PSYC 301 Final - Dysfunction Associated with Psychiatric Disorders 3
1/10
Earn XP
Description and Tags
Bipolar Disorder
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
11 Terms
What are the 3 main states of bipolar disorder?
Depressive
Hypomanic
Manic
Describe the DSM-5 criteria for a major depressive episode
New or worsened, daily, for two weeks in a row. 5+ of:
Depressed mood
Loss of interest or pleasure in almost all activities
Changes in weight or appetite
Sleep changes
Psychomotor changes (agitated or slowed)
Tiredness, fatigue, low energy
Sense of worthlessness or guilt
Impaired ability to think
Recurrent thoughts of death, suicidal ideation, or suicide attempts
Describe the DSM-5 criteria for hypomania
Abnormal/persistent/elevated/irritable mood + increased goal-directed activity/energy most of the time for at least 4 days
Some of the following:
Increased energy and activity
Persistent mild elevation of mood
Feelings of well-being and both physical + mental efficiency
Increased sociability and talkativeness (or increased irritability in some)
Increased sexual energy
Decreased need for sleep
None to the extent that they lead to severe disruption of work/result in social rejection, + no hallucinations/delusions (ex. psychosis)
Describe the DSM-5 criteria for a manic episode
Abnormal/persistent/elevated/expansive + increased goal directed energy, most of the time, for at least 1 week
3+ of the following to a significant degree:
Inflated self esteem or grandiosity
Decreased need for sleep
More talkative than usual/pressure to keep talking
Flight of ideas/subjective experience that thoughts are racing
Distractibility
Increase in goal-directed activity or psychomotor agitation
Excessive involvement in activities that have a high potential for painful consequences
Causes marked impairment in social or work life, necessitates hospitalization, or includes psychosis (hallucinations and/or delusions)
Bipolar I vs. Bipolar II
Bipolar I: Involves at least 1 manic episode (1 week/requires hospitalization)
Bipolar II: Hypomania + depressive episodes
In general, individuals with bipolar spend more time in deprressive than manic state
can have a combination of manic and depressive states (ex. risky behaviour + low mood)
What are the prevalences of the different types of BD?
0.6% for Bipolar I
0.4% for Bipolar II
Commonly begins in young adulthood
Potential high impact for either form
Ex. high risk of suicide attempts
Large changes in quality of life/socialization
Life course:
BD diagnosable after clear alternating waves of mania and depression

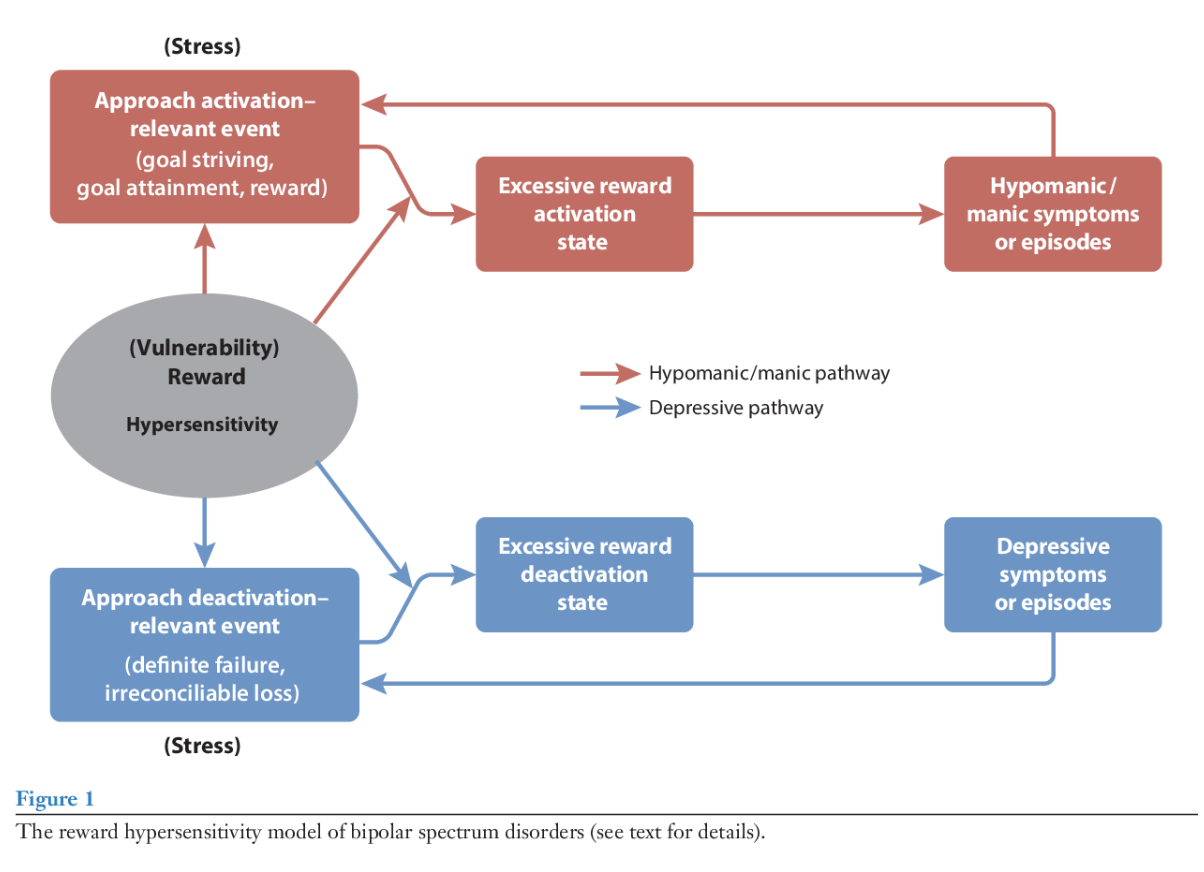
Reward Hypersensitivity Model of BD
Being hypersensitive to reward = trait that predisposes someone to developing BD
Goal attainment can lead to excessive reward states + ultimately (hypo)mania
Goal nonattainment can lead to excessive reward deactivation and a depressive state
What evidence is there for the Reward Hypersensitivity Model?
Euthymic (‘normal’ state) individuals with BD
Show excessive activity in frontal-striatal reward-related areas in response to reward related cues
Make more risky choices on controls (ex. Gambling tasks)
Prodromal Features
Hypomania + mania: Excessive goal setting + increased success expectancies
Depressive Episodes: Decreased motivation + goal setting and low self confidence
Teenagers (14-19) who score high on reward sensitivity → more likely to develop bipolar disorder in a prospective study
What are some structural brain changes associated with BD?
Structural reductions in gray matter (similar areas to functional, ex. PFC, limbic)
Driven by time spent in manic episodes
Associated with neuroinflammation, stress hormones, etc. that lead to structural changes
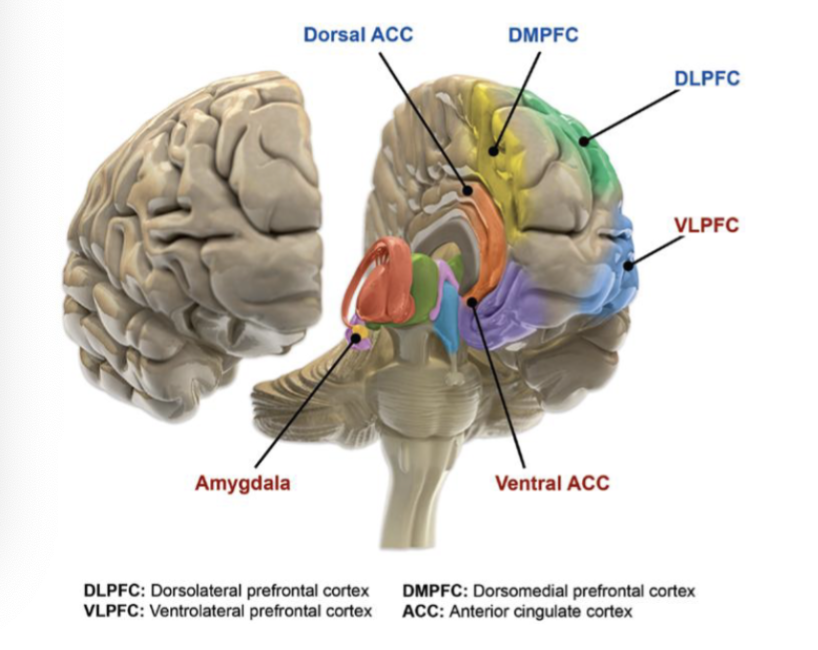
What are some functional brain changes associated with BD?
Increased responsiveness in limbic + Paralimbic areas (in red)
Amygdala
VLPFC (ventrolateral prefrontal cortex)
Ventral ACC (anterior cingulate cortex)
Decreased responsiveness in areas associated with cognitive control (in blue)
Dorsal ACC
DMPFC
DLPFC
What are some treatments for bipolar disorder?
Mood Stabilizers
Lithium
Alone or combined with atypical antipsychotics
Atypical Antipsychotics
Psychotherapy - CBT
Health education/family-focused treatments all have some evidence
Antidepressants alone are not recommended
> 50% of patients do not adhere to treatment