
Hard crusted sores beneath which ulcers form
~ begins as a vesicle or pustule on inflamed skin
~ removal of crust reveals red, swollen, indurated ulcer oozing with pus

Community-acquired MRSA
mostly occurs
~ in overcrowded places, due to frequent contact of skin and sharing things
~ in people with draining cut or sore or that are carriers of MRSA
Management
~ swab for MCS
PCR
Surgical drainage if required
Clindamycin or trimethoprim/sufamethoxazole
For severe infections vancomycin is indicated
Clinical features of hospital acquired MRSA
~ present as skin infections (abscesses, furuncles and carbuncles, impetigo and cellultiis) or as wound infections (at trauma and surgical sites)
Whereas
Clinical features of community-acquired MRSA mainly presents as bacterial folliculitis, boils, impetigo

Folliculitis
Inflamed hair follicles
Presentation
~ tender red papule or pustule centred on a hair follicle
~ more common in hot weater
~ often occurs in macerated areas
~ look at centre of the inflammatory papule for protruding hair shaft
Shaving and waxing common triggers
Investigation
MCS
Skin scraping for fungus
Hair pull test (if fungal scalp involvement suspected)
Treatment
• Depending on the organism or cause.
• Physical factors such as occlusive clothing, grease or massage oils or in a child case nappies need to be managed.

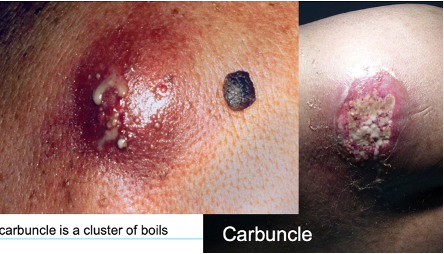
Furuncles and carbuncles
deep form of bacterial folliculitis
~ furuncles (boils) present as single or multiple tender, red, firm or fluctuant nodules or walled-off abscesses which eventually point and discharge pus from a central core
~ carbuncles are when multiple furuncles coalesce and extend to the subcutis
~ carbuncles often have systemic signs (malaise, chills, fever)
Treatment
~ apply topical antiseptic like povidone iodine or chlorhexidine cream
Then cover with gauze
~ oral antibiotics: fluclox, cephalexin
~ incision and drainage

Acute vs chronic paronychia
Acute paronychia
~ common in nail biters and those with chronically wet hands
Presentation
~ nail fold becomes painful, red and swollen, sometimes yellow pus under cuticle
Treatment
~ drainage with sterile needle, application of a topical antibiotic, sometimes oral
Acute herpetic paronychia
~ caused by HSV
Chronic paronychia
~ chronic irritant dermatitis and C.albicans superinfection
~ may start on one and spreads to several others
~ affected nail fold is swollen and lifted off nail plate
~ becomes distorted and ridged as it grows. May become yellow or green and brittle
~ common in people with chronically wet hands, such as bar tenders and housewives

SSSS
~ characterised by erythematous painful blistering
~ skin looks like a burn or ‘scald’
~usually from a local infection eg. impetigo
Treatment: systemic antibiotics
Mechanism of Staph to cause SSSS
~ release of epidermolytic toxins A and B from staph
~ toxins target desmoglein-1 (a cell adhesion protein) in the stratum granulosum
~ leads to intraepidermal splitting
~ results in blistering, skin peeling and positive nikolsky sign
What is Nikolsky’s sign?
shearing stress of skin causes separation of skin, results in traumatic bulla

Toxic shock syndrome
~ caused by release of exotoxins from staph and can also be caused by s.pyogenes
~ presents with sudden high fever, widespread erythematous rash, and multi-organ involvement
~ may lead to circulatory collapse
~ classically linked to tampon use but can arise from skin or wound infections
Cellulitis vs erysipelas
Cellulitis
~ acute diffuse spreading skin infection (what ur brother had)
Erysipelas
~ skin infection involving upper dermis with clearly delineated borders, eg. butterfly rash
Both present with localised redness, pain, swelling and +/- systemic symptoms (fever)
~ usually caused by s.pyogenes (GAS)
~ if around a wound, consider staph
~ periorbital cellulitis can occur in children (like ur bro) usually S.pyogenes. his was HSV, Hib is now rare due to vaccination
Cellulitis presentation
~ more raised n swollen, less marginated, favours lower legs in adults, and for children, limbs and periorbital region
Predisposition for cellulitis
On legs (lymphoedema, tinea of feet, chronic dermatitis, poor lower leg circulation arterial and venous, wounds)
On face: Herpes simplex infection, dental caries, chronic sinus infection, more common in diabetics, immunosuppression)
Treatment:
rest and elevation of area
analgesia
oral or IV antibiotics eg. cephalexin, fluclox, penicillin-dependent on sensitivities
Presentation for erysipelas
~ may see lymphatic streaking
~ blisters may develop on red plaques
~ most commonly affects lower limbs
Treatment:
Oral antibiotics or IV if severe, usually penicillin

Necrotising fasciitis
~ infection of soft tissue and fascia
~ presents as a dusky cellulitis which progresses to extensive necrosis
~ bacteria multiplies and releases toxins and enzymes that results in thrombosis in blood vessels destruction of soft tissues and fascia
~ due to mixture of staph, strep and anaerobes?
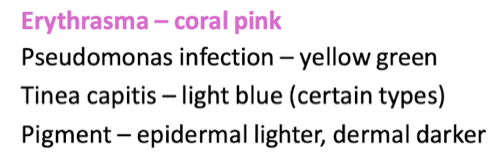
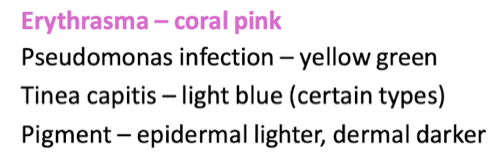
Erythrasma
~ in skin folds, axilla or groin or between the toes
~ macular wrinkled, slightly scaly, pink, brown or macerated
~ WOODS LIGHT: CORAL PINK
Treatment:
Fusidic acid cream, whitfield ointment, clindamycin solution

Trichomycosis Axillaris
Infection of underarm hair
~ characterised by yellow, black or red granular nodules or concretions that stick to hair shaft
~ caused by overgrowth of corynebacterium
~ topical antibiotics and shaving

Pitted keratolysis
~ combination of unusually sweaty feet and occlusive shoes encourages growth of microorganisms that digest keratin
~ results in honeycomb like pits in webs and toe pulps, forefott and heel
~ often with offensive odour
Treatment
~ keep feet dry
~ topical clindamycin, erythromycin, fuscidic acid
~ oral macrolides

Herpes Simplex Virus infection (types, recurrence, complications, diagnosis, treatment
clinical sign: grouped vesicles on an erythematous base
spread via resp droplets or direct contact with an infected lesion or bodily fluids
HSV enters host through abraded skin or intact mucous membranes
targets epithelial cells initially but retrograde transport through adjacent neural tissue to sensory ganglia leads to lifelong latent infection
two types: HSV1 and HSV2
HSV1 is more associated with oral n facial infections (cold sores)
often initial episode has no symptoms but can be severe if have systemic symptoms
vesicles turn quickly into ulcers (red based)
HSV2 more associated with anogenital herpes
presents after onset of sexual activity
painful vesicles, ulcers, redness and swelling last for 2-3 weeks, often accompanied by fever and tender inguinal lymphadenopathy
minor injury helps inoculate HSV into skin
How can HSV recur
can either be local or systemic stimuli
UV light
fever
trauma
mensturation
sexual intercourse
stress
immunodeficiency
recurrence is often less severe
Complications
eye infection: dendritic ulcer
throat infection
eczema herpeticum (in patients with history of atopic dermatitis or darier disease)
erythema multiforme (target lesions, symmetrical plaques on hands, forearms, feet and lower legs)
cranial/facial nerve infections by HSV (bells palsy)
widespread infection —> disseminated infection (eg. can occur in a HIV patient)
Diagnosis
clinical diagnosis, culture and PCR
treatment
mild uncomplicated eruptions of herpes simplex require no treatment
sunscreen and other sun protection measures are crucial as sun exposure often triggers facial herpes simplex
for mild oral lesions: topical acyclovir
severe infection may require treatment with an oral antiviral agent
acyclovir
valaciclovir
famciclovir
theyre suppressive not curative
How can HSV recur
can either be local or systemic stimuli
UV light
fever
trauma
mensturation
sexual intercourse
stress
immunodeficiency
recurrence is often less severe
Diagnosis for HSV
Clinical diagnosis, culture, PCR
Treatment for HSV
mild uncomplicated eruptions of herpes simplex require no treatment
sunscreen and other sun protection measures are crucial as sun exposure often triggers facial herpes simplex
for mild oral lesions: topical acyclovir
severe infection may require treatment with an oral antiviral agent
acyclovir
valaciclovir
famciclovir
theyre suppressive not curative
Varicella (chickenpox) (rash, lesion characteristics, diagnosis, complications, treatment, vax?)
caused by varicella-zoster virus
remains in dorsal ganglia of the spinal cord —> can reappear later as shingles or herpes zoster infection
spread via inhalation of resp droplets or direct contact with the vesicles’ fluid.
RASH: begins on trunk and spreads to face and extremities (the opposite of rubella and measles)
LESIONS are: 2-4mm red papules —> become vesicular and umbilicated —> breaks and crusts over leaving an eroded red base
diagnosis
made clinically in typical cases
can be confirmed by PCR on a viral swab from base of vesicle
complications
secondary bacterial infection from scratching
dehydration from vomiting and diarrhoea
systemic:
~ viral pneumonia
~ encephalitis
~ thrombocytopenia
~ hepatitis
~ scarring
pregnancy complications
• If a non-immune pregnant woman is infected:
◦ Maternal varicella pneumonia (serious).
◦ Congenital varicella syndrome (limb hypoplasia, eye/brain defects, skin scarring in fetus).
◦ Severe neonatal varicella if infection occurs just before or after delivery.
treatment
symptomatic eg. antipruritis lotions, antihistamines?
antiviral therapy is indicated for patients with complications or who are immunocompromised
antiviral agents include acyclovir, valacyclovir, famciclovir (same as HSV)
varicella-zoster immune globulin (VZIG) is indicated for immunocompromised and neonates exposed to varicella (must be given within 96 hours of exposure)
vaccination
immunisation schedule in australia for infants aged 18 months and children 10-13 years who have not been previously immunised or previously had varicella infection
zoster vax has also been introduced for patients over 60 and who are most at risk of this condition
Herpes Zoster (shingles) +diagnosis, clinical features, treatment
reactivation of varicella virus localised to one or two dermatomes (what ur auntie had)
virus remains in selected ?anterior? horn cells of spinal cord before it is reactivated and grows down the nerves to the skin
predisposing factors apart from age are immunocompromised individuals eg. HIV
Diagnosis
clinical
viral PCR for herpes zoster virus
clinical features
unitlateral
dermatome (one or several)
first sign of shingles is usually pain, which may be severe, in areas of one or more sensory nerves. the patient may appear quite unwell with fever and headache, lymph nodes draining the affected area are often enlarged and tender
pain —> closely grouped lesions start as erythematous papules or plaques —> turn vesicular and become crusted —>over a course of 2-3 weeks clear vesicles appear in the affected dermatome
complications
post-herpetic neuralgia (can last for years)
corneal damage if CN V involved
encephalitis
myelitis causing contralateral hemiplegia
*Hutchinson’s sign - vesicle on side or tip of nose in ophthalmic zoster (WHAT UR AUNTIE HAD)
treatment
antiviral medication within 72 hours
analgesia
vaccination for patients over 60
Viral exanthem
rash due to a virus
can be divided into
classic eg. measles rubella
non-specific (in children usually enteroviridae (coxsackie or echovirus))
whereas there are specific presentations with varicella, measles, rubella, hand, foot and mouth disease, parvovirus (slapped cheek), roseola, pityriasis rosea
What are the two non-specific presentations of viral exanthem in children
generalised, bilaterally symmetrical maculopapular rashes, often with confluence on the face
peripheral papular eruptions mainly on arms and leg
Measles (clinical presentation, diagnosis, complications)
spread via resp droplets
clin presentation
initially URTI symptoms of fever, malaise, cough and conjunctivitis
characteristic KOPLIK spots (pinhead size white spots on buccal mucosa) in prodromal stage —> a widespread morbilliform (macular) rash appears HEAD then spreads to TRUNK and limbs
non-pruritis rash
macules may coalesce, esp on face
when it fades —> purplish hue —> brown/coppery coloured lesions with fine scales
diagnosis
clinical n confirm with serology
complications (Did this in GH)
diarrhoea
otitis media
pneumonia
encephalitis
vax at 12 months of age
*notifiable disease
Rubella (german measles) = presentation, diagnosis, complications
mild pink maculopapular rash and lymphadenopathy
begins on FACE and spread to TRUNK and limbs (less widespread than measles)
mild fever, sore throat and rhinitis
adults have arthralgia and arthritis
infected by direct contact with nasal or throat secretions of infected individuals, infected personcontagious 7 days prior to rash, until 7 days after
diagnosis
clin and confirm with serology (same as measles)
complications
first trimester of pregnancy has 50% risk of congenital rubella syndrome (sensorineural deafness, CNS dysfunction, cataracts, cardiac defects)
*notifiable disease (like measles)
rubella vax is on national schedule
Hand, foot and mouth disease (clin presentation + DDx + diagnosis)
most often affecting young children under 5
due to coxsackie virus A16
children present with small red macules that rapidly evolve into cloud vesicles and surrounded by erythematous areola in the oral cavity
there may be lesions distributed over plams and soles, and dorsal fingers or toes
20% of cases have submandibular / cervical lymphadenopathy
DDx for hand, foot and mouth disease
enterovirus 71 infection
herpetic stomatitis
aphthous ulceration
herpangina
erythema multiforme
scabies
(see the ppt for explanation on ddx)
diagnosis
clin and serology (same as measles and german measles (rubella))
DDx for hand, foot and mouth disease
enterovirus 71 infection
herpetic stomatitis
aphthous ulceration
herpangina
erythema multiforme
scabies
(see the ppt for explanation on ddx)
Parvovirus infection - slapped cheek - fifth disease (clin features, treatment, complications, DDx)
parvovirus B19
transmitted via resp droplets
clin features
firm red burning-hot cheeks
rash follows with lace or network pattern on limbs and then trunk

treatment - supportive
complications
in pregnant women may cause foetal anemia and cardiac failure and fetal loss
arthralgia in adults
DDx
enterovirus exanthemata
rubella
scarlet fever
Roseola (clin presentation and treatment?)
transmitted via resp droplets
HHV-6B, HHV-7
clinical presentation
high fever and upper resp symptoms
rash appears as fever subsides (days 3-5)
rash: small pink or red maculopapular rash that blanch when touched, may be surrounded by lighter halo of pale skin
begins on TRUNK and may spread to neck, face, arms and legs (sort of like varicella)
non-itchy, painless and does not blister
no treatment required
Pityriasis Rosea (presentation)
rash of unknown cause (possible reactivation of Herpes 7 or 8 virus)
most commonly affects teenagers or young adults
PRESENTATION
single inner circlet of scaling, oval red or pink plaque (the HERALD patch) appears before general rash
few days later, smaller plaques appear on chest n back, uncommon on face
these lesions follow the relaxed skin tension lines (LANGER’S LINES) on both sides of upper trunk (so it looks like a fir tree?)
can be very itchy and sometimes not at all. on darker skin they appear more pigmented or white due to scales

Monkey pox (MPox) - presentation, transmission, prevention, diagnosis, treatment and vax
viral zoonotic disease
presentation
general symptoms (fever, chills, headache, muscle aches, back aches, fatigue, swollen lymph nodes)
USUAL symptoms: rashes, pimple-like lesions or sores, particularly in areas like genitals, anus or buttocks…. ulcers, lesions or sores in mouth… rectal pain (with or without rash)
all lesions go crusted and fall off to reveal a fresh layer of skin
most people with MPox get better within a few weeks without needing any specific treatment
Mpox spread via
direct contact w rashes, blisters or sores, or contact w bodily fluids also
TOUCHING contaminated objects
who is at risk: men who have sex w men
prevention
isolation
hand hygiene
keeping lesions covered and wear a face mask
diagnosis
by lab testing
treatment
supportive care —> pain relief
antivirals for more severe disease
vaccine for at risk population!

Molluscum contagiosum - presentation, DDx, control spread, treatment
poxvirus
two peaks: in children (3-9) and young adults
spread from direct contact
the papules form a row —> known as pseudokoebnerised molluscum
presents as clusters of small pearly papules with a central umbilication, core can be expressed by firm pressure, occurs in warm moist areas like armpits, groin or behind knees in kids, in adults in groin
DDx
verrucae (but have no central umbilication)
herpes (rapid onset and vesicles)
treatment
in children leave alone
cryotherapy
can use tape occlusion
immune techniques such as imiquimod creme, topical retinoids
Viral warts - transmission, presentation, DDx, treatment
common benign growths
usually on hands, feet and extensor surfaces
HPV
transmission
direct contact w infected skin or contaminated surfaces (breaks in skin increase transmission)
presentation
comon warts (verruca vulgaris)
plane warts
plantar warts
digitate/filiform warts
characterised by papillomatous surace, loss of skin lines and papillary capillaries
DDx
Bowen’s disease
seborrheic keratosis
corns and callous
penile pearly papules and equivalent papillomatosis of vulva
treatment
spontaneous resolution usually 2 years
topical salicylic acid, podophyllin or cryotherapy
imiquimod topical treatment
specialist referral if conservative fail
HV vax
reason we see viral warts as doctors
cosmetic
teasing from school mates
exclusion from sport
increasing number of warts
pain in weight bearing
distortion of structure
concern of diagnosis
Scabies * presentation, diagnosis, complications, treatment
scarcoptes sscabiei hominus
transmitted by body-to-body contact
burrow through strateum corneum, produce 2-3 eggs a day which mature in 2-3 weeks
presentation
variable due to allergic reaction which is dependent on individual
generalised eruption and itchiness is thought to be caused by sensitisation to their products eg. faeces and eggs
pruritic excoriated nonspecific rash on trunk with scaly burrows on fingers and wrists
papular or nodular lesions are often seen on genitals and nipples in adults and major flexor surfaces of children
in infancy, rash on face
diagnosis
confirm with scrapping from burror and examine under microscope
dermoscopy sometimes helps
pracical method is positive response to anti-scabicide
complications
secondary bacterial infection, rarely glomerulonepritis or RHD
crusted scabies —> more on this
treatment
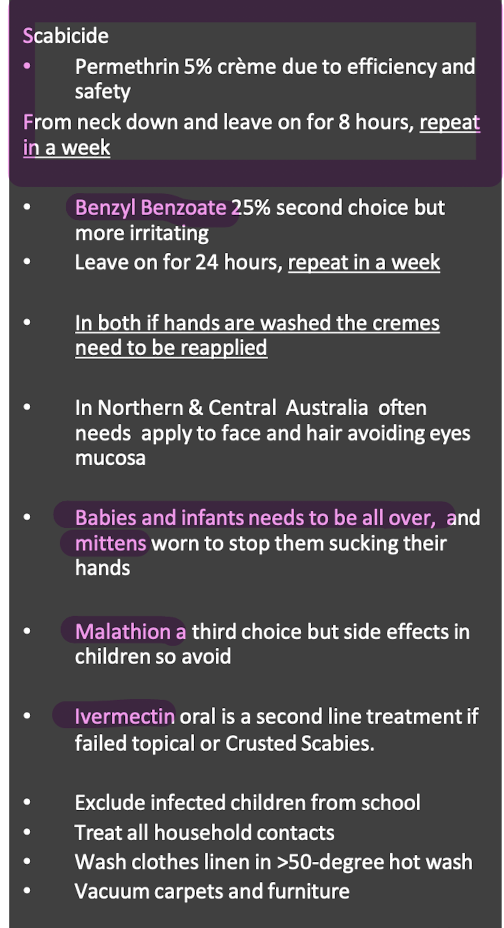
What are crusted scabies
severe variant of scabies
often seen in immunosuppressed
numerous more mites
widespread, scaly and hyperkeratotic rash
Head lice (transmission, presentation, complication, diagnosis, treatment, prevention)
head-to head contact
presentation
itching
may see excoriations or local lymphadenopathy
complication
secondary bacterial infection
Insect bites (presentation, treatment)
bites present as persistent itchy, oedematous papules
bullous reactions are common on legs of children
treatment
preventative measures like with insect sprays
treat fleas if present
treat infection if present
calamine lotion
local potent topical steroids
wet dressings for severe cases
Body and public lice
so yeah
Give me 4 resp causes of nail clubbing
TB
lung cancer
interstitial lung disease
sarcoidosis
Give 4 cardio causes of nail clubbing
CHD
tetralogy of fallot
subacute bacterial endocarditis
AA
Characteristics of nail clubbing
loss of small diamond window when index fingers are brought together
thickening of fingers
softening of nail beds
increased nail convexity
4 GI causes of nail clubbing
Crohns and UC
hepatocellular
Celiac disease
Liver cirrhosis
Treatment of nail clubbing
Treat underlying disease
Alopecia areata
Discrete annular areas of hair loss anywhere on body
sudden onset of hair loss, increasing area will have a smooth surface, completely devoid of hair or with scattered ‘exclamation mark’ hairs
Trichotillomania (+ddx)
condition where patients compulsively pull out their hair
can be a sign of stress relief habit, impulse control disorder, depression
DDx
alopecia areata
tinea capitis
NORMAL HAIR GROWTH IN THE BALDING AREAS
Telogen effluvium
when anagen stops prematurely and hair then enters telogen phase. anagen then recommences and telogen hairs are released from follicles after the shock
THIS OcCURS DUE TO A SHOCK OF THE SYSTEM
like acute telogen effluvium occurs folllowing childbirth or stopping OCP, any acute illness or major surgery and severe dieting
chronic may be primary and idiopathic or secondary to hypo/hyperthyroidism, malnutrition, cancer, TB, or iron deficiency anemia
CONFIRM by examining lost hair which is mostly in telogen stage (white bulb or club-shaped tip)
Anagen effluvium
drugs, toxins or inflammation cause interruption of active or anagen hair growth
Hypertrichosis vs hirsutism
widespread overgrowth of non–androgen-dependent hair, occasionally
seen with drugs such as cyclosporin and phenytoin.
• In hypertrichosis, areas like the forehead and forearms have increased hair growth— rather than the lower face and midline of the trunk that are preferentially affected by androgens