Ocular Physiology Flashcards
1/1144
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
1145 Terms
What are the functions of the Eyelid?
Provides oxygen to tear film in closed eyes (sleeping)
Globe Protection
Spread Tears
Assists in Tear Drainage
Produce Tear Film Components
What are the muscles of the palpebrae?
Orbicularis Oculi
Orbital Portion
Palpebral Portion
Horner’s
Riolan’s
Levator
Tarsal Muscles
Superior
Inferior
What Ligament is found in the palpebrae?
Whitnall’s Ligament
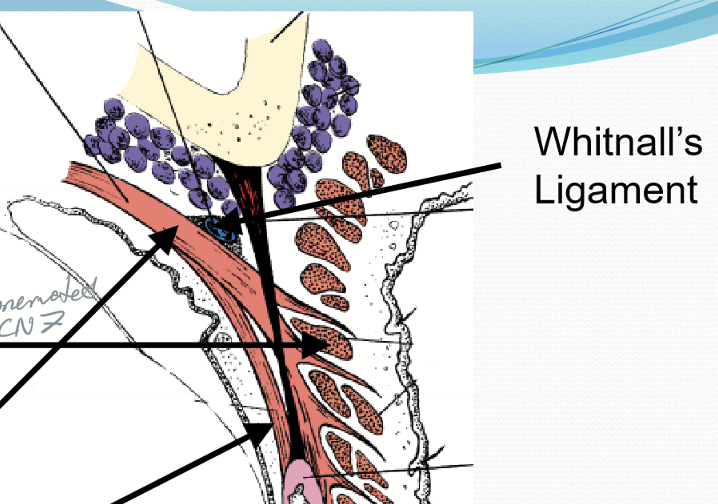
What nerve innervates the Orbicularis Oculi?
CN VII
What nerve innervates Horner’s Muscle?
CN VII
What nerve innervates Riolan’s Muscle?
CN VII
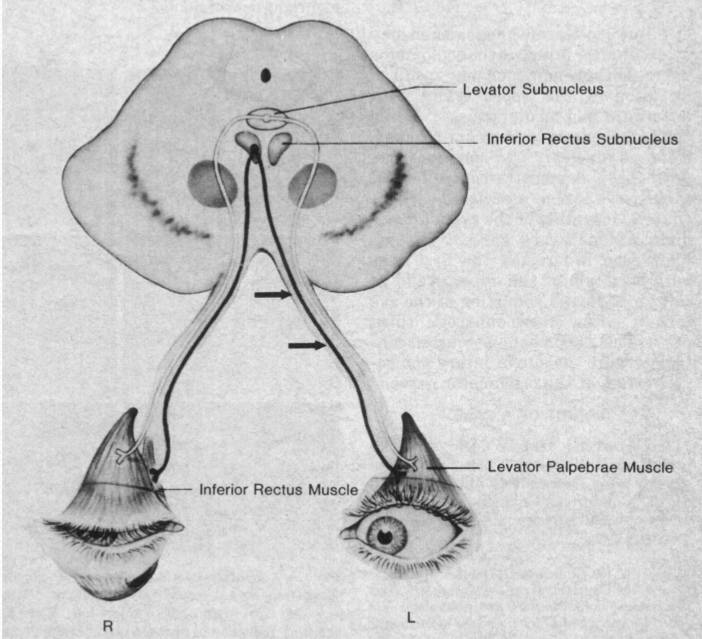
What nerve innervates the Levator Palpebrae Superioris
CN III
What nerve innervates the Tarsal Muscles (Muller’s)
Sympathetic Nervous System
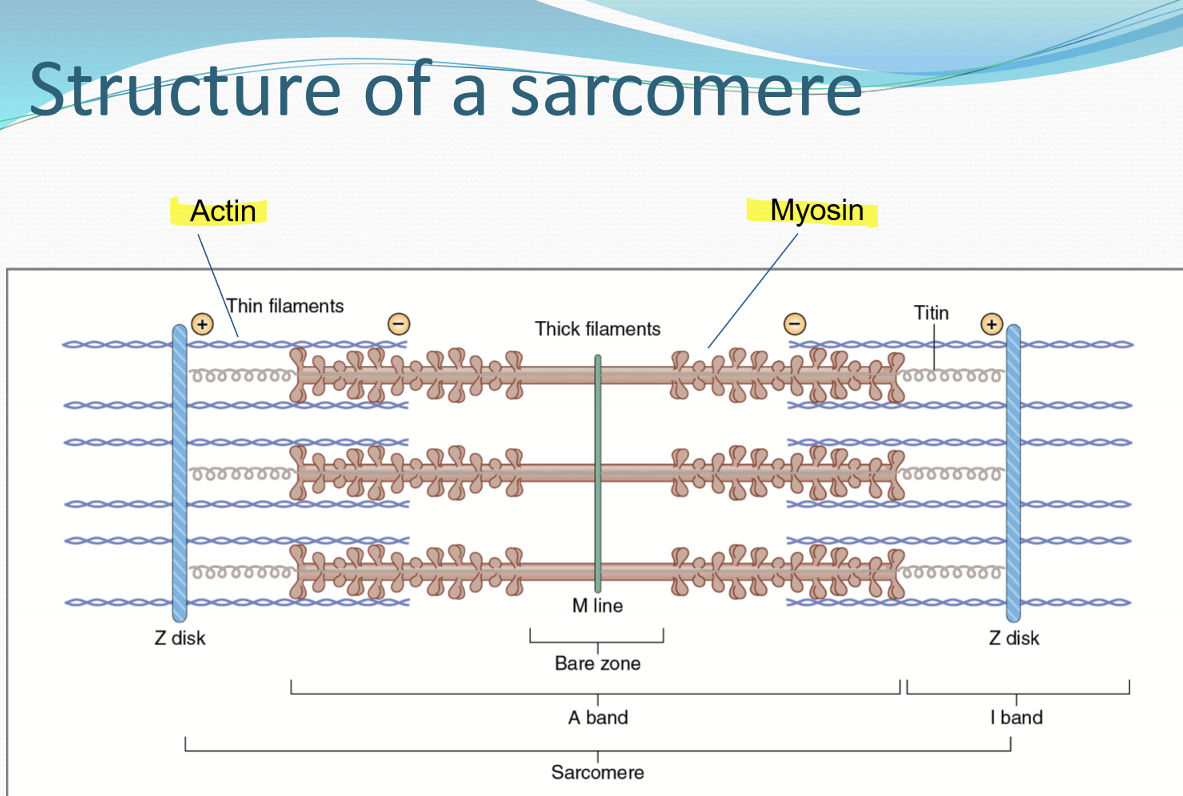
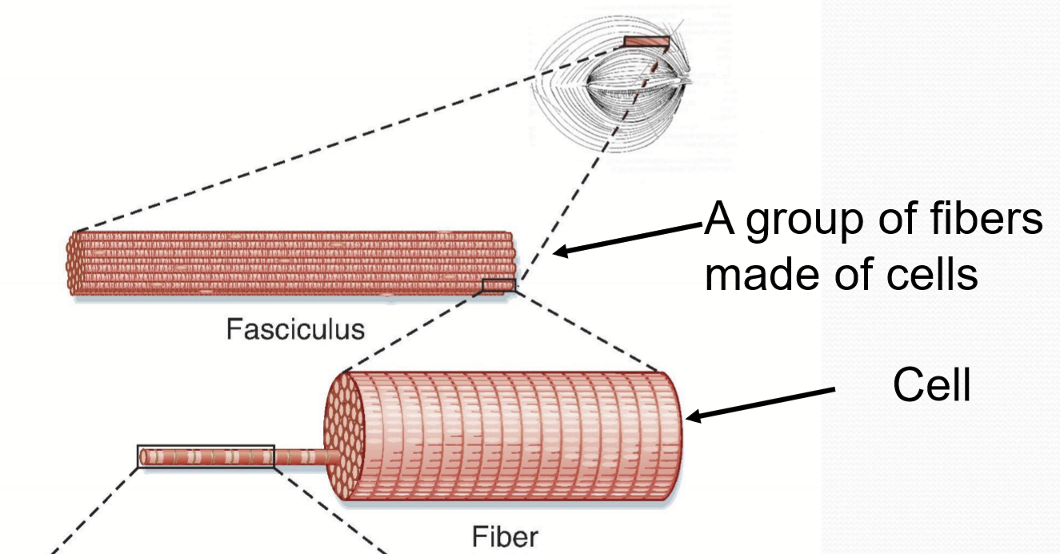
What are the major structure of a sarcomere?
Actin and Myosin
What are the units that make up a myofibril?
Sarcomere
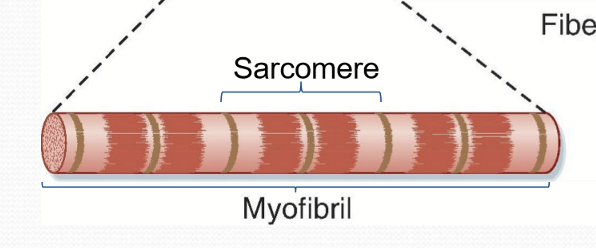
What do a bundle of myofibrils form?
A muscle fiber (a cell)
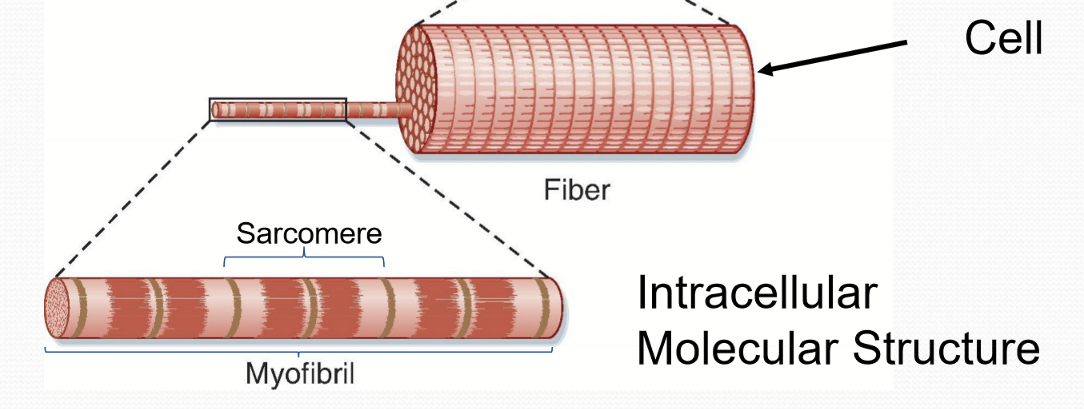
What do muscle fibers form?
Fasciculus
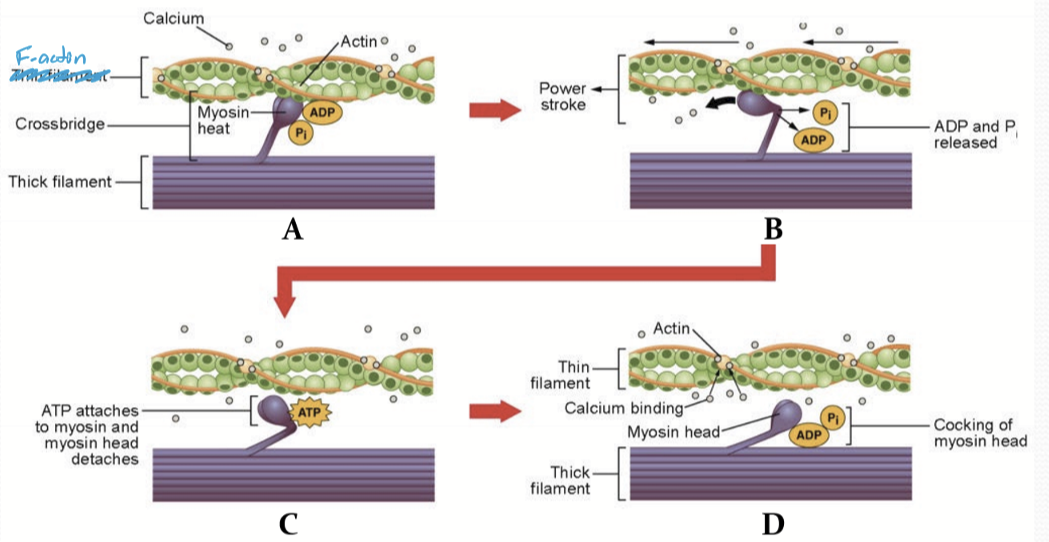
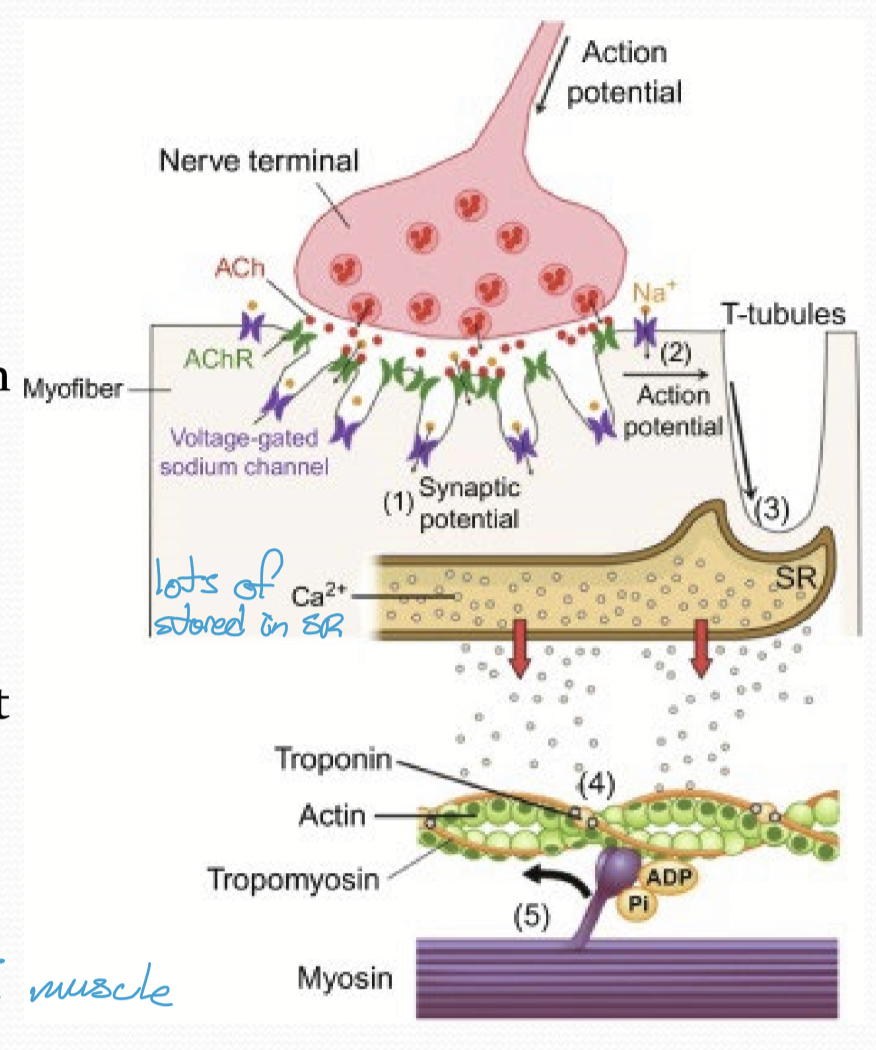
How does Sarcomere contract?
Myosin head associates with F-actin
The release of ADP/P induces myosin head to move/power stroke
Myosin head attaches to to ATP and releases F-actin (has ATPase to hydrolyze ATP)
ATP is hydrolyzed to ADP/P causing myosin head to bend backward, storing potential energy
How are skeletal muscle fibers categorized?
Speed of contraction
How ATP is generated
What types of skeletal muscles are there?
Type I, Type II a, Type II x
(Type II b is found in animals and is different)
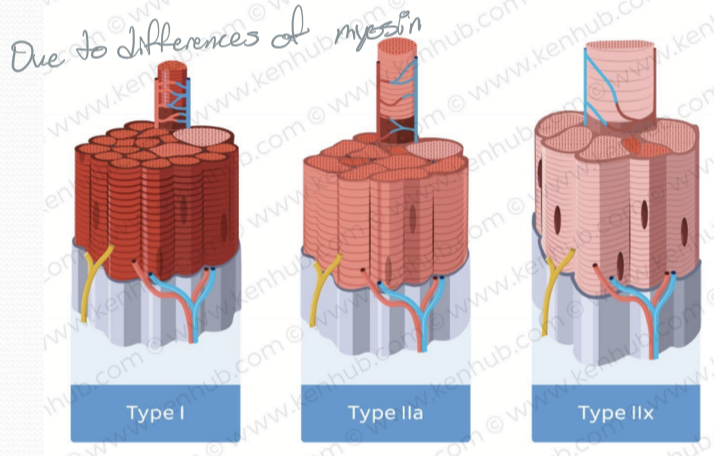
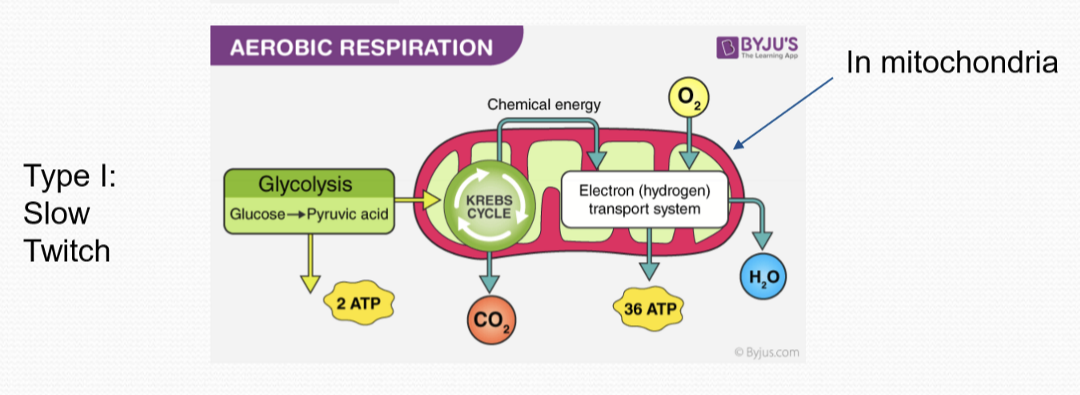
What are the characteristics of Type I muscles?
Slow twitch/slow oxidative
Slow Myosin ATPase activity
Higher capillary density
More Mitochondria
Utilize Aerobic Respiration > > > Anaerobic glycolysis
Slow to fatigue
What are the characteristics of Type II a muscles?
Fast twitch/fast oxidative
Fast Myosin ATPase activity
Lower capillary density than type I
Fewer mitochondria
Aerobic Respiration > anaerobic glycolysis
Fatigues faster than type I
What are the characteristics of Type II x muscles?
Fast twitch/fast glycotic
Fast myosin ATPase activity
Lowest capillary density
Fewest mitochondria
Anaerobic glycolysis > > > Aerobic Respiration
Fatigue fastest
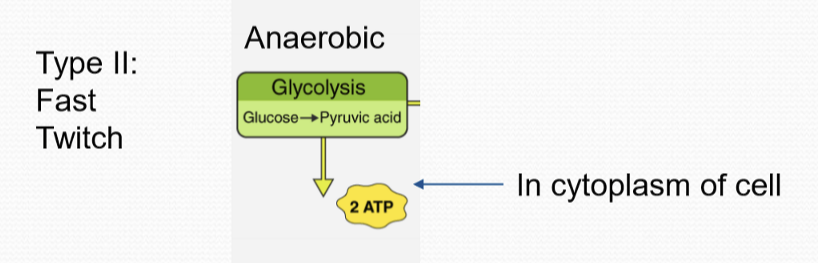
How does Anaerobic metabolism work?
Glucose is converted into pyruvic acid via glycolysis
How does Aerobic metabolism work?
Glucose is converted into pyruvic acid via glycolysis, which then undergoes the kreb cycle and ETC in the mitochondria.
What type of fibers does the Orbicularis Oculi have?
Type II > > > Type I
What type of fibers does the Levator (LPS) have?
Type II > > > Type I; is unique because it is resistant to fatigue
What is Type I fibers used for in Orbicularis Oculi?
It is for sustained closure
What is Type I fibers used for in the Levator m?
Sustained elevation of eyelids
What is Type II fibers used for in Orbicularis Oculi?
Rapid closure of palpebral
What is Type II fibers used for in Levator m?
Elevation during blinking
What is released between a neuromuscular junction?
Neurotransmitter; typically Acetylcholine/ACh, secreted from Synaptic Vesicles.
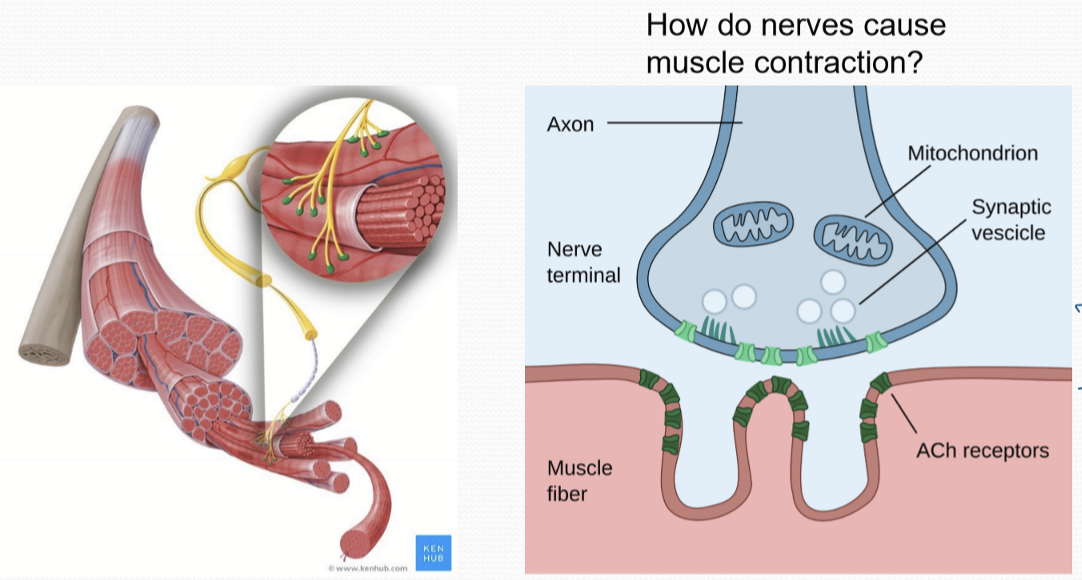
What does ACh do in the neuromuscular junction and muscle to cause contraction?
ACh binds to ACh receptors on the muscle cell, triggering the opening of ion channels.
Action potential is generated within the muscle cell within the T-tubules
The sarcoplasmic reticulum is triggered to release large amounts of calcium
Calcium binds to Troponin causing it to disassociate with F-actin
Troponin removal allows myosin to bind to actin and sarcomere contraction
What issues arise from faulty palpebral muscles?
Ptosis: drooping of superior eyelid
Diplopia: condition where a person sees two images of a single object
Peek sign: ocular surface uncovered following sustained closure
Issues with what muscle would cause Ptosis?
LPS, Muller muscle/tarsal muscle
Issues with what muscle would cause Diplopia?
EOM
Issues with what muscle would cause Peek sign?
Orbicularis Oculi
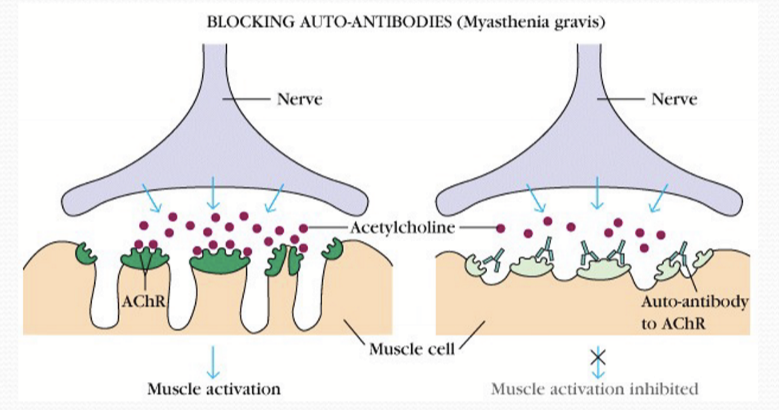
What is Ocular Myasthenia Gravis, and what are its symptoms?
An autoimmune neuromuscular junction (NMJ) disorder with unknown cause. Symptoms: weakness in eye muscles can lead to double vision, drooping eyelids, and difficulty focusing.
What causes Ocular Myasthenia Gravis?
Impaired NMJ commonly due to presence of antibodies binding to AChR of muscle cells in synaptic cleft, block ACh, and prevent receiving muscle cell from propagating signal
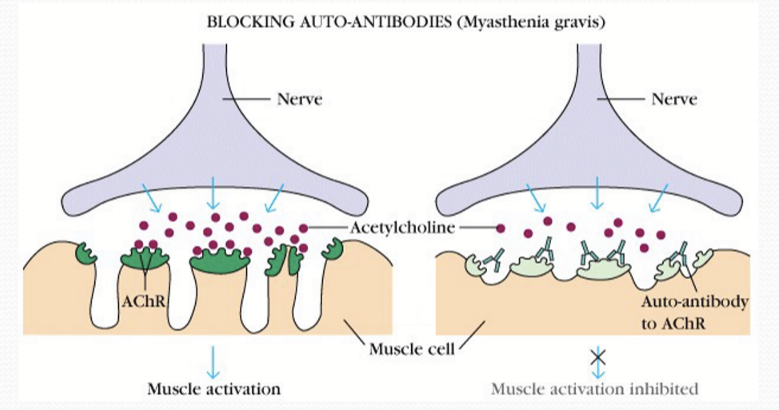
What type of muscles are more susceptible to Ocular Myasthenia Gravis
Type II Ocular Muscles
Why are fast twitch muscles more susceptible to Myasthenia Gravis?
The fast twitch muscles require repeated nervous stimulation, therefore they are more susceptible
Patients with Ocular Myasthenia Gravis will develop what issue later?
Systemic muscle weakness within 2 years, becoming Generalized Myasthenia Gravis.
What Muscles can Generalized Myasthenia Gravis affect?
Any skeletal muscles; seen as limb weakness, dysphagia, slurred speech, respiratory muscles.
How many patients with Ocular Myasthenia Gravis get Generalized Myasthenia Gravis
2/3 patients
What ages do males get more susceptible for OMG?
60-80 yrs
What ages do females get more susceptible for OMG?
23-30 and 60-80 yrs
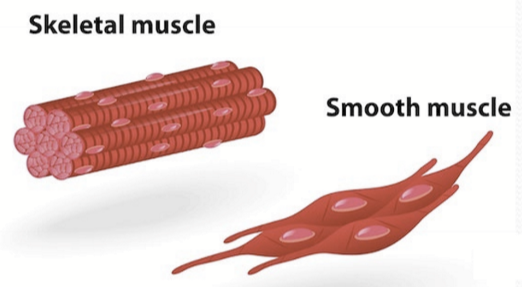
What type of muscles are Muller’s Muscles/Tarsal Muscles
Smooth Muscle
What innervates Muller’s Muscle/Tarsal muscles
Sympathetic Innervation
Features/characteristics of skeletal muscles
Striated
Multinuclear
Voluntary Movement
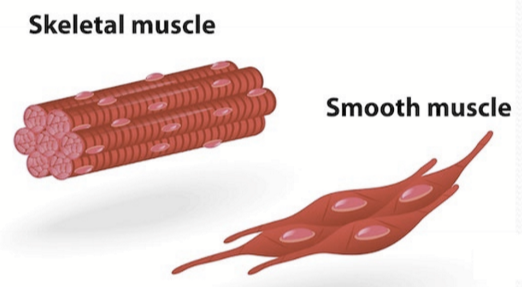
Features/characteristics of Smooth Muscles
Not striated
Single nucleus
Involuntary
Net-like structure
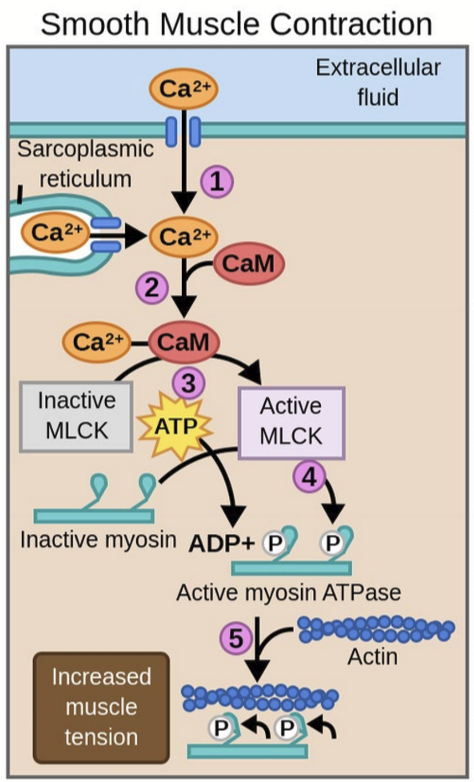
Steps for Smooth Muscle Contraction
Influx of calcium triggers more calcium release from SR
Calcium binds to Calmodulin
Ca-CaM activates myosin light chain kinase (MLCK)
MLCK activates myosin
Myosin contracts and pulls on actin
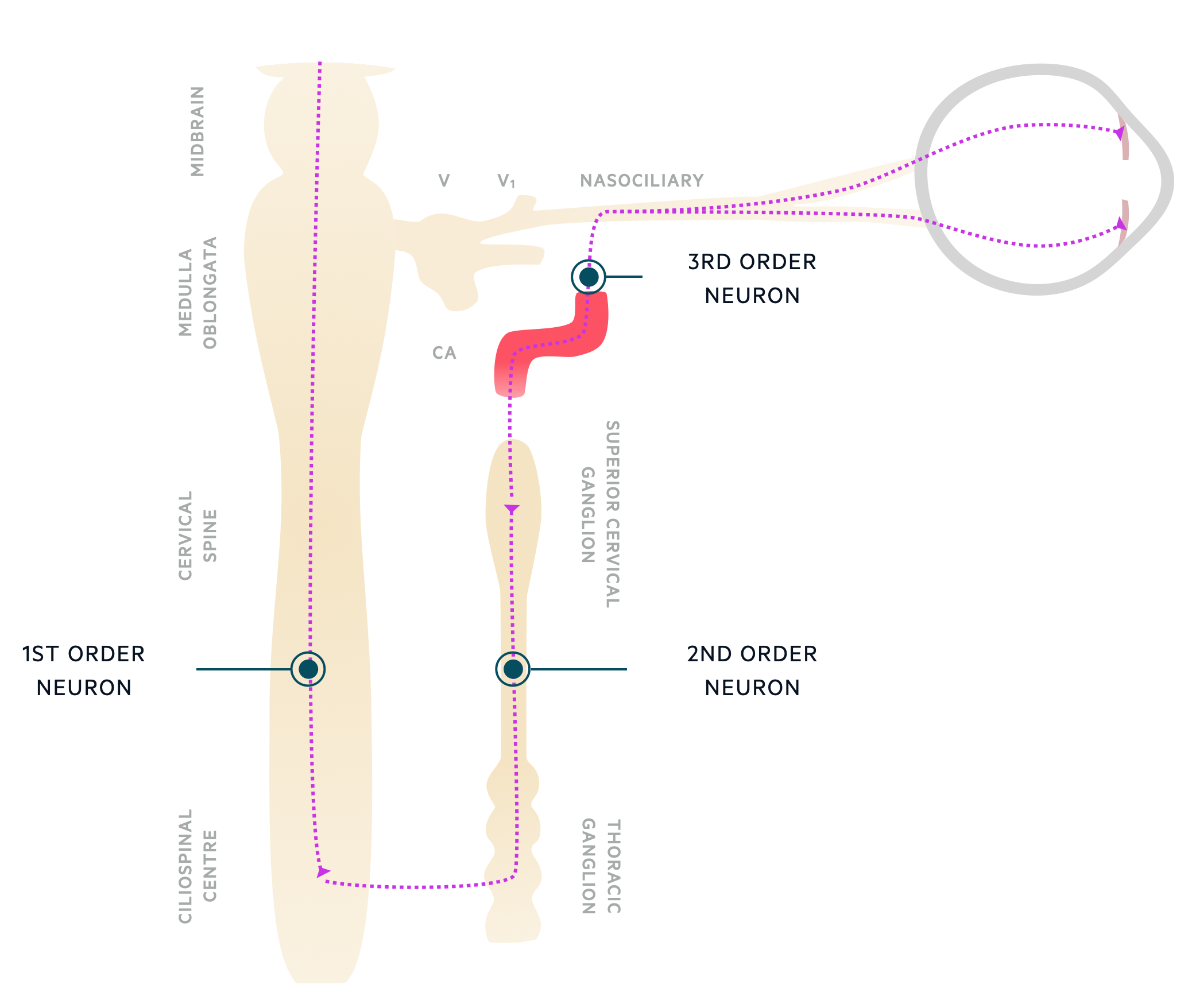
What is Horner’s Syndrome
A neurological condition caused by disruption of the sympathetic nerves supplying the eye and surrounding structures

Symptoms of Horner’s Syndrome
Ptosis: Muller muscle is inhibited, causing dropping of the upper eyelid
Miosis: constricted pupil d/t unopposed action of the parasympathetic system
Facial Anhidrosis: decreased or absent sweating depending on nerve damage
Enophthalmos: eye may appear sunken
Orders of Horner’s Syndrome
First Order: lesion before the hypothalamus and Superior Cervical Ganglion (SCG)
Second Order: lesion after the hypothalamus, but before the SCG
Third Order: lesion after the hypothalamus and SCG
What are the types of palpebral motions?
voluntary blink/closure
spontaneous blink to protect
reflexive blink from drying tear film sensed by a decrease in temperature
coordination with EOM
How do the parts of the eyelids move during a blink?
Nasal angle remains immobile
Temporal angle moves nasally and downward
Upper lid moves down and medially
Lower lid moves mostly medially
What does the LPS do during the down-phase of a blink?
It relaxes to allow the closing of the eyelids
What does the LPS do during the up-phase of a blink?
It contracts
Why do blinks close faster than they open?
Whitnall’s Ligament/Canthal Tendons lower superior palpebral AND population of fiber cell types differ between muscles
List the order of events that occur duing a blink
Baseline levator motorneuron firing ceases
LPS muslces relax
Passive downward force of canthal tendons lowers superior palpebrae
Orbicularis motoneuron firing begins causing further palpebral closure
Orbicularis motorneuron firing and muscle activity ceases
LPS motorneuron resume firing at baseline tonal rate, reopnening the palpebral aperature and re-stretching canthal tendons
Characteristics of spontaneous blink
multiple times per minute
duration is ¼ second
synchronous
amplitude varies
What increase blink rate?
decreased humidity
contact lens use
older age
speaking
emotional states
birth control medication
What decreases blink rate ?
increased humidity
younger age
during sustained visual tracking
reading
daydreaming
downward gaze
Dopamine’s affects on spontaneous blink rate
dopamine is a neurotransmitter, drugs that stimulate dopaminergic nerves increases SBR; drugs that inhibit dopaminergic nerves reduce SBR
How does Parkinson’s disease affects on SBR?
It decreases dopamine release, thus is associated with decreased SBR
How does Schizophrenia affect SBR?
It increases dopamine release; associated with increase in SBR
Which way does the eye move during a reflexive/spontaneous blink?
In primary gaze, it rotates downward and nasalward
In large saccade movements, what typically happens?
a blink
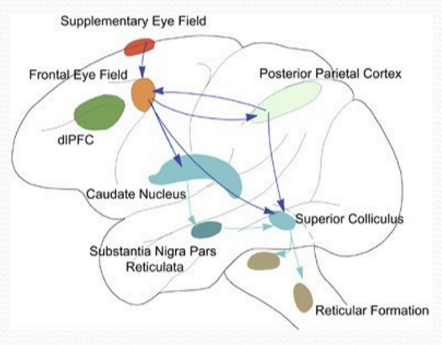
What controls the saccade (rapid simultaneous movement of both eyes in the same direction from one point of fixation to another)
Saccade is controled by the Frontal Eye Fields (FEF) and superior colliculus
What is Bell’s Phenomenon
Upward and outward (abducting) rotation of the eyes on prolonged bilateral closure or attempted closure
What is visual suppression?
The brain’s ability to temporarily ignore visual input during saccades or blinks
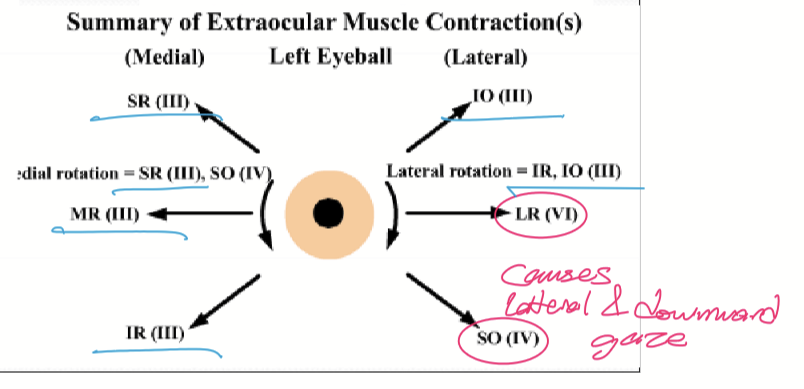
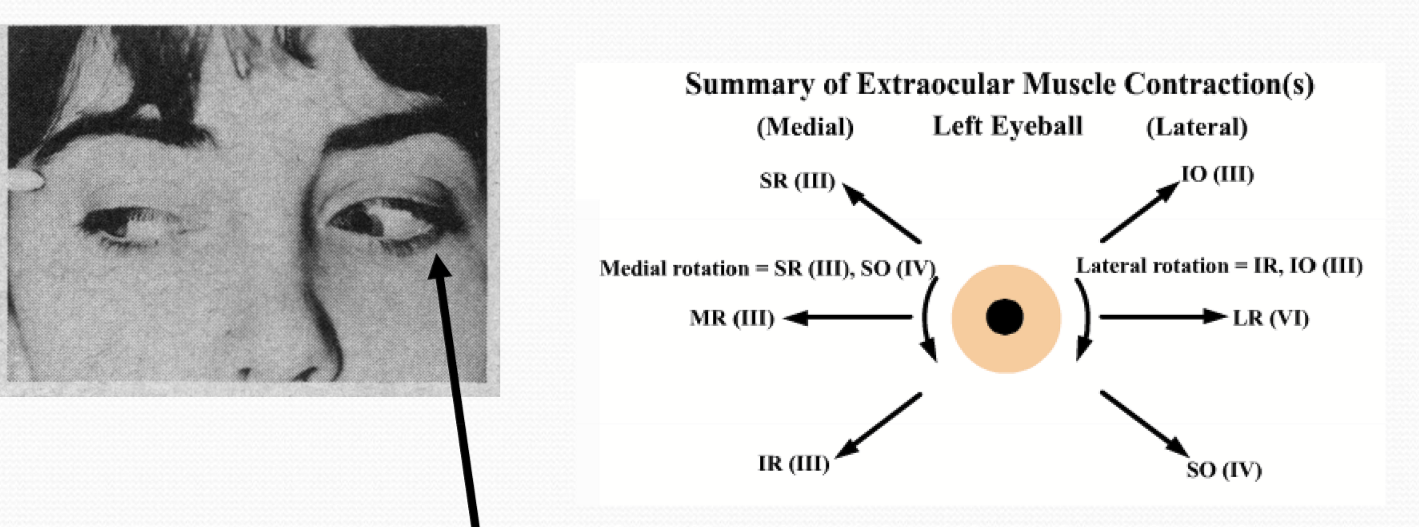
Where does a patient’s eye look when they have ptosis?
Their eye looks downward and lateral. CN III is damaged, so the IR, SR, MR, and IO don’t work, but CN VI does, so the LR and SO still work.
Marcus Gunn Jaw Winking Phenomenon
Chewing/sucking motions occur with eyelid motions because pterygoid muscle CN V linked to levator CN III; ptosis at rest
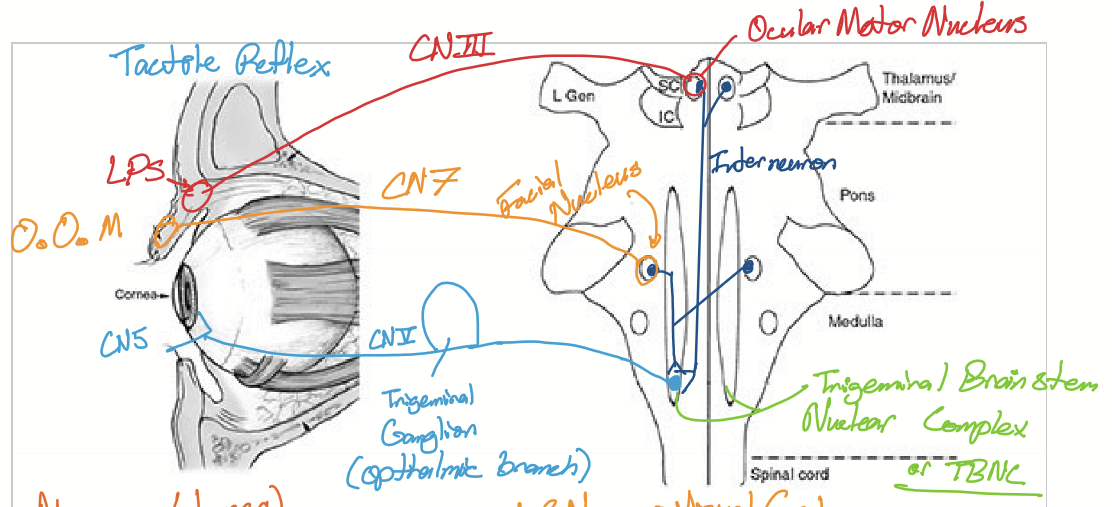
Pathway taken for tactile reflex blinking
Starts at CN5 at cornea, goes to trigeminal ganglion of opthalmic branch, goes to trigeminal brain stem nuclear complex or TBNC, goes to inter-neuron to facial nucleus and ocular motor nucleus before taking CN 7&3 to cause blink
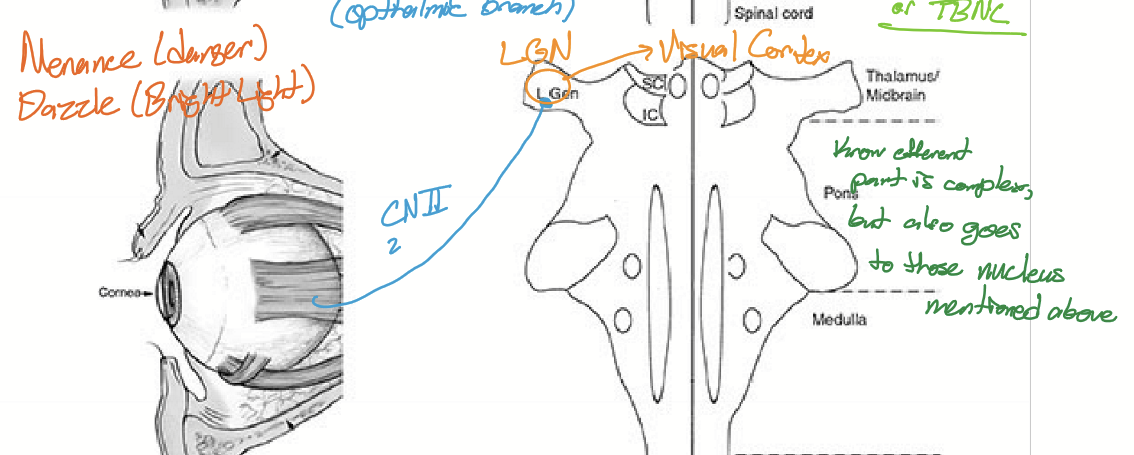
Pathway taken for menance or dazzle
Starts at CN2 going to lateral geniculate nucleus, then visual cortex
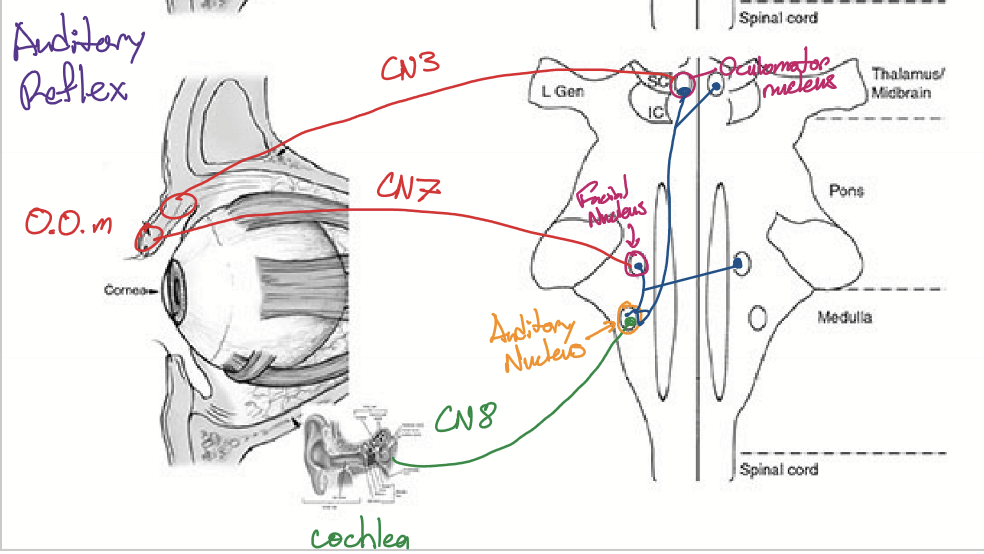
Pathway taken for auditory reflex
Starts at cochlea, takes CN8 to go to auditory nucleus, inter-neurons to go to facial nucleus and oculomotor nucleus, takes CN7 and 3 to go to O.O. muscle
Blepharospasm
Involuntary, forceful and repetitive bilateral spasms of lid closure. Begins with elevated blink rate that progressively increases
Causes of Blepharospasm
Idiopathic, but is associated with Trigeminal reflex blink hyperexcitability contractioning of orbicularis oculi. (not associated with other neurological abnormalities; more common in women vs men. associated with parkinsons)
What is Myokymia
Involuntary focal hyper-excitability of peripheral nerve motor axons of the orbicularis oculi (eye twitch)
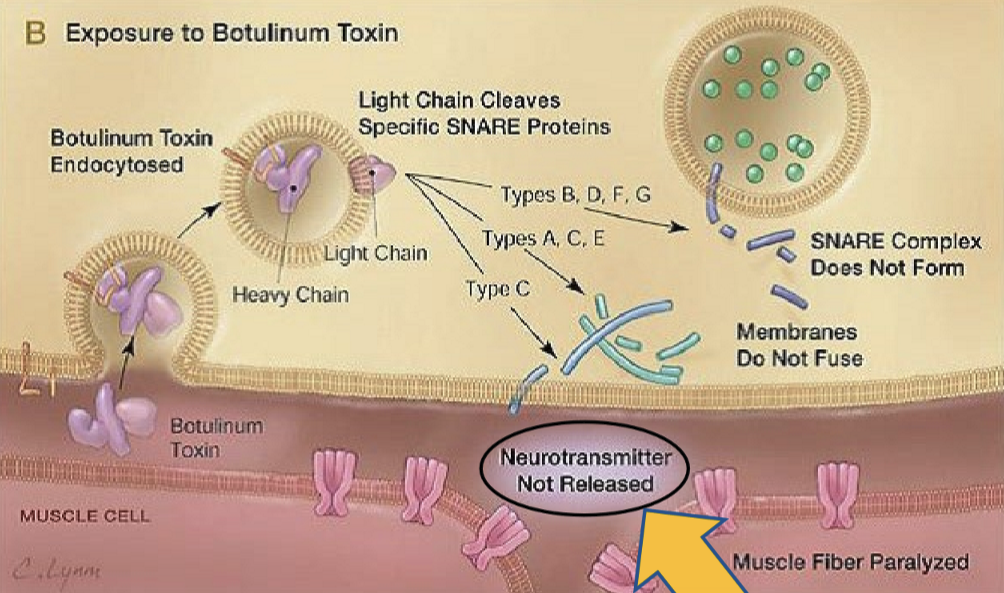
What is used to treat blepharospasm?
Botulism toxin, it works by cleaving specific SNARE proteins (used to anchor the synaptic vesicles against the cell membrane to release neurotransmitters)
Lid-Opening Apraxis (LOA) is what?
The inability to initiate and sustain eyelid opening after voluntary or involuntary eye closure
What causes LOA?
Abnormal involuntary inhibition of of LPS basal tonic activity or contraction of the pretarsal portion of O.O. muscle
Are blepharospasms observed with Lid-opening apraxia?
Yes, typically together.
Lagophtalmos is what
A condition that prevents the patient from closing their eyelids. Also seen with widening of palpebral aperture and laxity of lower lid
What causes Lagophthalmos
Infranuclear lesion of CN VII
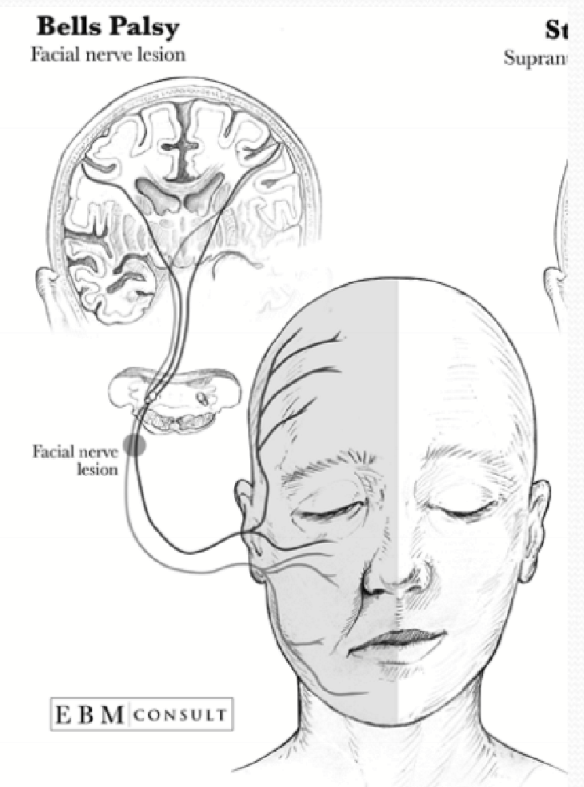
Bell’s Palsy is defined as what?
acute unilateral facial weakness

Thyroid eye disease is caused by what?
An autoimmune disorder where the thyroid stimulating hormone receptor is stimulated
Risk factors for Thyroid Eye Disease
Women 5-6x more likely vs Men & smoking
What are potential ocular issues from TED
Retraction of the upper lid/ Dalrymple’s Sign: activation of levator and Muller muscles and exophthalamos from orbital tissue swelling
Von Graefe’s Sign: upper lid lag on downward gase d/t overstimulation of levator muscle
Vision threat: Exposure keratopathy & compressive Optic neuropathy
What is Pseudo-Graefe Phenomenon?
Misdirection of fibers intented for the medial rectus to the levator, causing lid rectraction in downward inward gaze
What causes Pseudo-Graefe Phenomenon?
Typically, recovery from CN III paralysis
What are the function of tear
Maintain smooth optical surface
Primary source of atmospheric oxygen for cornea
Source of glucose/nutrients for cornea
Traps exogenous debris, helps remove sloughed cells, and flushes out metabolic/cellular waste products
Pathogen defense: physical barrier and contains antibacterial substances
Aids corneal hydration
aids wound repair
lubricates globe/eyelid apposition during palpebral closure
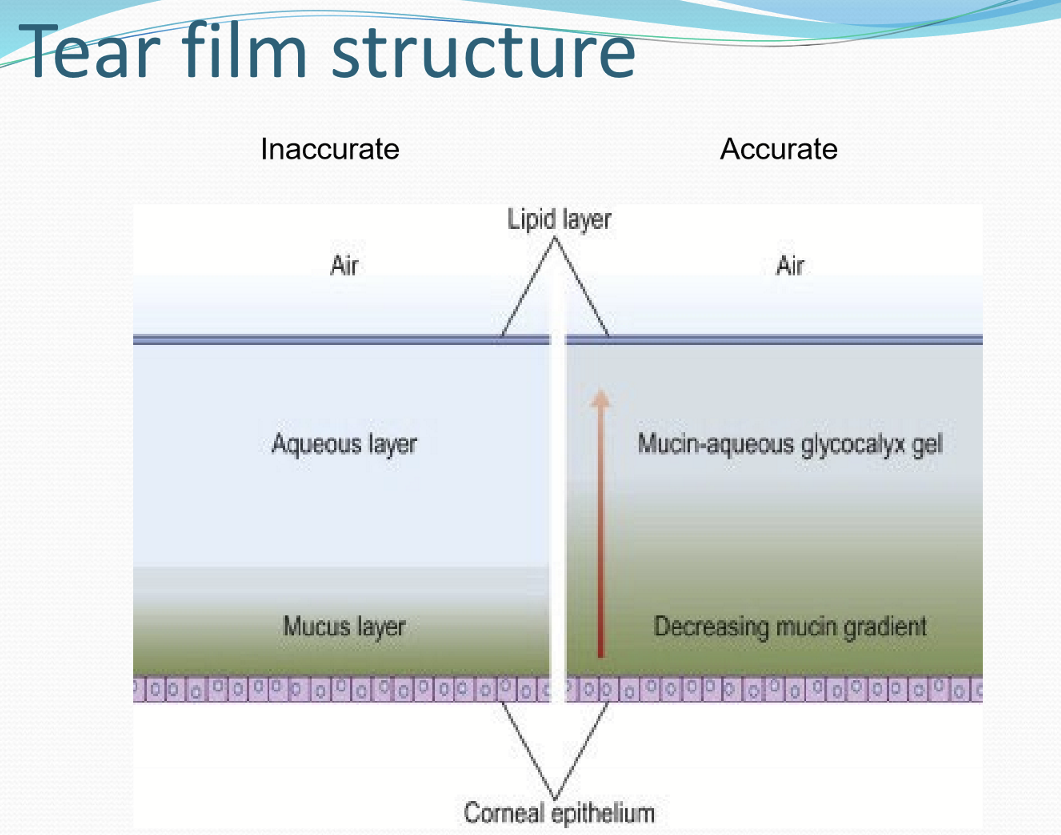
What layers compose the tear film structure?
top: lipid layer → mucin-aqueous glycocalyx gel→ thicker mucin layers → corneal epithelium
What is the thickness of the tear film?
Central thickness: ~3 micromemters
Meniscus: ~270 micrometers
How thick is the lipid layer?
50-100 nm lipid layer thickness
What is the tear volume in the eye?
~6.5 microliters
How much tear is drained/evaporated per minute?
~1.2 microliters per minutes
What are the types of tears?
basal tears
reflective tears
psycho-emotional tears
What are basal tears?
continuous basal rate of lacrimal secretion; decreases with age
What are reflexive tears?
response to external stimuli
Temperature
Chemical irritation
Pressure (oculo-lacrimal)
Nasal
Photo-lacrimal
Not found in infants
What are Psycho-emotional tears?
Tears made from emotional responses, unique to humans
What are the most common ions in tears?
Na, Cl, K, and HCO3
How are ions transported into the tears?
The are transported across plasma membranes of lacrimal and ocular surface cells for the purposes of transporting water via paracellular and transcellular pathways.
What is unique about glucose in tears?
The concentration in tears correlates with blood glucose
What is the typical glucose concentration in tears?
7.4 mg/dl