6. Somatic Motor System
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
38 Terms
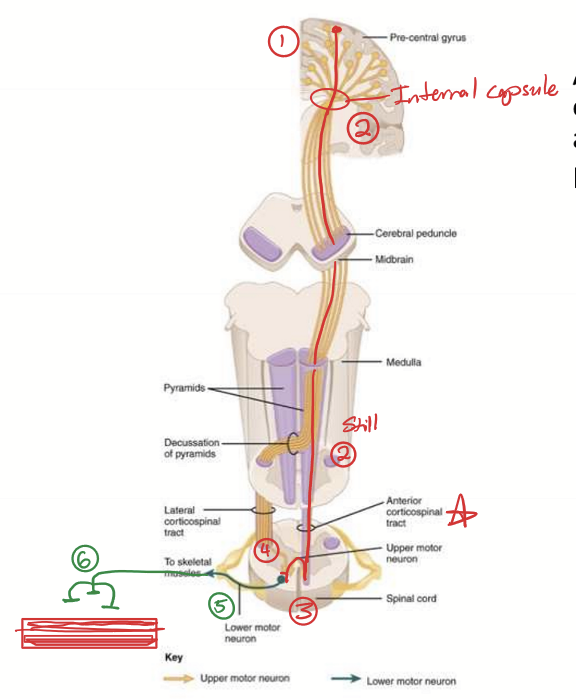
Corticorspinal tract (CST) or Pyramidal System Characteristics
Major descending tract with contralateral pattern. There is an upper motor and lower motor neuron in this tract.
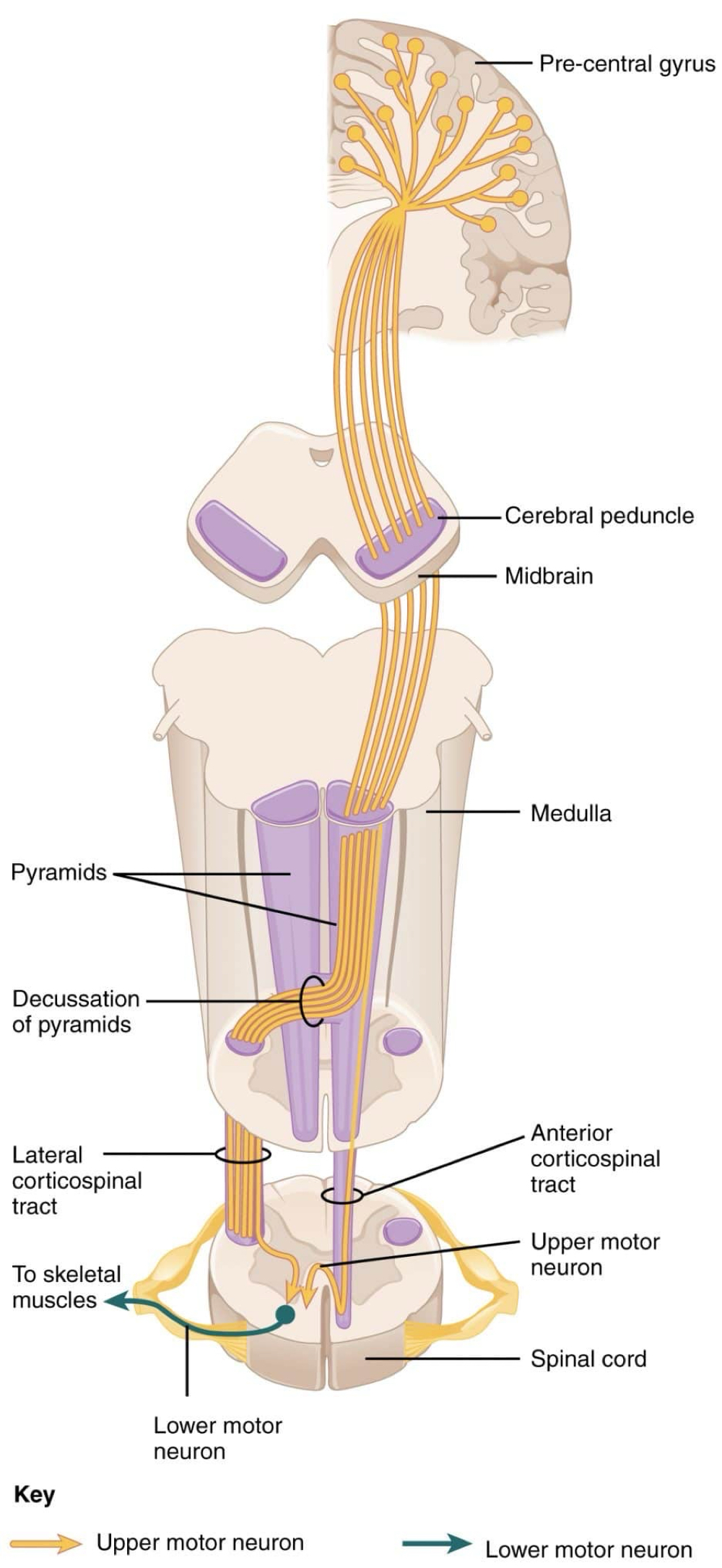
What does the corticospinal tract do?
Directing volitional movement
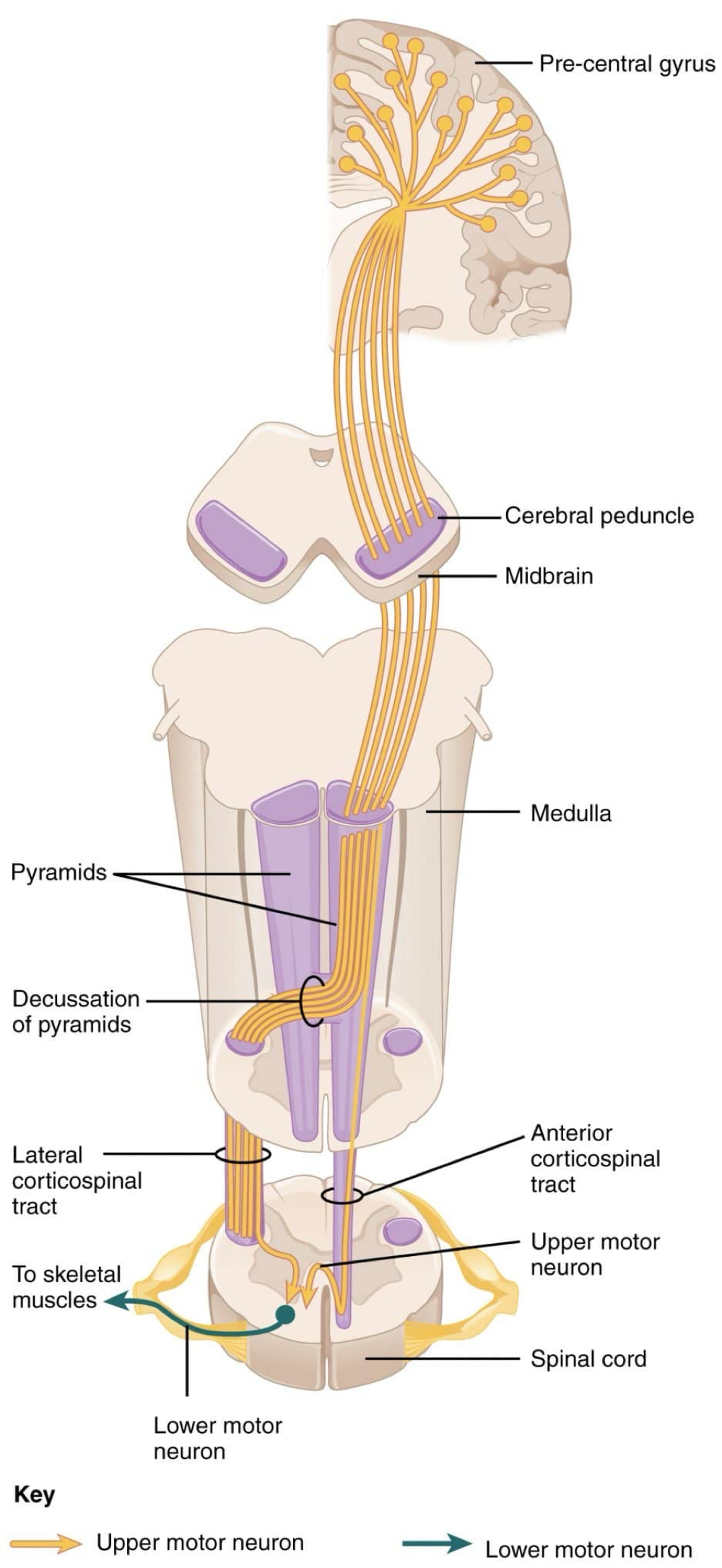
What are the two tracts of the corticospinal tract/pyramidal tracts?
Lateral and anterior corticospinal tract.
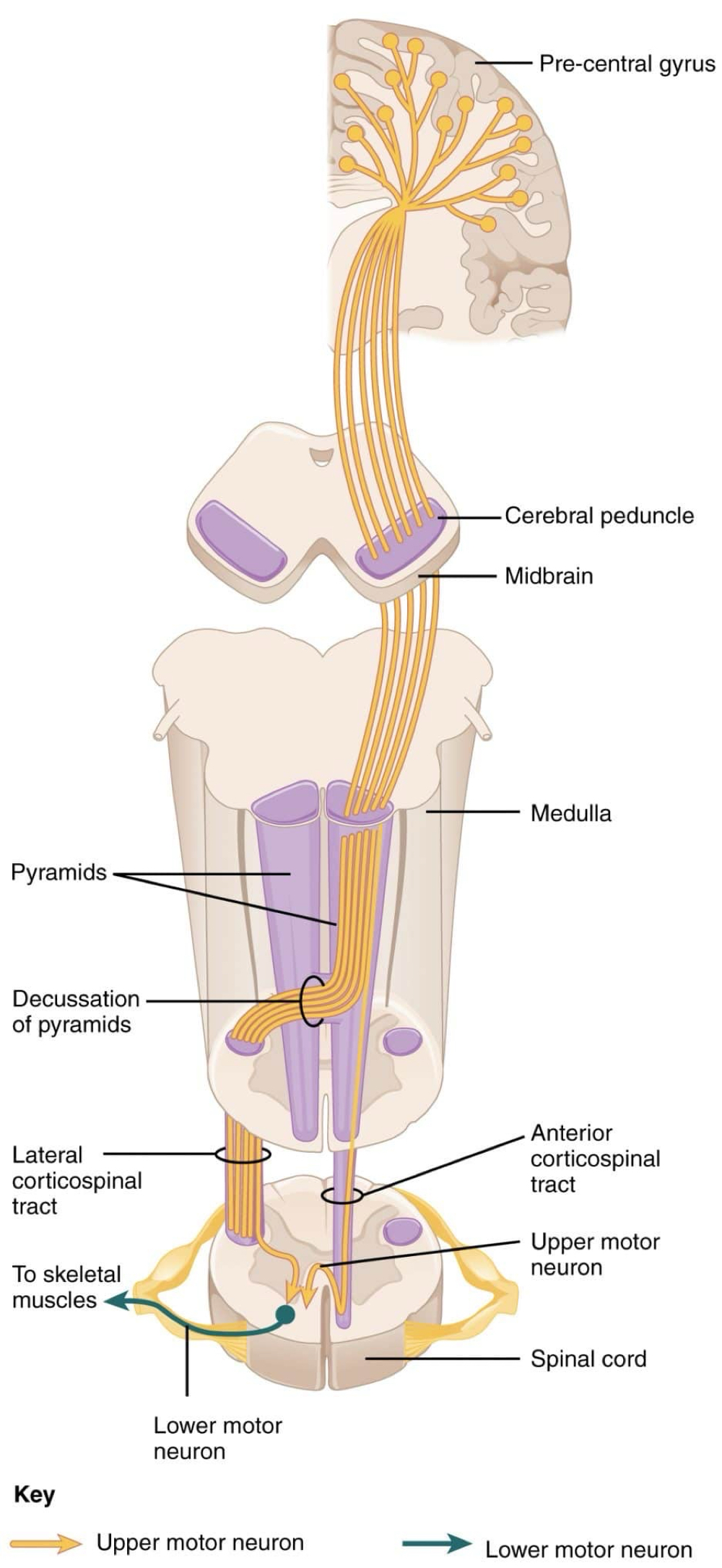
What does the lateral corticospinal tract control?
Distal muscles and fine movement
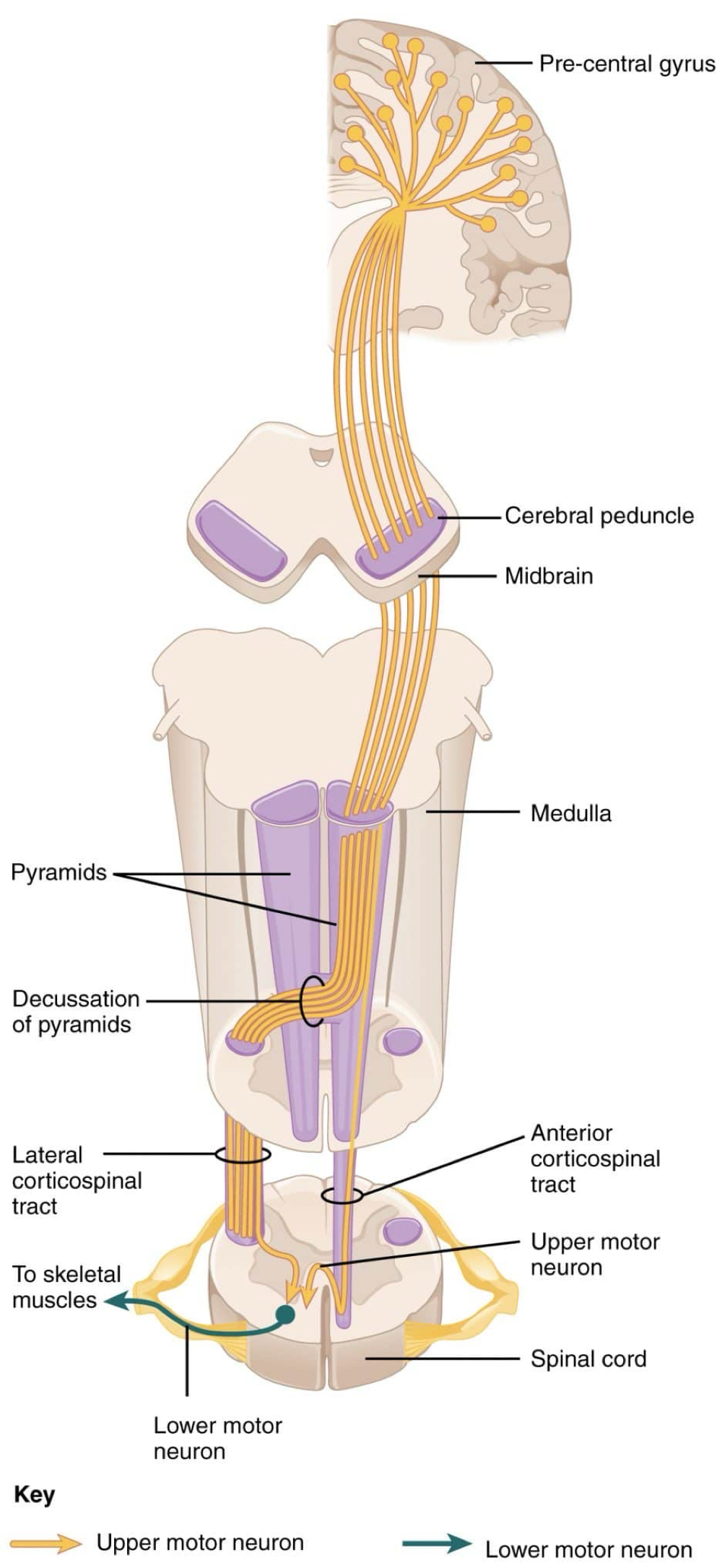
What does the anterior corticospinal tract control?
Proximal and axial muscles and large movement and posture
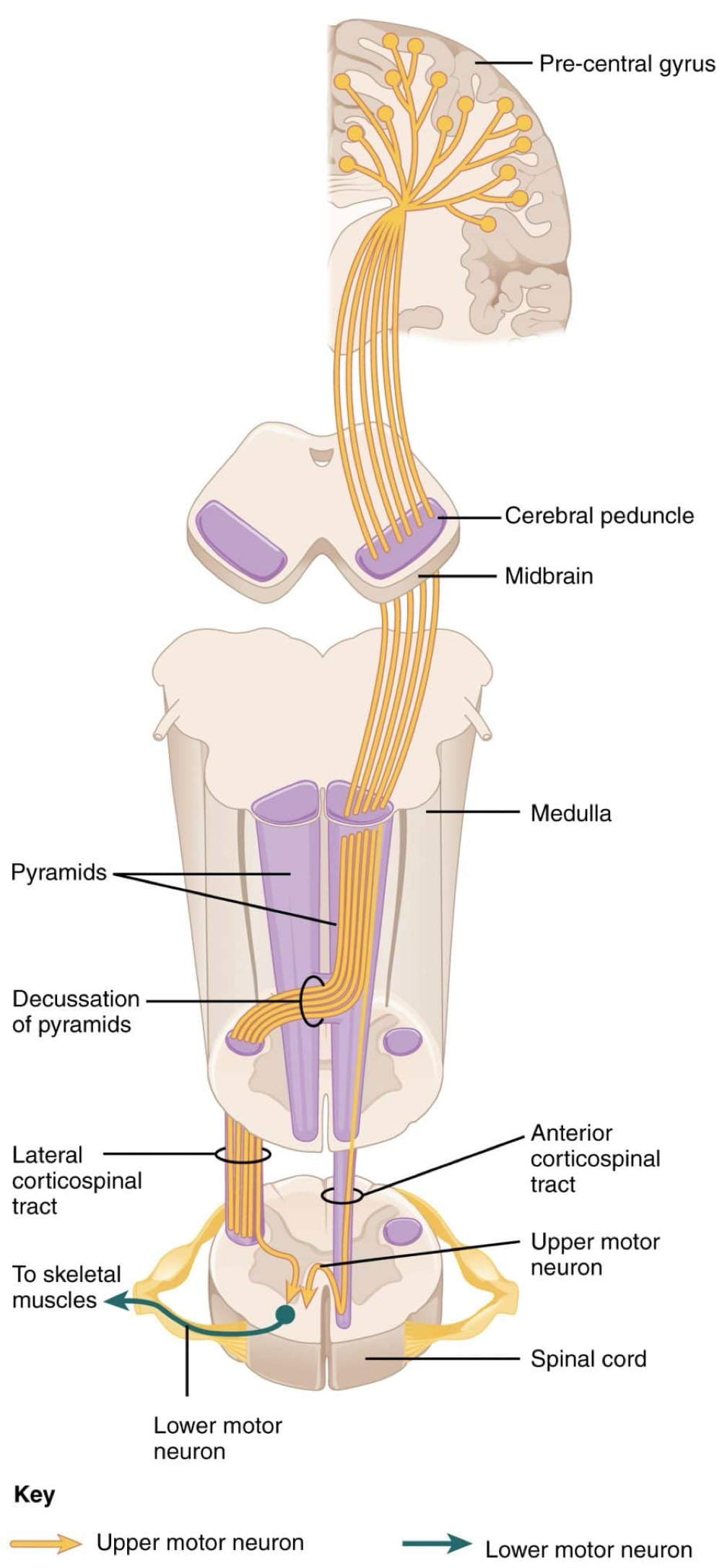
What is the path that the lateral corticospinal tract take?
Starts at upper motor neuron cell body in contralateral primary motor cortex (precentral gyrus/ BA4)
Descends through internal capsule in posterior limb
Decussates in the medullary pyramids
Synapses in ventral horn on lower motor neuron
Lower motor neuron is an A alpha neuron that projects from the ventral horn through the ventral root of spinal cord
Synapses on skeletal muscle fibers in neuromuscular junctions or end plates
Innervates only 1 muscle to control fine movement
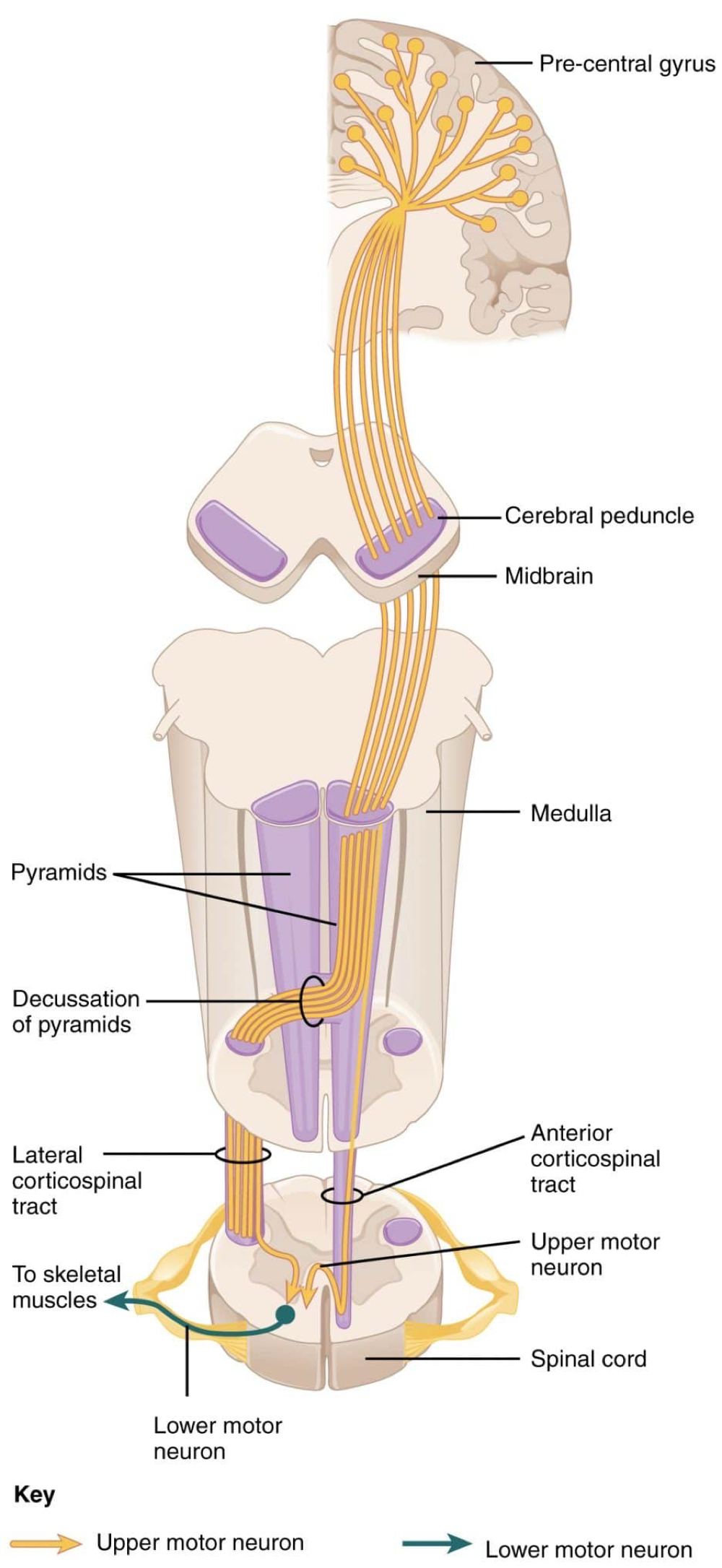
How are the motor of the limbs laid out on the ventral horn?
Proximal muscles are more centrally located compared to distal muscles
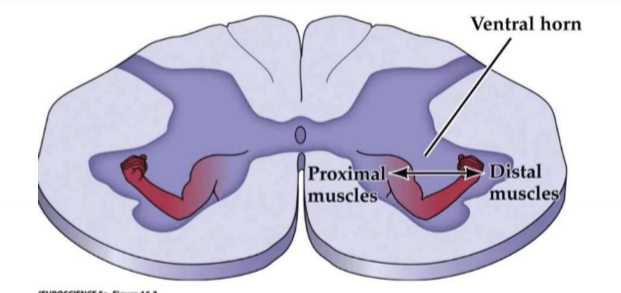
What units make up a motor unit?
Alpha motor neuron and skeletal muscle fibers
What are the types of motor units?
Small motor units for fine control with low divergence (innervates a small number of muscle fibers)
Large motor units are for postural (maintaining body posture and stability) and large movements. It has high divergence (innervates large number of muscle fibers)
What is the pathway nerves take for the anterior corticospinal tract (ventral)
Starts at UMN cell body in contralateral primary motor cortext (BA4/precentral gyrus)
Descends through internal capsule, medullary pyramids, and down spinal cord as anterior corticospinal tract without crossing over
Decussation occurs through anterior commissure of spinal cord at level of spinal nerve
Terminates in the medial ventral horn on cell body of the lower motor neuron
LMN axon exits through ventral root of spinal cord as an A alpha/ alpha motor neuron
Temrinates on skeletal muscle fibers to control large proximal muscles
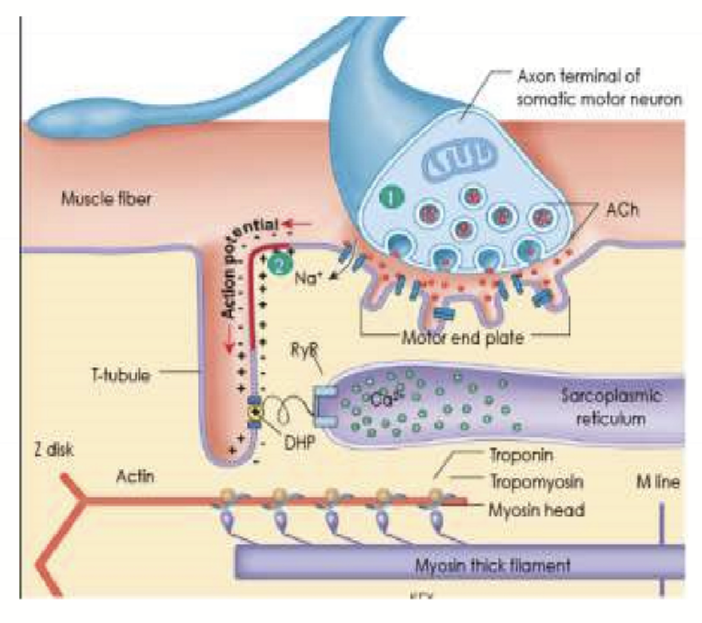
What is a neuromusclar junction?
The synapse between the lower motor neuron (an alpha motor neuron) and the skeletal muscle fiber
How does a NMJ work?
Depolarization of LMN releases a large amount of ACh
ACh binds to nicotinic cholinergic receptors on motor end plate of skeletal muscle fiber to open Na channels
Causes an End-plate potential/ EPP
ACh is removed by Acetylcholine esterase (AChE)
Causes an AP on the membrane of the skeletal muscle fiber to open Ca channels on SR
What are the structural characteristics of skeletal muscle?
Striated
Multinucleated
Sarcolemma has APs
APs travel to myofibrils/sarcomeres via t-tubules to excite entire cell
Contain several myofibrils
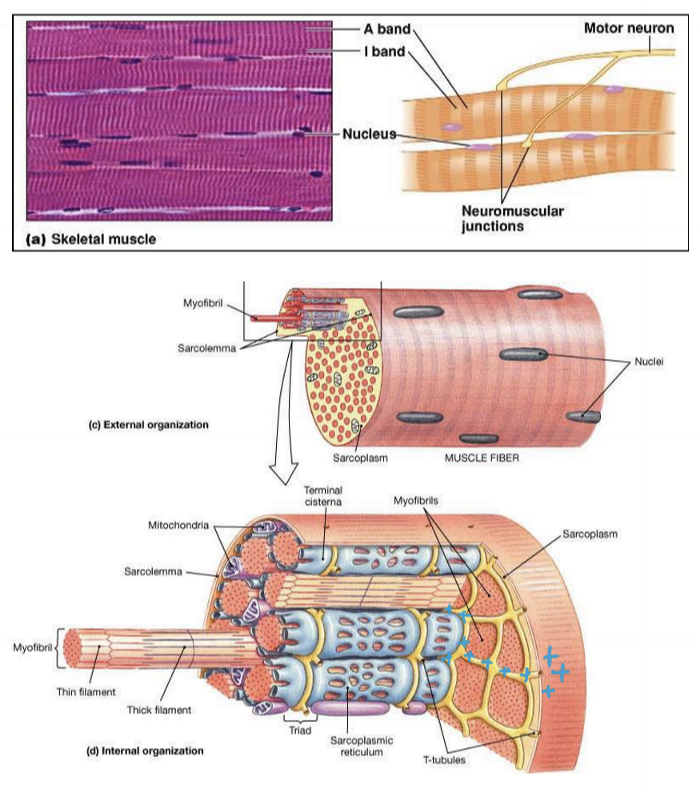
Describe a sarcomere unit
Extends from Z disc to Z disc. Contains thin actin filaments and thick myosin filaments.
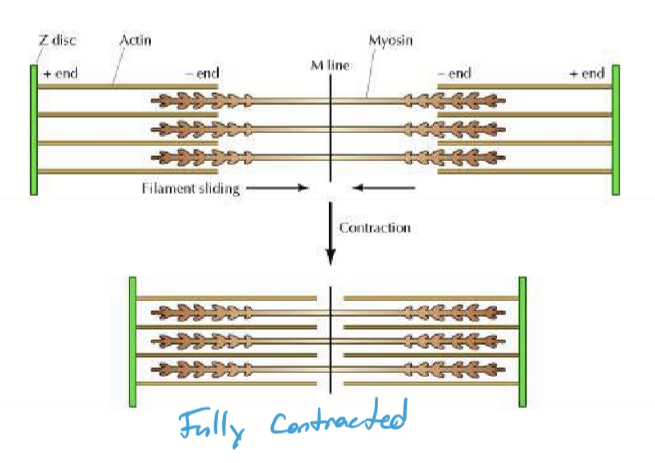
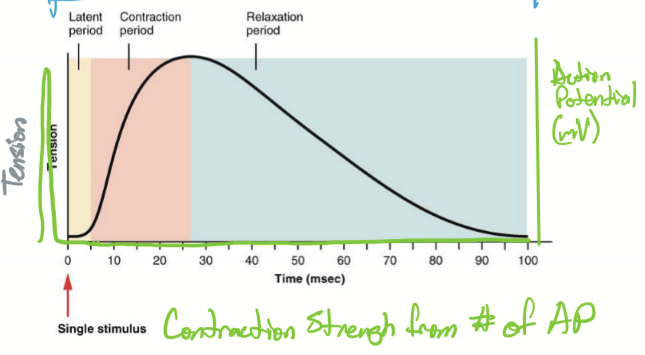
What are the phases of a twitch?
Latent period, where AP on sarcolemma travels down T-tubules to release Ca
Contraction phase, where myosin heads connect with actin
Relaxation phase, where Ca is removed
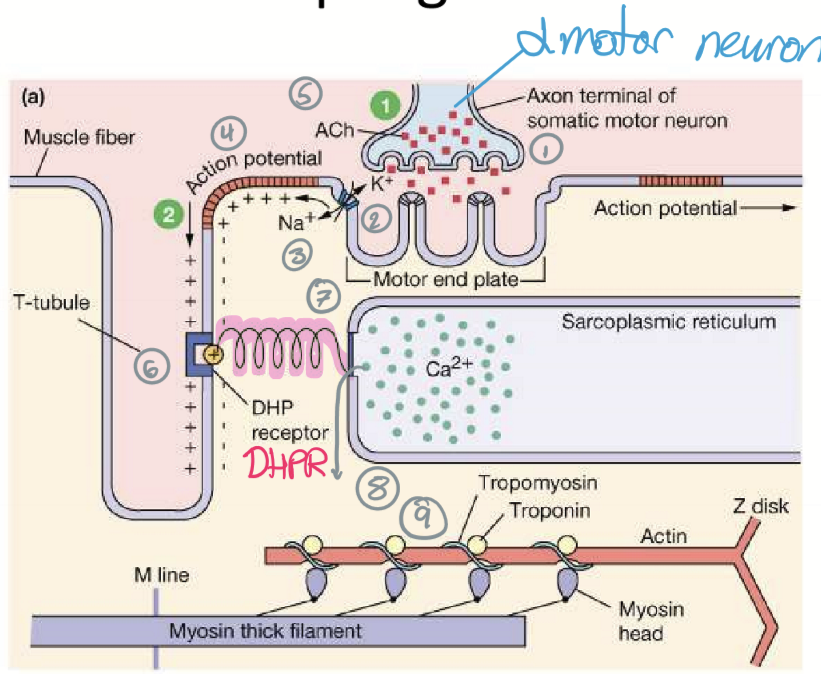
How does Excitation-Contraction Coupling Work in Skeletal Muscle Fibers?
ACh released from somatic motor neuron
nAChR open
Motor end-plate potential
Action potential forms inside sarcolemma
ACh is degraded while Dihydropyridine receptor (DHPR) is activated
DHPR opens Ryanodine (RyR)
Ca is released and binds to tropomyosin
Crossbridge cycling (more Ca present causes a stronger contraction)
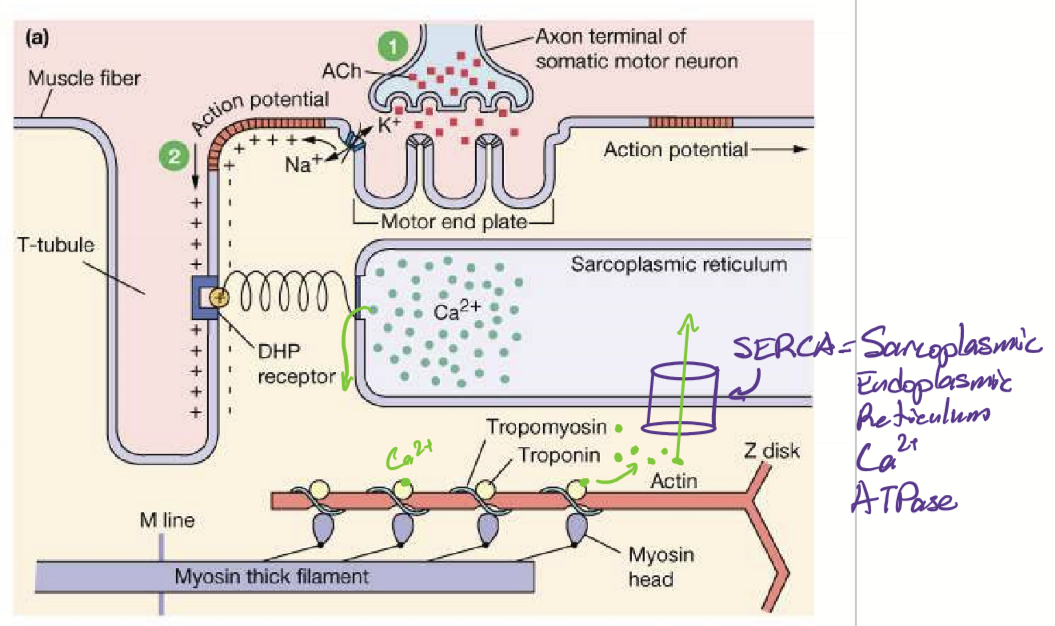
How does a muscle fiber relax?
Ca is removed by SERCA. The Ca ions detach from troponin, cuasing tropomyosin to move back into its position, covering the binding sites on actin filaments. mysin heads no long form cross-bridges with actin, leading to relaxation of muscle fiber.
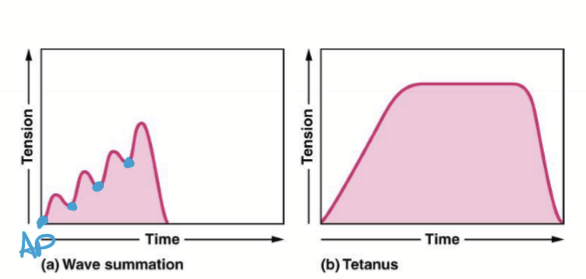
What is summation in skeletal muscles and what is its mechanism?
Summation is the characteristic where Ca concentrations determine strength of contraction.
Mechanism:
twitch beings
motor neurons fires before relaxation
More Ca released
More myosin-action cross-bridging
More tension
Eventually stops due to fatigue from lack of either ACh or ATP
What are some etiology for Upper Motor Neuron Syndrome?
CVA
Traumatic Denervation
TumorMultiple Sclerosis
Amyotrophic Lateral Sclerosis
Presentation of Upper motor neuron syndrome
Spastic paralysis/paresis
Hypertonia: Abnormally high level of muscle tone
Hyperreflexia: Overactive reflexes
Fasciculations: involuntary twitching
Positive Babinski Sign: fanning of toes from extensor plantar response
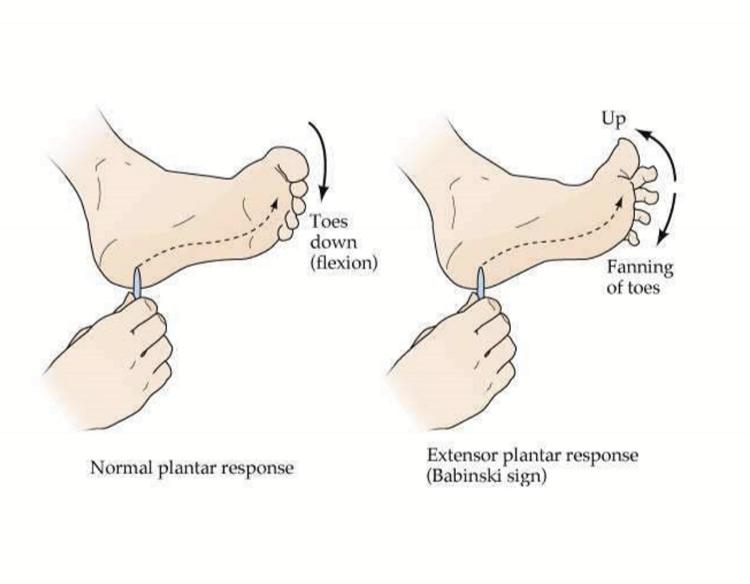
Why do the muscles become spastic in upper motor neuron syndrome?
Descending CST has both stimulator and inhibitor effects. Without inhibition on lower motor neuron, there is an increase in muscle spindle reflex. This makes the skeletal muscle spastic, but overtime atrophy.
What does Tetanus toxin from Clostridium tetani do?
Causes spastic paralysis, such as headache, lockjaw because it inhibits SNARES in inhibitory neurons from synapsing on axon termini
Lower Motor Neuron Symdrome etiologies
traumatic denervation (wallerian degeneration)
Diabetic neuropathy
Guiallain Barre
Amyotrophic lateral sclerosis
Polio
Bell Palsy
Herpes zoster oticus (Ramsay Hunt Syndrome)
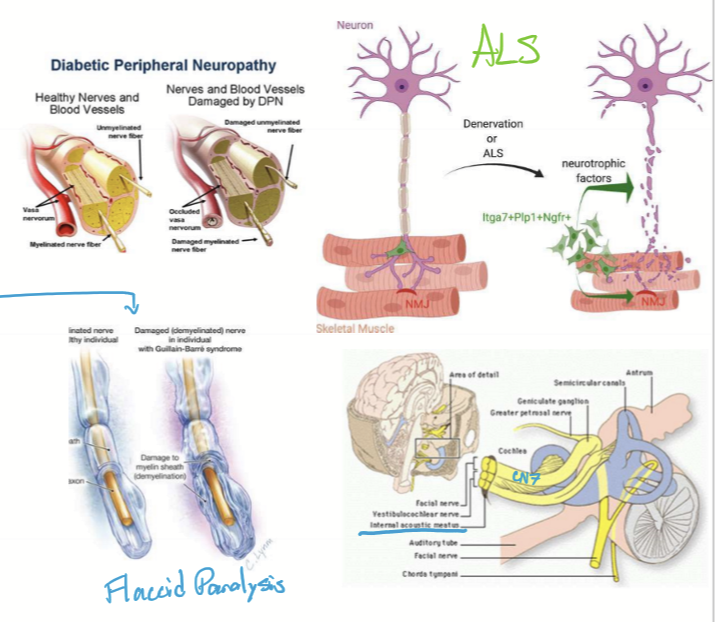
Presentation of Lower Motor Neuron Syndrome
Flaccid paralysis
Paresis
Areflexia: Absence of reflex
Hypotonia: Lack of tone
Fibrillations are spontaneous involuntary contractions of individual muscle fibers, not visible under the skin
Fasciculations: Brief spontaneous contractions of a small number of muscle fibers such as a twitch
Atrophy if late
What is botulism and what are its effects?
Botulism is a toxin released by Clostridium botulinum that causes flaccid paralysis by inhibiting SNAREs of lower motor neuron in NMJ (no ACh released)
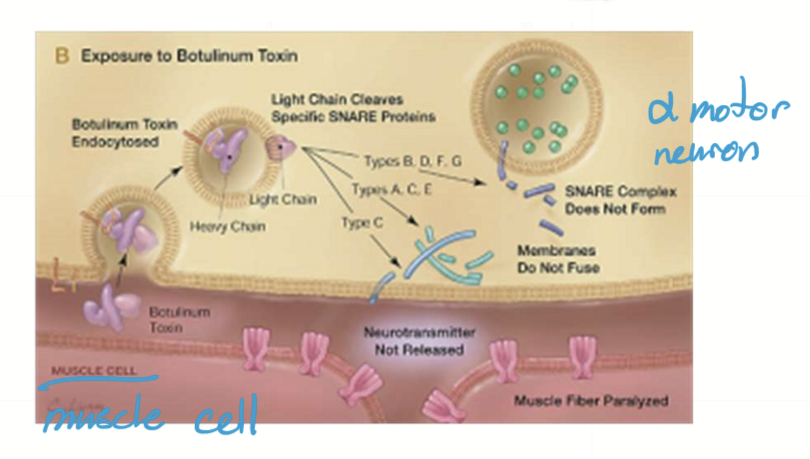
What is Botox used for?
cosmetic reasons
Decrease diplopia via 6th nerve palsy
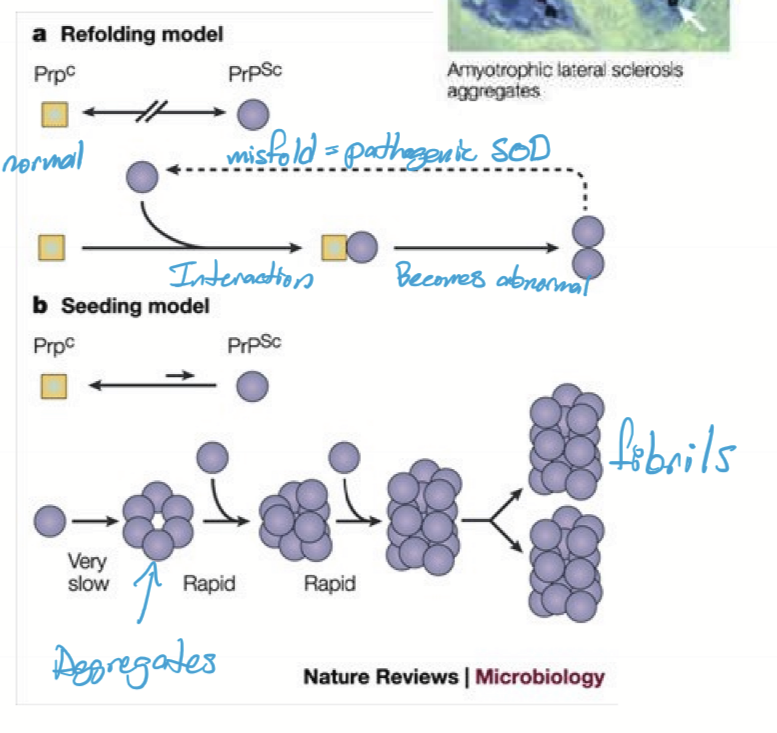
Amyotrophic Lateral Sclerosis (ALS) or Lou Gehrig’s disease is what?
A neurodegenerative disease that affects upper and lower motor neurons. It is Prion-like and patients tend to only live 1-3 years after diagnosis.
What are the presentation of ALS?
limb weakness and paralysis
weakness progresses to other muscles
Eventually respiratory failure
Extraocular muscles somewhat resistant
Etiology of ALS
Sporadic
20% AD in SOD1 gene (super oxide dismutase)
Pathogenesis of ALS:
protein is misfolded
Misfolded protein causes other proteins to misfold
Misfolded proteins aggregate
aggregations become fibrils
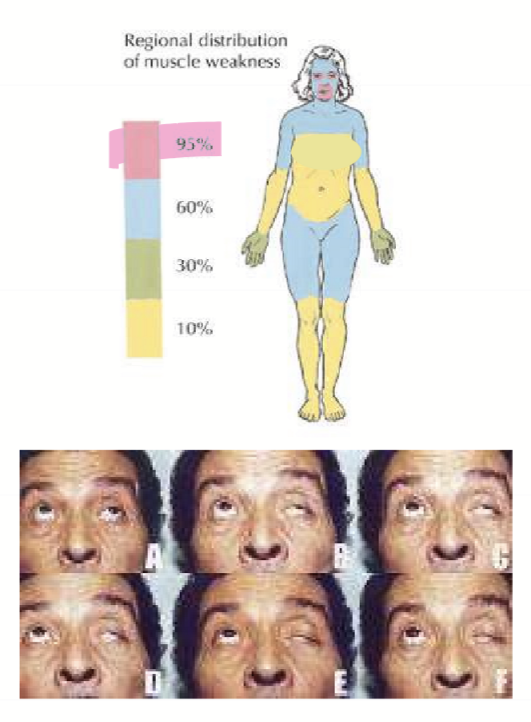
what is the pathogenesis of myasthenia gravis?
Abs bind nAChR
Causes downregulation of nAChR
Weak end-plate potential d/t lack of channels
Decreased frequency of AP = weaker contractions
Compensatory increased firing by alpha motor neuron causes ACh to be exhausted
Muscle fatigues with time
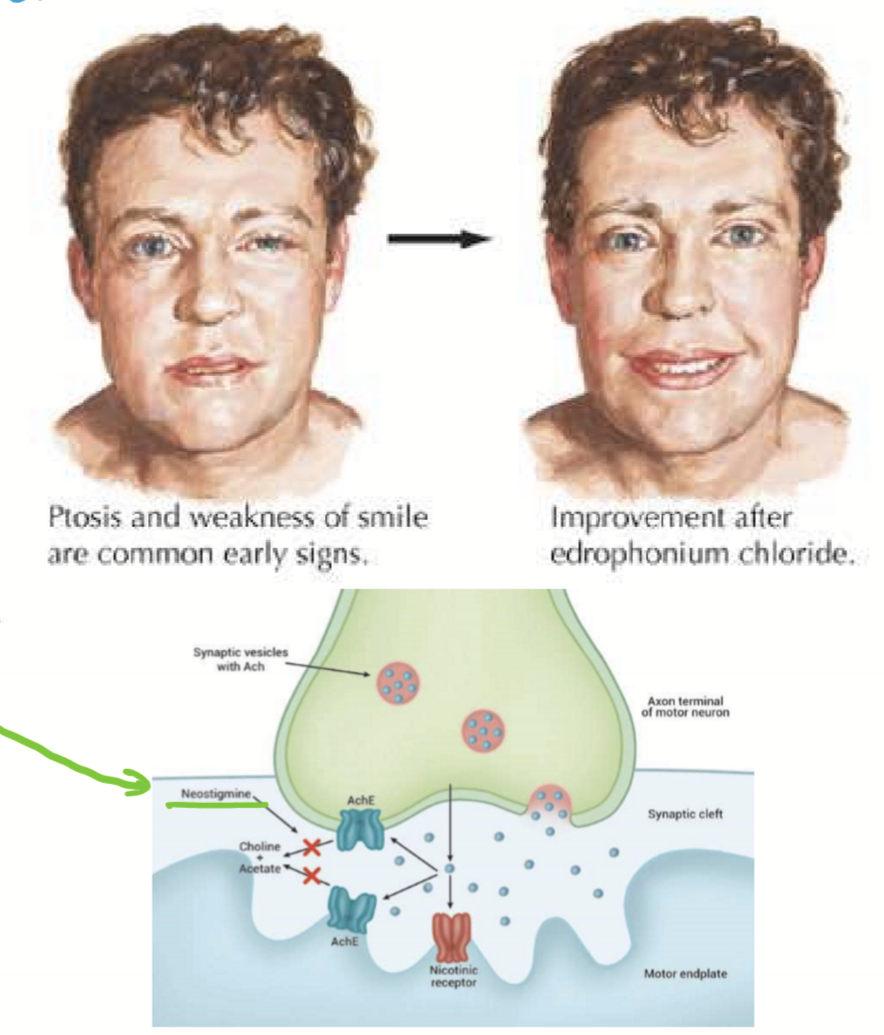
Clinical presentation of myasthenia gravis
first affects eyes and mouth:
ptosis
diplopia
dysphagia (difficulty eating)
Difficulty talking
Later effects neck, hips, and shoulders
Diagnostic tests for myasthenia gravis.
Ice test targets AChE (acettylcholine esterase) to slow down ACh degradation
Endrophonium test (Tensilon IV): a short-acting AChE
Treatment for myasthenia gravis
Neostigmine (inhibits AChE)
Steroids
Thymectomy (surgical procedure to remove thymus gland producing T-cells)
What are muscular dystrophy diseases?
Duchenne’s MD & Oculopharyngeal MD (affects lids and pharynx=swallowing)
What treatments are there for muscular dystrophy?
Currently no cures for genetic disorders cuasing muscular dystrophy
What causes unilateral ptosis?
trauma
horner syndrome
thrid nerve palsy
Botox
What causes bilateral ptosis?
aging
myathenia gravis
Oculopharyngeal muscular dystrophy