module 7/8 exam 2
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
parasympathetic
decrease HR
ACh muscarinic
SA node
hyperpolarizing graded potential due to G-protein coupled reaction that creates an increased permeability to K, hyperpolarizing it
long time for SA node to reach threshold
sympathetic
SA node, ventricular muscle, arterioles
increases HR, stroke volume contractility, resistance (vasoconstriction) to increase BP
depolarizes faster and reach threshold faster
beta-1 in SA node
HR is faster
beta-1 in contractile cells
increases Ca concentration
greater force of contraction = increased SV
beta-2
on smooth muscle
vasodilation
decrease intracellular Ca
alpha
vasoconstriction by increase intracellular Ca
smooth muscle and arterioles
CO
HR x SV
MAP
CO x R = (HR x SV) x R
tidal volume
500 mL
normal inspiration/expiration
expiratory reserve volume
1100 mL
additional air that can be expired by forceful effort
inspiratory reserve volume
3000 mL
max amount of additional air by forceful inspiration
residual volume
volume of air that’s left in alveoli
1200 mL
total lung capacity
5800 mL
vital capacity
max volume in or out - 4.6 L
capacity
sum of two or more
dead space
volume of air remaining in conducting airways at the end of each expiration (150 mL)
part of tidal volume
mixes w fresh air
diff from residual volume that’s always in alveoli
alveolar ventilation
(breath volume - dead space/150mL) x breaths per min
increasing ventilation rate is much better than volume
pulmonary circulatory
to lungs
systemic circulation
to body
pulmonary capillaries
O2 flows into the blood due to pressure gradient (blood PO2 < alveolar PO2)
CO2 into alveoli
blood leaving pulmonary/arterial is equal to alveolar
systemic capillaries
O2 into the cells/interstitial fluid
CO2 out of the cells into blood
blood leaving systemic capillary/venous blood is equal to interstitial fluid
partial pressure of O2 is due to…
dissolved O2 in plasma (2%)
what effect do hydrogen ions have on conformation of hemoglobin
decreases its affinity for oxygen
thus, the P50 value will be larger as it takes more pressure of O2 in order to have 2 binding sites full
decreasing pH, increases O2 release onto active tissue
what other factors create rightward shift in HbO2
increase in temp
high PCO2
myoglobin
one binding site
in muscle cells
higher affinity for oxygen than hemoglobin
at 20 mmHg, more than 80% saturated, which hemoglobin has given up most of its oxygen
O2 reserve
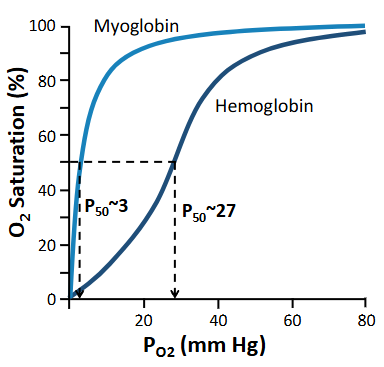
cooperativity
in hemoglobin, changes shape
allows for subsequent O2 to bind easier on hemoglobin
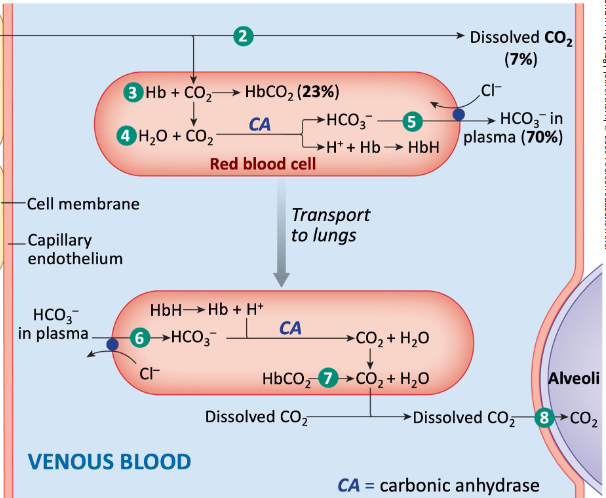
CO2 in blood
7% dissolved in plasma (PCO2)
bicarbonate (HCO3-) in plasma 70%
most of H+ bound to hemoglobin
respiratory drive
PCO2, PO2, pH (involuntary)
conscious volition
controlling ventilation
medulla is the respiratory control centers and have chemoreceptors (chemical changes) that respond indirectly to CO2 lvls (main signal for respiratory)
as CO2 lvls increase, orchestrate signals to respiratory muscles (diaphragm, external intercostals) and then relax
increase in plasma CO2
dissolved in the plasma and goes thru BBB
H+ can’t
chemoreceptor in medulla detects acid/H+ concentration
neg feedback to increase ventilation
hyperventilation
decrease PCO2
increases pH of CSF/decrease H+
decrease respiratory drive
hypoventilation
hold your breath
decreases pH, increase PCO2
Describe the general characteristics of asthmatic airways
exaggerated immune response to triggers
inflammation of the conducting airways → mucus buildup
diameter for air decreases, increases resistance to airflow
smooth muscle that circles the airways, contracts - B2 adrenergic receptors
fluticasone
maintenance medicine
dry powder inhalers (DPIs)
the receptor determines the response in fluticasone (synthetic cortisol)
cytoplasmic receptor changes gene expression (anti-inflammatory genes expressed in response)
salmeterol and albuterol
long-acting vs short-acting
both beta2 adrenergic agonists
airway smooth muscle relaxation, so diameter increases = improves airflow