Drug distribution ( Pharmacokinetics)
1/21
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
Define Pharmacokinetics vs Pharmacodynamics
Pharmacokinetics :effect of the body on the drug
Pharmacodynamic: effect of the drug on the body
Types of Pharmacokinetics
Drug absorption (administration)
Drug distribution
Drug metabolism
Drug excretion
Where are drugs are distributed first
Drugs are rapidly distributed to blood rich organs (heart, liver, kidney, brain)
then to muscles fat skin (which have poor blood supply)
Which drugs have selective accumulation in certain tissue
Iodide → thyroid tissue
Tetracyclines → bone
Chloroquine → eye, liver
Some body areas (eg brain) protected from drugs → special barrier (eg BBB)
The use of drug redistribution
Termination of action of some drugs
Drug redistributed from action site to other tissues where still active but not produce any action
How is Thiopental used in drug redistribution
IV injection acts on CNS → Anesthesia →Redistributed from CNS to storage sites in muscles & fat → action termination within 10-15 mins.
Thiopental characteristics
Ultrashort
active
Highly lipid soluble Barbiturate
Repeated injection Thiopental leads to
Repeated Thiopental injection (eg: 3/4)
→ storage site saturation→ ↑plasma conc → Return again to CNS → prolonged action (termination of action depends on metabolism and excretion)
2 characteristic of plasma protein bound drugs
Inactive (no diffuse from vasc space = no effect produced , metabolised or excretion)
acts as a reservoir (when free drug conc ↓ by metabolism or excretion unbounding occurs = Reversible)
Binding in plasma protein binding
non selective and competition of many drugs/subst for same binding site leads to ↑ free form of one drug
Sulfonamide vs bilirubin
Sulfonamides displace bilirubin from albumin binding → ↑.free bilirubin → ↑ risk of bilirubin encephalopathy/ Kernicterus in neonates
If there is high plasma protein binding and example
Bolus injection (Very rapid IV)
Eg: diazoxide in hypertension
If there is decrease in plasma proteins (hypoproteinemia) due to liver/renal disease or malnutrition
Reduce drug dose of drugs with high plasma protein binding
Eg: Warafrin
Example of tissue protein binding replacement
Quinidine displaces digoxin from plasma protein and tissue protein binding & ↓ renal excretion of digoxin —> ↑ free digoxin —> precipitate digoxin toxicity
Volume of distribution meaning
Apparent vol req to contain all drug in body at same conc as in plasma provided body acts as single homogenous compartment for drug.
Volume of distribution formula
Vd = amount drug given to body / Plasma conc
(after distribution equilibrium (0.5-1 hr))
What does High Volume distribution mean
High Vd as plasma conc is low means most drug distributed to diff organs in high conc
Factors affecting Vd (Favouring)
Highly unionized
Highly lipid soluble
Low binding to plasma protein
Highly binding to tissue protein
= High Vd
Drugs with high Vd vs low Vd on haemodialysis
Drugs with high Vd (eg:digoxin) if toxicity occur no adv of haemodialysis to remove drug as plasma level low and most of drug conc in tissue
Drugs with low Vd (eg: aspirin) in case of toxicity haemodialysis remove most drug as it is conc in blood.
Why does drugs with high Vd have minimal fluctuations in blood conc
high Vd drugs minimum fluctuations in blood conc as tissues act as reservoir for the drug and provide the blood by the drug when its concentration in the blood ↓.
Define steady state concentration (Css)
Rate of drug elimination = Rate of administration
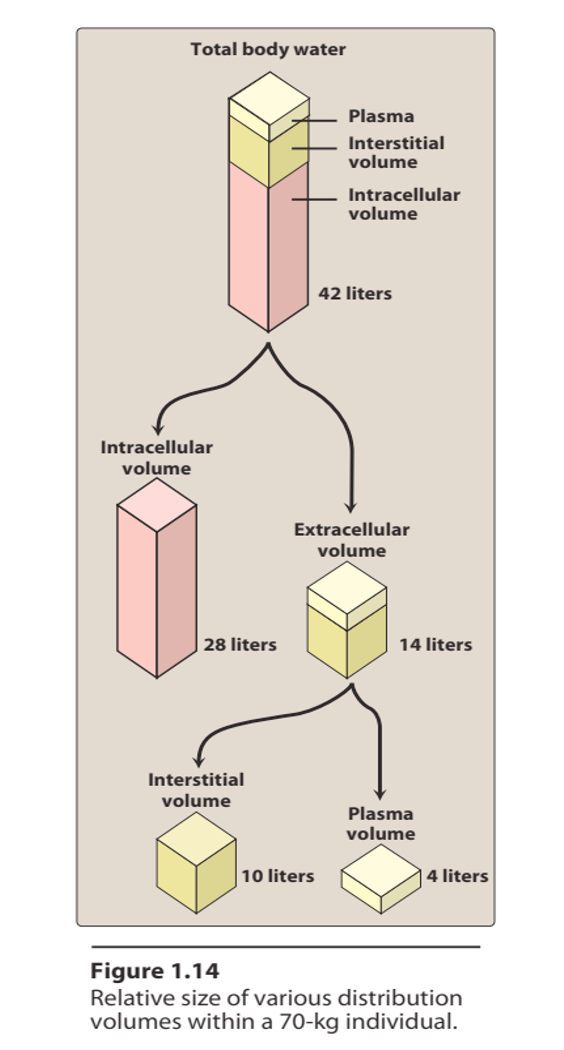
Site of distribution Compartment theory levels
Vd 3-5 = Plasma
Vd 5-15 = Interstitial
Vd 20+ = Intracellular