neurophysiology 4 and 5
Spinal Reflex
A spinal reflex is an automatic, involuntary response mediated by the spinal cord without direct involvement of the brain. This mechanism enables rapid responses to stimuli, bypassing cortical processing for quicker reaction times. It involves:
Sensory Neurons: These neurons carry afferent signals from sensory receptors to the spinal cord, initiating the reflex.
Interneurons: Located within the spinal cord, these neurons process sensory information and facilitate the appropriate motor response by connecting sensory and motor neurons. (reflex pathway)
Motor Neurons: Activated by interneurons, these neurons transmit efferent signals from the spinal cord to muscles or glands, causing a response.
This reflex arc includes:
Sensory Input: The process begins with the detection of a stimulus by sensory receptors.
Integration in the Spinal Cord: The sensory input is then processed by interneurons within the spinal cord to determine the appropriate response. This processing occurs without immediate involvement from the brain.
Cranial Reflex
A reflex integrated within the brainstem, rather than the spinal cord.
These reflexes control many of the body's involuntary functions such as heart rate, respiration, and digestion. Cranial reflexes utilize cranial nerves to relay sensory input and motor output.
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
Spinal Reflex
A spinal reflex is an automatic, involuntary response mediated by the spinal cord without direct involvement of the brain. This mechanism enables rapid responses to stimuli, bypassing cortical processing for quicker reaction times. It involves:
Sensory Neurons: These neurons carry afferent signals from sensory receptors to the spinal cord, initiating the reflex.
Interneurons: Located within the spinal cord, these neurons process sensory information and facilitate the appropriate motor response by connecting sensory and motor neurons. (reflex pathway)
Motor Neurons: Activated by interneurons, these neurons transmit efferent signals from the spinal cord to muscles or glands, causing a response.
This reflex arc includes:
Sensory Input: The process begins with the detection of a stimulus by sensory receptors.
Integration in the Spinal Cord: The sensory input is then processed by interneurons within the spinal cord to determine the appropriate response. This processing occurs without immediate involvement from the brain.
Cranial Reflex
A reflex integrated within the brainstem, rather than the spinal cord.
These reflexes control many of the body's involuntary functions such as heart rate, respiration, and digestion. Cranial reflexes utilize cranial nerves to relay sensory input and motor output.
Somatic Reflex
Reflexes that involve the contraction of skeletal muscle, which are typically consciously perceived.
These reflexes are crucial for actions like quickly removing your hand from a hot surface or maintaining balance.
Example: patellar reflex and the withdrawal reflex.
Autonomic Reflex
Reflexes that involve the activation of smooth muscle, cardiac muscle, or glands, typically without conscious awareness.
These reflexes control involuntary bodily functions such as blood pressure, digestion, and sweating. Because many of these reflexes occur without conscious awareness, issues may be present without even realizing it.
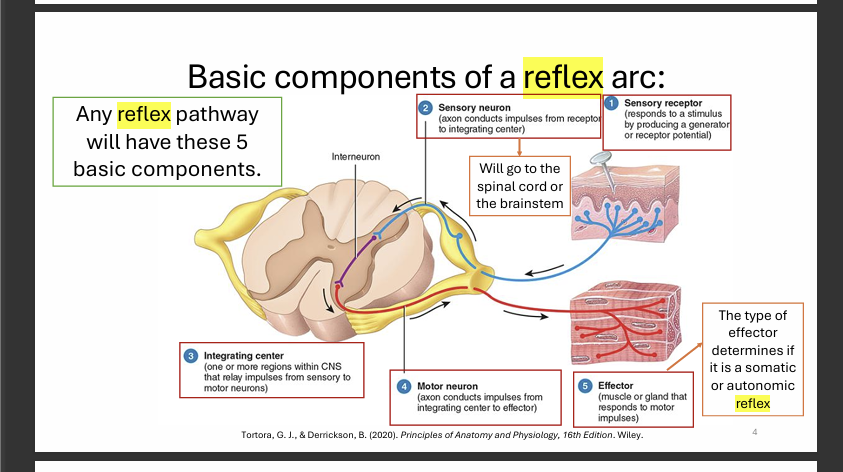
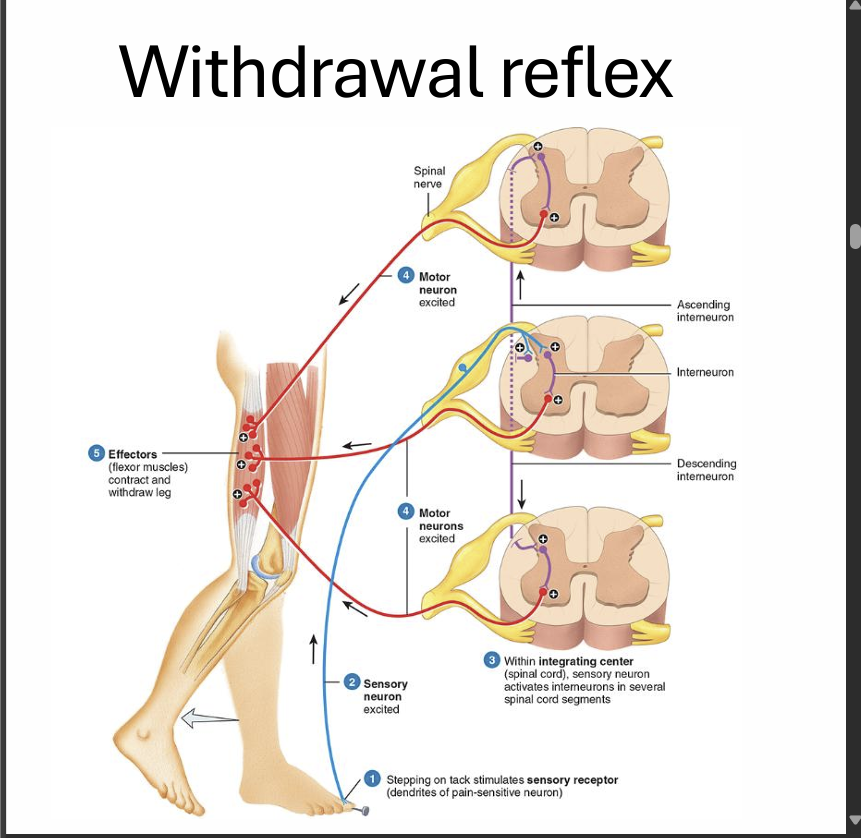
Basic Components of a Reflex Arc
The fundamental elements present in any reflex pathway. Key components include:
Sensory Receptor: Detects the initial stimulus and converts it into an electrical signal.
Sensory Neuron: Transmits the sensory information from the receptor to the integrating center (spinal cord or brainstem).
Integrating Center: Processes the sensory information and formulates an appropriate response; this can be a single synapse (monosynaptic) or multiple synapses involving interneurons (polysynaptic).
Motor Neuron: Carries the response signal from the integrating center to the effector.
Effector: The muscle or gland that carries out the response.
Stretch Reflex
A stretch reflex, also known as a myotatic reflex, is a type of monosynaptic reflex that is activated when a muscle is stretched. This reflex helps to maintain muscle tone, posture, and protect muscles from injury by causing them to contract when they are stretched too far or too quickly.
Mechanism:
Muscle spindles, specialized sensory receptors within the muscle, detect stretching.
Sensory neurons transmit signals from the muscle spindles to the spinal cord.
In the spinal cord, sensory neurons directly synapse with motor neurons, creating a monosynaptic connection.
Motor neurons are activated, causing the stretched muscle to contract. This contraction resists further stretching.
Function:
Prevents overstretching and potential muscle damage by causing immediate muscle contraction.
Helps maintain posture and balance by continuously adjusting muscle tone in response to subtle changes in muscle length.
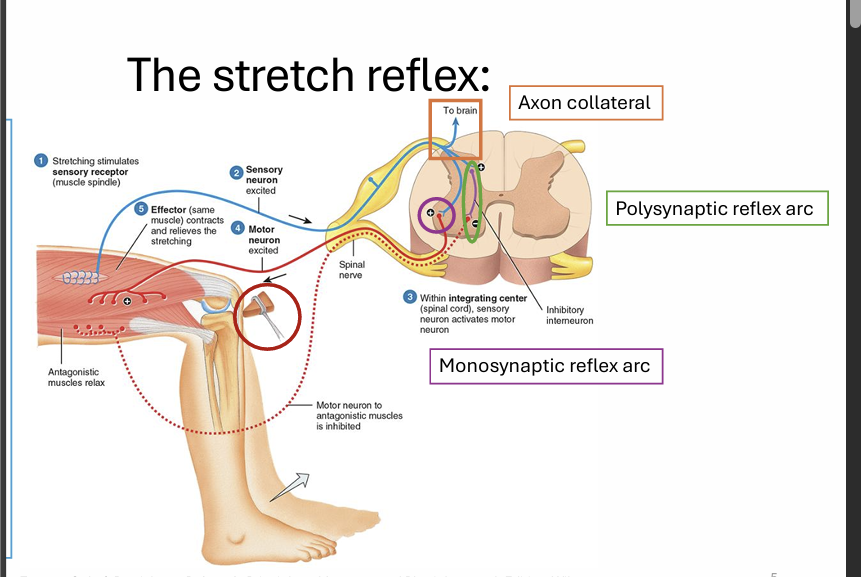
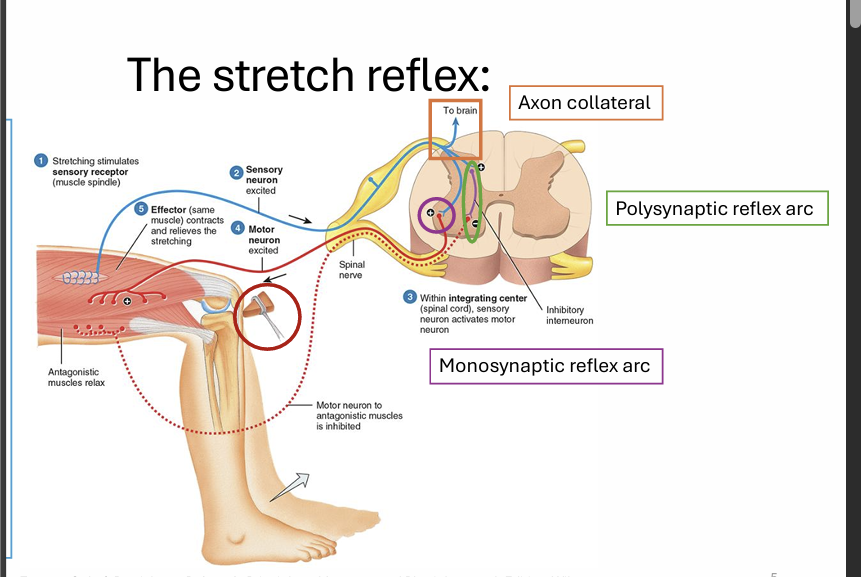
Polysynaptic Reflex Arc
A reflex arc that involves multiple synapses, typically involving one or more interneurons, between the sensory and motor neurons. Due to the involvement of interneurons, these reflexes can produce more complex and coordinated responses.
Examples include the withdrawal reflex and the crossed extensor reflex, where multiple muscle groups are activated to produce a coordinated movement.
Monosynaptic Reflex Arc
A reflex arc that involves a single synapse between a sensory and motor neuron. This direct connection allows for very rapid responses. The stretch reflex, such as the knee-jerk reflex, is a classic example of a monosynaptic reflex arc.
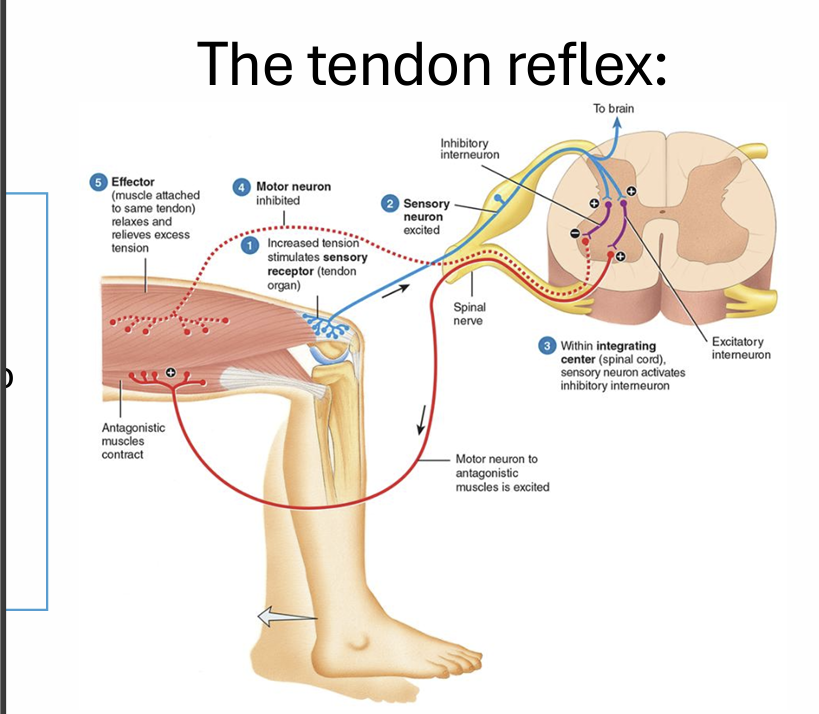
Tendon Reflex
A reflex that initiates muscle relaxation to prevent excessive muscle tension, mediated by Golgi tendon organs.
When muscle tension becomes too high, Golgi tendon organs are activated, which then inhibit the motor neurons supplying the muscle, causing it to relax. This protects the muscle and tendons from damage.
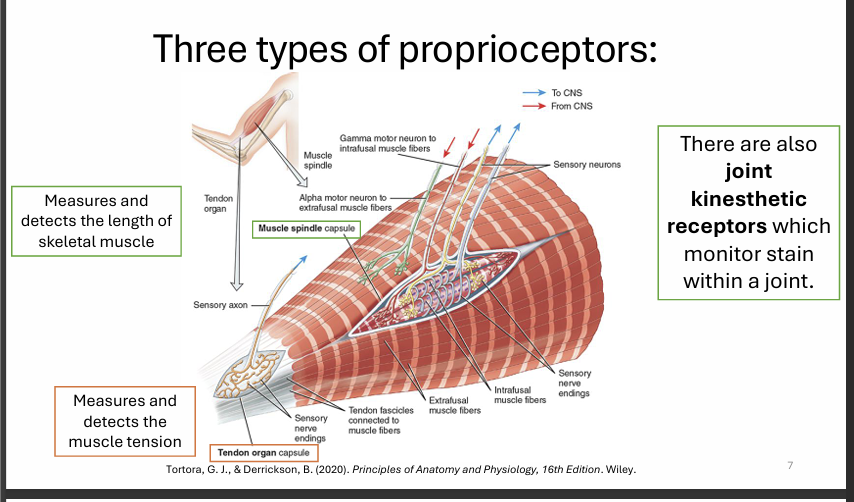
Proprioceptors
Sensory receptors located within muscles, tendons, and joints that measure and detect the length and tension of skeletal muscles.
They monitor strain within a joint to provide information about body position, muscle tone, and movement.
This information is crucial for coordinating movement and maintaining posture and balance.
Withdrawal Reflex
A protective reflex to avoid further tissue damage by rapidly withdrawing from a painful stimulus. This reflex involves multiple synapses (polysynaptic) to coordinate the action of several muscle groups: flexor muscles contract to withdraw the limb, while extensor muscles are inhibited to facilitate the movement. This process occurs almost instantaneously to minimize harm.
Sensory Signalling
The process of transmitting sensory information from the periphery (sensory receptors) to the brain for interpretation and conscious perception. This complex process involves several steps:
- Reception: Sensory receptors detect stimuli.
- Transduction: Receptors convert the stimuli into electrical signals (action potentials).
- Conduction: Neurons transmit these signals along sensory pathways to the brain.
- Interpretation: The brain processes and interprets the sensory information, allowing for conscious awareness.
Spinal Cord Signalling
The transmission of sensory input coming into the spinal cord from the periphery via three possible routes:
To Higher Brain Centers: Sensory information is transmitted through ascending tracts to the brain for conscious perception and further processing.
Local Interneurons: Sensory input synapses with local interneurons to modulate local reflexes and spinal cord circuitry.
Motor Neurons: Sensory input directly activates motor neurons to produce rapid reflex responses.
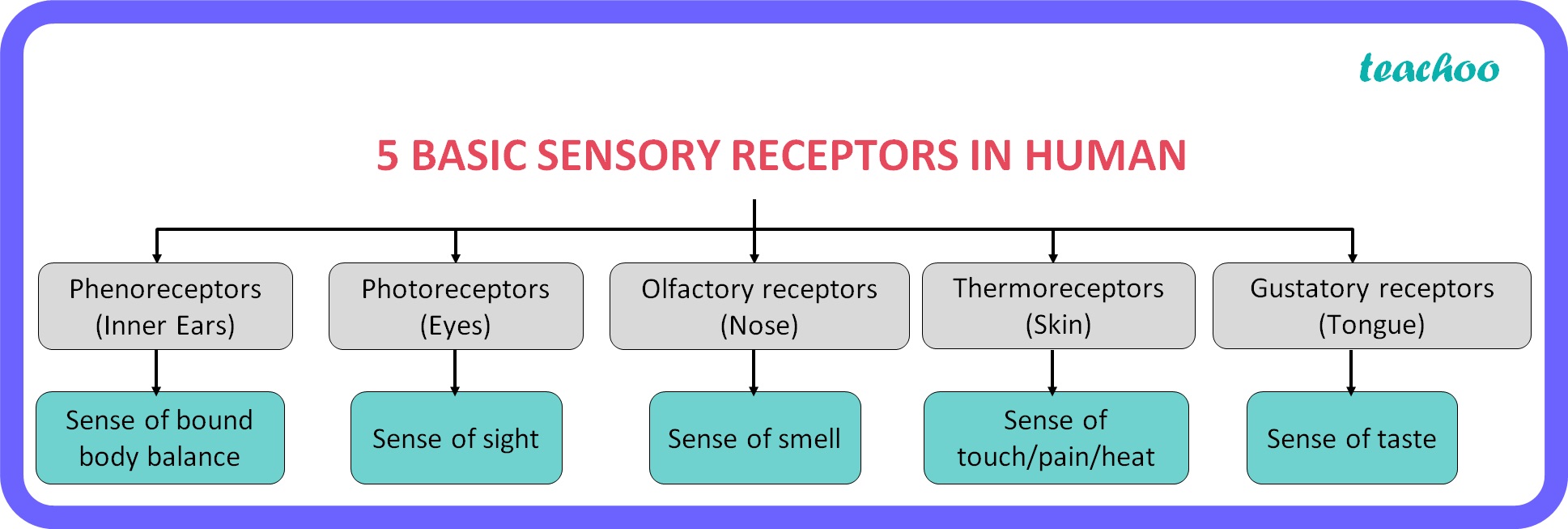
General Senses
Sensory modalities that include:
somatic:
Tactile: Touch, vibration, pressure, itch, and tickle.
Thermal: Temperature sensations (hot and cold).
Pain: Nociception, the sensation of pain.
Proprioception: Awareness of body position and movement.
Visceral Senses:
Sensations arising from internal organs, such as hunger, nausea, and fullness.
Special Senses
Sensory modalities including:
- Smell (Olfaction)
- Taste (Gustation)
- Vision (Sight)
- Hearing (Audition)
- Balance/Equilibrium: Senses related to spatial orientation and balance.
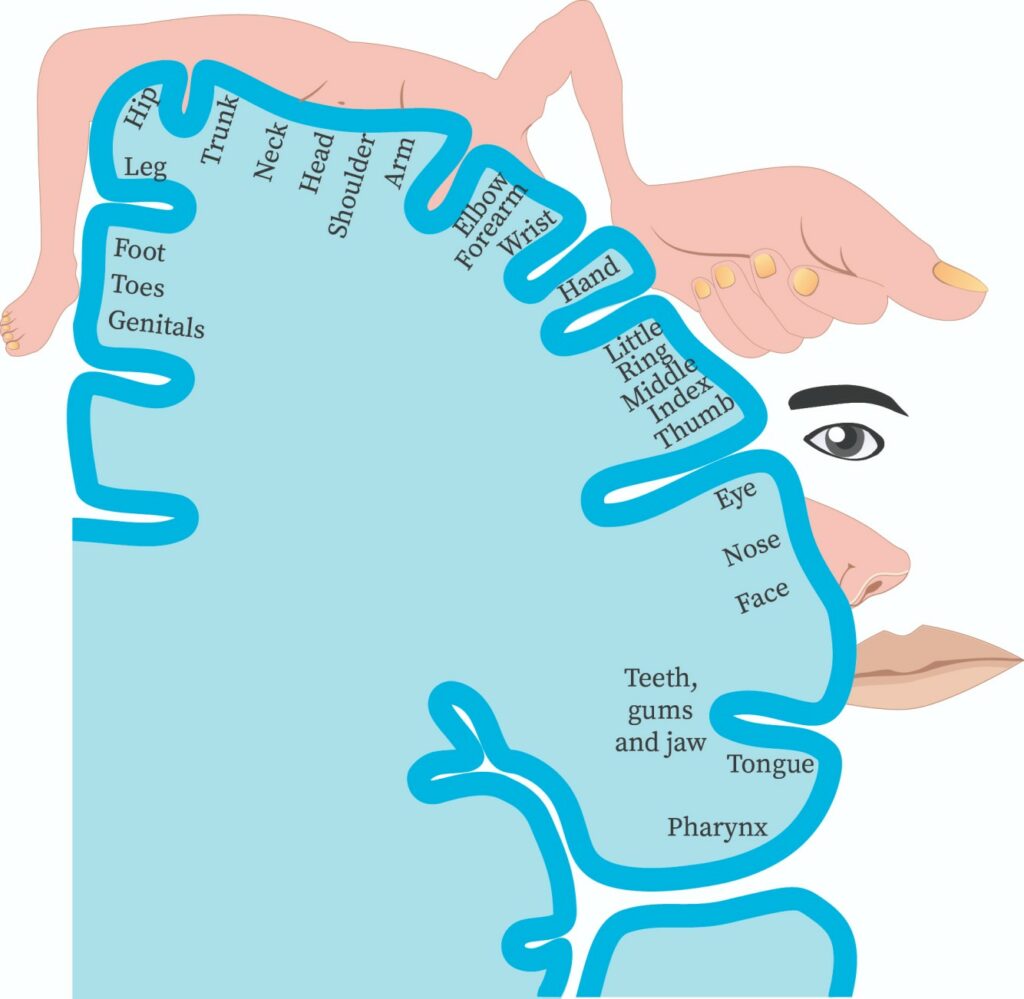
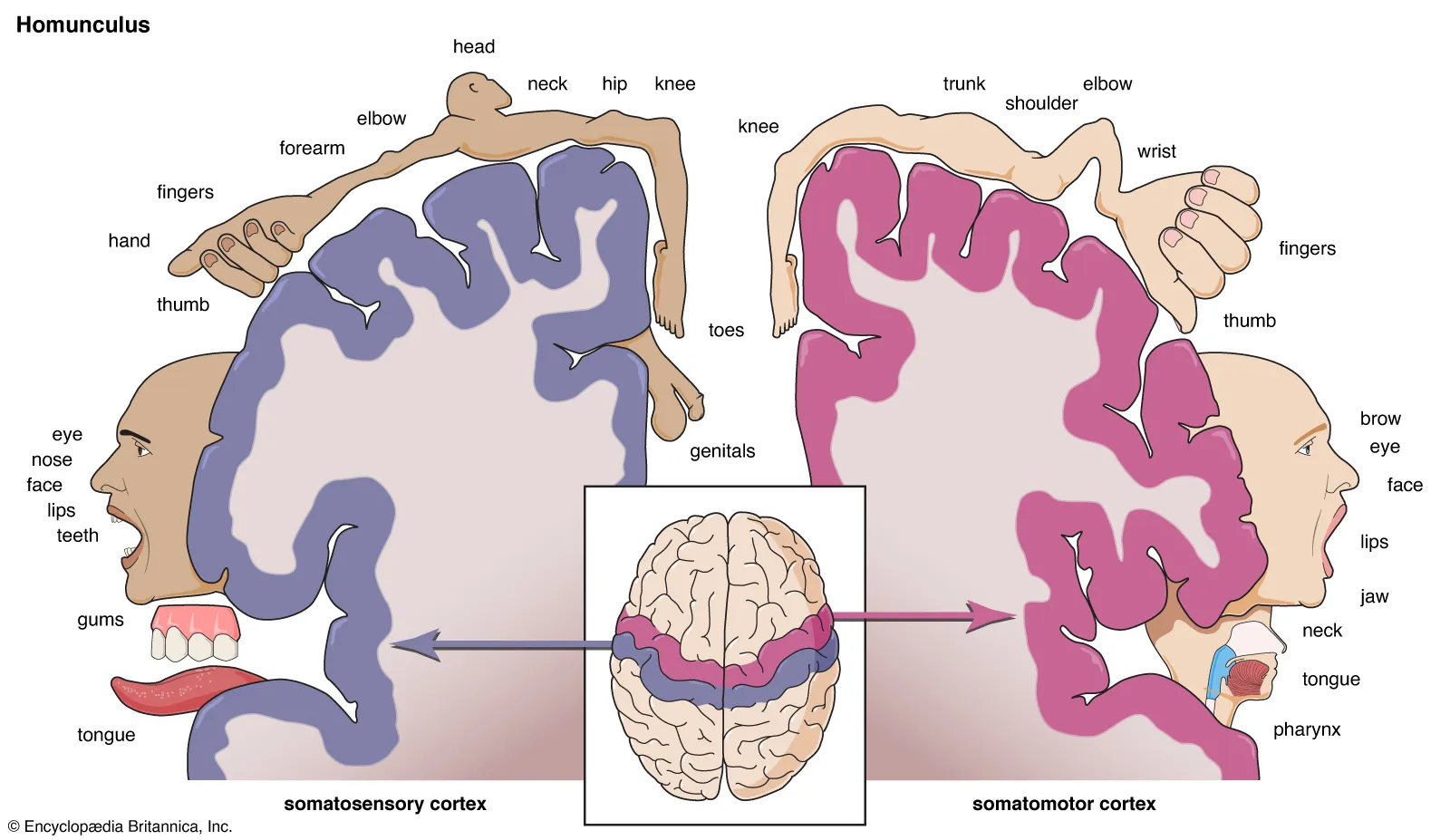
Primary Somatosensory Cortex
Located in the parietal lobe, this cortical area receives and processes information related to:
Touch
Temperature
Pressure
Vibration
Proprioception
Itch
Tickle
Pain
sensory homunculus
This allows for conscious perception of these sensations, enabling the discrimination of different stimuli and their location on the body.
Sensory Homunculus
A cortical map located on the primary somatosensory cortex that represents the areas dedicated to processing sensory information from different parts of the body.
Areas with higher sensitivity (e.g., lips, hands) have larger representations on the homunculus, indicating a greater density of sensory receptors and a higher degree of cortical processing.
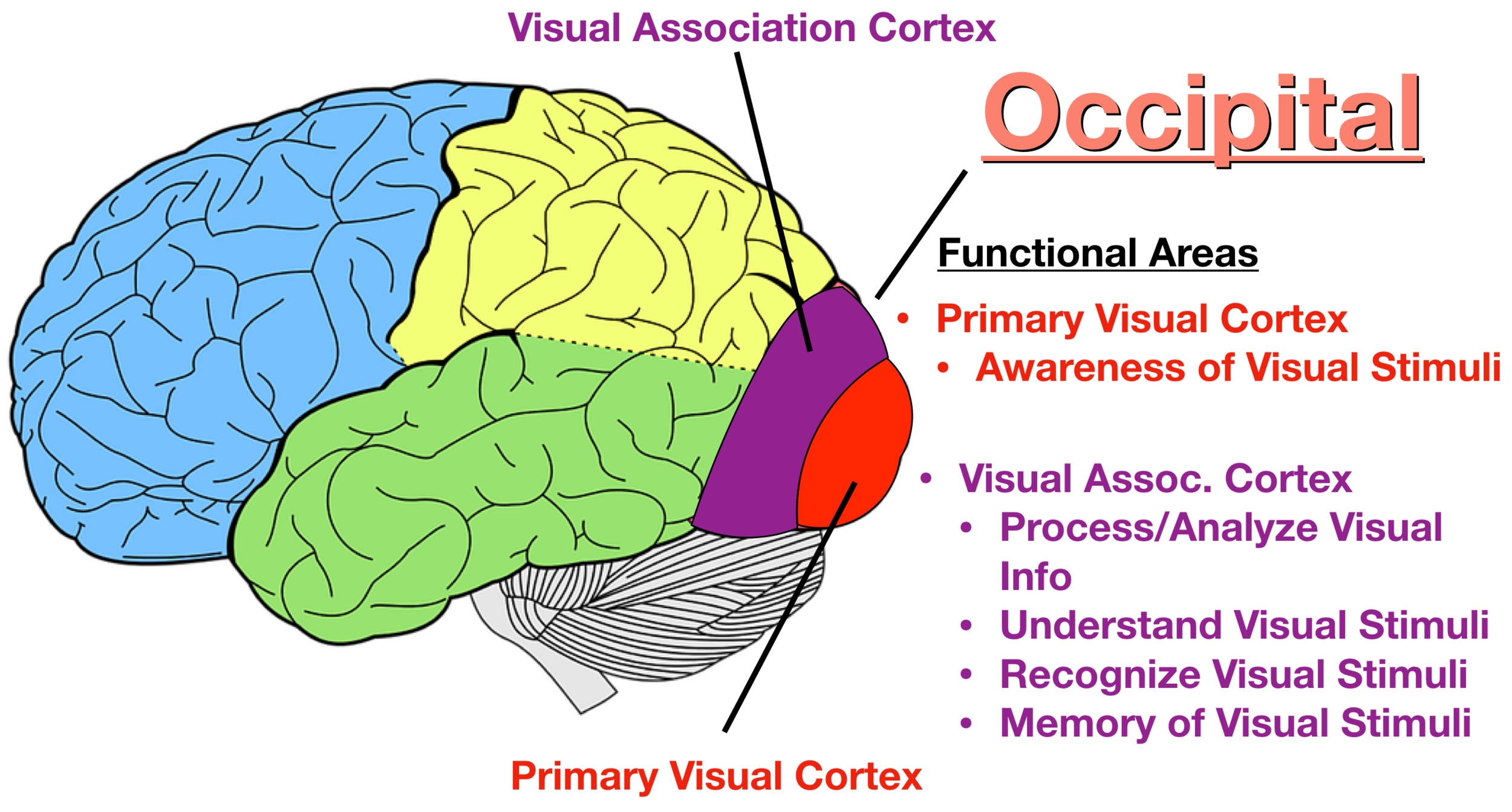
Primary Visual Cortex
Located in the occipital lobe, this cortical area receives visual input from the eyes. It is crucial Initial processing of visual information involves:
Detection of basic features like edges, lines, and colors.
Integration of visual signals to form a basic representation of the visual scene.
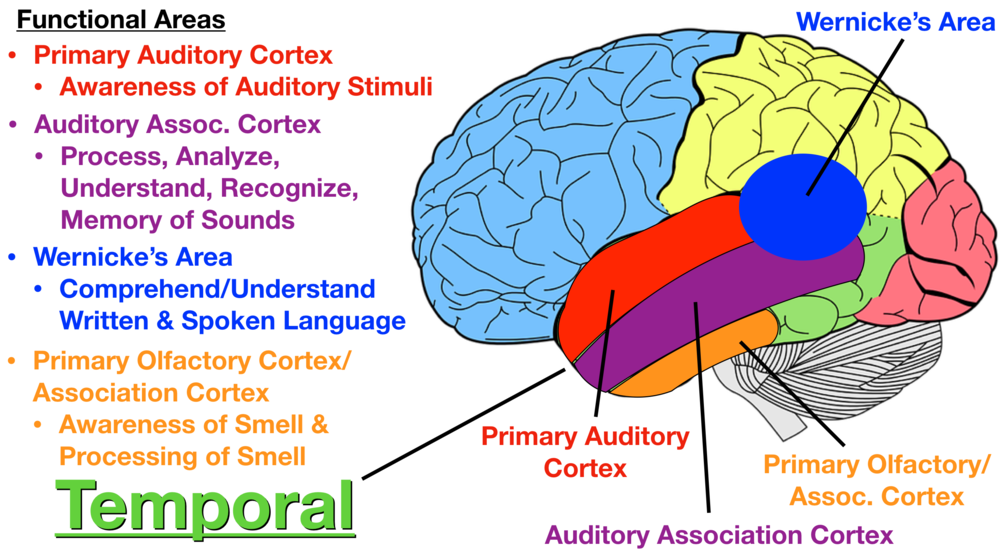
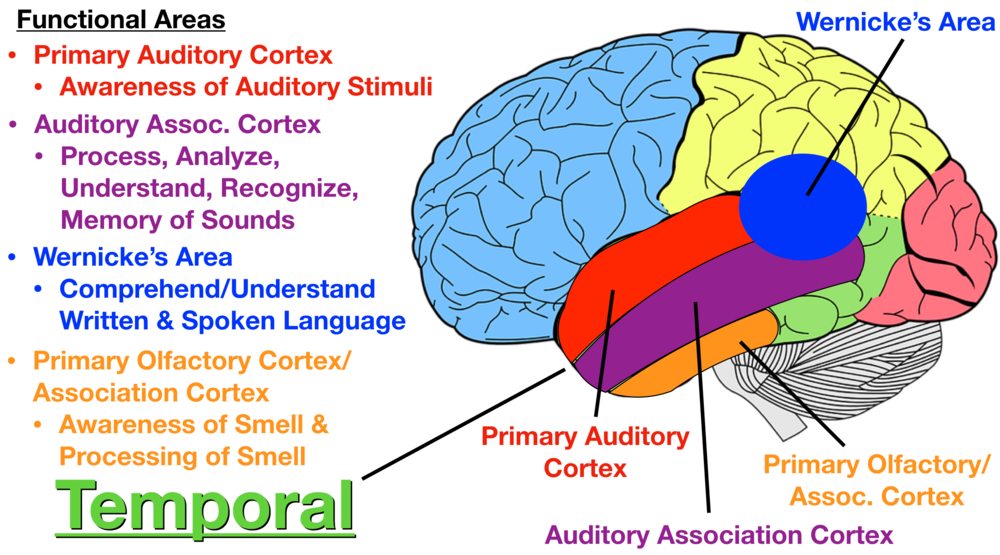
Primary Auditory Cortex
Located in the temporal lobe, this cortical area receives auditory input from the ears. Initial processing of sound information includes:
Detection of sound frequency (pitch), intensity (loudness), and location.
Integration of auditory signals to form a basic representation of sounds.
Gustatory Cortex
Located in the insula, this cortical area receives taste input from taste receptors on the tongue. The gustatory cortex processes information about:
Basic taste qualities (sweet, sour, salty, bitter, and umami).
Integration of taste signals to create a perception of flavor.
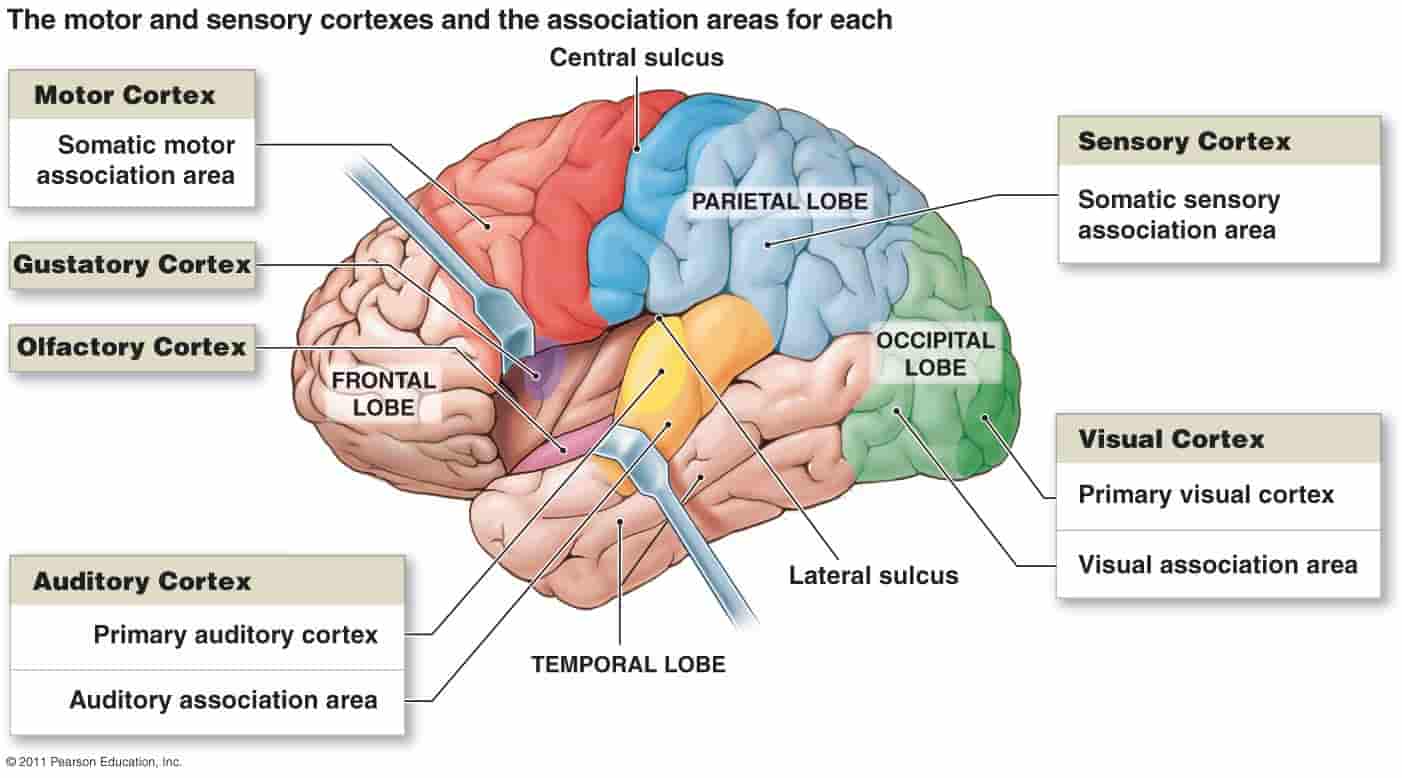
Olfactory Cortex
Located in the temporal lobe, this cortical area receives smell input from olfactory receptors in the nasal cavity. The olfactory cortex is involved in:
Processing different odor qualities.
Associating smells with memories and emotions, thanks to its close connections with the limbic system.
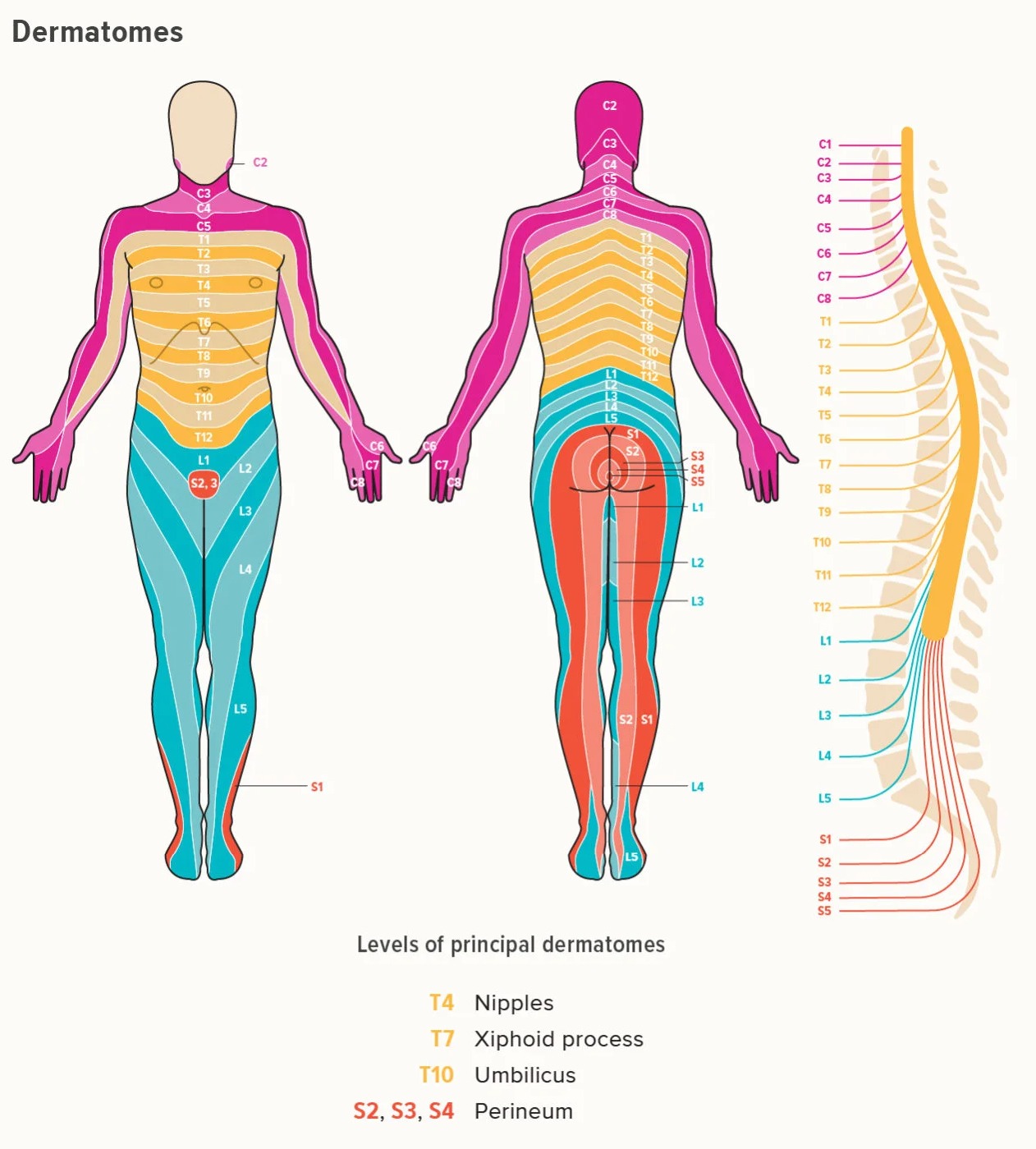
Sensory Input: Dermatomes
All incoming sensory information from the skin (except the front of the face) is sent to the spinal cord via specific spinal nerves. Each spinal nerve corresponds to a specific area of skin called a dermatome. Dermatomes are clinically important because:
Each dermatome is associated with a specific spinal nerve, allowing clinicians to identify the level of spinal injury based on sensory loss.
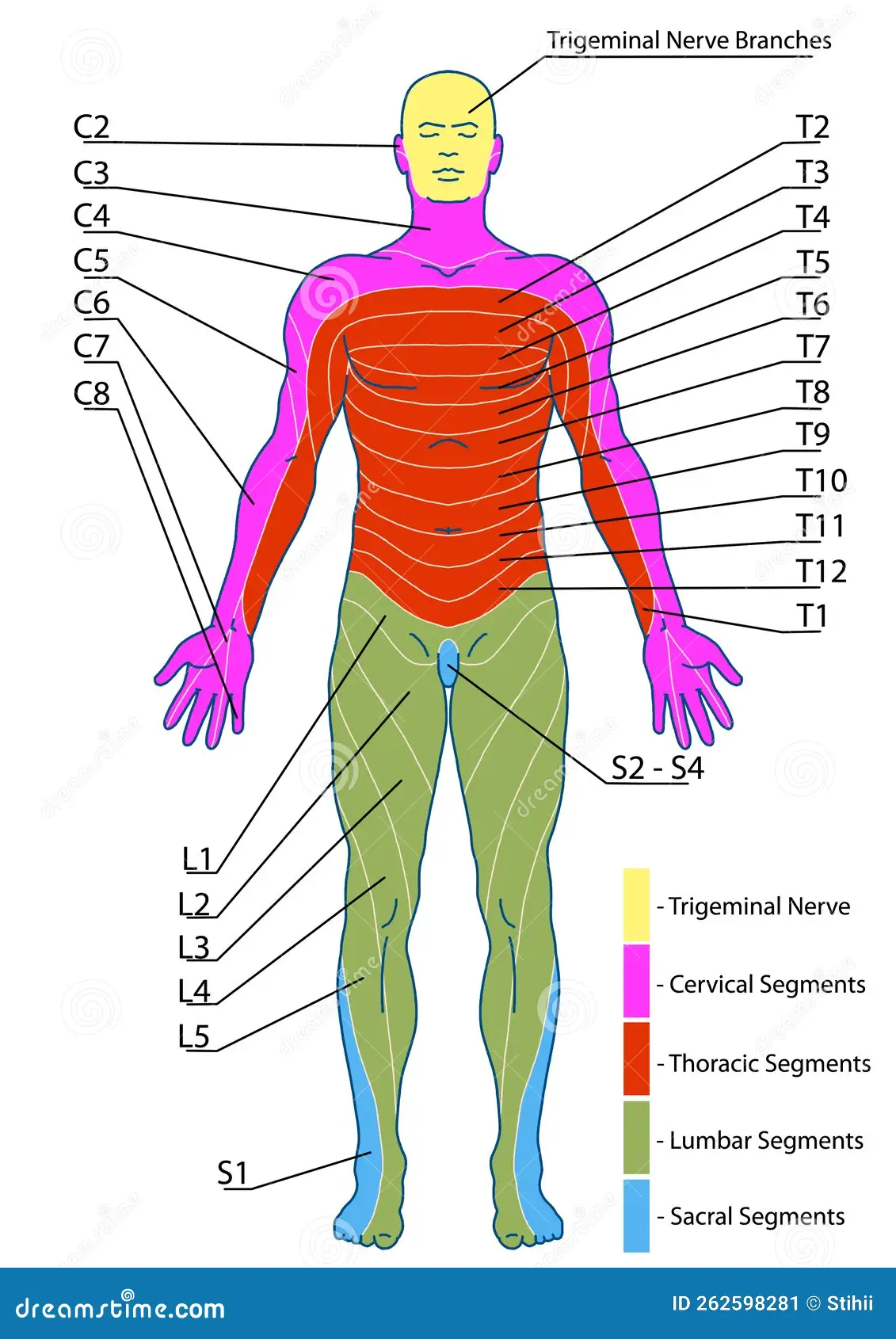
Dermatome Map
A map that shows the area of skin that each spinal nerve (dermatome) covers. This is useful for:
Diagnosing spinal nerve damage: By testing sensory function in different dermatomes, clinicians can identify which spinal nerve(s) are affected.
Understanding referred pain: Pain from internal organs may be referred to specific dermatomes, aiding in diagnosis.
Somatic Sensory Pathways
The two main pathways that transmit somatic sensory information to the brain:
Posterior column-medial lemniscus pathway:
Carries information about fine touch, vibration, and proprioception.
Signals ascend ipsilaterally (on the same side of the body) in the posterior columns of the spinal cord before crossing over in the medulla.
Anterolateral pathway (also known as the spinothalamic tract):
Carries information about pain, temperature, and crude touch.
Signals cross over in the spinal cord before ascending to the thalamus.
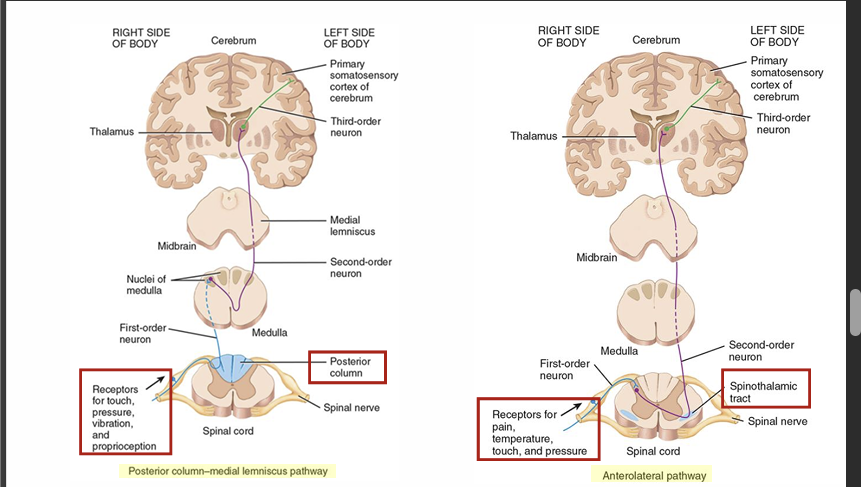
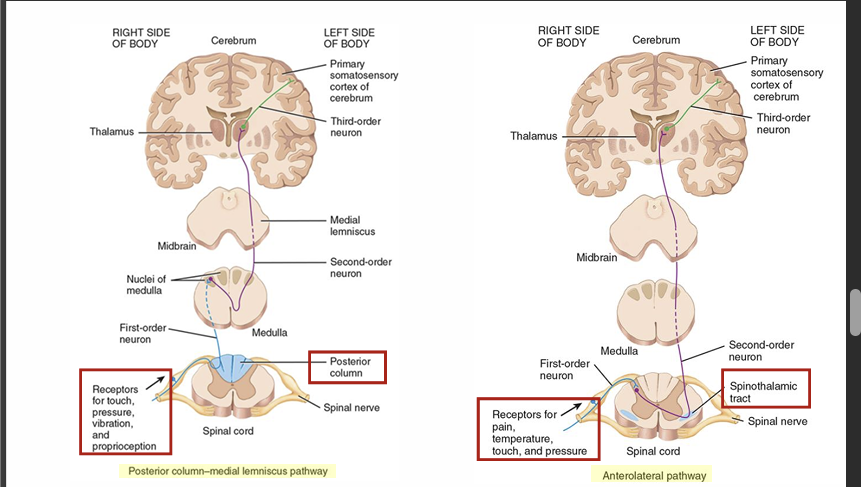
Spinal Cord Tracts for Sensory Signals
Specific bundles of nerve fibers in the spinal cord that transmit different types of sensory information:
Touch: Carried by pathways such as the anterior spinothalamic tract.
Pressure: Also carried by the anterior spinothalamic tract.
Vibration: Carried by the posterior column-medial lemniscus pathway.
Conscious Proprioception: Carried by the posterior column-medial lemniscus pathway.
Unconscious Proprioception: Carried by the spinocerebellar tracts to the cerebellum.
Pain: Carried by the lateral spinothalamic tract.
Temperature: Carried by the lateral spinothalamic tract.
Itch and Tickle: Believed to be carried by the anterior spinothalamic tract, though the specific pathways are still being researched.
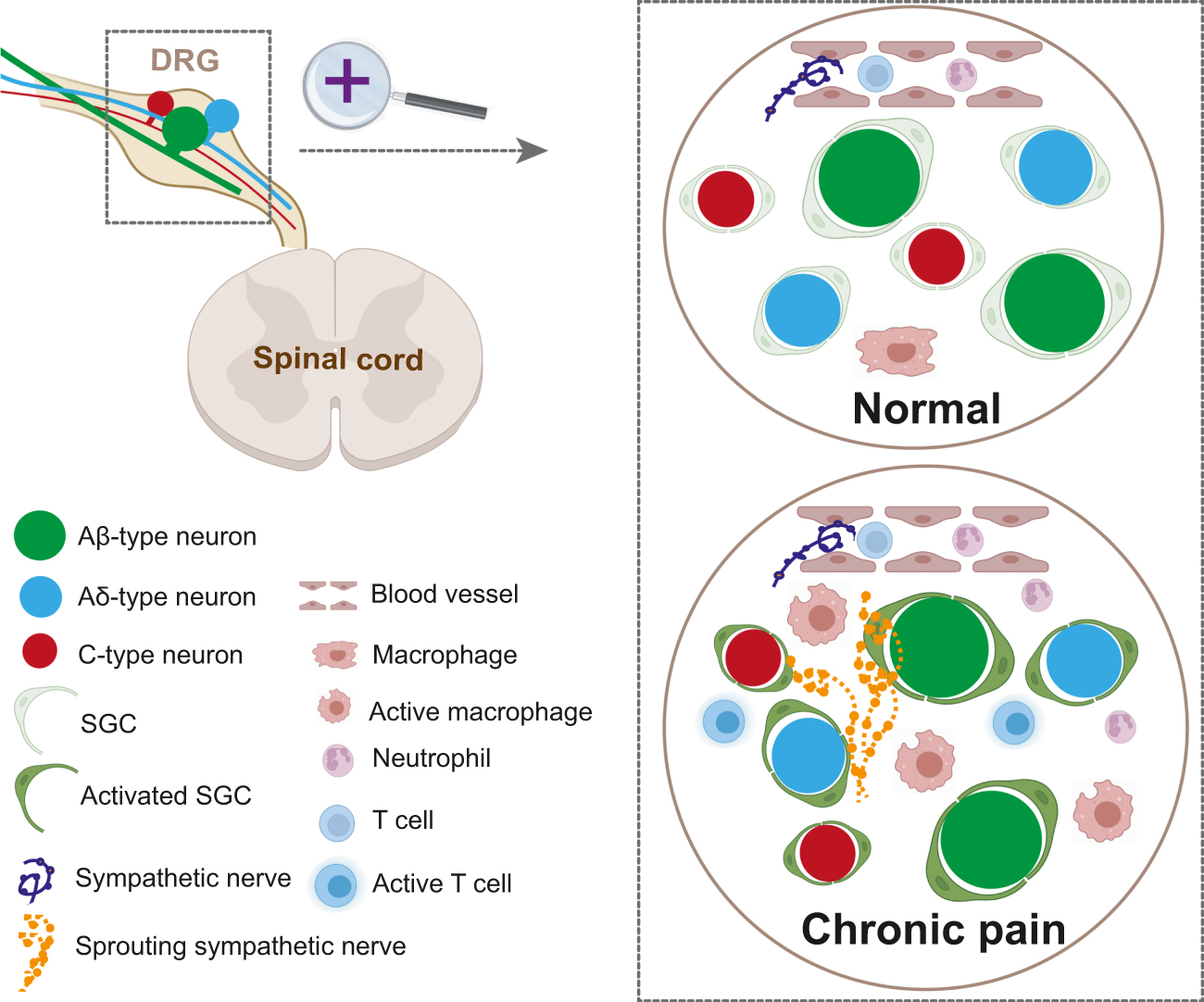
Types of Pain Sensations
Two primary types of pain:
Slow (Chronic) Pain:
Has a relatively slow onset (>1 second after the stimulus).
Characterized by burning, aching, or throbbing sensations.
Typically mediated by unmyelinated C fibers, which conduct signals more slowly.
Fast (Acute) Pain:
Has a rapid onset (approximately 0.1 second after the stimulus).
Characterized by a pricking or sharp sensation.
Typically mediated by myelinated Aδ fibers, which conduct signals more quickly.
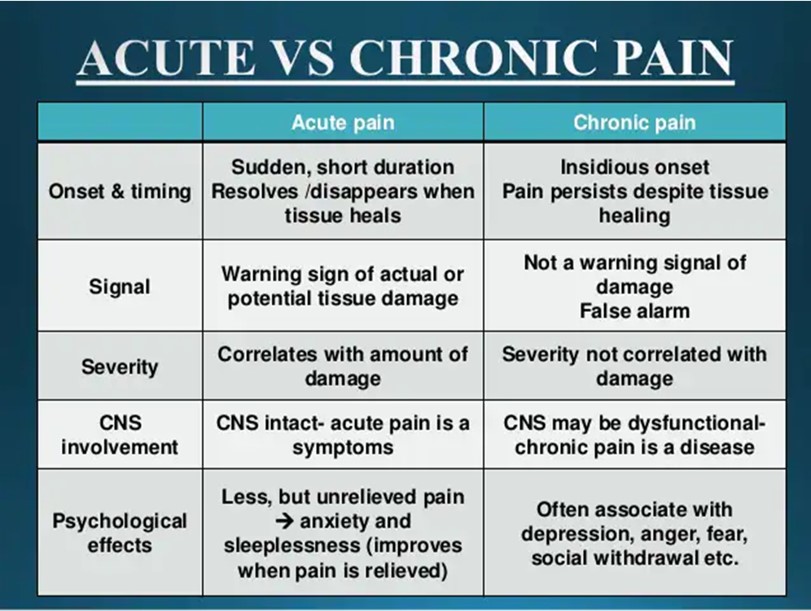
Slow (Chronic) Pain
Pain that onsets more than 1 second after the stimulus and involves burning, aching, or throbbing sensations. This type of pain is:
Typically mediated by unmyelinated C fibers, which conduct signals slowly.
Often associated with chronic conditions and can be more diffuse and long-lasting.
exmaple: toothache
Fast (Acute) Pain
Pain with a rapid onset (approximately 0.1 second after the stimulus) and involves a pricking or sharp sensation. This type of pain is:
Typically mediated by myelinated Aδ fibers, allowing for rapid signal conduction.
Highly localized and allows for quick responses to acute injury.
example: needle
Primary Motor Cortex
Located in the frontal lobe, this cortical area is the primary region involved in the voluntary control of movement. It:
- Initiates movements in specific parts of the body by sending signals down motor pathways to the muscles.
- Contains a somatotopic map (motor homunculus) where different parts of the cortex control different body regions.
Motor Homunculus
A cortical map located on the primary motor cortex that represents the areas dedicated to controlling muscles in different parts of the body. Areas with finer motor control:
- (e.g., hands, face) have larger representations on the homunculus, indicating a greater number of motor neurons dedicated to those regions.
Premotor Cortex
Located in the frontal lobe, this cortical area works in coordination with the primary motor cortex to:
- Coordinate complex movements that involve multiple muscle groups.
- Plan movements based on sensory feedback and learned motor patterns.
- Control movements that are guided by sensory information (e.g., reaching for an object).
Broca's Area
Located in the frontal lobe, typically on the left side, this cortical area is responsible for:
- Coordinating the motor components of speech production.
- Forming words and sentences by controlling the muscles of the face, tongue, and throat.
- Damage to Broca's area results in expressive aphasia, characterized by difficulty forming words but comprehension is still there.
Frontal Eye Field
Located in the frontal lobe, this cortical area is responsible for:
- Voluntary eye scanning movements, allowing for conscious control of eye movements.
- Coordinating eye movements with other motor and sensory functions.
Motor Pathways
Two main pathways that transmit motor commands from the brain to the spinal cord:
Lateral corticospinal pathway:
Controls precise, voluntary movements of the limbs. Signals cross over in the medulla, and then descends in the lateral white matter to control the limbs.
Anterior corticospinal pathway:
Controls voluntary movements of the trunk and proximal limbs.
Signals do not cross over in the medulla, and descends in the anterior white matter to control the midline muscles of the trunk.
both control voluntary movements of the skeletal muscles in the trunk and limbs
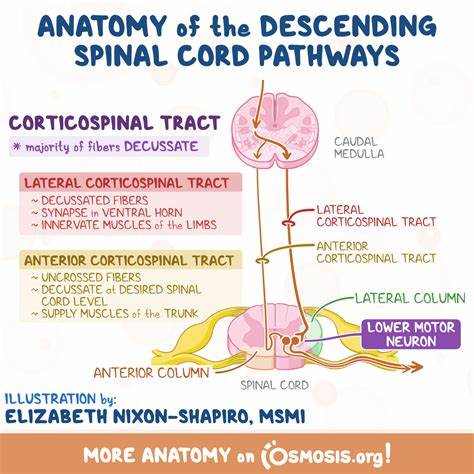
Spinal Cord Tracts for Motor Signals
Specific bundles of nerve fibers in the spinal cord that transmit motor signals. These are divided into:
- DIRECT (Pyramidal) Pathways:
- For voluntary movement, such as the corticospinal tracts controlling limb and axial musculature.
- INDIRECT (Extrapyramidal) Pathways:
- For involuntary movement, such as the vestibulospinal, tectospinal, and reticulospinal tracts for balance, posture, and muscle tone.
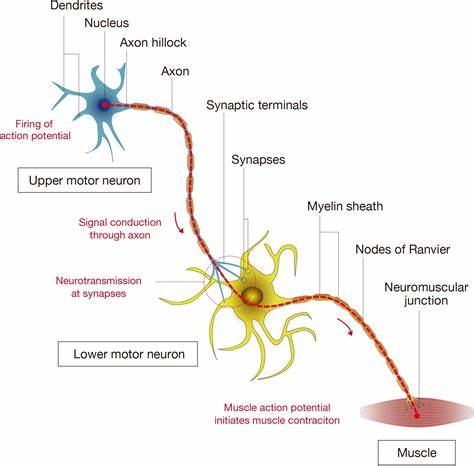
Lower Motor Neurons (LMNs)
Neurons that originate in the spinal cord or brainstem and extend to the skeletal muscle fibers. They are also known as:
Alpha motor neurons: Innervate extrafusal muscle fibers, responsible for muscle contraction.
Gamma motor neurons: Innervate intrafusal muscle fibers in muscle spindles, regulating muscle tone.
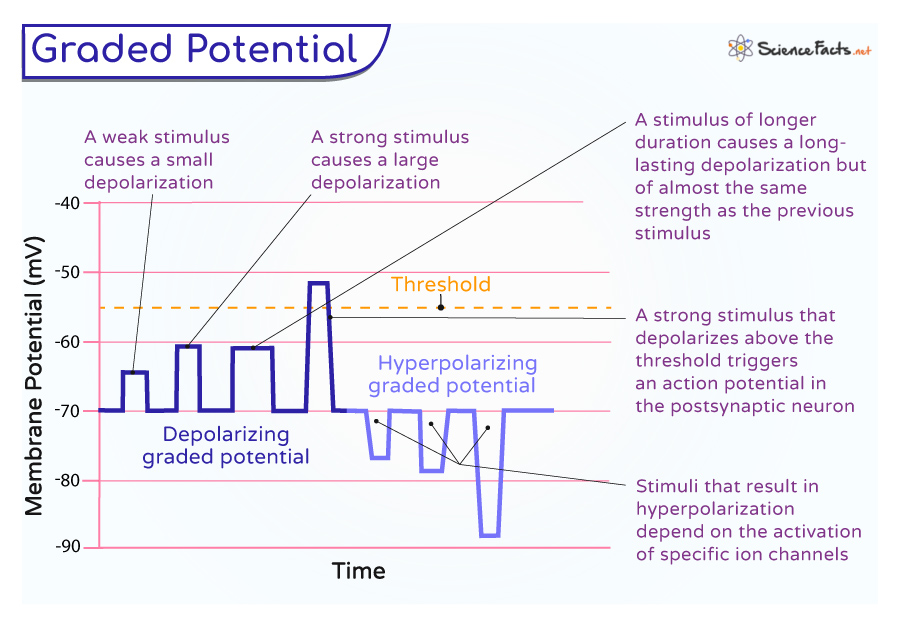
Graded Potentials
Local changes in membrane potential that are specialized for communication over short distances. These changes do not propagate down the axon like an action potential, but they are important for:
Integration of synaptic inputs: Graded potentials can summate to reach the threshold for triggering an action potential.
Varying amplitude: The amplitude of a graded potential is directly proportional to the strength of the stimuli. Larger stimuli result in greater changes in membrane potential.
travel a small distance by decremental conduction
electrical signaling of neurons is facilitated through the membrane potential created by the movement and location of ions
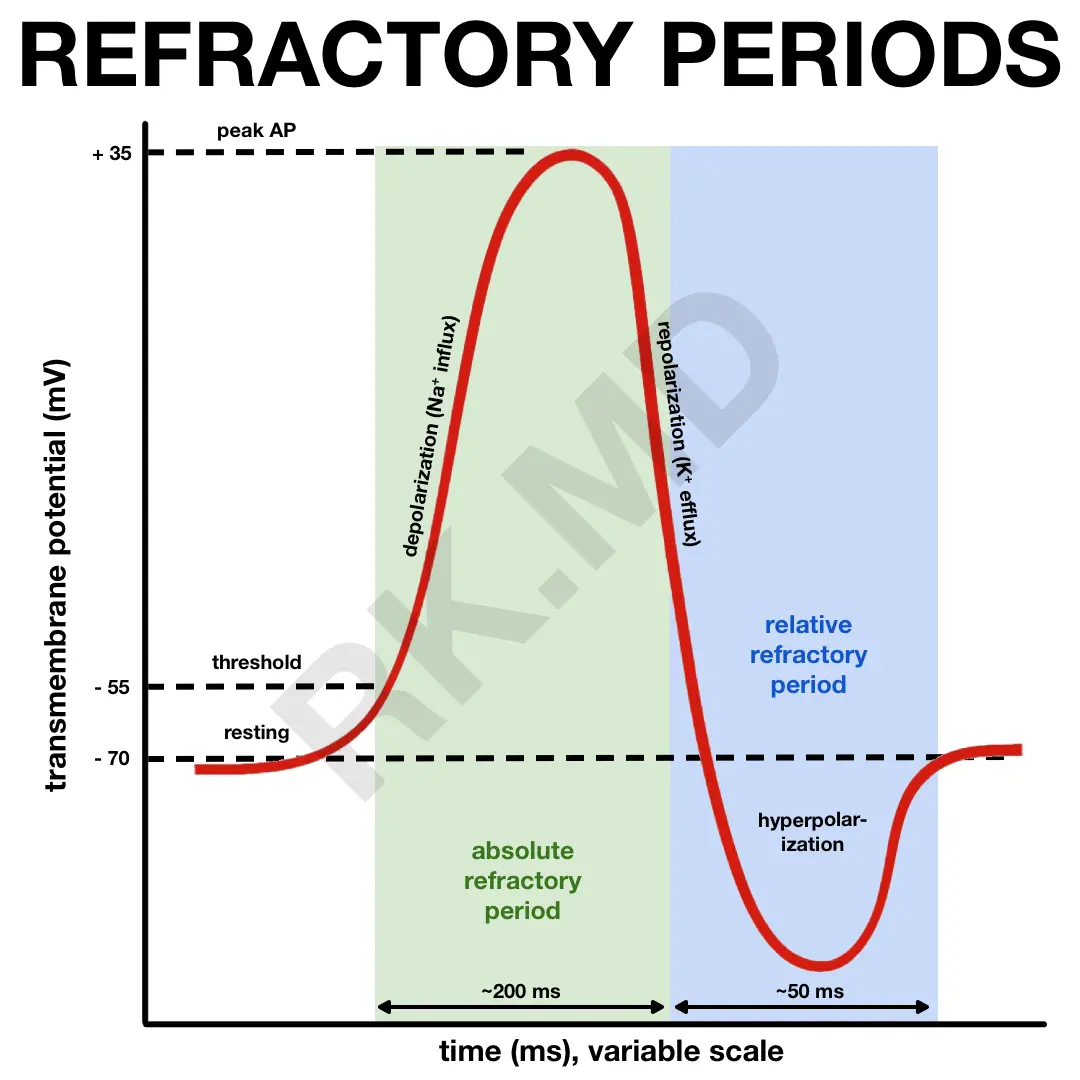
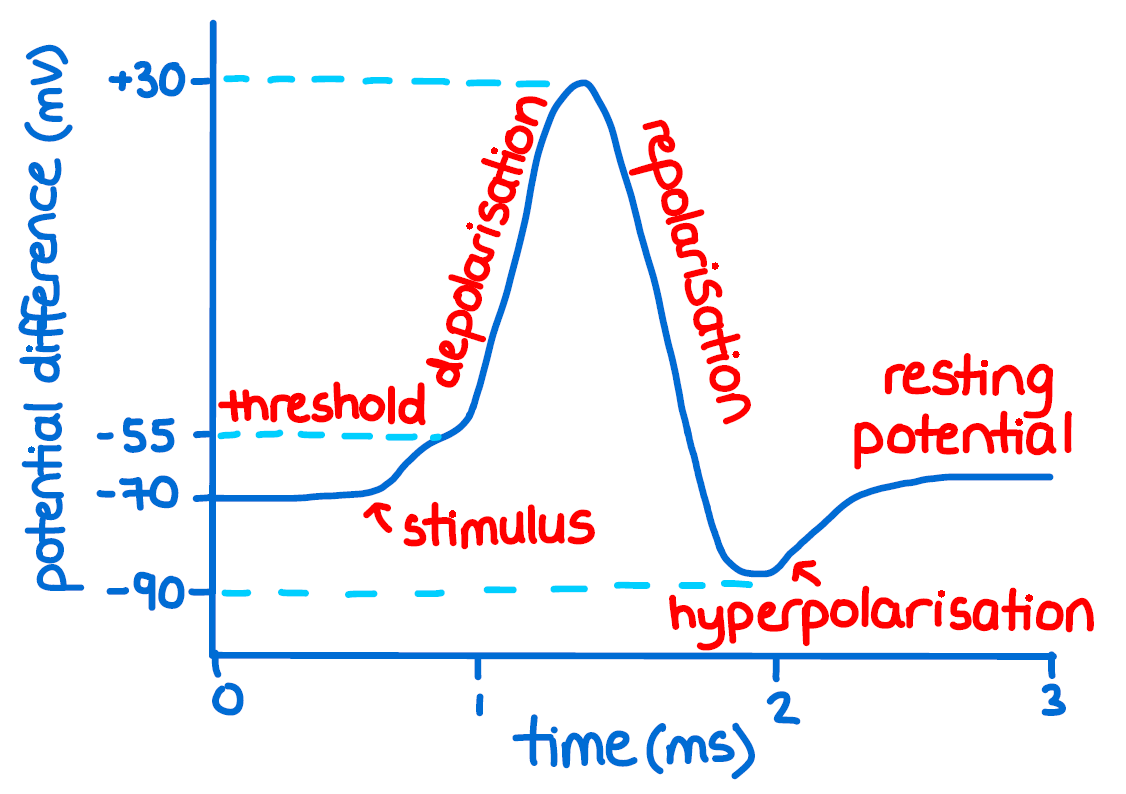
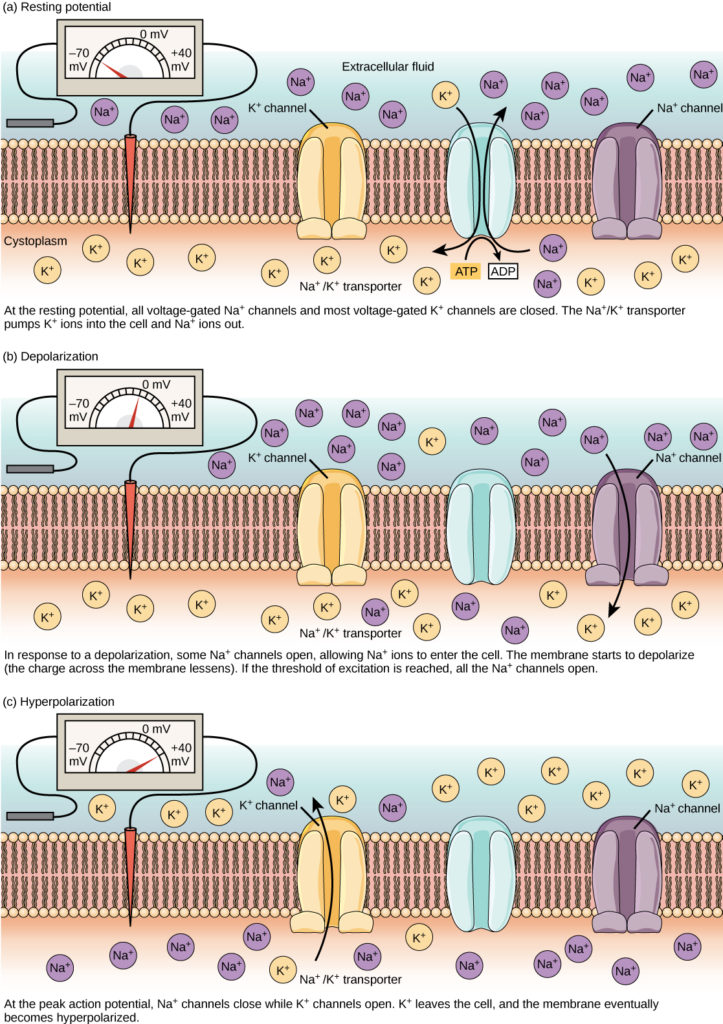
Action Potentials
Electrical signals that are specialized for communication over long distances within a neuron. Unlike graded potentials, action potentials are:
All-or-nothing Events: Once the threshold of membrane potential is reached, an action potential fires with a consistent amplitude.
Capable of propagating: Action potentials propagate down the axon without decreasing in amplitude, allowing for long-distance communication.
as the action potential occurs the K+ voltage channels are activated but tale longer to open compared to the Na+ gates
return to resting state when K+ gates close
Membrane Potential
The difference in electrical voltage across the cell membrane, created by the unequal distribution of ions (such as sodium, potassium, chloride, and calcium) between the inside and outside of the cell. This difference in charge is crucial for:
Neuronal Communication: Changes in membrane potential are fundamental to electrical signaling in neurons.
resting membrane potential = -40mV to 90mV (most common is -70mV)
establishes the movement of ions via ion channels
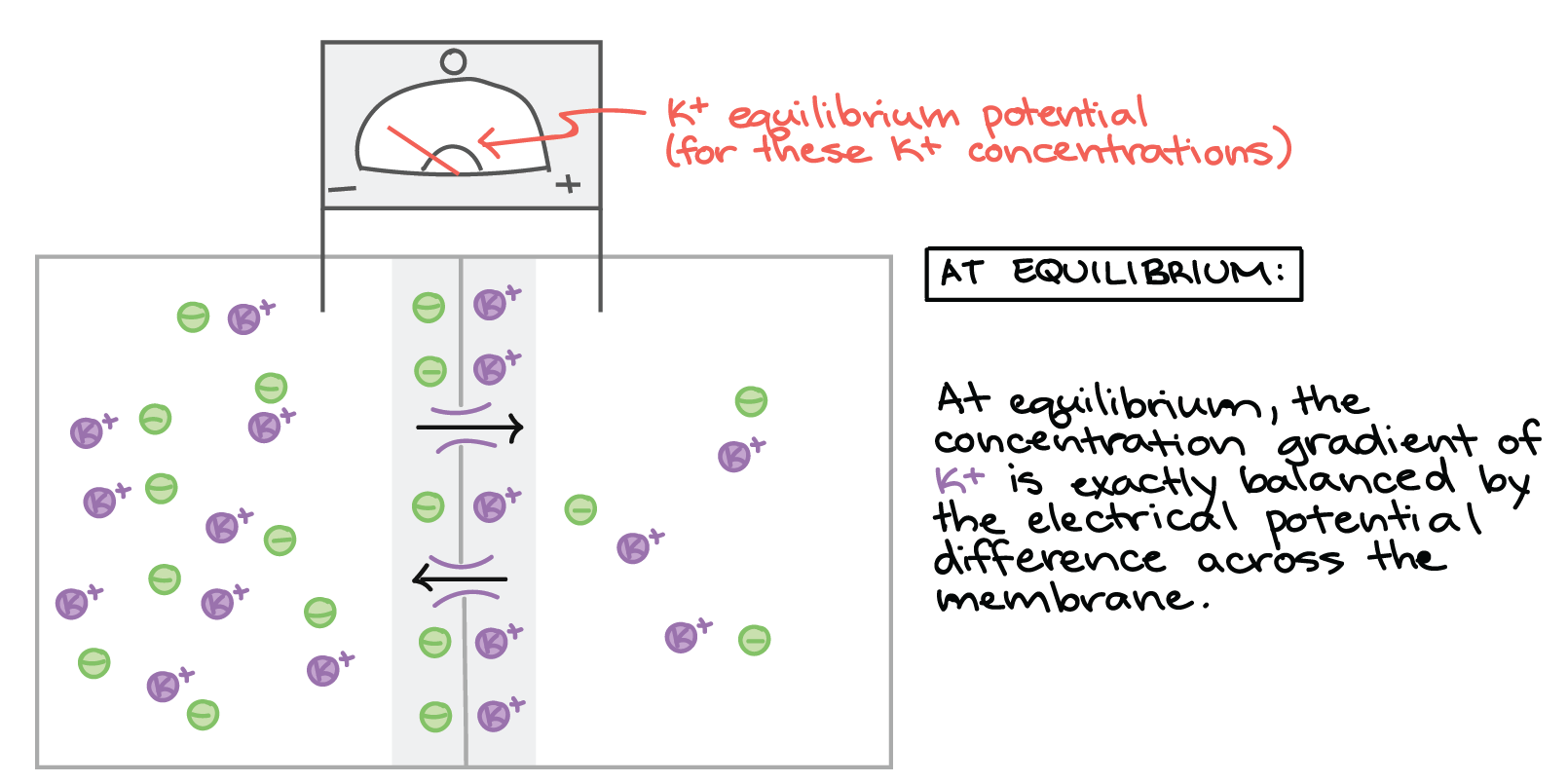
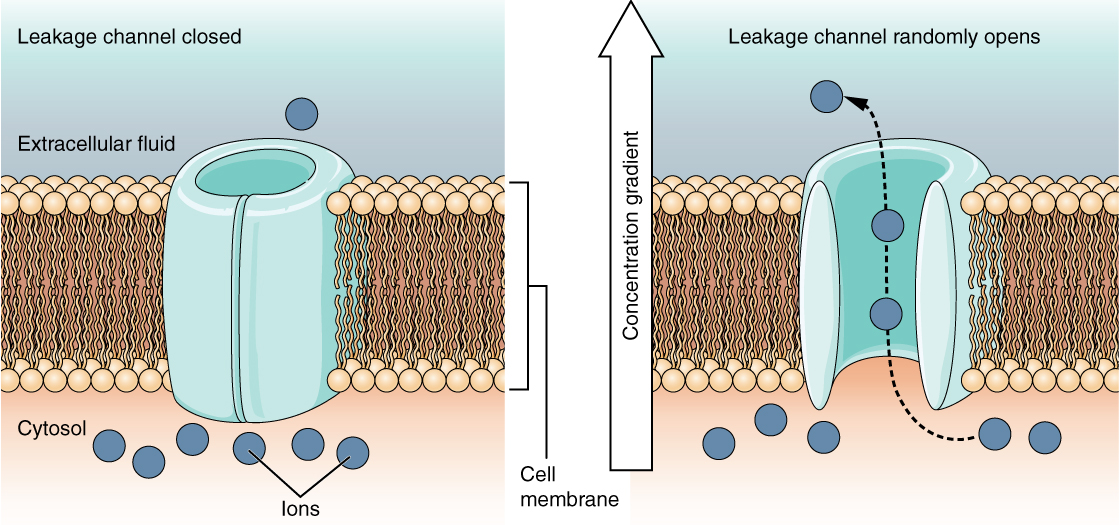
Resting Membrane Potential
The stable membrane potential of a cell when it is not being stimulated, typically ranging from -40mV to -90mV (most commonly -70mV). This resting state is maintained by:
Leak Channels: Allowing continuous diffusion of ions across the membrane.
Unequal Ion Distribution: Higher concentration of Na+ outside the cell and a higher concentration of K+ inside the cell.
Sodium-Potassium Pump: Actively transports Na+ and K+ to maintain ion gradients.
the charge only appears directly on either side of the membrane where there is buildup of the positive and negative ions
polarized cells are any cell with a membrane potential
extracellular fluid and cytosol usually have equal + and -
caused by uneven movement of K+ out compared to Na+ in leak channels
anions remaining inside the cell
Na+ - K + ATPase
Leak Channels
Ion channels that randomly open, allowing for the continuous diffusion of ions across the membrane, which contributes to permeability. Potassium (K+) and sodium (Na+) leak channels are crucial for maintaining resting membrane potential:
K+ Leak Channels: More numerous and leakier than Na+ channels, allowing more K+ to flow out of the cell, contributing to the negative resting membrane potential.
K+ Permeability
The degree to which potassium ions can flow across the cell membrane. K+ permeability is greater than Na+ permeability, which leads to:
- Higher concentration of Na+ outside the cell at rest.
- Negative resting membrane potential due to the efflux of K+ from the cell.
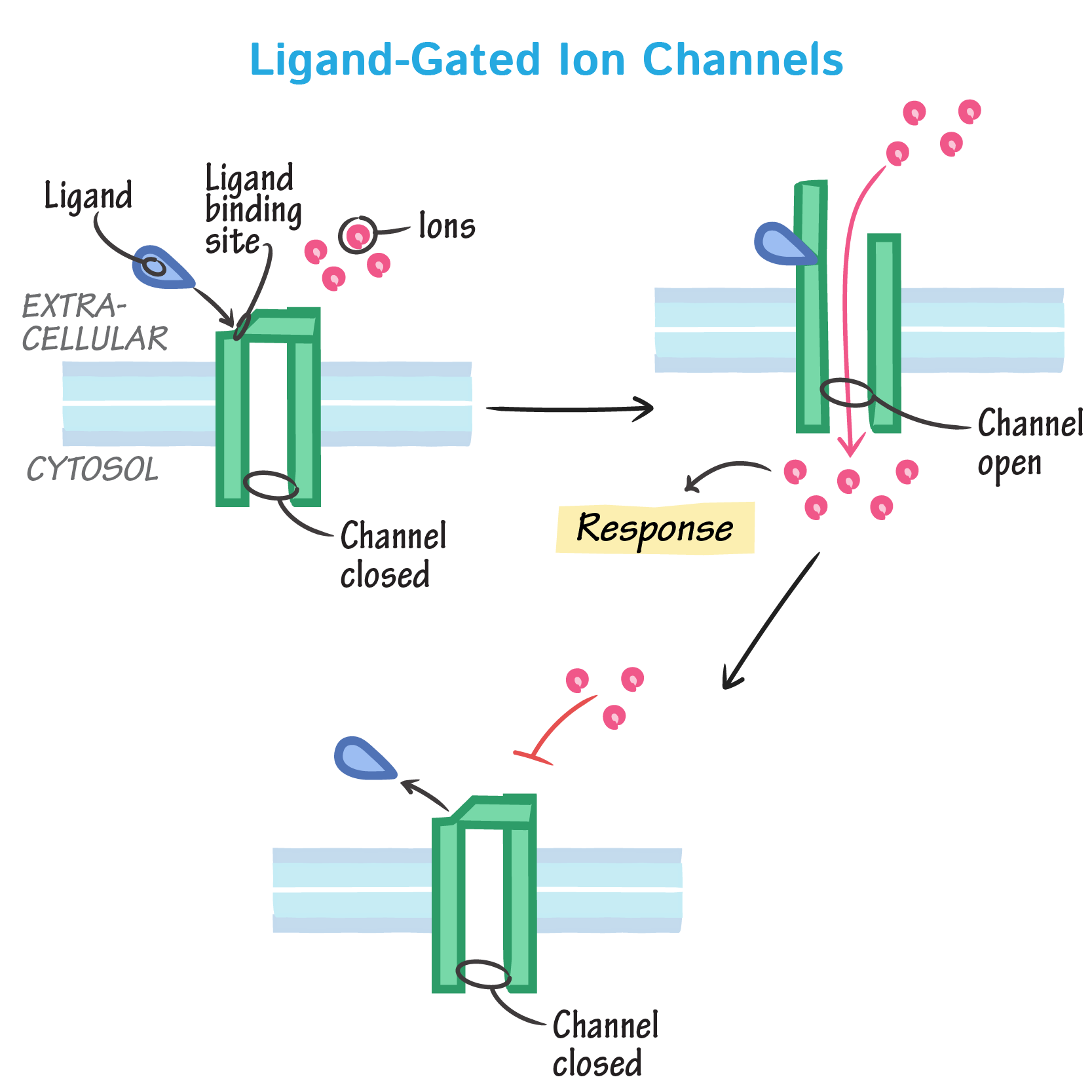
Ligand-Gated Channels
Ion channels that open or close in response to the binding of a specific ligand, such as neurotransmitters, hormones, or ions, to a receptor on the channel. These channels are essential for:
Chemical Synapses: Neurotransmitters bind to ligand-gated channels on the postsynaptic neuron, causing a change in membrane potential.
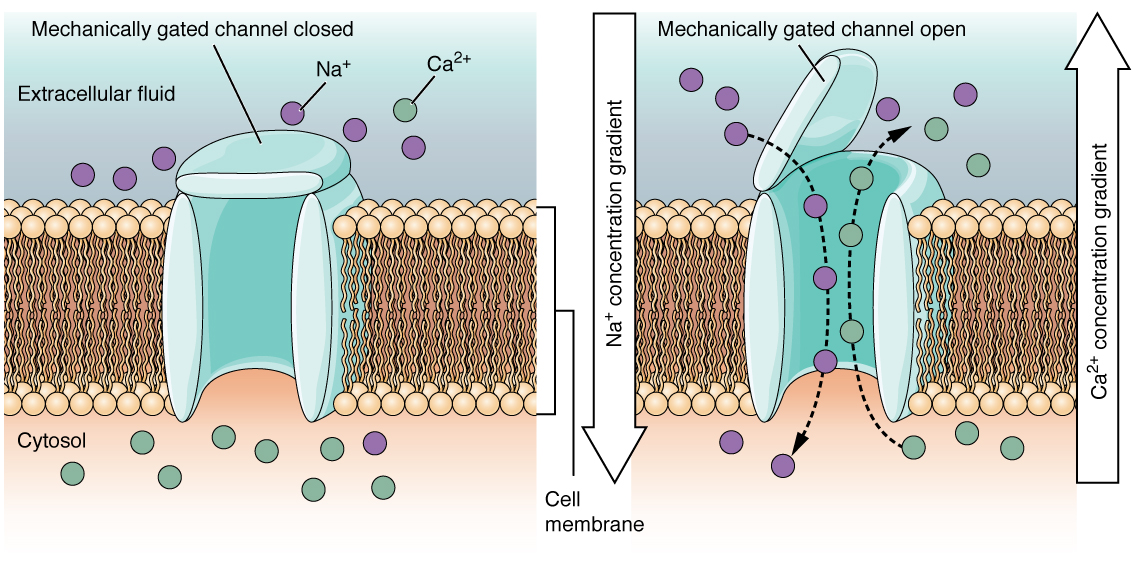
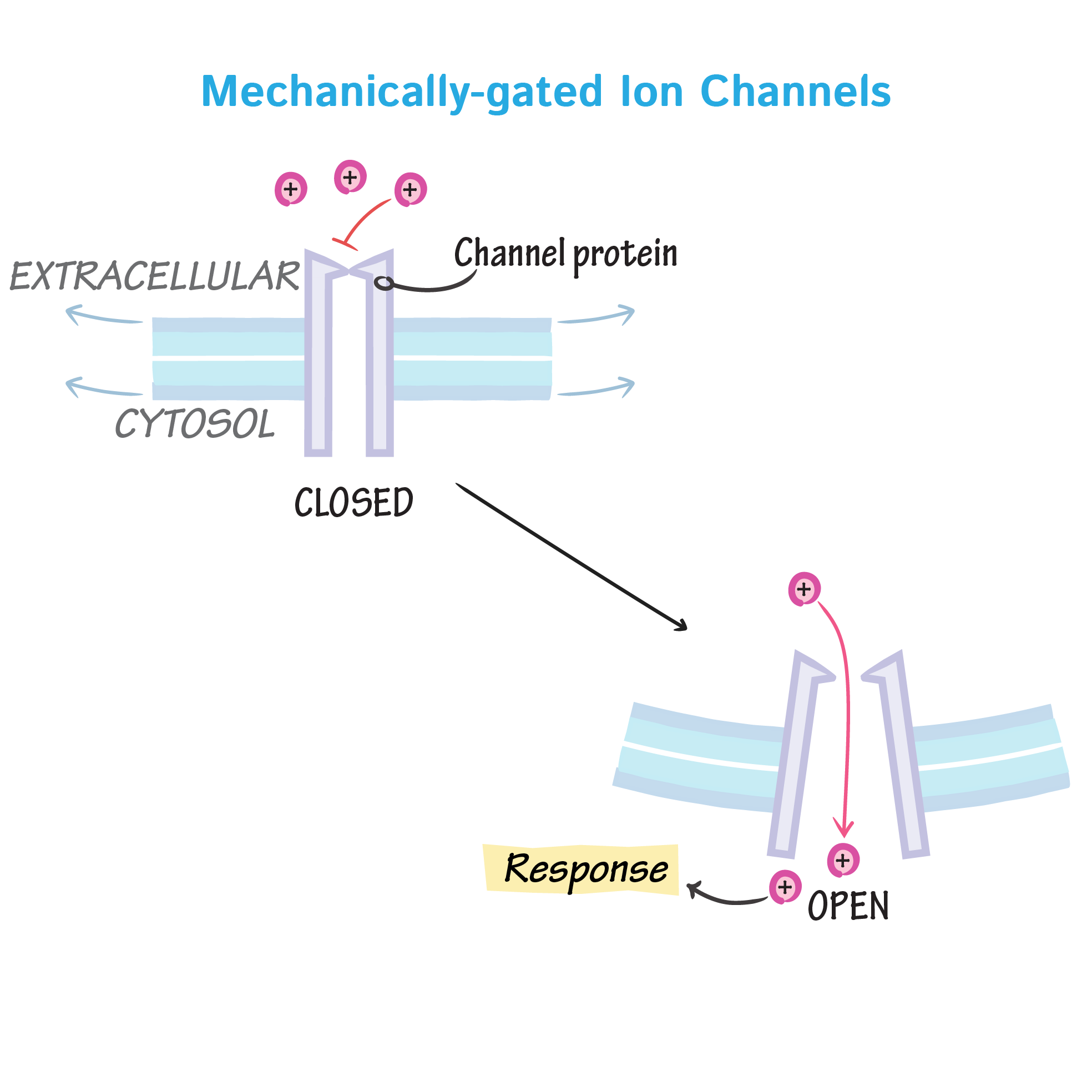
Mechanically-Gated Channels
Ion channels that open or close in response to mechanical stimuli, such as touch, pressure, vibration (in the form of sound waves), or tissue stretching. These channels are important in:
Sensory Transduction: Converting mechanical forces into electrical signals in sensory receptors.
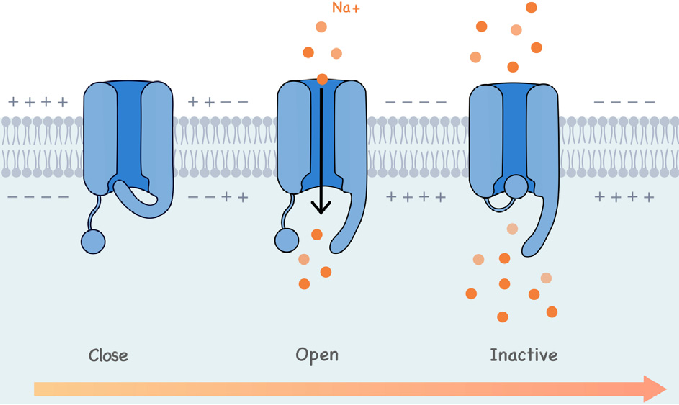
Voltage-Gated Channels
Ion channels that open or close in response to changes in membrane potential. These are crucial for generating action potentials:
Depolarization: When the membrane potential reaches a certain threshold, voltage-gated Na+ channels open, allowing Na+ to flow into the cell, causing further depolarization.
Repolarization: Voltage-gated K+ channels open, allowing K+ to flow out of the cell, restoring the resting membrane potential.
Polarized Cells
Any cell that has a membrane potential, meaning there is a difference in electrical charge across its membrane. Polarized cells maintain:
- Unequal distribution of ions: Contributing to the charge difference.
Membrane Potential Range
The range of possible values for the membrane potential of a cell, with the resting membrane potential typically between -40mV and -90mV (most commonly -70mV). The specific value of the membrane potential depends on:
- The type of cell.
- The distribution of ions across the membrane.
- The activity of ion channels and pumps.
Purpose of EPSPs
Excitatory postsynaptic potentials (EPSPs) are local depolarizations of the postsynaptic membrane. These:
Move the membrane potential towards the threshold for firing an action potential (AP), increasing the likelihood of the neuron firing.
ex. neurotransmitter binding opens Na+ channels
typically required to initiate an action potential
polarization
Purpose of IPSPs
Inhibitory postsynaptic potentials (IPSPs) are local hyperpolarizations of the postsynaptic membrane. These:
Move the membrane potential away from the threshold for firing an action potential (AP), effectively reducing the likelihood of the neuron firing.
hyperpolarization
cancel out EPSP
closing K+ gates
Summation
The process by which multiple synaptic potentials (EPSPs and IPSPs) combine at the axon hillock to affect the likelihood of a neuron firing an action potential. Summation can be either:
Spatial: Occurs when multiple presynaptic neurons release neurotransmitters simultaneously at different locations on the postsynaptic neuron.
Temporal: Occurs when a single presynaptic neuron releases neurotransmitters in rapid succession at the same location on the postsynaptic neuron.
typically simultaneous
Flow of Ions During an Action Potential
During an action potential, the rapid change in membrane potential activates voltage-gated channels:
- Voltage-gated K+ channels are slower to open compared to voltage-gated Na+ channels
- This sequential opening contributes to repolarization, as K+ efflux helps restore the negative membrane potential.
After-Hyperpolarizing Phase
A brief period following repolarization where the membrane potential becomes more negative than the resting membrane potential. This occurs because:
- K+ voltage-gated channels may not close right away, allowing excessive efflux of K+ and causing hyperpolarization.
Continuous Conduction
Action potential propagation that occurs:
In unmyelinated axons.
Is slower because it involves continuous movement of the action potential along the entire axon.
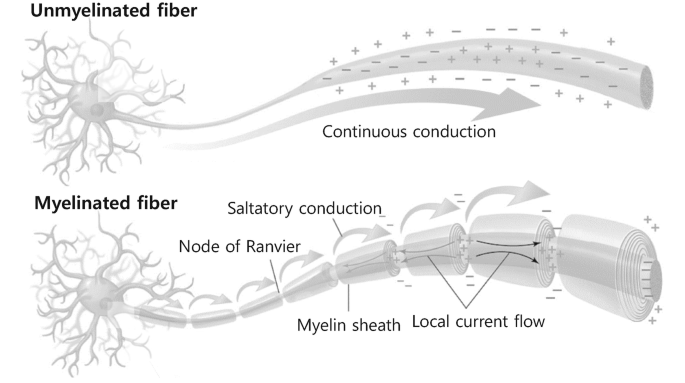
Saltatory Conduction
Action potential propagation that occurs:
- In myelinated axons.
- Is faster because the action potential 'jumps' along the axon between the myelin sheath gaps (Nodes of Ranvier).
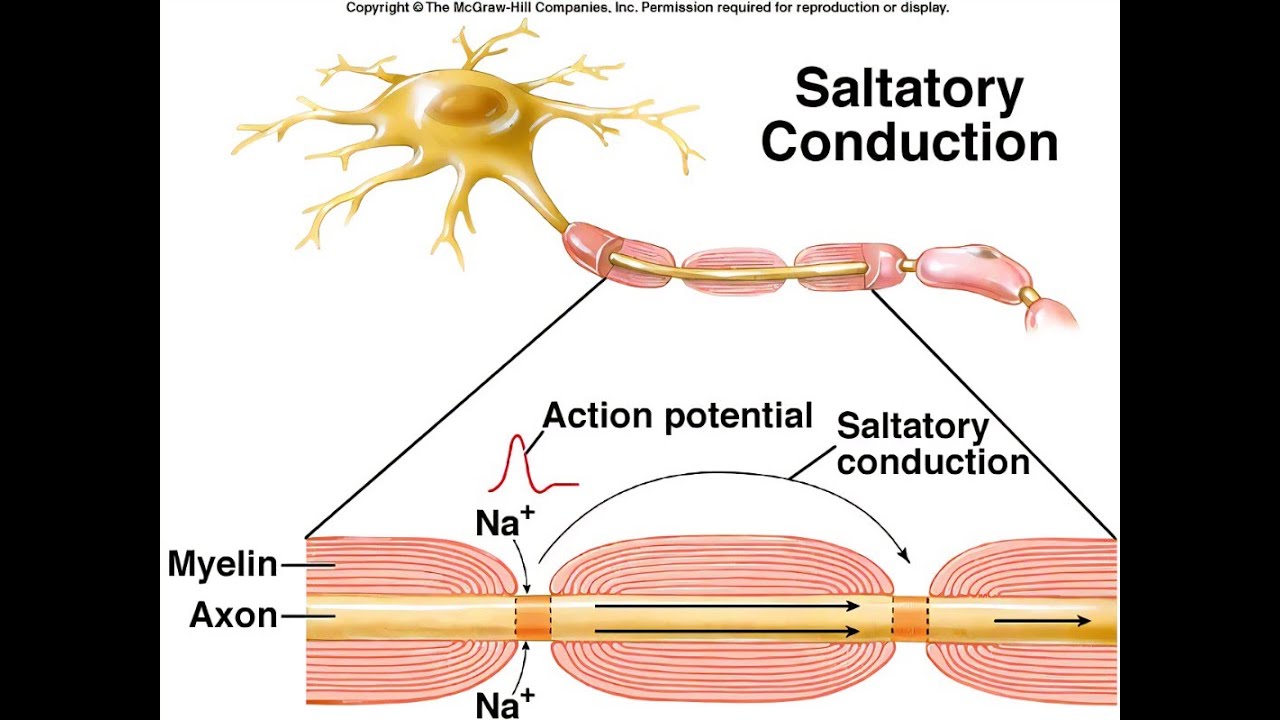
Energy Efficiency of Saltatory Conduction
Saltatory conduction is more energy efficient because:
- It involves fewer voltage-gated channels opening compared to continuous conduction.
- This reduces the energy needed to restore ion gradients across the membrane.
Na+ - K+ ATPase in Conduction
Less energy is expended by the Na+ - K+ ATPase to restore resting membrane potential during saltatory conduction compared to continuous conduction because:
- Fewer ions need to be moved across the membrane thanks to the reduced activity of voltage-gated channels.
AP Propagation Speed
The speed of action potential (AP) propagation is directly proportional to the axon's properties and environmental conditions:
- Quantity of Myelin: Increased myelin increases AP speed due to saltatory conduction.
- Diameter of the Axon: Larger diameter increases AP speed by reducing internal resistance to ion flow.
- Temperature: Higher temperature increases AP speed by enhancing ion diffusion and channel kinetics up to a certain point.
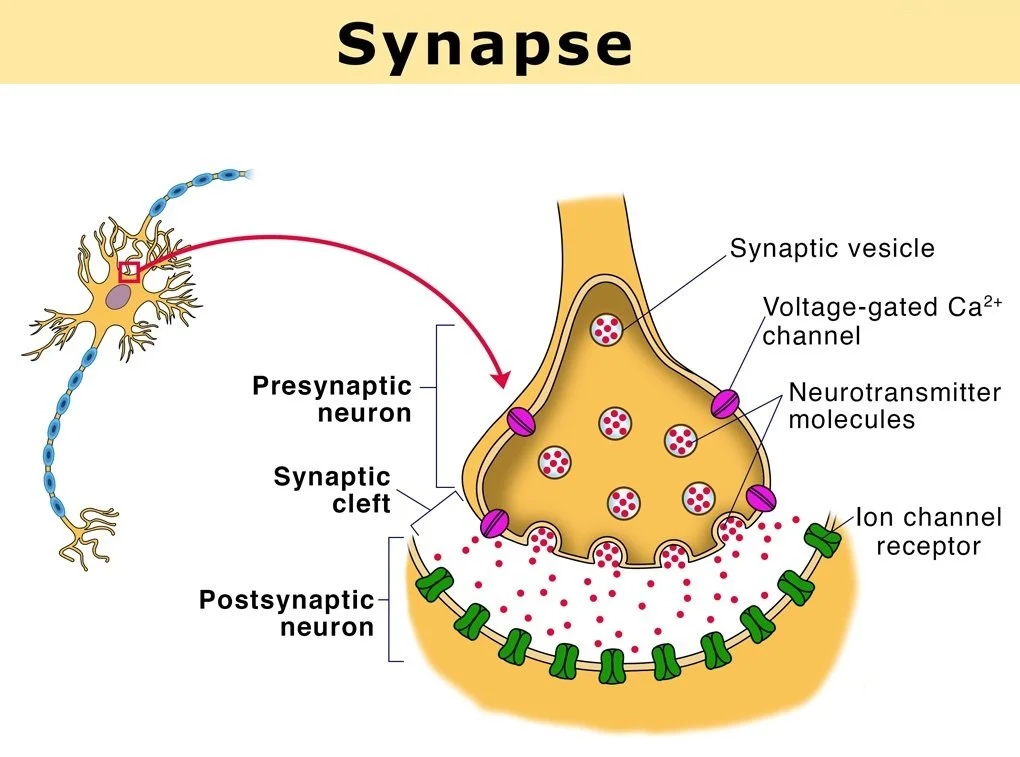
Synapse
The location where a neuron lies in close spatial proximity to another neuron or an effector cell (such as a muscle or gland) for the purpose of communication. Synapses enable:
- The transmission of electrical or chemical signals between cells, facilitating neural communication.
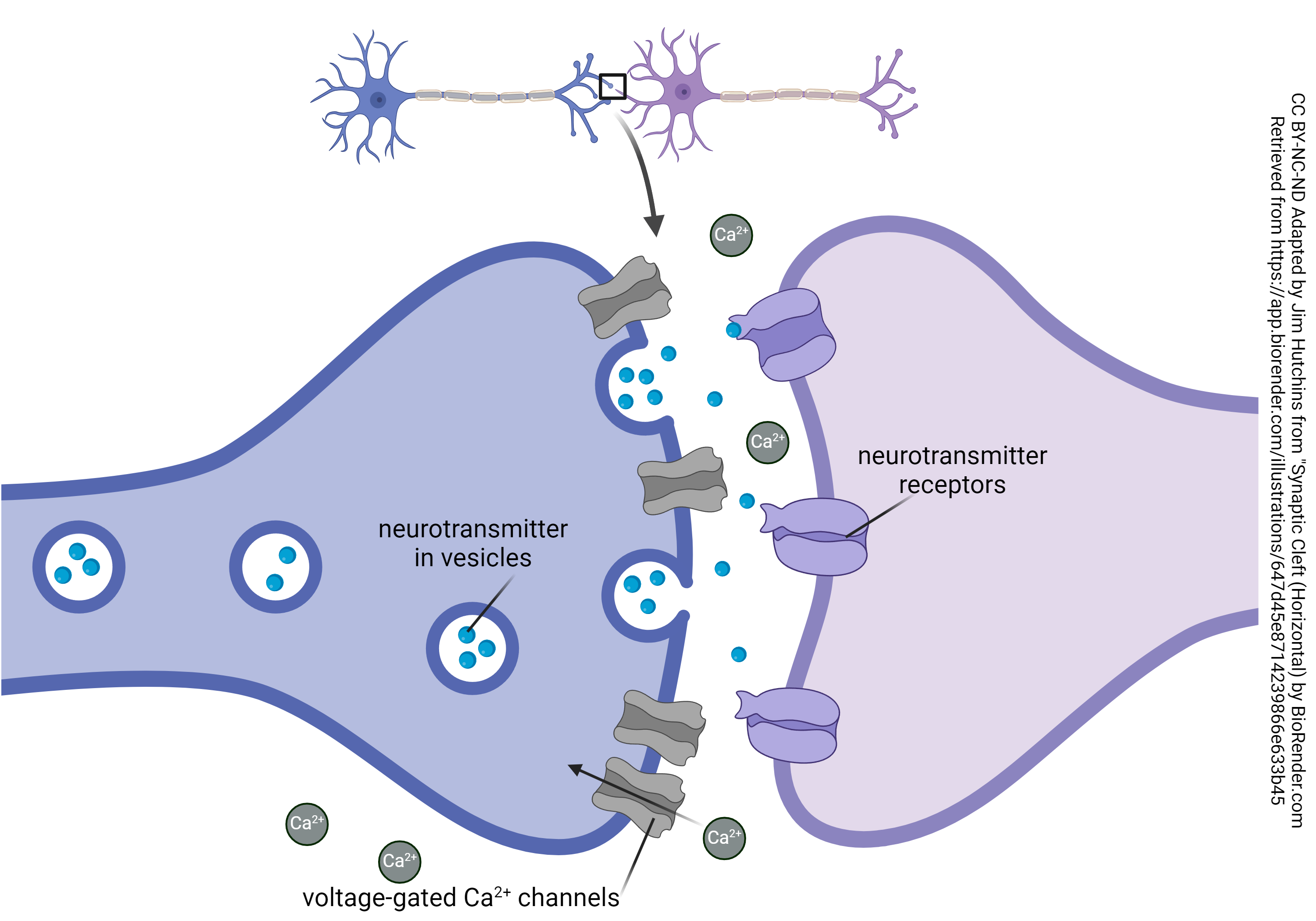
Order of Communication in a Synapse
The typical flow of information in a synapse:
- 1. Presynaptic neuron
- The neuron sending the signal.
2. Synapse
The junction between two neurons (or a neuron and an effector cell).
3. Postsynaptic cell
The neuron or effector cell receiving the signal.
Electrical Synapse
A type of synapse where the action potential (AP):
- Moves through gap junctions that connect adjacent cells.
- Allows the direct flow of ions from the presynaptic neuron into the postsynaptic cell, enabling rapid and synchronized communication.
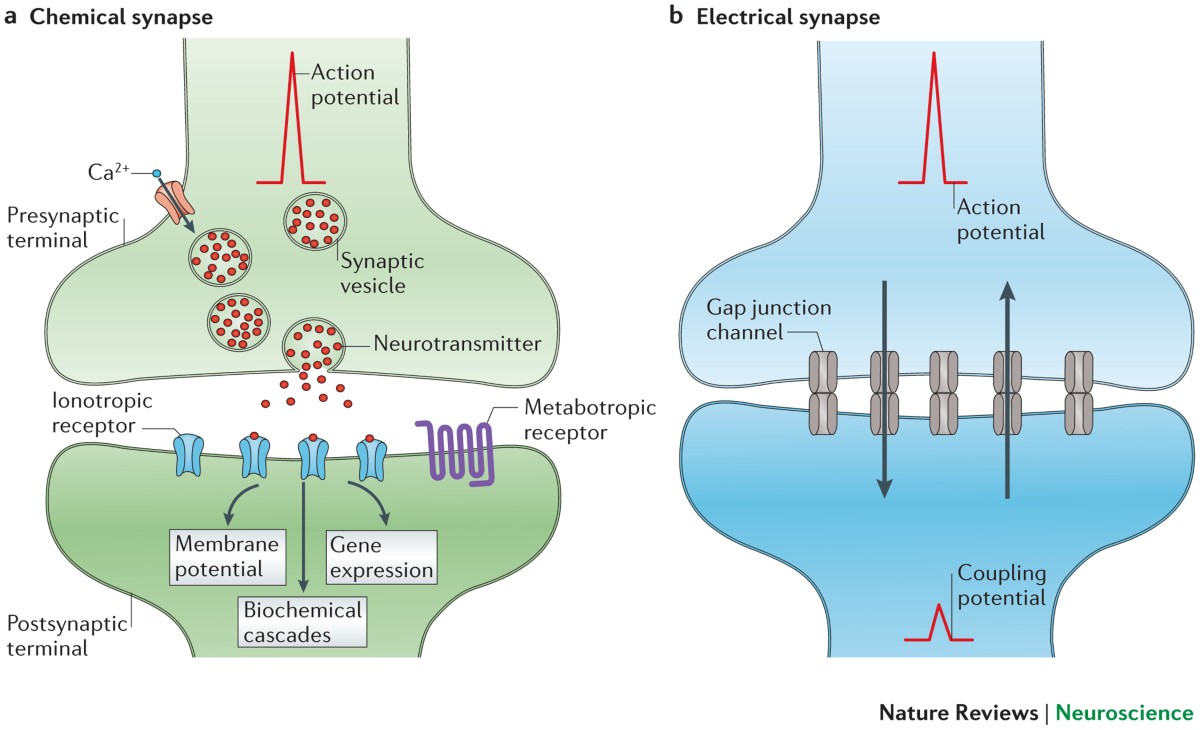
Common Locations for Electrical Synapses
Cardiac muscle, visceral smooth muscle, the brain, and embryos are common locations for electrical synapses. These locations benefit from:
- Rapid and synchronized communication to coordinate cellular activity.
Function of Electrical Synapses
Electrical synapses increase:
- The speed of signal transmission and communication between cells due to the direct ion flow through gap junctions.
- They produce synchronized/coordinated action potentials across many cells at once, facilitating coordinated activity.
Chemical Synapse
A type of synapse where the action potential (AP):
Is communicated between cells through the release of neurotransmitters from the presynaptic cell into the synaptic cleft.
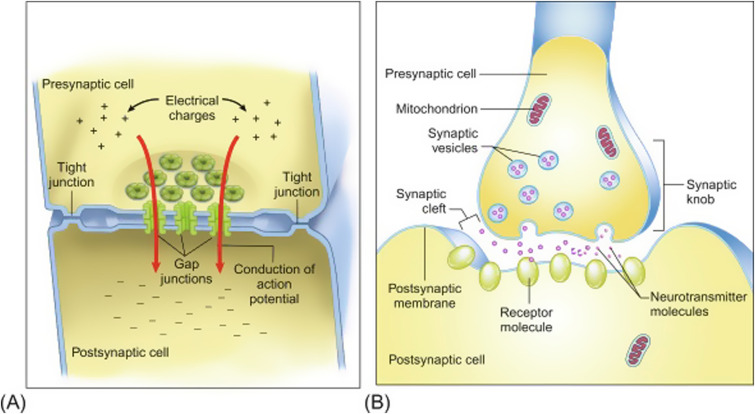
Neurotransmitter Function in Chemical Synapse
Neurotransmitters:
- Bind onto receptors on the postsynaptic cell membrane creating a postsynaptic potential (PSP)
- May trigger an action potential (AP) if the threshold is reached.
Spatial Summation
A type of summation that typically occurs when:
- Multiple presynaptic neurons release neurotransmitters simultaneously at different locations on the postsynaptic neuron.
- This is done so their effects are combined.
Temporal Summation
A type of summation that occurs when:
- A single presynaptic neuron releases neurotransmitters in rapid succession at the same location on the postsynaptic neuron.
- This is done so their effects are combined over time.
Summation of Postsynaptic Potentials
The combined effect of excitatory postsynaptic potentials (EPSPs) and inhibitory postsynaptic potentials (IPSPs) on the postsynaptic neuron:
- Determines whether or not it will fire an action potential. If the sum of EPSPs is strong enough to reach