Group A β-Hemolytic Streptococci (GAS): Streptococcus pyogenes
1/114
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
115 Terms
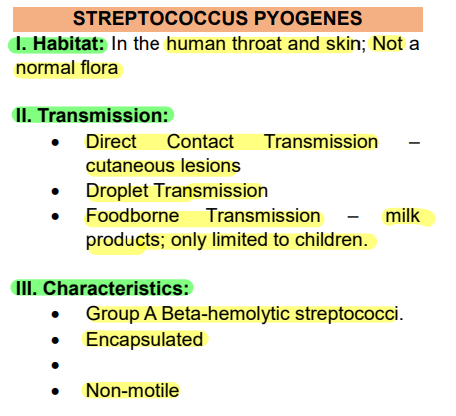
Habitat, Transmission, and Characteristics of S. pyogenes
PATHOGENESIS AND CLINICAL MANIFESTATIONS
S. pyogenes as most common causative agent of pharyngitis.
Pharyngitis or streptococcal sore throat
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Usually self-limiting (illness resolves on its own even without medical intervention). Typically, the fever is gone by the third to fifth day, and other manifestations subside within 1 week.
Pharyngitis or streptococcal sore throat
PATHOGENESIS AND CLINICAL MANIFESTATIONS
The most common infection caused by S. pyogenes.
Pharyngitis or streptococcal sore throat
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Although it may occur at any age, it occurs most frequently between the ages of 5 and 15 years.
Pharyngitis or streptococcal sore throat
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Characterized by acute sore throat, malaise, fever, and headache.
Pharyngitis or streptococcal sore throat
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Typically involves the tonsillar pillars, uvula, and soft palate, which become red, swollen, and covered with a yellow-white exudate.
Pharyngitis or streptococcal sore throat
PATHOGENESIS AND CLINICAL MANIFESTATIONS
The cervical lymph nodes that drain this area may also become swollen and tender.
Pharyngitis or streptococcal sore throat
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Caused by lysogenized strains of S. pyogenes that produce pyrogenic exotoxins A - C
Scarlet Fever or Scarlatina
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Occurs in association with streptococcal pharyngitis
Scarlet Fever or Scarlatina
PATHOGENESIS AND CLINICAL MANIFESTATIONS
The buccal mucosa, temples, and cheeks are deep red, except for a pale area around the mouth and nose (circumoral pallor).
Scarlet Fever or Scarlatina
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Punctate hemorrhages appear on the hard and soft palates, and the tongue becomes covered with a yellow-white exudate through which the red papillae are prominent (strawberry tongue).
Scarlet Fever or Scarlatina
PATHOGENESIS AND CLINICAL MANIFESTATIONS
A diffuse red “sandpaper” rash appears on the second day of illness, spreading from the upper chest to the trunk and extremities.
Scarlet Fever or Scarlatina
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Circulating antibody to the toxin neutralizes its effects.
Scarlet Fever or Scarlatina
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Due to erythrogenic toxin
Scarlet Fever or Scarlatina
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Starts with strep throat (occurs in association with streptococcal pharyngitis).
Scarlet Fever or Scarlatina
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Signs and Symptoms of Scarlet Fever
Strawberry Tongue – due to hyperemia
Rashes – usually starts at trunk and spread to the extremities.
PATHOGENESIS AND CLINICAL MANIFESTATIONS
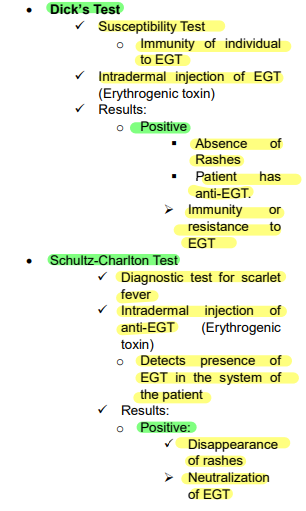
Tests Involve in Scarlet Fever or Scarlatina
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Infection of superficial layer of skin
Streptococcal pyoderma (or impetigo)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Lesions are often seen on the lower extremities and may also involve other pathogens such as S. aureus.
Streptococcal pyoderma (or impetigo)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Infection of superficial layers of skin
Streptococcal pyoderma (or impetigo)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Usually occurs in children ages 2-15 years old, with peak incidence in the 2- to 5-year age group.
Streptococcal pyoderma (or impetigo)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Characterized by the formation of papules that develop into vesicular lesions and evolve into pustules. These pustules break down over the next 5 to 7 days to form thick scabs.
Streptococcal pyoderma (or impetigo)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Lesions are often seen on the lower extremities and may also involve other pathogens such as S. aureus.
Streptococcal pyoderma (or impetigo)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
An infection of the dermis and subcutaneous tissues
Erysipelas
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Organism enters through a small wound or incision on the face or extremities
Erysipelas
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Characterized by edema and erythematous (red) lesion that is hot, and often vesicular with rapidly advancing, well-demarcated edges
Erysipelas
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Pain, and systemic manifestations, such fever and lymphadenopathy are evident.
Erysipelas
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Infection usually occurs on the face and commonly in association with a history of streptococcal sore throat
Erysipelas
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Infection of the dermis and subcutaneous tissues
Erysipelas
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Reddening and thickening of skin
Erysipelas
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Rapidly advancing brawny edema
Erysipelas
PATHOGENESIS AND CLINICAL MANIFESTATIONS
An acute, rapidly spreading infection of the skin and subcutaneous tissues.
Cellulitis
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Occurs following streptococcal infection of preexisting lesions (i.e., mild trauma, burns, wounds, or surgical incisions).
Cellulitis
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Symptoms include pain, tenderness, swelling, and erythema particularly occurring within the affected area.
Cellulitis
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Differentiated from erysipelas by two clinical findings:
Cellulitis
In cellulitis, the lesion is not raised, and the line between the involved and uninvolved tissue is indistinct.
PATHOGENESIS AND CLINICAL MANIFESTATIONS
An acute, rapidly spreading infection of the skin and subcutaneous tissue.
Cellulitis
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Organism enters at the site of localized trauma or previous surgery, or via hematogenous seeding of subcutaneous muscles and soft tissue.
Necrotizing fasciitis (streptococcal gangrene)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Bacteria other than S pyogenes can also cause necrotizing fasciitis.
Necrotizing fasciitis (streptococcal gangrene)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Consists of extensive and very rapidly spreading necrosis of the skin, tissues, and fascia.
Necrotizing fasciitis (streptococcal gangrene)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Organism enters at the site of localized trauma or previous surgery, or via hematogenous seeding of subcutaneous muscles and soft tissue.
Necrotizing fasciitis (streptococcal gangrene)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Affected tissues become gangrenous, with sloughing of devitalized tissues and extensive subcutaneous tissue necrosis.
Necrotizing fasciitis (streptococcal gangrene)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Group A streptococci that cause necrotizing fasciitis are termed “flesh-eating bacteria”.
Necrotizing fasciitis (streptococcal gangrene)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Bacteria other than S pyogenes can also cause necrotizing fasciitis.
Necrotizing fasciitis (streptococcal gangrene)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Occurs in women following child birth (either by vaginal or abdominal/Csection) or abortion.
Puerperal fever
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Organisms colonizing the genital tract or from an obstetrical personnel invade the upper genital tract, causing endometritis, lymphangitis, bacteremia, necrotizing fasciitis, and streptococcal toxic shock syndrome.
Puerperal fever
PATHOGENESIS AND CLINICAL MANIFESTATIONS
_______________, may lead to severe and often fatal group A streptococcal disease in the neonate.
Puerperal fever
Intrapartum (occurring during pregnancy) transmission of group A streptococci
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Manifestations in the neonate include septicemia, jaundice, and cellulitis, or stillbirth.
Puerperal fever
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Puerperal fever is Aka
“Childbirth Fever”
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Infection of uterus and the rest of reproductive tract.
Puerperal fever
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Occurs in women following childbirth (either by vaginal or abdominal/Csection) or abortion.
Puerperal fever
PATHOGENESIS AND CLINICAL MANIFESTATIONS
May result from streptococcal infection of traumatic or surgical wounds.
Bacteremia or Sepsis
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Can be rapidly fatal.
Bacteremia or Sepsis
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Can also occur with skin infections, such as cellulitis and rarely pharyngitis.
Bacteremia or Sepsis
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Are non-suppurative sequelae that occur weeks after GAS infection in the throat and/or skin.
Post Streptococcal Diseases
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Post Streptococcal Diseases:
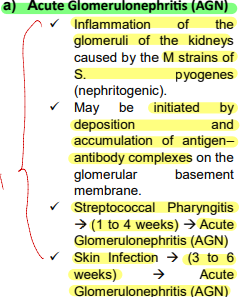
Begins 1 to 4 weeks after streptococcal pharyngitis or 3 to 6 weeks after skin infection; primarily a disease of childhood.
Acute Glomerulonephritis (AGN)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Post Streptococcal Diseases:
Inflammation of the glomeruli of the kidneys caused by the M strains of S. pyogenes (nephritogenic).
Acute Glomerulonephritis (AGN)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Post Streptococcal Diseases:
May be initiated by deposition and accumulation of antigen– antibody complexes on the glomerular basement membrane
Acute Glomerulonephritis (AGN)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Post Streptococcal Diseases:
Signs symptoms: dark, smoky urine (due to blood and proteins) edema, hypertension, and urea nitrogen retention.
Acute Glomerulonephritis (AGN)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Post Streptococcal Diseases:
Majority recover completely while some develop chronic glomerulonephritis with kidney failure, and a few die
Acute Glomerulonephritis (AGN)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Acute Glomerulonephritis (AGN)
Provide the overview.
PATHOGENESIS AND CLINICAL MANIFESTATIONS
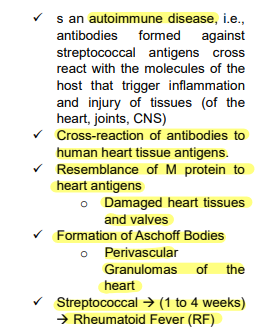
Post Streptococcal Diseases:
Is an autoimmune disease, i.e., antibodies formed against streptococcal antigens cross react with the molecules of the host that trigger inflammation and injury of tissues (of the heart, joints, CNS)
Rheumatic fever (RF)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Post Streptococcal Diseases:
Signs and symptoms: fever, malaise, arthritis, carditis, chorea (neurologic disorder characterized by involuntary jerky movements), and skin nodules
Rheumatic fever (RF)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Post Streptococcal Diseases:
Pathologic processes of S. pyogenes infection can extend to the heart. The cross-reaction between streptococcal-induced antibodies and heart proteins have a gradual destructive effect on atrioventricular valve. Scarring and deformation change the capacity of the valves to close and shine the blood properly leading to Rheumatic Heart Disease.
Rheumatic fever (RF)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Post Streptococcal Diseases:
Has a marked tendency to be reactivated by recurrent streptococcal infections in contrast with nephritis.
Rheumatic fever (RF)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Post Streptococcal Diseases:
Occur more frequently in tropical countries and is the most important cause of heart disease in young people in developing countries.
Rheumatic fever (RF)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Post Streptococcal Diseases:
Considered as the most serious sequela of S. pyogenes because it results in damage to heart muscle and valves.
Rheumatic fever (RF)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Post Streptococcal Diseases:
Occurs 1–4 weeks after S. pyogenes pharyngitis
Rheumatic fever (RF)
PATHOGENESIS AND CLINICAL MANIFESTATIONS
Rheumatic fever (RF)
Provide the overview
Considered as the most serious sequela of S. pyogenes because it results in damage to heart muscle and valves.
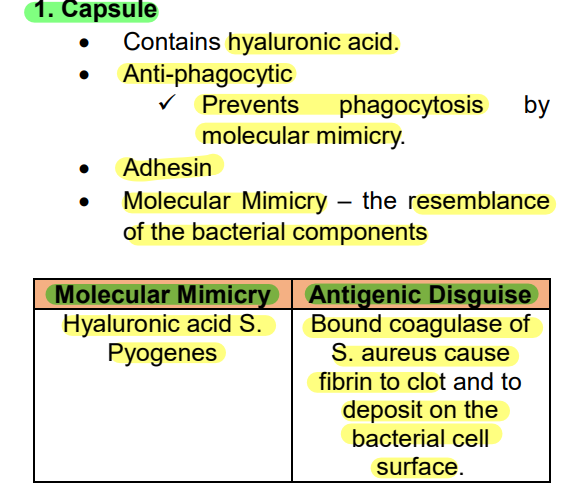
VIRULENCE FACTORS
A. Surface Structures
Overview of Capsule
VIRULENCE FACTORS
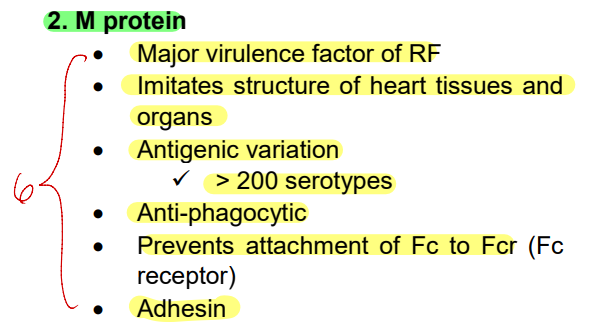
A. Surface Structures
Overview of M Protein
VIRULENCE FACTORS
A. Surface Structures
Overview of Protein F
VIRULENCE FACTORS
A. Surface Structures
Overview of Protein G
VIRULENCE FACTORS
A. Surface Structures
______________________ is a major virulence factor of S. pyogenes (those that lack M protein are not virulent).
M Protein
VIRULENCE FACTORS
A. Surface Structures
Found on the bacterial cell surface associated with fimbriae.
M Protein
VIRULENCE FACTORS
A. Surface Structures
There are more than __________________; _______________ is related to the production or presence of type specific antibodies against M protein; subsequent infections may occur with different M serotypes
M Protein
200 types of S. pyogenes M proteins
immunity to infection with GAS
VIRULENCE FACTORS
A. Surface Structures
Inhibits activation of the complement pathway by destroying C3-convertase thereby prevents formation of the opsonin C3b
M Protein
VIRULENCE FACTORS
A. Surface Structures
A polysaccharide capsule, which is composed of hyaluronic acid
Capsule
VIRULENCE FACTORS
A. Surface Structures
Prevents opsonized phagocytosis by neutrophils or macrophages.
Capsule
VIRULENCE FACTORS
A. Surface Structures
Is non-immunogenic; it is chemically similar with the hyaluronic acid in the host's connective tissue ground substance
Capsule
VIRULENCE FACTORS
A. Surface Structures
Allows the bacterium to mask its antigens and remain unrecognized by its host’s immune system
Capsule
VIRULENCE FACTORS
A. Surface Structures
Erythrogenic Toxins is formerly called______________________
streptococcal pyrogenic exotoxins (Spe)
VIRULENCE FACTORS
A. Surface Structures
Erythrogenic Toxins have a four antigenically distinct streptococcal pyrogenic exotoxins — __________________________.
SpeA, SpeB, SpeC, and SpeF
VIRULENCE FACTORS
A. Surface Structures
In erythrogenic toxins, in the four antigenically streptococcal pyrogenic exotoxins, _________________ has been most widely studied.
SpeA
VIRULENCE FACTORS
A. Surface Structures
Elaborated by lysogenic S. pyogenes that contain genes from temperate bacteriophage.
Erythrogenic Toxin
VIRULENCE FACTORS
A. Surface Structures
Act as superantigens which stimulate monocytes and T cells. When activated, these cells proliferate and produce tumor necrosis factor, which in high quantities leads to damage of the plasma membrane of blood capillaries.
Erythrogenic Toxin
VIRULENCE FACTORS
A. Surface Structures
Responsible for the manifestations of scarlet fever
Erythrogenic Toxin
VIRULENCE FACTORS
A. Surface Structures
______________ is a skin test for scarlet fever that uses antitoxin to the erythrogenic toxin of Streptococcus pyogenes subcutaneously: a positive reaction is _______________________
Schultz-Charlton Test
blanching of the rash in the area around the injection site
VIRULENCE FACTORS
A. Surface Structures
________________ is a skin test performed to determine an individual’s susceptibility to scarlet fever.
Development of a red rash with a diameter of 10 mm or greater indicates _________________________.
Dick Test
lack of immunity to the disease.
VIRULENCE FACTORS
A. Surface Structures
It is a test consists of intradermal injection of diluted scarlet fever toxin on the arm of a suspected patient.
Dick Test
VIRULENCE FACTORS
B. Toxins and Enzymes
S. pyogenes elaborates two hemolytic exotoxins, proteins that not only lyse the membranes of erythrocytes but also damage a variety of other cell types.
Streptolysins
VIRULENCE FACTORS
B. Toxins and Enzymes
The _________________ refers to this hemolysin being oxygen labile. It is active only in the reduced form.
Streptolysin O (SLO)
VIRULENCE FACTORS
B. Toxins and Enzymes
Is responsible for hemolysis on sheep blood agar (SBA) plates incubated anaerobically or subsurface hemolysis when growth occurs in cuts (stabs) made deep into the blood agar plates
Streptolysin O (SLO)
VIRULENCE FACTORS
B. Toxins and Enzymes
It lyses a variety of host cells including leukocytes, platelets, as well as RBCs.
Streptolysin O (SLO)
VIRULENCE FACTORS
B. Toxins and Enzymes
It is highly immunogenic, and infected individuals readily form antibodies against it known as ___________________ which blocks hemolysis caused by streptolysin O.
Streptolysin O (SLO)
anti-streptolysin O (ASO)
VIRULENCE FACTORS
B. Toxins and Enzymes
_______________ combines quantitatively with streptolysin O and is measured in the _______________
Streptolysin O (SLO)
anti-streptolysin O (ASO)
Anti-streptolysin O Test
VIRULENCE FACTORS
B. Toxins and Enzymes
___________________ is a test performed to determine whether an individual has had a recent infection with S. pyogenes.
Anti-Streptolysin O Test (ASTO or ASOT)
VIRULENCE FACTORS
B. Toxins and Enzymes
It involves detection and quantitation of Anti-Streptolysin O antibodies in the serum
Anti-Streptolysin O Test (ASTO or ASOT)
VIRULENCE FACTORS
B. Toxins and Enzymes
An abnormally high serum titer suggests either recent infection with S. pyogenes or persistently high antibody levels caused by an exaggerated immune response to an earlier exposure in a hypersensitive person.
Anti-Streptolysin O Test (ASTO or ASOT)
VIRULENCE FACTORS
B. Toxins and Enzymes
Anti-Streptolysin O Test (ASTO or ASOT) is also related to the ________________________ (to check whether rheumatic fever is caused by a previous streptococcal infection or by other etiologies).
retro-diagnosis of rheumatic fever